Abstract
The purpose of this study was to evaluate the feasibility of delivering a supervised physical activity program plus standard exercise counseling (PA + EC) versus a supervised physical activity plus motivationally-enhanced behavioral counseling (PA + BC) in prostate cancer survivors. Secondary outcomes included objectively assessed PA, quality of life, body composition, cardiorespiratory fitness, cognitive functioning, and physical function. Twenty-six prostate cancer survivors were randomized to a 12-week supervised PA program plus standard exercise counseling or a 12-week supervised PA plus behavioral counseling based on the Multi-Process Action Control framework. Feasibility was determined through enrolment rate, measurement completion rate, loss-to-follow-up, adherence to the intervention, adverse events, and program evaluation items assessing burden and satisfaction. Of the 26 prostate cancer survivors enrolled (Mage = 65.6 ± 6.8), 96% completed the intervention. Measurement completion rates for the study measures were 88.5%. Adherence to the supervised PA sessions was 92% (completed 11/12 supervised PA sessions) and 100% (completed 12/12 supervised PA sessions) in the PA + EC and PA + BC group, respectively. Adherence to the home-based PA sessions was 70% (completed 7/10 home-based sessions) and 90% (completed 9/10 home-based sessions) in the PA + EC and PA + BC group, respectively. Overall, prostate cancer survivors were highly satisfied with the intervention components and found it rewarding, useful for research helping others, and useful for them personally. The patterns in the secondary outcomes were consistent with a positive impact of the intervention, favoring the PA + BC group. Preliminary evidence suggests that adding behavioral counseling to supervised PA in prostate cancer survivors may be feasible and result in better adherence to PA compared to exercise counseling alone, although additional refinement is needed. A combination of supervised and home-based PA may be feasible for behavior change in the self-management of prostate cancer. The study is registered with http://ClinicalTrials.gov (ID NCT03191968).
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Over the past two decades, the 5-year relative survival rate in prostate cancer for all stages combined has increased from 68% to nearly 100%, resulting in a growing number of prostate cancer survivors (Siegel, Miller, & Jemal, 2019). Supportive care interventions are needed to reduce the chronic and late-appearing treatment-related side effects during the transition into survivorship. Physical activity (PA) has a positive impact on clinical outcomes such as improvements in overall quality of life (QoL), cancer-specific mortality, and reducing treatment-related toxicities across many cancer survivor groups (Mishra et al., 2012), including prostate cancer survivors (Antonelli, Freedland, & Jones, 2009; Bonn et al., 2015; Keogh & MacLeod, 2012).
There is strong evidence that aerobic and resistance exercise in prostate cancer survivors result in clinically meaningful improvements in cardiorespiratory fitness, muscular strength, physical functioning, QoL, and fatigue (Baumann, Zopf, & Bloch, 2012; Bourke et al., 2016; Keogh & MacLeod, 2012). Furthermore, anticancer therapy, radiotherapy, or androgen-deprivation therapy (ADT) can cause short-term and long-term cognitive impairment for prostate cancer patients (Fang et al., 2020). However, the evidence supporting PA as a strategy to mitigate cancer-related cognitive impairment is still limited. These positive benefits resulting from PA are only realized if cancer survivors adhere and maintain their PA levels. Nevertheless, the majority of prostate cancer survivors are not meeting public health PA guidelines of 150 min of moderate-to-vigorous PA (MVPA) per week, and at least 2 days of strength training per week (Campbell et al., 2019; Schmitz et al., 2010) to accrue these benefits.
PA prescriptions consisting of supervised exercise consisting of thrice-weekly aerobic activity for 30 min and twice-weekly of resistance exercise for at least 12 weeks has shown the strongest evidence for cancer-related health outcomes including anxiety, depressive symptoms, fatigue, physical functioning, and QoL (Campbell et al., 2019). In addition, supervised programs produced larger effects on PA compared to unsupervised programs (Sheeran et al., 2019). Supervised exercise programs have the advantage of ongoing monitoring and support to minimize treatment-related side effects by qualified healthcare professionals and fitness instructors with specialized knowledge in physical therapy or clinical exercise physiology, exercise prescriptions, and working with cancer survivors (Schmitz et al., 2019). However, given that cancer survivors may face several barriers to engaging in supervised PA (e.g., distance from clinical or community programs, program cost, lack of childcare), there is a growing need to develop and assess the efficacy of interventions that employ home-based approaches (Groen, van Harten, & Vallance, 2018; Schmitz et al., 2019).
However, PA declines significantly after the supervised intervention has been completed (Courneya et al., 2008, Courneya et al., 2009). Therefore, home-based interventions may be efficacious for implementing behavior change. They are less burdensome for those who experience travel and scheduling barriers and have broad reach (Groen et al., 2018; Schmitz et al., 2019). Research examining the effect of short-term supervised exercise programs on motivational outcomes and longer term PA among cancer survivors is limited, especially theoretical approaches to identify key motivational outcomes to facilitate the adoption and maintenance of PA (Grimmett et al., 2019; Finlay, Wittert, & Short, 2018). Little is known about which intervention modalities are feasible and efficacious. Previous studies examining exercise in prostate cancer survivors have compared supervised PA to usual care (Bourke et al., 2014), with only one behavior change intervention comparing two different types of implementation intentions intervention (self-administered vs. telephone-assisted) in prostate cancer survivors to increase PA levels (McGowan, North, & Courneya, 2013).
For successful behavior change, it is necessary to move beyond intention-focused theories to reduce the intention-behavior gap (Rhodes, 2017). One such framework is the Multi-process Action Control (M-PAC) framework (Rhodes, 2017), which has a causal structure where an individual moves from intention formation to adoption of action control and onto maintenance of action control. Intention formation is predicated on initiating reflective processes (i.e., instrumental attitude and perceived capability). Reflective processes are hypothesized to influence intention formation and initiate regulatory processes to enact this intention (i.e., affective attitude and perceived opportunity). The translation of intention into PA (i.e., action control) is determined partially by regulatory processes (e.g., action planning, coping planning, self-monitoring, social support) during the initial adoption of the behavior. Continuation of PA action control is thought to include the addition of reflexive processes (habit, identity) for long-term PA maintenance. The utility of the M-PAC has shown promise in an exercise telephone counseling intervention in hematological cancer survivors (Vallerand, Rhodes, Walker, & Courneya, 2018).
No study has compared two different counseling components, in addition to supervised PA, in prostate cancer survivors. Feasibility studies are essential before designing larger scale efficacy trials to determine acceptability, recruitment, retention, and to determine intervention components that are essential for behavior change (Eldridge et al., 2016; Lancaster, Dodd, & Williamson, 2004; Leon, Davis, & Kraemer, 2011). Following the conceptual framework for defining pilot and feasibility studies (Eldridge et al., 2016), a pilot RCT is the necessary step towards examining if and how behavioural regulation strategies improve PA levels in prostate cancer survivors in preparation for a larger RCT. Therefore, the primary purpose of this study is to evaluate the feasibility of delivering a supervised PA program plus standard exercise counseling (PA + EC) versus a supervised physical activity plus motivationally-enhanced behavioral counseling (PA + BC) in prostate cancer survivors. Secondary outcomes include examining the effects of the intervention on objectively assessed PA, QoL, body composition, cardiorespiratory fitness, objectively-assessed cognitive functioning, and physical function.
Methods
Study design
This study was a pilot single center, two-armed, single blind, RCT comparing PA + EC to PA + BC.
Setting and participants
This study took place at the University of Illinois at Urbana-Champaign from July 2017 to May 2018. Prostate cancer survivors were recruited through the Carle Cancer Center through oncologist referral, mailing brochures using a tumor registry at the cancer center, university listservs, flyers, and newspaper advertisements. Eligibility criteria included: (a) 18–80 years; (b) histologically confirmed prostate cancer (Stage I-IIIa) but now cured or in remission; (c) ability to communicate in English; (d) not meeting PA guidelines of ≥ 150 min of moderate-to-vigorous PA per week; and (e) obtaining written approval from their physician to participate. Exclusion criteria included: (i) neurological or musculoskeletal comorbidities inhibiting exercise; (ii) absent for more than 3 consecutive days (pre-planned or anticipated absences) during the period of their 12-week intervention; and (iii) uncontrolled comorbidities. Potentially eligible patients at the cancer center were screened by their oncologist and referred to the study staff for further screening by phone to determine eligibility. Participants recruited through other channels outside of the cancer center were requested to contact the research staff by telephone or e-mail. The study was approved by the Institutional Review Board at the University of Illinois, and all participants provided written informed consent.
Randomization and blinding
Following completion of baseline measures, eligible participants were randomized using permutated blocks of 4 in a 1:1 ratio to either the PA + EC group or PA + BC group using a web-based randomization program (Research Randomizer). The allocation sequence was concealed from the study staff enrolling and assessing participants in sequentially numbered, opaque, and sealed envelopes. Participants were blinded to group assignment and outcome assessors were kept blinded to the allocation.
Physical activity interventions
Prior to randomization, participants completed two study visits. Visit one consisted of a graded submaximal treadmill exercise test, anthropometrics (height and weight), and questionnaire completion. Visit 2 consisted of a neuropsychological test battery.
The goal of both arms of the intervention was to gradually increase PA to a minimum of 150 min of moderate intensity or 75 min of vigorous intensity PA per week. Prostate cancer survivors in both arms were given an individualized aerobic prescription at a moderate-to-vigorous intensity. The duration and intensity accounted for the participant’s baseline fitness test results, PA history, and PA-related preferences. The prescribed intensity was 50–60% of the maximum heart rate reserve (i.e., moderate intensity) for weeks 1–5 and 60–75% (i.e., moderate to vigorous) for the remainder of the program. Initial exercise duration was individualized, but the target duration was at least 10 min per session. The aerobic duration gradually increased by 5 min each subsequent week. An aerobic duration of 50 min was achieved by and maintained after week 6 of the program to meet exercise guidelines (i.e., 150 min/week). Heart rate monitors were provided to all participants during the supervised PA sessions to monitor their target heart rate zones (calculated based on baseline cardiorespiratory fitness data). The PA specialists recorded the type and duration of exercise performed, as well as participants’ average heart rate and rating of perceived exertion scale (i.e., 6–20 Borg scale). Participants were also instructed by the PA specialists on how to take their resting heart rate using a heart rate monitor, to evaluate their rating of perceived exertion (i.e., 6–20 Borg scale) and record their warm-up, exercise, and cool down heart rate when they exercised at home. Supervised aerobic PA sessions were completed on treadmills, cycle ergometers, or a combination. Prostate cancer survivors were also provided with a resistance training component using resistance bands. The whole-body strength training program consisted of 2 sets of 10 to 12 repetitions targeting legs, abdominals, and arms. These sessions followed immediately after the aerobic PA sessions.
Over the 6-week period, both intervention groups were prescribed a combination of face-to-face supervised PA sessions, and unsupervised home-based sessions as seen in Table 1. The supervised PA program was 6 weeks in duration and prostate cancer survivors were asked to exercise on their own for 6 weeks for the home-based portion, for a total of 12 weeks. Prostate cancer survivors were provided with a logsheet to track the type of PA performed, PA duration, average heart rate using a heart rate monitor, and their rating of perceived exertion when they exercised at home. The PA specialists (JW [female] and DS [male]) were certified personal trainers from the American College of Sports Medicine (ACSM-CPT) and delivered the counseling sessions. The supervised PA sessions were delivered by male and female senior undergraduate students majoring in Kinesiology. Our study followed the treatment fidelity guidelines for health behavior research that have been recommended by the National Institutes of Health (NIH) Behavior Change Consortium (Bellg et al., 2004). The components of treatment fidelity include: (a) study design, (b) provider training, (c) treatment delivery, (d) treatment receipt, and (e) enactment of treatment skills. Specifically, the PA specialists received three training workshops with the Principal Investigator consisting of the delivery of exercise testing (workshop 1; 5 h), counseling sessions (workshop 2; 6 h), and neuropsychological testing (workshop 3; 3 h). These workshops were accompanied by scripted training and a detailed manual used to prepare PA specialists for their mock sessions. The mock sessions were an additional three days of training with the Principal Investigator on the delivery of exercise testing, counseling sessions, and neuropsychological testing. To further improve the fidelity of the intervention delivery, PA specialists were provided with checklists to ensure that the core components of the supervised PA and counseling sessions were delivered as intended. After each session with the participant, the Principal Investigator reviewed the checklists for completion, and provided further feedback to the PA specialists. All supervised PA and counselling sessions were delivered as intended to all participants in the study.
Intervention: supervised physical activity (PA) program plus behavioral counseling (PA + BC)
The PA + BC group received a total of nine behavioral counseling sessions with a PA specialist, and the corresponding counseling session was delivered after each supervised PA session. The behavioral counseling sessions were based on the M-PAC (Rhodes, 2017), and included behavior change techniques such as social support, goal setting, self-monitoring, action planning, habit, and identity. Each of these techniques mapped onto M-PAC’s targeted constructs of reflective, regulatory, and reflexive processes (Table 1). A PA manual was distributed to each participant as an ongoing resource, which was developed separately for each of the two groups, with the behavioral counseling group containing additional content (i.e., theory-based counseling). Upon completion of the 6-week supervised PA program, participants were provided with an individualized PA prescription based on their fitness level to continue achieving the PA intervention goal for the home-based component. Prostate cancer survivors were encouraged to formulate short- and long-term goals, as well as creating a detailed plan for achieving PA guidelines. Each counseling session was approximately 30–45 min in duration (Table 1).
Attention control: supervised physical activity (PA) program plus standard exercise counseling (PA + EC)
In addition to the supervised PA sessions, the PA + EC received nine standard PA counseling sessions based on exercise training principles to teach proper PA and resistance training techniques, how to monitor intensity, and to progress PA safely and effectively to achieve the public health PA guidelines. These sessions were delivered by PA specialists (JW and DS) immediately following the supervised PA sessions. Each counseling session was approximately 30–45 min in duration (Table 1).
Measures
Feasibility was determined through enrollment rate, measurement completion rate, loss-to-follow-up, adherence to the intervention, adverse events, and program evaluation items assessing burden and satisfaction. Adherence to the supervised PA was based on the number of supervised PA (i.e., completing the PA minutes prescribed) and counseling sessions completed, defined as the number of supervised PA and counseling sessions attended, divided by the number of supervised PA and counseling sessions prescribed. Adherence to the home-based program was defined as the number of home-based sessions completed divided by the number of home-based PA sessions prescribed. Adverse events were monitored, assessed and recorded during exercise testing and supervised PA sessions throughout the intervention period. Acceptability was measured through a program satisfaction survey completed post-intervention (i.e., 12-weeks) that assessed the burden of exercise testing and participant’s perception regarding the PA manual, individual counseling sessions (only for the PA + BC group), and the overall impression of the trial. Closed-ended questions with responses options on a Likert 7-point scale ranging from 1 (not at all) to 7 (very much) were used.
Secondary outcomes
The secondary outcomes were objectively assessed PA, cardiorespiratory fitness, physical function, QoL, cognitive functioning, and anthropometric measures assessed at baseline and 12 weeks (post-intervention).
Physical activity
Objectively assessed PA was measured using Actigraph GTX3+ accelerometers (Pensacola, FL). Participants wore the accelerometer on their non-dominant hip during waking hours for 7 consecutive days. Data were analyzed if there were no extreme counts (> 20,000) and if data were available for at least 10 valid hours of wear time on 4 or more days per assessment period. Data were downloaded in 60-s epochs and processed and converted to mean counts per minute in ActiLife software package (Version 6; Actigraph) to estimate daily minutes of light (101–1951 counts min−1), moderate (1952–5724 counts min−1), vigorous (≥ 5725 counts min−1), and total moderate-to-vigorous physical activity (MVPA; ≥ 1952 counts min−1) based on established cut-points (Freedson, Melanson, & Sirard, 1998). Estimated average daily minutes spent in each activity intensity category was calculated by dividing the number of minutes spent in each category by the total number of valid days worn.
Cardiorespiratory fitness
A modified Balke (Pollock et al., 1982) treadmill test protocol to assess a submaximal oxygen consumption, which was used to predict VO2max (Ferguson, 2014). Participants walked on a treadmill while speed and/or grade increased in 3-min stages until the participant achieved 85% of a pre-determined, age-predicted maximum (220–age) heart rate.
Physical function
The Seniors’ Fitness Test (SFT) (Rikli & Jones, 1999) was used to assess physical function, which consists of a battery of six items used to determine mobility-related fitness parameters: 30-s chair stand test for lower body strength; arm curl test for upper body strength; chair sit-and-reach test for lower body flexibility; back scratch test for upper body (shoulder) flexibility; 8-foot up-and-go test for agility and dynamic balance; and the 6-min walk test for aerobic endurance.
Cognitive functioning
The NIH toolbox cognition battery with computerized cognitive tasks and automated scoring was used (Weintraub et al., 2013). The toolbox generated individual measure scores and the following summary scores: Cognitive Function Composite Score, Fluid Cognition Composite Score (includes Dimensional Change Card Sort Test, Flanker, Picture Sequence Memory, List Sorting, and Pattern Comparison measures), and Crystallized Cognition Composite Score (includes Picture Vocabulary and Reading Recognition measures). These measures have been validated against gold standard measures and have high internal consistency and test–retest reliabilities.(Weintraub et al., 2013) Self-reported cognitive function was measured using the Functional Assessment of Cancer Therapy Cognitive Scale–Version 3 (FACT-Cog-3) (Wagner et al., 2009). Higher scores indicate better perceived cognitive function.
Quality of life
Disease-specific QoL was assessed by the well-validated Functional Assessment of Cancer Therapy-Fatigue (FACT-G) which consists of 27-items assessing physical well-being (PWB), functional well-being (FWB), emotional well-being (EWB), and social well-being (SWB) (Cella et al., 1993). Cancer-specific symptoms of fatigue were assessed using the FACT-Fatigue (Cella, Eton, Lai, Peterman, & Merkel, 2002) The validated FACT-Prostate (FACT-P), which includes the prostate cancer subscale, was used to assess the most important targeted symptoms and concerns for prostate cancer survivors (Esper et al., 1997). Physical and functional well-being was also assessed using the Trial Outcome Index (TOI)-Prostate (Cella, Nichol, Eton, Nelson, & Mulani, 2009) and TOI-Fatigue (Cella et al., 2002). TOI-Prostate and TOI-Fatigue were calculated by summing the PWB and FWB subscales along with the prostate cancer subscale and fatigue subscale, respectively. On all scales, higher scores indicate better QoL and fewer symptoms.
Anthropometric measures
Height and weight were measured using an electronic stadiometer and scale (model 763, Seca: Chino, CA) and used to calculate body mass index (BMI) [weight per height squared (kg/m2)]. Waist circumference was measured using a horizontal measure taken directly above the iliac crest.
Demographic and medical information
Standard health history questionnaire assessing self-reported demographic (e.g., age, marital status, education) and medical history (e.g., treatments received, date of diagnosis, disease state) were collected (Courneya et al., 2014; Vallance, Courneya, Plotnikoff, Yasui, & Mackey, 2007).
Data analyses
All statistical analyses were performed using SPSS 24. An a priori sample size calculation was not conducted due to the feasibility nature of this study (Lancaster et al., 2004; Leon et al., 2011). Descriptive statistics including frequencies, means, and standard deviations were used to characterize the sample and report on feasibility outcomes. The intervention effect on PA behavior (and all secondary outcomes) was assessed using an analysis of covariance (ANCOVA), where the dependent variable was post-intervention outcomes and the independent variable was group assignment, while controlling for the baseline value of the outcome and time since treatment. All analyses were conducted based on an intention-to-treat basis. Given that the purpose of this feasibility trial was to inform a larger RCT, outcomes were interpreted for potential clinical significance based on the direction and magnitude of numerical differences.
Results
Participant flow through the trial is reported in Fig. 1. Of the 56 prostate cancer survivors that responded to our invitation, 26 prostate cancer survivors were eligible and randomized in the trial, generating a 46.4% enrollment rate. Twenty-five participants completed the PA intervention, representing a 96.2% retention rate. Measurement completion rates for the study measures were 88.5%. Three participants were lost-to-follow-up. One participant from the PA + EC group dropped out after week 3 due to a scheduled surgery, but agreed to complete the questionnaires and cognitive assessments post-intervention. However, all participants who were randomized were included in the analysis following an intention-to-treat approach.
Sample characteristics
Baseline demographic, medical, and clinical characteristics of the participants are reported in Table 2. Overall, participants had a mean age of 65.6 ± 6.8, 84.6% were married, and the mean BMI was 30.2 ± 5.8 kg/m2. The mean number of months since diagnosis was 95.8 ± 67.8, mean number of months since treatment was 87.5 ± 72.2, 69.2% had received surgery, and 92.3% had localized prostate cancer.
Intervention adherence
In terms of intervention delivery, prostate cancer survivors completed an average of 11.5 of the 12 supervised exercise and counseling sessions over the 12-week period (96%), with the PA + EC group and PA + BC group completing 92% and 100% of the supervised exercise and counseling session, respectively. In terms of the home-based sessions, prostate cancer survivors completed an average of 8 of the 10 home-based exercise sessions (80%). The PA + EC group and PA + BC group completed 70% and 90% of the home-based sessions, respectively.
Program evaluation and satisfaction
Program evaluation and satisfaction with the trial is presented in Table 3. Overall, prostate cancer survivors were highly satisfied with the intervention components and found it rewarding, useful for research helping others, and useful for them personally (means > 6/7; higher scores indicate high satisfaction). Burden of all aspects of the trial was also quite low (means < 2/7; lower scores indicate low burden). Prostate cancer survivors also found the supervised PA and overall counseling sessions to be quite helpful in increasing PA levels.
Secondary outcomes
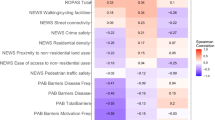
Mean number of minutes for objectively assessed total PA, moderate PA, vigorous PA, and percentage of prostate cancer survivors meeting PA guidelines for baseline and post-intervention are displayed in Table 4. Objectively assessed MVPA minutes favored the PA + BC group by +24.0 min. The percentage of prostate cancer survivors meeting objectively assessed PA guidelines favored the PA + BC group with 76.9% (10/13) meeting PA guidelines at post-intervention compared to the PA + EC group with 53.8% (7/13).
Supplementary Table 5 provides the change in objective measures of fitness from baseline to post-intervention for the PA + EC versus PA + BC group. A decrease was observed for the 30-s arm curls for the PA + BC group compared to the PA + EC group (mean change = − 2.0). Increases were noted in VO2max by 3.2 ml/kg/min, 6-min walk by 28.9 ft, sit and reach by 0.9 cm, 8-foot up & go by 0.2 s, and BMI by 0.1 kg/m2, that favored the PA + BC group. Adjusted between-group differences for health-related QoL scales are presented in Supplementary Table 6. Adjusted between-group differences in prostate cancer-specific QoL reached the cut-point to be considered clinically meaningful (i.e., 6–10 for FACT–Prostate; 2 to 3 for prostate cancer subscale) (Cella et al., 2009) Specifically, prostate-specific QoL as assessed by the FACT-Prostate worsened by 6.4 points and 2.9 points in the prostate cancer survivors subscale in the PA + BC group. There were no clinically meaningful changes observed in other health-related QoL scores.
Changes in objectively assessed and self-reported cognitive function scores from baseline to post-intervention for the PA + EC versus PA + BC group are presented in Supplementary Table 7. Adjusted group mean differences favoring the PA + BC group were noted in the scores for the picture vocabulary test by 0.5, flanker task by 1.4, dimensional change card sort test by 0.8, list sorting working memory test by 3.5, pattern comparison processing speed test by 2.7, and auditory verbal learning test (a measure of immediate recall) by 2.6. Furthermore, improvements in the composite scores were noted including the fluid cognition composite score by 2.2, crystalized cognition composite score by 0.3, and the total cognition composite score of 1.2, favoring the PA + BC group. There were no clinically meaningful changes observed in the self-reported cognitive function as assessed by the FACT-Cog and its subscales.
Discussion
To our knowledge, this is the first study to pilot a PA behavior change intervention with prostate cancer survivors using the M-PAC. The findings of this study will be used to inform larger, definitive RCTs by examining what aspects of the trial methods were feasible, as well as further refinements that need to be made. Specifically, previous behavior change trials in prostate cancer survivors have typically employed PA adoption and action control processes with limited attention to PA maintenance (Finlay et al., 2018; Hallward et al., 2018). Our pilot RCT is noteworthy given that it differed from standard approaches to supervised PA interventions with the addition of reflective, regulatory, and reflexive processes used to facilitate behavior change. The intervention was feasible and well received by prostate cancer survivors, with recruitment and adherence rates that were consistent or higher than other distance-based PA interventions in cancer survivors (McGowan et al., 2013; Vallerand et al., 2018). In terms of our secondary outcomes, the PA + BC group increased MVPA by 24 min more than the PA + EC group did. However, there remain some modifications to trial methods and intervention components that are needed for PA adherence before advancing to a definitive RCT.
Enrollment rates for distance-based PA interventions vary widely with reported rates between 24–89% (Goode, Lawler, Brakenridge, Reeves, & Eakin, 2015). While our enrollment rate (46.4%) was consistent with previous research, our study relied mainly on self-referrals, which attracts highly motivated cancer survivors, well-educated, Caucasian, and those with better health and functioning. This does not appear to be representative of the larger cancer population and is a common observation in many exercise oncology trials, including distance-based interventions (Groen et al., 2018). Efforts are needed to recruit prostate cancer survivors that are less educated, more ethnically diverse, diagnosed with later stage disease, obese, and poorer functioning (Groen et al., 2018). Attending hospital rounds and having a clinical research coordinator recruiting in-person at the cancer center would further assist oncologists in patient referrals to the study. Furthermore, adopting multi-site trials to increase the sample size are also needed to ensure adequately powered RCTs.
We report a retention rate of 96.2% and intervention adherence of with the PA + EC group and PA + BC group completing 92% and 100% of the supervised exercise and counseling session, respectively. The high retention and adherence rates are encouraging and are similar to another PA intervention, although in breast cancer survivors, that have adopted a combination of supervised and home-based components (Rogers et al., 2015). In addition, our retention and adherence rates were superior to other behavior change interventions in prostate cancer survivors (Finlay et al., 2018; McGowan et al., 2013). It is possible that transitioning prostate cancer survivors from supervised to home-based programs are needed to demonstrate the exercises that need to be performed, as well as how to successfully apply behavioral regulation strategies in the initial stages of the intervention.
Although few interventions have targeted behavior change as a primary outcome in prostate cancer survivors, the majority of these trials included either supervised PA programs in a gym or clinic setting, home-based programs, or online programs only (Finlay et al., 2018). However, our results are consistent with a behavior change intervention focusing on implementation intentions in prostate cancer survivors, although telephone-based (McGowan et al., 2013). Furthermore, Vallerand et al. (2018) assessed the feasibility of a telephone counseling intervention based on the M-PAC framework to increase PA in hematologic cancer survivors. Although this was telephone-delivered, it was the only study in cancer survivors that have employed the M-PAC framework similar to our study. Consistent with our trial, Vallerand et al. (2018) found that the telephone counseling group increased weekly aerobic exercise by 139 min more compared to the standard education group (i.e., PA guidelines), representing a large between group difference. This suggests that behavioral support interventions grounded in a theoretical framework such as the M-PAC that focus on translation intentions into actions, developing PA habits (i.e., cue-based reminders) and forming an exercise identity may be a useful framework for PA maintenance.
The increase in PA in our trial (i.e., +24.0 MVPA/wk difference) could result in clinically meaningful improvements for health outcomes in prostate cancer survivors. Previous studies in prostate cancer survivors have reported a benefit with one hour of PA per week for reducing prostate cancer-specific mortality (Bonn et al., 2015), while another study reported greater than 13 MET-h/wk (i.e., ~ 4 h of walking or 2 h of jogging per week) of leisure-time PA was needed (Friedenreich et al., 2016). A recent meta-analysis reported that postdiagnosis PA was associated with greater reductions (i.e., ~ 30% reduction) in cancer-specific and all-cause mortality in cancer survivors, including prostate cancer survivors (Friedenreich, Stone, Cheung, & Hayes, 2020). Future research in larger, definitive RCTs are needed to determine changes in PA needed to achieve a clinically meaningful improvement in health outcomes in prostate cancer survivors.
It is important to note that our trial did not produce nearly as large group differences compared to previous behavior change trials. Future studies should seek to understand the motivational processes responsible for behavior change that our feasibility study was unable to address. However, our trial was able to demonstrate that even with a supervised PA intervention (considered the ‘gold-standard’ for exercise oncology trials), the addition of behavioral counseling strategies was encouraging for increasing PA in prostate cancer survivors. Specifically, motivational processes (i.e., attitudes, perceived capability) were positioned earlier in the intervention as the foundation of motivated action. Reflective processes (i.e., planning, goal setting) regarding managing PA behavior through strategies to translate intentions into behavior were then targeted. Finally, reflexive processes (i.e., habit, identity) were positioned at the end of the intervention for maintaining the behavior and making it a part of who you are. Together, these behavioral counseling strategies represent promising strategies that prostate cancer survivors can use during self-directed, home-based exercise. Following our intervention, 76.9% of prostate cancer survivors in the PA + BC group met the PA guidelines as compared to 53.8% in the PA + EC group, which is promising but additional work is needed. PA is difficult to maintain during follow-up periods of distance-based PA interventions (Goode et al., 2015). Future efforts are needed to examine if prostate cancer survivors require longer periods of behavioral support with booster sessions beyond 12 weeks for PA maintenance. The frequency of delivery of the behavioral support sessions need to be revisited as certain behavior change techniques such as prompts/cues and action and coping planning may need to be repeated during the home-based component of the intervention for sustained PA. While prostate cancer survivors were highly satisfied with the intervention components, further work is needed on how to make the counseling sessions more engaging that may result in greater interest in using these behavior change techniques.
In terms of our secondary outcomes, the intervention produced positive changes in objectively assessed cognitive function. For example, improvements in the auditory verbal learning test, fluid cognition, and overall cognitive function favored the PA + BC group. There are a limited number of exercise RCTs examining cognitive function as an outcome (Campbell et al., 2017; Hartman et al., 2017; Myers, Erickson, Sereika, & Bender, 2017), and no RCTs in prostate cancer survivors that include both subjective and objective cognitive function measures with which to compare our findings to. However, a review of the use of exercise as a potential intervention for cognitive deficits associated with cancer and its treatment demonstrated notable improvements in the cognitive domains of working and visual memory, attention and concentration, cognitive flexibility and inhibitory control and verbal fluency (Myers et al., 2017), consistent with our study. Cognitive changes have been consistently identified by clinicians as one of the most persistent late effects of treatment and difficult to manage for clinicians (LoBiondo-Wood et al., 2014). Therefore, future research is needed to understand the effects of PA on cognitive function in prostate cancer survivors.
Although both PA intervention groups increased their scores in VO2max and the 6-min walk for the fitness-related outcomes, the PA + BC group reached clinically meaningful thresholds of 3.2 ml/kg/min for VO2max and 28.9 feet (~ 8.8 meters) for the 6-min walk (Barlow et al., 2012; Granger, Holland, Gordon, & Denehy, 2015; Holland et al., 2010; Myers et al., 2002). The clinically meaningful change in VO2max is noteworthy given that cardiorespiratory fitness is a strong and independent marker of cardiovascular risk and all-cause mortality. Furthermore, numerous studies have noted a survival benefit with changes in the metabolic equivalent (MET), where each 1-MET (~ 3.5 mL kg−1 min−1) increase in cardiorespiratory fitness was associated with 10–25% improvement in survival (Ross et al., 2016; Kodama et al., 2009). This is encouraging as this small increment is achievable by most individuals, including prostate cancer survivors.
On the contrary, prostate-specific QoL worsened in the PA + BC group compared to the PA + EC group, which were clinically meaningful. However, it is important to note that most QoL scores in both groups improved from baseline to post-intervention, but it did not result in better outcomes when examining between-group differences. It is possible that an extended supervised and home-based intervention, with each component lasting 12 weeks for a total of 24 weeks is needed for better QoL outcomes in prostate cancer survivors. A systematic review in lifestyle interventions in prostate cancer survivors reported that most QoL outcomes were observed for supervised exercise of 12 or 24 weeks, but no significant results on QoL outcomes were observed after non-supervised interventions aimed at motivating and support goal setting for PA (Menichetti et al., 2016).
Our trial should be interpreted within the context of important strengths and limitations. To the best of our knowledge, our study is the first to pilot the effects of adding behavioral counseling to supervised PA in prostate cancer survivors, as well as a focus on cognitive function as a secondary outcome. A strength of our study included the rigorous comparison group since both intervention groups received supervised PA. Other strengths included the combination of face-to-face and home-based PA, the theoretically-based intervention content focused on PA maintenance, the use of objective measures of PA, high rates of adherence, and trivial loss to follow-up. The study limitations included the small sample size, lack of long-term follow-up to determine if PA levels are maintained over time, a highly educated and Caucasian sample that does impact study generalizability, and the self-selected entry into the study may suggest highly motivated prostate cancer survivors with the intention to increase PA.
In conclusion, this pilot study provides preliminary evidence that adding behavioral counseling to supervised PA in prostate cancer survivors is feasible and may improve adherence to PA. Our results highlight the potential of the M-PAC as a theoretical framework to guide and understand behavior change. A combination of supervised PA with a home-based component to transition prostate cancer survivors to unsupervised PA may be feasible and efficacious in producing long-term behavior change. However, further refinement is needed to increase engagement in the use of behavior change techniques. This study provides useful data to inform future RCTs in behavior change, and if replicated, meaningful changes in PA may result in clinically relevant cancer outcomes.
Data availability
The datasets analyzed during the current study are available from the corresponding author on reasonable request.
References
Antonelli, J., Freedland, S. J., & Jones, L. W. (2009). Exercise therapy across the prostate cancer continuum. Prostate Cancer and Prostatic Diseases, 12, 110–115. https://doi.org/10.1038/pcan.2009.4
Barlow, C. E., DeFina, L. F., Radford, N. B., Berry, J. D., Cooper, K. H., Haskell, W. L., et al. (2012). Cardiorespiratory fitness and long-term survival in “low-risk” adults. Journal of the American Heart Association, 1, e001354. https://doi.org/10.1161/jaha.112.001354
Baumann, F. T., Zopf, E. M., & Bloch, W. (2012). Clinical exercise interventions in prostate cancer patients—a systematic review of randomized controlled trials. Supportive Care in Cancer, 20, 221–233.
Bellg, A. J., Borrelli, B., Resnick, B., Hecht, J., Minicucci, D. S., Ory, M., et al. (2004). Enhancing treatment fidelity in health behavior change studies: Best practices and recommendations from the NIH Behavior Change Consortium. Health Psychology, 23, 443–451. https://doi.org/10.1037/0278-6133.23.5.443
Bonn, S. E., Sjölander, A., Lagerros, Y. T., Wiklund, F., Stattin, P., Holmberg, E., et al. (2015). Physical activity and survival among men diagnosed with prostate cancer. Cancer Epidemiology, Biomarkers and Prevention, 24, 57–64. https://doi.org/10.1158/1055-9965.EPI-14-0707
Bourke, L., Gilbert, S., Hooper, R., Steed, L. A., Joshi, M., Catto, J. W. F., et al. (2014). Lifestyle changes for improving disease-specific quality of life in sedentary men on long-term androgen-deprivation therapy for advanced prostate cancer: A randomised controlled trial. European Urology, 65, 865–872. https://doi.org/10.1016/j.eururo.2013.09.040
Bourke, L., Smith, D., Steed, L., Hooper, R., Carter, A., Catto, J., et al. (2016). Exercise for men with prostate cancer: A systematic review and meta-analysis. European Urology, 69, 693–703. https://doi.org/10.1016/j.eururo.2015.10.047
Campbell, K. L., Kam, J. W. Y., Neil-Sztramko, S. E., Liu Ambrose, T., Handy, T. C., Lim, H. J., et al. (2017). Effect of aerobic exercise on cancer-associated cognitive impairment: A proof-of-concept RCT. Psycho-Oncology, 27, 53–60. https://doi.org/10.1002/pon.4370
Campbell, Kristin L., Winters-stone, K. M., Wiskemann, J., May, A. M., Schwartz, A. L., Courneya, K. S., et al. (2019). Exercise guidelines for cancer survivors: Consensus statement from international multidisciplinary roundtable exercise guidelines for cancer survivors: Consensus statement from international multidisciplinary roundtable. Medicine and Science in Sports and Exercise, 51, 2375–2390. https://doi.org/10.1249/MSS.0000000000002116
Cella, D., Eton, D. T., Lai, J.-S., Peterman, A. H., & Merkel, D. E. (2002). Combining anchor and distribution-based methods to derive minimal clinically important differences on the Functional Assessment of Cancer Therapy (FACT) anemia and fatigue scales. Journal of Pain and Symptom Management, 24, 547–561.
Cella, D., Nichol, M. B., Eton, D., Nelson, J. B., & Mulani, P. (2009). Estimating clinically meaningful changes for the Functional Assessment of Cancer Therapy—Prostate: Results from a clinical trial of patients with metastatic hormone-refractory prostate cancer. Value in Health, 12, 124–129. https://doi.org/10.1111/J.1524-4733.2008.00409.X
Cella, D. F., Tulsky, D. S., Gray, G., Sarafian, B., Linn, E., Bonomi, A., et al. (1993). The functional assessment of cancer therapy scale: Development and validation of the general measure. Journal of Clinical Oncology, 11, 570–579.
Courneya, K. S., Friedenreich, C. M., Reid, R. D., Gelmon, K., Mackey, J. R., Ladha, A. B., et al. (2009). Predictors of follow-up exercise behavior 6 months after a randomized trial of exercise training during breast cancer chemotherapy. Breast Cancer Research and Treatment, 114, 179–187.
Courneya, K. S., McKenzie, D. C., Gelmon, K., Mackey, J. R., Reid, R. D., Yasui, Y., et al. (2014). A multicenter randomized trial of the effects of exercise dose and type on psychosocial distress in breast cancer patients undergoing chemotherapy. Cancer Epidemiology, Biomarkers and Prevention, 23, 857–864. https://doi.org/10.1158/1055-9965.EPI-13-1163
Courneya, K. S., Segal, R. J., Gelmon, K., Reid, R. D., Mackey, J. R., Friedenreich, C. M., et al. (2008). Predictors of supervised exercise adherence during breast cancer chemotherapy. Medicine and Science in Sports and Exercise, 40, 1180–1187.
Eldridge, S. M., Lancaster, G. A., Campbell, M. J., Thabane, L., Hopewell, S., Coleman, C. L., et al. (2016). Defining feasibility and pilot studies in preparation for randomised controlled trials: Development of a conceptual framework. PLoS ONE, 11, e0150205. https://doi.org/10.1371/journal.pone.0150205
Esper, P., Mo, F., Chodak, G., Sinner, M., Cella, D., & Pienta, K. J. (1997). Measuring quality of life in men with prostate cancer using the functional assessment of cancer therapy-prostate instrument. Urology, 50, 920–928. https://doi.org/10.1016/S0090-4295(97)00459-7
Fang, Y.-Y., Lee, Y.-H., Chan, J.-C., Chiou, P.-Y., Chou, X.-Y., Chiu, W.-T., et al. (2020). Effects of exercise interventions on social and cognitive functioning of men with prostate cancer: A meta-analysis. Supportive Care in Cancer, 28, 2043–2057. https://doi.org/10.1007/s00520-019-05278-y
Finlay, A., Wittert, G., & Short, C. E. (2018). A systematic review of physical activity-based behaviour change interventions reaching men with prostate cancer. Journal of Cancer Survivorship, 12, 571–591. https://doi.org/10.1007/s11764-018-0694-8
Freedson, P. S., Melanson, E., & Sirard, J. (1998). Calibration of the computer science and applications, Inc. accelerometer. Medicine and Science in Sports and Exercise, 30, 777–781.
Friedenreich, C. M., Stone, C. R., Cheung, W. Y., & Hayes, S. C. (2020). Physical activity and mortality in cancer survivors: A systematic review and meta-analysis. JNCI Cancer Spectrum. https://doi.org/10.1093/jncics/pkz080
Friedenreich, C. M., Wang, Q., Neilson, H. K., Kopciuk, K. A., McGregor, S. E., & Courneya, K. S. (2016). Physical activity and survival after prostate cancer. European Urology, 70, 576–585. https://doi.org/10.1016/j.eururo.2015.12.032
Goode, A. D., Lawler, S. P., Brakenridge, C. L., Reeves, M. M., & Eakin, E. G. (2015). Telephone, print, and web-based interventions for physical activity, diet, and weight control among cancer survivors: A systematic review. Journal of Cancer Survivorship, 9, 660–682. https://doi.org/10.1007/s11764-015-0442-2
Granger, C. L., Holland, A. E., Gordon, I. R., & Denehy, L. (2015). Minimal important difference of the 6-minute walk distance in lung cancer. Chronic Respiratory Disease, 12, 146–154. https://doi.org/10.1177/1479972315575715
Grimmett, C., Corbett, T., Brunet, J., Shepherd, J., Pinto, B. M., May, C. R., et al. (2019). Systematic review and meta-analysis of maintenance of physical activity behaviour change in cancer survivors. International Journal of Behavioral Nutrition and Physical Activity, 16, 37. https://doi.org/10.1186/s12966-019-0787-4
Groen, W. G., van Harten, W. H., & Vallance, J. K. (2018). Systematic review and meta-analysis of distance-based physical activity interventions for cancer survivors (2013–2018): We still haven’t found what we’re looking for. Cancer Treatment Reviews, 69, 188–203. https://doi.org/10.1016/J.CTRV.2018.07.012
Hallward, L., Patel, N., & Duncan, L. R. (2018). Behaviour change techniques in physical activity interventions for men with prostate cancer: A systematic review. Journal of Health Psychology, 25, 105–122. https://doi.org/10.1177/1359105318756501
Hartman, S. J., Nelson, S. H., Myers, E., Natarajan, L., Sears, D. D., Palmer, B. W., et al. (2017). Randomized controlled trial of increasing physical activity on objectively measured and self-reported cognitive functioning among breast cancer survivors: The memory & motion study. Cancer, 124, 192–202. https://doi.org/10.1002/cncr.30987
Holland, A. E., Hill, C. J., Rasekaba, T., Lee, A., Naughton, M. T., & McDonald, C. F. (2010). Updating the minimal important difference for six-minute walk distance in patients with chronic obstructive pulmonary disease. Archives of Physical Medicine and Rehabilitation, 91, 221–225. https://doi.org/10.1016/j.apmr.2009.10.017
Keogh, J., & MacLeod, R. (2012). Body composition, physical fitness, functional performance, quality of life, and fatigue benefits of exercise for prostate cancer patients: A systematic review. Journal of Pain and Symptom Management, 43, 96–110.
Kodama, S., Saito, K., Tanaka, S., Maki, M., Yachi, Y., Asumi, M., et al. (2009). Cardiorespiratory fitness as a quantitative predictor of all-cause mortality and cardiovascular events in healthy men and women: A meta-analysis. JAMA, 301, 2024–2035.
Lancaster, G. A., Dodd, S., & Williamson, P. R. (2004). Design and analysis of pilot studies: Recommendations for good practice. Journal of Evaluation in Clinical Practice, 10, 307–312. https://doi.org/10.1111/j.2002.384.doc.x
Leon, A. C., Davis, L. L., & Kraemer, H. C. (2011). The role and interpretation of pilot studies in clinical research. Journal of Psychiatric Research, 45, 626–629. https://doi.org/10.1016/j.jpsychires.2010.10.008
LoBiondo-Wood, G., Brown, C. G., Knobf, M. T., Lyon, D., Mallory, G., Mitchell, S. A., et al. (2014). Priorities for oncology nursing research: The 2013 national survey. Oncology Nursing Forum, 41, 67–76. https://doi.org/10.1188/14.ONF.67-76
McGowan, E. L., North, S., & Courneya, K. S. (2013). Randomized controlled trial of a behavior change intervention to increase physical activity and quality of life in prostate cancer survivors. Annals of Behavioral Medicine, 46, 382–393. https://doi.org/10.1007/s12160-013-9519-1
Menichetti, J., Villa, S., Magnani, T., Avuzzi, B., Bosetti, D., Marenghi, C., et al. (2016). Lifestyle interventions to improve the quality of life of men with prostate cancer: A systematic review of randomized controlled trials. Critical Reviews in Oncology/Hematology, 108, 13–22. https://doi.org/10.1016/J.CRITREVONC.2016.10.007
Mishra, S. I., Scherer, R. W., Geigle, P. M., Berlanstein, D. R., Topaloglu, O., Gotay, C. C., et al. (2012). Exercise interventions on health-related quality of life for cancer survivors (Review). The Cochrane Database of Systematic Reviews, 8, CD007566. https://doi.org/10.1002/14651858.CD007566.pub2
Myers, J. S., Erickson, K. I., Sereika, S. M., & Bender, C. M. (2017). Exercise as an intervention to mitigate decreased cognitive function from cancer and cancer treatment: An integrative review. Cancer Nursing, 41, 327–343. https://doi.org/10.1097/NCC.0000000000000549
Myers, J., Prakash, M., Froelicher, V., Do, D., Partington, S., & Edwin Atwood, J. (2002). Exercise capacity and mortality among men referred for exercise testing. New England Journal of Medicine, 346, 793–801. https://doi.org/10.1056/NEJMoa011858
Pollock, M. L., Foster, C., Schmidt, D., Hellman, C., Linnerud, A. C., & Ward, A. (1982). Comparative analysis of physiologic responses to three different maximal graded exercise test protocols in healthy women. American Heart Journal, 103, 363–373.
Rhodes, R. E. (2017). The evolving understanding of physical activity behavior: A multi-process action control approach. Advances in Motivation Science, 4, 171–205. https://doi.org/10.1016/BS.ADMS.2016.11.001
Rikli, R., & Jones, C. (1999). Development and validation of a functional fitness test for community-residing older adults. Journal of Aging and Physical Activity, 7, 129–161. https://doi.org/10.1123/japa.7.2.129
Rogers, L. Q., Courneya, K. S., Anton, P. M., Hopkins-Price, P., Verhulst, S., Vicari, S. K., et al. (2015). Effects of the BEAT cancer physical activity behavior change intervention on physical activity, aerobic fitness, and quality of life in breast cancer survivors: A multicenter randomized controlled trial. Breast Cancer Research and Treatment, 149, 109–119. https://doi.org/10.1007/s10549-014-3216-z
Ross, R., Blair, S. N., Arena, R., Church, T. S., Després, J. P., Franklin, B. A., et al. (2016). Importance of assessing cardiorespiratory fitness in clinical practice: A case for fitness as a clinical vital sign: A scientific statement from the American Heart Association. Circulation, 134, e653–e699.
Schmitz, K. H., Campbell, A. M., Stuiver, M. M., Pinto, B. M., Schwartz, A. L., Morris, G. S., et al. (2019). Exercise is medicine in oncology: Engaging clinicians to help patients move through cancer. CA: A Cancer Journal for Clinicians, 69, 468–484. https://doi.org/10.3322/CAAC.21579
Schmitz, K. H., Courneya, K. S., Matthews, C., Demark-Wahnefried, W., Galvão, D. A., Pinto, B. M., et al. (2010). American College of Sports Medicine roundtable on exercise guidelines for cancer survivors. Medicine and Science in Sports and Exercise, 42, 1409–1426. https://doi.org/10.1249/MSS.0b013e3181e0c112
Sheeran, P., Abraham, C., Jones, K., Villegas, M. E., Avishai, A., Symes, Y. R., et al. (2019). Promoting physical activity among cancer survivors: Meta-analysis and meta-CART analysis of randomized controlled trials. Health Psychology, 38, 467–482. https://doi.org/10.1037/hea0000712
Siegel, R. L., Miller, K. D., & Jemal, A. (2019). Cancer statistics, 2019. CA: A Cancer Journal for Clinicians, 69, 7–34. https://doi.org/10.3322/caac.21551
Vallance, J. K., Courneya, K. S., Plotnikoff, R. C., Yasui, Y., & Mackey, J. R. (2007). Randomized controlled trial of the effects of print materials and step pedometers on physical activity and quality of life in breast cancer survivors. Journal of Clinical Oncology, 25, 2352–2359. https://doi.org/10.1200/JCO.2006.07.9988
Vallerand, J. R., Rhodes, R. E., Walker, G. J., & Courneya, K. S. (2018). Feasibility and preliminary efficacy of an exercise telephone counseling intervention for hematologic cancer survivors: A phase II randomized controlled trial. Journal of Cancer Survivorship, 12, 357–370. https://doi.org/10.1007/s11764-018-0675-y
Wagner, L. I., Sweet, J., Butt, Z., Lai, J. S., & Cella, D. (2009). Measuring patient self-reported cognitive function: Development of the functional assessment of cancer therapy-cognitive function instrument. Journal of Supportive Oncology, 7, W32–W39.
Weintraub, S., Dikmen, S. S., Heaton, R. K., Tulsky, D. S., Zelazo, P. D., Bauer, P. J., et al. (2013). Cognition assessment using the NIH Toolbox. Neurology, 80, S54–S64. https://doi.org/10.1212/WNL.0b013e3182872ded
Acknowledgements
We thank the undergraduate research assistants at the University of Illinois for their assistance in conducting this study. We would also like to acknowledge Dr. Ryan E. Rhodes for his guidance with the use of the Multi-Process Action Control (M-PAC) framework.
Funding
This work was supported by a Campus Research Board Award [#RB16051] from the University of Illinois.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of interest
Linda Trinh, Arthur F. Kramer, Kendrith Rowland, Dominick A. Strom, Jaime N. Wong, and Edward McAuley have no conflicts of interest to declare.
Human and animal rights and Informed Consent
All procedures performed in studies involving human participants were in accordance with the ethical standards of the institutional research committee and with the 1964 Helsinki declaration and its later amendments or comparable ethical standards. The study was approved by the institutional review board and written informed consent was obtained from all participants.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Electronic supplementary material
Below is the link to the electronic supplementary material.
Rights and permissions
About this article
Cite this article
Trinh, L., Kramer, A.F., Rowland, K. et al. A pilot feasibility randomized controlled trial adding behavioral counseling to supervised physical activity in prostate cancer survivors: behavior change in prostate cancer survivors trial (BOOST). J Behav Med 44, 172–186 (2021). https://doi.org/10.1007/s10865-020-00185-8
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s10865-020-00185-8