Abstract
This study conducted among adults with obesity examined the associations between implicit attitudes toward physical activity and sedentary behavior, and physical activity behavior measured 4 months later. At baseline, 76 participants (M AGE = 56; M BMI = 39.1) completed a questionnaire assessing intentions toward physical activity and sedentary behavior and two computerized Single-Category Implicit Association Tests assessing implicit attitudes toward these two behaviors. At follow-up, physical activity was measured with accelerometers. Multiple regression analysis showed that implicit attitudes toward physical activity were positively and significantly associated with physical activity when participants’ age, BMI, past physical activity and intentions were controlled for. Implicit attitudes toward sedentary behavior were not associated with physical activity. Adults with obesity who implicitly reported more favorable attitudes toward physical activity at baseline were more likely to present higher physical activity levels at follow-up. Implicit attitudes could be targeted in future research to enhance physical activity.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Obesity rates are increasing (Finucane et al., 2011), and current forecasts indicate that the situation will worsen in the next decades (Finkelstein et al., 2012). In 2014, 39% of adults worldwide were overweight, 13% were obese, and recent estimations predict an increase of 33% in the prevalence of obesity for the next two decades (Finkelstein et al., 2012). Although the strategies vary, lifestyle interventions promoting change in physical activity are recognized as a key component of obesity management (Jensen et al., 2013). Nonetheless, results from randomized controlled trials evaluating the effectiveness of programs targeting behavior change have displayed inconsistent effects regarding physical activity change (Rhodes et al., 2017) and evidence for the sustainability of such behavioral change remains limited (Gourlan et al., 2011). Therefore, identifying the psychological determinants implicated in physical activity behavior is crucial for obesity management (Teixeira et al., 2015). Theoretically, health-related behaviors can be influenced by both explicit and implicit processes (Hofmann et al., 2008). Although the role of explicit processes has been widely studied in past research (McEachan et al., 2016), the contribution of implicit processes in physical activity over several months remains to be confirmed (Endrighi et al., 2016; Rebar et al., 2016).
Of the explicit motivational processes, the concept of intention has received considerable attention in past literature (Rhodes & Yao, 2015). Intention can be defined as the quantity of personal resources that an individual is prepared to invest in executing a particular behavior (Hall & Fong, 2007). This concept is present in several theories including the Theory of Planned Behavior (Ajzen, 1991) and more recent models such as the Temporal Self-regulation Theory (Hall & Fong, 2007). In the physical activity context, intentions were first described as strong predictors of physical activity, with correlations between intentions and physical activity estimated in two meta-analyses at r = .50 (Downs & Hausenblas, 2005; Hagger et al., 2002). However, a more recent review of experimental studies demonstrated that increases in physical activity intentions (d = .45) are accompanied by lower increases in physical activity behavior (d = .15; Rhodes & Dickau, 2012). It thus seems clear that focusing on explicit motivational processes alone is too restrictive to gain insight into the complex processes of change and maintenance of health behaviors (Sheeran et al., 2016). Implicit processes have not yet received as much research attention as explicit processes, but their investigation may hold the promise of enriching our current understanding of the complexities surrounding physical activity adoption (Rhodes, 2017).
According to the definition of Sheeran et al. (2013), implicit processes are cognitive, affective and motivational processes that may influence health behaviors without the person perceiving that influence. In the physical activity literature, the concept of implicit attitudes has arguably received more attention than the other implicit processes (Rebar et al., 2016). Implicit attitudes are automatic evaluations of an object as pleasant or unpleasant, which result in behavioral tendencies of approach to or avoidance of the object (e.g., physical activity), partly outside of awareness (Greenwald & Banaji, 1995). To date, studies have reported that implicit attitudes are significantly associated with physical activity behavior, whether self-reported (Bluemke et al., 2010; Calitri et al., 2009; Chevance et al., 2017; Chevance et al., 2016; Eves et al., 2007) or objectively measured (Conroy et al., 2010; Rebar et al., 2015). Despite these findings, however, only one cross-sectional study has highlighted a significant association between implicit attitudes and physical activity measured with questionnaires in obese adults (Chevance et al., 2016). Moreover, the role of implicit attitudes in physical activity objectively measured over several months remains to be confirmed (Endrighi et al., 2016; Rebar et al., 2016).
In addition to the distinction between explicit and implicit processes, one hypothesis of dual-process models (Hofmann et al., 2008) is that an individual’s difficulties in maintaining desired health-related behaviors can be explained by motives in favor of a competing behavior. For example, in the physical activity context, it could be hypothesized that motivation toward sedentary activities (e.g., TV viewing, reading, playing video games) impedes physical activity practice, independently of physical activity motivation. This hypothesis might be crucial for counseling persons with obesity about physical activity. Indeed, if motives for sedentary behavior have an impact on physical activity, counseling and weight management programs should specifically address sedentary behavior motivation (Rollo et al., 2016). Recent research indicates that obese individuals engage in more sedentary behavior than normal-weight individuals, and this behavioral pattern may limit physical activity (Baruth et al., 2013). Yet, to our knowledge, only two studies have investigated the association between sedentary motives and physical activity behavior. Regarding explicit processes, Rhodes and Blanchard (2008) found that TV viewing intentions were negatively associated with physical activity in students and adults when the authors controlled for physical activity-related explicit constructs (i.e., variables from the Theory of Planned Behavior). Regarding implicit processes, Cheval et al. (2015) reported that implicit processes toward sedentary behavior were negatively associated with physical activity in adults when they controlled for implicit processes and intentions toward physical activity. In conclusion, both implicit and explicit processes toward physical activity and sedentary behavior may have an independent contribution to physical activity adoption, and thus should be considered together in the understanding of this behavior.
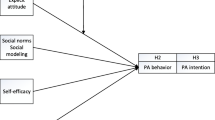
The present study
Based on the aforementioned research (Cheval et al., 2015; Hofmann et al., 2008; Rebar et al., 2016; Rhodes & Blanchard, 2008), the aim of the present study was to examine the specific contribution of implicit attitudes, toward both physical activity and sedentary behavior, in the prediction of physical activity in obese adults. This investigation was conducted over approximately 4 months to extend the previous results from the literature (Endrighi et al., 2016; Rebar et al., 2016). The contribution of implicit attitudes was tested after controlling for the variance explained by physical activity and sedentary behavior intentions, as well as physical activity covariates (i.e., past behavior, age, body mass index (BMI); Bauman et al., 2012; Hagger et al., 2002; Trost et al., 2002). It was expected that physical activity implicit attitudes would be positively—and sedentary behavior implicit attitudes would be negatively—associated with physical activity behavior, independently of intentions toward these two behaviors and physical activity covariates.
Methods
Study context and design
This prospective study took place during a weight management program, and was conducted between December 2015 and December 2016. The program comprised two separate periods. The first clinical stay lasted 2 weeks, during which participants had several meetings with physicians, psychologists, nutritionists, physiologists and kinesiologists. The objective of this first stay was to prompt multiple behavior change in participants (e.g., physical activity, eating behavior, tobacco) and prepare a longer inpatient program planned 4 months later. During this first stay, participants performed various daily exercises (e.g., treadmill, outdoor walking) in group, as well as in-group and individual education sessions about nutrition, physical activity and healthy lifestyle. None of the health care professionals involved were trained in behavior change theories and techniques. In the present study, motivational variables and covariates were measured at the end of the first inpatient program (Time 1). Physical activity behavior was measured with an accelerometer sent to participant’s domicile, 10 days before inclusion for the second inpatient program (Time 2). The mean time interval between Time 1 and Time 2 was 132 days (SD = 15 days).
Participants
Participants were included in this program with a prescription of a medical doctor and for the purpose of weight management. Then, individuals were eligible for study enrollment if they were between 18 and 75 years old, presented a BMI ≥ 30 kg/m2, and had healthcare coverage. They were not included in the study if they had a medical contraindication to exercise or were unable to respond to paper-based questionnaires or perform computerized tests. No financial incentives were provided to participate and no encouragement was given to maintain participation in the study. Procedures were in accordance with the principles of the Declaration of Helsinki of 1975, as revised in 2000, and approved by the local ethics committee.
One hundred individuals showed interest in participating in the study, signed a consent form and completed baseline measures (Time 1); among them, 76% (N = 76) provided an appropriate measure of physical activity in the follow-up period (Time 2). Due to the following reasons, valid accelerometer data were unavailable for twenty-four patients: insufficient accelerometer wear time (N = 8), unavailable by phone for sending the accelerometer (N = 5), hospitalizations reported during the follow-up phase (N = 4), technical problems with the accelerometers or inability to compute the physical activity score (N = 3), and post-delivery issues (N = 2). In addition, one participant declined to enroll and one died during follow-up (a study flowchart is provided in supplemental material). Given these reasons, data could not be considered as missing completely at random, and multiple imputations were not performed for these participants (Allison, 2000). The compliance rate is comparable to that observed in research using accelerometers in a similar context and time span (Endrighi et al., 2016). Demographic, motivational and clinical descriptive statistics for these 24 participants are displayed in supplemental data. Attrition analyses (i.e., Chi squared tests and independent sample t tests) compared these participants with those who provided physical activity data at Time 2. Only sedentary behavior intentions were significantly higher in patients who did not provide physical activity data at Time 2 (see supplemental data). The subsequent analyses included 76 participants.
Measures
Demographic and clinical characteristics
Demographic characteristics included self-reported age, sex, education, marital status, employment, and income. Clinical characteristics included self-report depressive symptoms (i.e., Hospital Anxiety and Depression Scale; Zigmond & Snaith, 1983). A score below 7 on a 0–21 scale indicated no depressive symptomatology. Cognitive impairment was measured with the Montreal Cognitive Assessment test (Nasreddine et al., 2005). A score above or equal to 26 on a 0–30 point scale was considered normal. BMI and the number of comorbidities were recorded during an interview with a physician. These variables were assessed at Time 1 (i.e., at the end of the first clinical stay).
Physical activity intentions
At Time 1, items measuring intentions were formulated following the recommendations of Ajzen (1991) as well as Rhodes and Horne (2013). Thus, the measure of intentions was slightly different from traditional items by taking into account contextual barriers and competing goals. This measure was preferred to typical measures of intentions due to the stronger correlations with physical activity demonstrated in previous research (Rhodes & Horne, 2013). Participants were first reminded of the definition of regular physical activity according to the French national plan for nutrition and health (i.e., doing at least 30 min per day of moderate to vigorous physical activity, 5 days per week). Following this definition, three items were proposed with a 7-point Likert scale ranging from (1) “do not agree at all” to (7) “totally agree.” Those items were: “I intend to practice a regular physical activity after my weight management program”; “Even if I am tired, alone, or sick, I have set the objective of practicing a regular physical activity after my weight management program”; “Even if I have other demands on my time, I will practice a regular physical activity after my weight management program.” These three items were summed (i.e., Cronbach’s alpha = .86), leading to a score comprised between 3 (weak intentions to practice a regular physical activity) and 21 (strong intentions to practice a regular physical activity).
Sedentary behavior intentions
At Time 1, sedentary behavior intentions were measured following the same procedure (Rhodes & Horne, 2013). The questionnaire started with a definition of sedentary activities (i.e., time spent by a person sitting or lying down in waking hours, Sedentary Behavior Research Network, 2012). In line with recent research (Maher & Conroy, 2016), three items were formulated regarding the limitation of sedentary behavior: “I intend to limit my sedentary behaviors after my weight management program”; “Even if I am tired, alone, or sick, I have set the objective of limiting my sedentary behaviors after my weight management program”; “Even if I have other demands on my time, I will limit my sedentary behavior after my weight management program.” These three items were summed (i.e., Cronbach’s alpha = .88), leading to a score comprised between 3 (weak intentions to limit one’s sedentary behaviors) and 21 (strong intentions to limit one’s sedentary behavior).
Physical activity implicit attitudes
At Time 1, physical activity implicit attitudes were measured with the computerized Single-Category Implicit Association Test (SC-IAT), following the recommendations of Karpinski and Steinman (2006) and in line with previous research on physical activity (Conroy et al., 2010; Hyde et al., 2012; Rebar et al., 2015). This test evaluates the strength of automatic associations that one holds in memory between two attributes (e.g., positive and negative) and one conceptual target (e.g., physical activity).
During the SC-IAT, participants are required to sort stimuli (i.e., words) representing three categories with only two response keys, each assigned to two of the three categories (e.g., positive + physical activity vs. negative; positive vs. negative + physical activity). If two categories are highly associated cognitively, the sorting task is expected to be easier when they share the same response key than when they do not. Hence, ease of sorting can be estimated by the speed of responding (Richetin et al., 2015). Stimuli for the categories “positive” and “negative” were: pleasant/unpleasant; happy/sad; favorable/unfavorable; beneficial/harmful. Stimuli selected to represent the conceptual category “physical activity” were: running, walking, hiking, dancing, stairs, swimming, bike, lift, gardening, effort (see supplemental material for a more precise description of the task).
The score of the SC-IAT was computed according to the most recent recommendations, using the DW-Score (Richetin et al., 2015). This score was calculated as follows: (1) for each participant, the 10% fastest and slowest latencies were replaced by the last untrimmed latencies, for both error and correct responses; (2) the difference between the average latencies of the two critical blocks (i.e., practice and test blocks together) were divided by the pooled SD of all the latencies; and (3) the score was computed based on practice and critical trials together. Scores were comprised between −2 and +2, with 0 representing a neutral score and positive scores revealing favorable implicit attitudes toward physical activity. The statistical software R (R Core Team, 2013) was used to compute the scores, using the IAT.Score package provided by Richetin et al. (2015).
Sedentary behavior implicit attitudes
At Time 1, sedentary behavior implicit attitudes were also measured using an SC-IAT, following the same procedure and scoring algorithm as for the physical activity SC-IAT (i.e., except that the category “physical activity” was replaced by “sedentary behavior”). Stimuli selected to represent the conceptual category “sedentary behavior” were: sitting, armchair, chair, television, reading, computer, couch, lying, desk, read. A higher score indicated more favorable implicit attitudes toward sedentary behavior.
Physical activity covariates
Hagger et al. (2002) demonstrated that when past behavior was controlled for, the strength of the path between motivation and physical activity behavior was reduced. Thus, the authors suggested that studies that do not assess past behavior might obtain artificially high correlations between motivational constructs and behavior (Hagger et al., 2002). In the present study, past physical activity was measured with one item, following the definition of regular physical activity (i.e., doing at least 30 min per day of moderate to vigorous physical activity, 5 days per week): “Before your weight management program, how many times per week were you physically active for at least 30 min, during an ordinary week?”
Regarding demographic and clinical covariates, an exploratory analysis (i.e., stepwise regression) was conducted to determine the best set of variables in the present sample. In line with studies reviewing demographic and clinical correlates of physical activity in adults (Bauman et al., 2012; Trost et al., 2002), physical activity measured at Time 2 was thus first regressed on age, gender, BMI, education level, number of comorbidities, depressive symptoms, cognitive capacities and past physical activity. Variables that displayed significant associations with physical activity were selected as covariates for subsequent analysis in this study (see the data analysis and results sections).
Physical activity behavior
At follow-up, participants were asked to wear ActiGraph GT3X+ (ActiGraph, Pensacola, FL) accelerometers on their non-dominant wrist 24 h per day for an entire week. The ActiGraph GT3X+ captured triaxial accelerations at 30 Hz. Accelerometer data in raw format were processed with R using the GGIR package (van Hees et al., 2013, 2014) and the default parameters of the function g.shell.GGIR. This recent method is increasingly used in human movement sciences (Sabia et al., 2015) and has demonstrated its validity in the obese population in comparison with other objective methods measuring physical activity (Ellis et al., 2016). Participants included in the analyses displayed at least 10 h per day, including at least 1 weekend day (Mean = 1.9, SD = .27) and 2 week days (Mean = 4.6, SD = 1). Then, for each participant, the duration of moderate-to-vigorous physical activity (MVPA) was calculated. To qualify as MVPA, ≥80% of the activity needed to be ≥100 milligravity units, for at least a period (bout) of 1 min, using moving 10-min windows. Valid days were averaged to represent one unique day according to current recommendations [Sabia et al., 2015; i.e., ((5 × mean valid weekday acceleration) + (2 × mean valid weekend days acceleration))/7]. MVPA was reported in mean minutes per day.
Procedure
At Time 1 (i.e., at the end of the first inpatient program), after they signed the consent form, participants met an experimenter for a face-to-face meeting of approximately one hour. They were first asked to complete the two SC-IATs in a 1:1 randomized ratio to control for potential order effect. They then completed questionnaires measuring demographic variables, intentions, the HADS, and the MoCA. At Time 2 (i.e., 2 weeks before the second inpatient program), participants were called by phone. If they accepted to wear an accelerometer during a week, accelerometers were sent by regular mail to their address. Participants were asked to bring the accelerometer back to the clinic for their second inpatient program.
Data analysis
An exploratory stepwise regression analysis was first conducted to select the best set of demographic and clinical physical activity covariates. Then, a three-step hierarchical multiple regression analysis was conducted to identify the independent contribution of physical activity covariates (step 1), intentions (step 2) and implicit attitudes (step 3) on physical activity at follow-up.
Before running the analyses, outliers were checked and all the independent variables were standardized or dummy coded (Tabachnick & Fidell, 2007). Given that physical activity was positively skewed, we performed a logarithmic transformation of this variable (Tabachnick & Fidell, 2007). Regarding the statistical assumptions associated with multiple regression analyses, standardized residuals as well as variance inflation factors were examined, revealing no major signs of nonlinearity, heteroscedasticity or multicollinearity. Post-hoc power analyses were conducted according to current recommendations (Cohen et al., 2003; Soper, 2017). Effect sizes were interpreted using adjusted R 2, and standardized β (Ferguson, 2008). Analyses were performed with JASP (2016) statistical software (version .08).
Results
Descriptive data
The mean age of participants was 56 years old (SD = 11.9), 65% were female (see Table 1). Regarding clinical characteristics, mean BMI was 39.1 kg/m2 (SD = 6.6), and on average participants did not report depressive symptoms, but the sample was characterized by light cognitive impairment (i.e., mean score under the MoCA’s cut-off of 26; M = 24.3, SD = 3). Participants reported a mean number of two comorbidities; arterial hypertension, type 2 diabetes and sleep apnea syndrome were the most frequently reported. Regarding behavioral and motivational data, participants reported being active 3.5 (SD = 2.5) times per week at Time 1. Mean physical activity and sedentary behaviors intentions were high [17.5 (SD = 3.2), and 15.7 (SD = 4) respectively], indicating strong intentions to be physically active and to limit sedentary behaviors after the program. Mean physical activity implicit attitudes was .40 (SD = .34), indicating implicit attitudes moderately in favor of physical activity, and mean sedentary behavior implicit attitudes was .14 (SD = .37), indicating implicit attitudes slightly in favor of sedentary behavior. At Time 2, participants were active on average 17 min per day (SD = 15.69). Means, standard deviation and correlations between variables are displayed in Table 2.
Explanatory analyses for covariate selection
Physical activity measured at Time 2 was regressed on age, gender, BMI, education level, depressive symptoms, number of comorbidities, cognitive capacities and past physical activity. In the stepwise regression, step 1 identified age as the most robust predictor of Time 2 physical activity, accounting for 19% of the variance (β = −.45, p < .001). In a second step, BMI emerged as a significant predictor, accounting for an additional variance of 19% (β = −.45, p < .001). In a third step, self-report past physical activity emerged as a significant predictor, accounting for an additional variance of 4% (β = .22, p = .021). Thus, study participants with younger age, lower BMI and higher levels of past physical activity were more likely to display a higher level of objective physical activity 4 months later. Education level, number of comorbidities, depressive symptoms and cognitive capacities were not significantly associated with prospective physical activity in this study (see Table 3). Age, BMI and past physical activity were entered as covariates in subsequent analyses.
Prediction of physical activity behavior
A three-step hierarchical multiple regression was conducted to identify the independent contribution of physical activity covariates (step 1), intentions toward physical activity and sedentary behaviors (step 2) and implicit attitudes (step 3) assessed at Time 1 on physical activity behavior measured 4 months later (see Table 4). In the first step, age (β = −.45, p < .001), BMI (β = −.43, p = .001), and past behavior (β = .22, p = .019) were significantly associated with physical activity. The equation was significant, F (3, 73) = 18.05, p < .001, adjusted R 2 = .405. In the second step, intentions toward physical activity and sedentary behavior were entered in the regression model. These two variables were not significantly associated with physical activity and did not add a significant increase in explained variance (β = −.05, p = .652 for intentions toward physical activity, and β = .14, p = .169 for intentions toward sedentary behavior, ΔR 2 = .015, p = .383). The equation was significant, F (5, 71) = 18.05, p < .001, adjusted R 2 = .405. In the third step, implicit attitudes toward physical activity and sedentary behavior were entered in the model. Physical activity implicit attitudes accounted for a significant portion of physical activity (β = .21, p = .04), and a statistical tendency was observed regarding sedentary behavior implicit attitudes (β = −.18, p = .06). The equation was significant, F (7, 68) = 8.99, p < .001, adjusted R 2 = .434, however the percentage of variance explained in the third step did not significantly increase: ΔR 2 = .043, p = .067. Post-hoc statistical power analysis indicated a risk of type I error (1-β = .40) regarding the integration of implicit attitudes in the model (step 3).Footnote 1
Discussion
Grounded in a dual-processes approach (Hofmann et al., 2008), this study aimed to explore the role of physical activity and sedentary behavior implicit attitudes in the prediction of prospective physical activity in obese adults. The results highlight that participants who held more favorable implicit attitudes towards physical activity exhibited higher objective level of physical activity 4 months later. This result is important because identifying the determinants of physical activity over time represents a crucial step in designing better theory-based physical activity programs in the future (Teixeira et al., 2015). Nonetheless, these results should be interpreted with caution given the weak additional contribution of implicit attitudes after controlling for participants’ age, BMI, and past physical activity, as well as type I error risk for the integration of implicit attitudes in the regression model.
Dual-processes approach to physical activity
A previous cross-sectional study, conducted among adults with obesity, found that implicit attitudes were significantly associated with self-reported physical activity when intentions and other related explicit constructs were controlled for (i.e., variables from the Theory of Planned Behavior; Chevance et al., 2016). The present study confirms and extends this result over a longer interval and with an objective measure of physical activity. Theoretically, these consistent associations between implicit attitudes and physical activity among adults with obesity could be explained by individual dispositions (Friese et al., 2008). Indeed, it is assumed that implicit processes are strongly associated with behavior in individuals who have difficulty in engaging in controlled processing compared with individuals with greater resources (Cheval et al., 2016; Friese et al., 2008). In the field of obesity, studies have found reciprocal relationships between weight gain over time and an increase in impulsivity (Sutin et al., 2011, 2013). Hence, it could be hypothesized that implicit processes are important behavioral predictors among adults with obesity because, on average, these individuals are more impulsive. Nonetheless, any interpretation should be tempered because in the current study sedentary behavior implicit attitudes did not reach statistical significance, which does not confirm previous research (Cheval et al., 2015). Other studies are thus needed to investigate the role of sedentary behavior-related implicit cognitions in physical activity adoption. It would also be particularly interesting in future research to examine the associations between sedentary behavior implicit attitudes and other dependent variables, such as light physical activity or the time spent sitting, which represent relevant lifestyle markers in adults with obesity.
Regarding the lack of associations between behavioral intentions and physical activity, both methodological and contextual explanations can be advanced. For example, although implicit attitudes were measured through computerized reaction-time tasks in this study, intentions were self-reported and thus more likely to be contaminated by social desirability bias (Greenwald et al., 2009). Indeed, during a weight management program, social desirability toward exercise and sedentary behavior may be particularly salient, thereby influencing responses to self-report questionnaires (Adams et al., 2005). This issue would explain the lack of sensitivity in the measure of intentions, which in turn would explain the lack of association between this variable and physical activity. Consequently, the utilization of indirect measures of motivation (e.g., SC-IAT) could be useful for researchers and clinicians to complete self-reported assessments of motivation. Regarding the overall high level of intentions displayed in this study at baseline, it could also be hypothesized that the participants might have benefited from the program and developed strong intentions during the intervention, but failed to maintain them after the program (Rhodes & Dickau, 2013). Finally, it should be noted that in the present study intentions toward sedentary behavior were the unique motivational variable significantly correlated with Time 2 physical activity. However, this variable was also correlated with BMI (r = −.27, p = .019, see Table 2). This shared variance might explain the non-significant association found in the regression model between intentions toward sedentary behavior and Time 2 physical activity when BMI was controlled for.
In summary, physical activity implicit attitudes were the only motivational variable prospectively associated with objective physical activity in this study after controlling for age, BMI and self-report past physical activity. This variable might thus be targeted in future research aiming to enhance physical activity. Currently, experimental studies examining a change in implicit attitudes are scarce in the literature. An observational study found that implicit attitudes can change over one week, and that change might impact physical activity behavior (Hyde et al., 2012); moreover, previous studies found that implicit attitudes could be enhanced throughout a week (Berry, 2016) or along a 5-week rehabilitation program (Chevance et al., 2017). Given the aforementioned results and those obtained in the present study, targeting implicit attitudes in an intervention offers novel interventional perspectives for improving the promotion of physical activity among obese individuals.
Targeting implicit processes to enhance physical activity
Recently, two general frameworks were developed to guide the experimental manipulation of implicit processes (Hollands et al., 2016; Papies, 2016). These frameworks are based on the premises that “discrete” interventions that do not require participants to think about them can be designed (i.e., in contrast to interventions focusing on change in explicit processes; see Hollands et al., 2016). Papies (2016) pointed out that these interventions could change the features of the environment to influence the activation of implicit processes (i.e., cueing interventions) and/or directly change the implicit processes that drive behaviors (i.e., training interventions). To date, a handful of studies have started exploring training interventions in the physical activity context. Retraining approach-avoidance tendencies (Cheval et al., 2016), evaluative conditioning (Antoniewicz & Brand, 2016), delivering tailored exercise-related messages (Berry, 2016), and mental imagery (Markland et al., 2015) have all shown promise in modifying implicit processes. However, these studies have been conducted with students in a laboratory context, and the next step would be to examine their relevance in more ecological and clinical settings (e.g., among adults with obesity).
Strengths, limits and perspectives
The strengths of this research reside in the study of both explicit and implicit motivational constructs toward physical activity and sedentary behaviors, its prospective design, and the assessment of physical activity with accelerometers. For these reasons, this study makes an important contribution toward understanding the role of implicit attitudes in the physical activity context. However, the results were obtained in a highly specific weight management program, and other associations could be expected with different contexts and time intervals (see Endrighi et al., 2016). For example, it is possible that this study sample was particularly motivated, given their participation in a weight management program, and in comparison with other adults with obesity from the general population. Moreover, participants from this study were characterized by light cognitive impairment according to the MoCA’s cut-off, which could be explained by the fact that obesity is negatively associated with cognitive functions (Miller & Spencer, 2014). In past literature, it has been shown that lower cognitive capacities (i.e., executive functions) could weaken the positive association between intentions and physical activity (Hall et al., 2008). Thus, it is possible that participants’ mean cognitive impairment has impacted the relationships observed in this study between motivational factors and physical activity behavior. For generalization purpose, it is necessary to replicate the results of this study in other samples.
Second, physical activity implicit attitudes were a significant predictor of physical activity independently of intentions, but intentions were not prospectively associated with behavior. Hence, it would be challenging in future research to examine the contribution of implicit attitudes while controlling for other motivational constructs (for a recent discussion on the additional contribution of implicit processes over explicit processes, see Blanton et al., 2016). A recent review noted that autonomous motivation, barrier self-efficacy and the use of self-regulation skills were consistent predictors of physical activity maintenance in obese adults (Teixeira et al., 2015). Demonstrating the additional contribution of implicit attitudes beyond the effects of these variables would further support their role in the adoption of regular physical activity in this population. Moreover, other physical activity covariates could be controlled for in future research, such as physical limitations or disabilities, or baseline physical activity measured with accelerometers.
Finally, some bivariate correlations (see Table 2) obtained in this study between the motivational variables should be discussed. At the explicit level, intentions toward physical activity were positively correlated with intentions toward sedentary behavior, indicating that the more people intended to adopt a regular physical activity, the more they intended to limit their sedentary behavior. However, at the implicit level, attitudes toward physical activity were also positively correlated with attitudes toward sedentary behavior, indicating that participants with more favorable implicit attitudes toward physical activity also displayed more favorable implicit attitudes toward sedentary behavior. This result differs from one previous study investigating implicit processes toward these two behaviors and highlighting that implicit processes toward physical activity and sedentary behavior were negatively correlated (Cheval et al., 2015). Other studies are thus needed to further explore the complex relationships between implicit and explicit processes toward physical activity and sedentary behavior.
In conclusion, physical activity implicit attitudes were the only motivational variable prospectively associated with physical activity in this study. This result was obtained while controlling for participant’s age, BMI, past physical activity, and intentions toward physical activity and sedentary behavior. Given that implicit attitudes can be modified through structured interventions, it would be interesting to target this construct in future experimental research. Such an initiative might enhance future physical activity promotion and weight management programs.
Notes
Additional regression models are provided in supplemental data. In accordance with dual-process assumptions (Perugini, 2005), we examined potential interactions between explicit and implicit motivational processes. No interaction was significant. We also examined the associations between the four motivational variables and Time 2 physical activity without controlling for age, BMI and past physical activity. The model was significant F (4, 74) = 3.07, p = .022, adjusted R 2 = .10; implicit attitudes toward physical activity and sedentary behavior were significantly associated with Time 2 physical activity (β = .23, p = .05, β = −.26, p = .04, respectively), as well as intentions toward sedentary behavior (β = .24, p = .05). Intentions toward physical activity were not significantly associated with physical activity (β = −.03, p = .78).
References
Adams, S. A., Matthews, C. E., Ebbeling, C. B., Moore, C. G., Cunningham, J. E., Fulton, J., et al. (2005). The effect of social desirability and social approval on self-reports of physical activity. American Journal of Epidemiology, 161, 389–398.
Ajzen, I. (1991). The theory of planned behavior. Organizational Behavior and Human Decision Processes, 50, 179–211.
Allison, P. D. (2000). Multiple imputation for missing data: A cautionary tale. Sociological Methods and Research, 28, 301–309.
Antoniewicz, F., & Brand, R. (2016). Learning to like exercising: Evaluative conditioning changes automatic evaluations of exercising and influences subsequent exercising behavior. Journal of Sport & Exercise Psychology, 38, 138–148.
Baruth, M., Sharpe, P. A., Hutto, B., Wilcox, S., & Warren, T. Y. (2013). Patterns of sedentary behavior in overweight and obese women. Ethnicity and Disease, 23, 336–342.
Bauman, A. E., Reis, R. S., Sallis, J. F., Wells, J. C., Loos, R. J., & Martin, B. W. (2012). Correlates of physical activity: Why are some people physically active and others not? The Lancet, 380, 258–271.
Berry, T. R. (2016). Changes in implicit and explicit exercise-related attitudes after reading targeted exercise-related information. Psychology of Sport and Exercise, 22, 273–278.
Blanton, H., Burrows, C. N., & Jaccard, J. (2016). To accurately estimate implicit influences on health behavior, accurately estimate explicit influences. Health Psychology, 35, 856–860.
Bluemke, M., Brand, R., Schweizer, G., & Kahlert, D. (2010). Exercise might be good for me, but I don’t feel good about it: Do automatic associations predict exercise behavior? Journal of Sport & Exercise Psychology, 32, 137–153.
Calitri, R., Lowe, R., Eves, F. F., & Bennett, P. (2009). Associations between visual attention, implicit and explicit attitude and behavior for physical activity. Psychology & Health, 24, 1105–1123.
Cheval, B., Sarrazin, P., Isoard-Gautheur, S., Radel, R., & Friese, M. (2015). Reflective and impulsive processes explain (in)effectiveness of messages promoting physical activity: A randomized controlled trial. Health Psychology, 34, 10–19.
Cheval, B., Sarrazin, P., Isoard-Gautheur, S., Radel, R., & Friese, M. (2016). How impulsivity shapes the interplay of impulsive and reflective processes involved in objective physical activity. Personality and Individual Differences, 96, 132–137.
Chevance, G., Caudroit, J., Romain, A., & Boiché, J. (2016). The adoption of physical activity and eating behaviors among persons with obesity and in the general population: The role of implicit attitudes within the theory of planned behavior. Psychology, Health & Medicine, 22, 319–324.
Chevance, G., Héraud, N., Varray, A., & Boiché, J. (2017). Change in explicit and implicit motivation toward physical activity and sedentary behavior in pulmonary rehabilitation and associations with post-rehabilitation. Rehabilitation Psychology, 62, 119–129.
Cohen, J., Cohen, P., West, S. G., & Aiken, L. S. (2003). Applied multiple regression/correlation analysis for the behavioral sciences (3rd ed.). Mahwah, NJ: Lawrence Earlbaum Associates.
Conroy, D. E., Hyde, A. L., Doerksen, S. E., & Ribeiro, N. F. (2010). Implicit attitudes and explicit motivation prospectively predict physical activity. Annals of Behavioral Medicine, 39, 112–118.
Downs, D., & Hausenblas, H. (2005). Elicitation studies and the theory of planned behavior: A systematic review of exercise beliefs. Psychology of Sport and Exercise, 6, 1–31.
Ellis, K., Kerr, J., Godbole, S., Staudenmayer, J., & Lanckriet, G. (2016). Hip and wrist accelerometer algorithms for free-living behavior classification. Medicine and Science in Sports and Exercise, 48, 933–940.
Endrighi, R., Basen-Engquist, K., Szeto, E., Perkins, H., Baum, G., Cox-Martin, M., et al. (2016). Self-reported and automatic cognitions are associated with exercise behavior in cancer survivors. Health Psychology, 35, 824–828.
Eves, F. F., Scott, E. J., Hoppé, R., & French, D. P. (2007). Using the affective priming paradigm to explore the attitudes underlying walking behaviour. British Journal of Health Psychology, 12, 571–585.
Ferguson, C. J. (2008). An effect size primer: A guide for clinicians and researchers. Professional Psychology: Research and Practice, 40, 532–538.
Finkelstein, E., Khavjou, O., Thompson, H., Trogdon, J., Pan, L., Sherry, B., et al. (2012). Obesity and severe obesity forecasts through 2030. American Journal of Preventive Medicine, 42, 563–570.
Finucane, M., Stevens, G., Cowan, M., Danaei, G., Lin, J., Paciorek, C., et al. (2011). National, regional, and global trends in body-mass index since 1980: Systematic analysis of health examination surveys and epidemiological studies with 960 country-years and 9·1 million participants. The Lancet, 377, 557–567.
Friese, M., Hofmann, W., & Schmitt, M. (2008). When and why do implicit measures predict behavior? Empirical evidence for the moderating role of opportunity, motivation, and process reliance. European Review of Social Psychology, 19, 285–338.
Gourlan, M., Trouilloud, D., & Sarrazin, P. (2011). Interventions promoting physical activity among obese populations: A meta-analysis considering global effect, long-term maintenance, physical activity indicators and dose characteristics. Obesity Reviews, 12, 633–645.
Greenwald, A. G., & Banaji, M. R. (1995). Implicit social cognition: Attitudes, self-esteem, and stereotypes. Psychological Review, 102, 4–27. doi:10.1037//0033-295x.102.1.4
Greenwald, A. G., Poehlman, T. A., Uhlmann, E., & Banaji, M. R. (2009). Understanding and using the Implicit Association Test: III. Meta-analysis of predictive validity. Journal of Personality and Social Psychology, 97, 17–41.
Hagger, M., Chatzisarantis, N., & Biddle, S. (2002). The influence of autonomous and controlling motives on physical activity intentions within the Theory of Planned Behaviour. British Journal of Health Psychology, 7, 283–297.
Hall, P., & Fong, G. (2007). Temporal self-regulation theory: A model for individual health behavior. Health Psychology Review, 1, 6–52.
Hall, P., Fong, G. T., Epp, L. J., & Elias, L. J. (2008). Executive function moderates the intention-behavior link for physical activity and dietary behavior. Psychology & Health, 23, 309–326.
Hofmann, W., Friese, M., & Wiers, R. (2008). Impulsive versus reflective influences on health behavior: A theoretical framework and empirical review. Health Psychology Review, 2, 111–137.
Hollands, G. J., Marteau, T. M., & Fletcher, P. C. (2016). Nonconscious processes in changing health-related behaviour: A conceptual analysis and framework. Health Psychology Review, 10, 1–28.
Hyde, A. L., Elavsky, S., Doerksen, S. E., & Conroy, D. E. (2012). The stability of automatic evaluations of physical activity and their relations with physical activity. Journal of Sport & Exercise Psychology, 34, 715–736. doi:10.1123/jsep.34.6.715
JASP Team. (2016). JASP [Computer software]. Retrieved from, https://jasp-stats.org/download/
Jensen, M., Ryan, D., Apovian, C., Ard, J., Comuzzie, A., Donato, K., et al. (2013). Guideline for the management of overweight and obesity in adults. Circulation, 129, 102–138.
Karpinski, A., & Steinman, R. B. (2006). The single category implicit association test as a measure of implicit social cognition. Journal of Personality and Social Psychology, 91, 16–32.
Maher, J. P., & Conroy, D. E. (2016). A dual-process model of older adults’ sedentary behavior. Health Psychology, 35, 262–272.
Markland, D., Hall, C. R., Duncan, L. R., & Simatovic, J. (2015). The effects of an imagery intervention on implicit and explicit exercise attitudes. Psychology of Sport and Exercise, 17, 24–31.
McEachan, R., Taylor, N., Harrison, R., Lawton, R., Gardner, P., & Conner, M. (2016). Meta-analysis of the reasoned action approach (RAA) to understanding health behaviors. Annals of Behavioral Medicine, 50, 592–612.
Miller, A. A., & Spencer, S. J. (2014). Obesity and neuroinflammation: A pathway to cognitive impairment. Brain, Behavior, and Immunity, 42, 10–21.
Nasreddine, Z. S., Phillips, N. A., Bédirian, V., Charbonneau, S., Whitehead, V., Collin, I., et al. (2005). The montreal cognitive assessment, MoCA: A brief screening tool for mild cognitive impairment. Journal of the American Geriatrics Society, 53, 695–699.
Papies, E. K. (2016). Health goal priming as a situated intervention tool: How to benefit from nonconscious motivational routes to health behaviour. Health Psychology Review, 10, 408–424.
Perugini, M. (2005). Predictive models of implicit and explicit attitudes. British Journal of Social Psychology, 44, 29–45.
R Core Team (2013). R: A language and environment for statistical computing. Vienna, Austria: R Foundation for Statistical Computing. http://www.R-project.org/
Rebar, A., Dimmock, J., Jackson, B., Rhodes, R., Kates, A., Starling, J., et al. (2016). A systematic review of the effects of non-conscious regulatory processes in physical activity. Health Psychology Review, 10, 395–407.
Rebar, A. L., Ram, N., & Conroy, D. E. (2015). Using the EZ-diffusion model to score a single-category implicit association test of physical activity. Psychology of Sport and Exercise, 16, 96–105.
Rhodes, R. E. (2017). The evolving understanding of physical activity behavior: A multi-process action control approach. Advances in Motivation Science, 4, 171–205. doi:10.1016/bs.adms.2016.11.001
Rhodes, R. E., & Blanchard, C. M. (2008). Do sedentary motives adversely affect physical activity? Adding cross-behavioural cognitions to the theory of planned behaviour. Psychology & Health, 23, 789–805.
Rhodes, R. E., & Dickau, L. (2012). Experimental evidence for the intention–behavior relationship in the physical activity domain: A meta-analysis. Health Psychology, 31, 724–727.
Rhodes, R. E., & Horne, L. (2013). Deepening the measurement of motivation in the physical activity domain: Introducing behavioural resolve. Psychology of Sport and Exercise, 14, 455–460.
Rhodes, R. E., Janssen, I., Bredin, S. S. D., Warburton, D. E. R., & Bauman, A. (2017). Physical activity: Health impact, prevalence, correlates and interventions. Psychology & Health. doi:10.1080/08870446.2017.1325486
Rhodes, R. E., & Yao, C. (2015). Models accounting for intention-behavior discordance in the physical activity domain: A user’s guide, content overview, and review of current evidence. International Journal of Behavioral Nutrition and Physical Activity, 12, 9.
Richetin, J., Costantini, G., Perugini, M., & Schönbrodt, F. (2015). Should we stop looking for a better scoring algorithm for handling implicit association test data? Test of the role of errors, extreme latencies treatment, scoring formula, and practice trials on reliability and validity. PLoS ONE, 10, 0129601.
Rollo, S., Gaston, A., & Prapavessis, H. (2016). Cognitive and motivational factors associated with sedentary behavior: A systematic review. AIMS Public Health, 3, 956–984.
Sabia, S., Cogranne, P., van Hees, V. T., Bell, J. A., Elbaz, A., Kivimaki, M., et al. (2015). Physical activity and adiposity markers at older ages: Accelerometer vs questionnaire data. Journal of the American Medical Directors Association, 16, 7–13.
Sedentary Behaviour Research Networ. (2012). Letter to the editor: Standardized use of the terms “sedentary” and “sedentary behaviours”. Applied Physiology, Nutrition and Metabolism, 37, 540–542.
Sheeran, P., Bosch, J., Crombez, G., Hall, P., Harris, J., Papies, E., et al. (2016). Implicit processes in health psychology: Diversity and promise. Health Psychology, 35, 761–766.
Sheeran, P., Gollwitzer, P., & Bargh, J. (2013). Nonconscious processes and health. Health Psychology, 32, 460–473.
Soper, D. S. (2017). Effect size calculator for multiple regression [software]. Available from, http://www.danielsoper.com/statcalc
Sutin, A. R., Costa, P. T., Chan, W., Milaneschi, Y., Eaton, W. W., Zonderman, A. B., et al. (2013). I know not to, but i can’t help it: Weight gain and changes in impulsivity-related personality traits. Psychological Science, 24, 1323–1328.
Sutin, A. R., Ferrucci, L., Zonderman, A. B., & Terracciano, A. (2011). Personality and obesity across the adult life span. Journal of Personality and Social Psychology, 101, 579–592.
Tabachnick, B. G., & Fidell, S. L. (2007). Using multivariate statistics (5th ed.). Boston: Allyn and Bacon.
Teixeira, P., Carraça, E., Marques, M., Rutter, H., Oppert, J., De Bourdeaudhuij, I., et al. (2015). Successful behavior change in obesity interventions in adults: A systematic review of self-regulation mediators. BMC Medicine, 13, 13–84.
Trost, S. G., Owen, N., Bauman, A. E., Salles, J. F., & Brown, W. (2002). Correlates of adults’ participation in physical activity: Review and update. Medicine and Science in Sports and Exercise, 34, 1996–2001. doi:10.1097/00005768-200212000-00020
van Hees, V. T., Fang, Z., Langford, J., Assah, F., Mohammad, A., Da Silva, I. C., et al. (2014). Autocalibration of accelerometer data for free-living physical activity assessment using local gravity and temperature: An evaluation on four continents. Journal of Applied Physiology, 117, 738–744.
van Hees, V. T., Gorzelniak, L., León, E. C., Eder, M., Pias, M., Taherian, S., et al. (2013). Separating movement and gravity components in an acceleration signal and implications for the assessment of human daily physical activity. PLoS ONE. doi:10.1371/journal.pone.0061691
Zigmond, A. S., & Snaith, R. P. (1983). The hospital anxiety and depression scale. Acta Psychiatrica Scandinavica, 67, 361–370.
Acknowledgements
Guillaume Chevance is funded by a grant from the French Agency for Research and Technology (ANRT). This study has received financial support from the fundation APARD and the region Occitanie. The authors wish to thank Marie-Ange Dubois for her help in the follow-up phase, as well as La Poste for their support all along the study.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of interest
Guillaume Chevance, Johan Caudroit, Thomas Henry, Philippe Guerin, Julie Boiché and Nelly Héraud declare that they have no conflicts of interest in the present research.
Human and animal rights and Informed consent
This study was approved by the ethical committee: 5 Santé. All procedures were in accordance with the Helsinki Declaration of 1975, as revised in 2000. Informed consent was obtained from all participants before being included in the study.
Electronic supplementary material
Below is the link to the electronic supplementary material.
Rights and permissions
About this article
Cite this article
Chevance, G., Caudroit, J., Henry, T. et al. Do implicit attitudes toward physical activity and sedentary behavior prospectively predict objective physical activity among persons with obesity?. J Behav Med 41, 31–42 (2018). https://doi.org/10.1007/s10865-017-9881-8
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s10865-017-9881-8