Abstract
Caring for adolescents with congenital heart disease requires attention to physical health but also to psychosocial functioning. Identifying how such psychosocial variables influence one another over time is important for designing health care strategies. The present study examined how depressive symptoms, loneliness, paternal and maternal support, and quality of life predicted one another. A total of 429 mid- to late adolescents with congenital heart disease (53.4 % boys) participated in a three-wave longitudinal study. Cross-lagged analyses indicated that depressive symptoms and loneliness mutually reinforced one another over time and led to relative decreases in quality of life. Paternal- and not so much maternal-support predicted relative decreases in depressive symptoms and loneliness and relative increases in quality of life. Maternal and paternal support, in turn, were negatively predicted by previous levels of adolescent depressive symptoms. In sum, important temporal sequences were uncovered potentially providing information for prevention and intervention targeting psychosocial functioning in adolescents with congenital heart disease.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Congenital heart disease, comprising a wide spectrum of simple, moderate, and complex heart lesions, is the most common birth defect (i.e., approximately 9 in 1,000 births) (van der Linde et al., 2011). Because of advances in pediatric cardiology and cardiac surgery, the life expectancy of these children has increased substantially over the past decades. To date, about 90 % of patients survive into adulthood (Moons et al., 2010). For many of these patients, congenital heart disease is accompanied by substantial stressors and challenges throughout their lifespan (Mussatto, 2006). Adolescence constitutes a crucial period in life in which individuals have to tackle various developmental challenges, such as establishing a mature identity and integrating themselves into the peer group (Luyckx et al., 2011a). Therefore, disease-specific challenges such as follow-up visits to physicians, therapeutic changes, limitations of physical activity, and transferring to different caregivers might be particularly stressful during this period in life. In sum, caring for adolescents with congenital heart disease requires attention to physical health but also to psychosocial health (Mussatto, 2006).
Research has increasingly focused on psychosocial functioning in children and adolescents with congenital heart disease (Fredriksen et al., 2009; Karsdorp et al., 2007). This body of research focused mainly on comparing individuals’ functioning with that of reference or control groups. Although individual studies tended to yield contradictory results and, consequently, a consensus among researchers has not been reached (Kovacs et al., 2005; Utens et al., 1998), a meta-analysis indicated that adolescents with congenital heart disease potentially show more internalizing problems as compared to controls (Karsdorp et al., 2007). Internalizing problems (e.g., depressed mood) are associated with inner turmoil and may not be readily visible to external observers such as parents and clinicians. Such problems represent an important challenge in the care for adolescents with congenital heart disease and, consequently, are in need of careful scientific inquiry into potential antecedents and outcomes. What is largely missing from the literature, however, is a longitudinal inquiry into how such internalizing symptoms influence (and are influenced by) quality of life in adolescents with congenital heart disease. If specific temporal sequences can be identified, they could potentially inform prevention and intervention efforts aimed at improving patients’ functioning and quality of life.
It should be emphasized that, for quality of life, a multitude of definitions and measurements prevail in cardiology and related fields. Quality of life is often used as a generic label to describe a variety of physical and psychosocial variables, which renders it an ambiguous concept (Moons et al., 2006a, b). Moons et al. (2006a, b) reviewed the literature and concluded their critique with stating that (a) quality of life must not be used interchangeably with health status or functional abilities; (b) quality of life basically is a subjective appraisal; and (c) overall quality of life needs to be assessed in complement to health-related quality of life. Hence, in the present study, quality of life is defined as the degree of overall life satisfaction that is positively or negatively influenced by individuals’ perceptions of certain important aspects of life, both related and unrelated to health (and their heart condition in this specific case) (Moons et al., 2005).
With respect to internalizing symptoms, depressive symptoms and loneliness are among the most frequently studied in both community and clinical samples. Both constructs are substantially interrelated and reciprocal influences have been found to operate across time in adolescence (Vanhalst et al., 2012). Suboptimal social relationships, social rejection, or a lack of social competence—all being germane to the experience of loneliness—indeed can result in depressive symptoms (Blatt, 1990). Conversely, depressive symptoms can give rise to feelings of loneliness as well because depressive symptoms may elicit social rejection by peers (Coyne, 1976). Despite the fact that such reciprocal influences potentially constitute a negative vicious circle substantially affecting quality of life, such longitudinal mechanisms remain to be investigated in adolescents with congenital heart disease.
Of crucial importance, depressive symptoms and loneliness do not develop in isolation. Parental support (defined as the emotional support and empathy towards the child and his or her needs and wishes) has been found to be a consistent predictor of internalizing symptoms in childhood and adolescence (Barber et al., 2005; Luyckx et al., 2011b). A recent study already pointed to the importance of parental support for psychosocial functioning in adolescents with congenital heart disease, as parental support was found to predict quality of life over time (Luyckx et al., 2012). However, this study did not include measures of depressive symptoms and loneliness and did not distinguish between maternal and paternal support. In fact, few studies to date focused explicitly on both paternal and maternal support in pediatric populations and mainly assessed (adolescent perceptions of) maternal support only. Studies that did focus on both fathers and mothers found that paternal support and involvement uniquely contributed to illness adaptation and treatment adherence in chronically ill adolescents (Berg et al., 2008; Shorer et al., 2011; Wysocki & Gavin, 2006).
The present study
The present longitudinal study investigated how internalizing symptoms (i.e., depressive symptoms and loneliness), paternal and maternal support, and quality of life predicted one another over time. Only recently, Chen et al. (2011) investigated how a broad array of biopsychosocial variables related to quality of life in an adult sample of patients with congenital heart disease and found psychological distress and social support to be the most important correlates. However, their questionnaire study was cross-sectional in nature which precluded any sound conclusions about the directionality of effect, which is crucial information if one wants to design intervention efforts.
In the present study, all variables were assessed at baseline and at two follow-up time points with 9-months intervals, resulting in a longitudinal design with three time points spanning a total of 18 months. Using cross-lagged analysis (which basically assesses directionality of effect), we hypothesized that depressive symptoms and loneliness would mutually reinforce one another over time, possibly resulting in a detrimental vicious circle over time. Further, we hypothesized that parental support could partially protect against internalizing symptoms and, hence, has the potential to offset such a vicious circle. Differential hypotheses for maternal and paternal support could not be forwarded at this point, but we expected that both maternal and paternal support could influence psychosocial functioning. Finally, increased levels of depressive symptoms and loneliness were expected to lead to decreases in quality of life, whereas both maternal and paternal support were expected to lead to increases in quality of life.
In addressing these relationships, we also examined the role of perceived health status because perceived health status has been related longitudinally to quality of life in the present sample of patients with congenital heart disease (Luyckx et al., 2012). In doing so, we also could examine, for instance, if internalizing symptoms would lead to a worsening of perceived health over time. In addition, clinical and demographic variables assessed at baseline, such as sex, age, and disease complexity, were controlled for. Previous research indicated that mean differences based on these control variables could emerge. For instance, girls typically report higher levels of depressive symptoms than boys (Petersen et al., 1993). Further, although internalizing symptoms have been shown to occur relatively independent of disease complexity in patients with congenital heart disease, the role of disease complexity remains rather unclear to date and, hence, will be explored (Kovacs et al., 2005).
Methods
Participants and procedure
As part of i-DETACH (Information technology Devices and Education programme for Transitioning Adolescents with Congenital Heart disease; PI: Philip Moons; Luyckx et al., 2011a, b), eligible patients were selected from the database of pediatric and congenital cardiology of the University Hospitals Leuven, Belgium. As the main goal of this ongoing longitudinal project is to chart how adolescents with congenital heart disease make the transition to and experience adult care (and adult roles in general), the time points were chosen to correspond with this challenging period in life (i.e., with the study being initiated at ages 14–18 years). Further, relatively short time intervals in-between the three time points of the present study (i.e., 9 months) were used to allow for a detailed mapping of development and change in this transitional stage. Patients were included if they met the following criteria: confirmed diagnosis of congenital heart disease, defined as structural abnormalities of the heart and/or great intrathoracic vessels that are actually or potentially of functional significance (Mitchell et al., 1971); aged 14–18 years at the start of the study on October 22, 2009; last cardiac outpatient visit at our tertiary care centre performed ≤5 years ago; being able to read and write Dutch; and the availability of valid contact details. Patients were excluded if they had cognitive and/or physical limitations that inhibit them to fill out questionnaires; if they previously underwent heart transplantation; and if patients and/or their parents did not consent to participate.
Of the 33,895 patients in the clinical database in September 2009, 17,199 had a congenital heart disease. A vast majority of these patients (91 %), however, were not within the age range targeted; 498 met all of the inclusion criteria. At each of the three time points spanning a total of 18 months, all eligible adolescents received a package by surface mail, which included a set of questionnaires, an information letter, an informed consent form (for parents and adolescents), and a pre-stamped and addressed return envelope. To obtain a high response rate, a modified Dillman’s (1983) approach was used (see Luyckx et al., 2011a, b). The proposed study protocol was approved by the Institutional Review Board of the University Hospitals Leuven, Belgium. This study was performed in accordance with ethical standards, as described in the 2002 Declaration of Helsinki.
A total of 429 adolescents with congenital heart disease participated at Time 1 (86 % participation rate), 398 participated at Time 2 (9 months after Time 1), and 365 participated at Time 3 (9 months after Time 2). A total of 348 individuals participated at all three time points. Hence, all 429 participants completed questionnaires on the study variables at Time 1, but a minority of them did not do so at Times 2 and/or 3. Participants with and without complete data were compared using Little’s (1988) Missing Completely At Random (MCAR) test. Only 11.33 % of data at the scale level was missing. A non-significant MCAR test statistic, χ2 (505) = 46.20, suggested that these missing values at Times 2 and 3 could be reliably estimated and allowed us to conduct analyses on all 429 participants. Further, a multivariate analysis of variance (MANOVA) at Time 1 indicated no mean differences on any of the study variables between the 346 longitudinal participants and those who dropped-out from the study after Time 1 (Wilks’ Lambda = 0.99; F (6, 400) = 0.61, p = .72, η2 = .01). Similarly, no differences were obtained on disease complexity (χ2 (2) = 0.70, p = .71), sex (χ2 (1) = 3.20, p = .07), and age (F (1, 427) = 0.03, p = .87, η2 = .00). Accordingly, to deal with missing values, we used the full information maximum likelihood (FIML) procedure provided in MPLUS 4.0 (Muthén & Muthén, 2002) which produces less biased and more reliable results as compared with conventional methods such as listwise deletion (Enders, 2010).
Measures
Quality of life
Quality of life was measured using a Linear Analogue Scale (LAS), which is a vertically oriented, 10-cm line, graded with indicators ranging from 0 (worst imaginable quality of life) to 100 (best imaginable quality of life). Participants were asked to rate their overall quality of life by marking a point on this scale. Validity and reliability of the LAS have been detailed elsewhere (Moons et al., 2006a, b). For instance, Moons et al. (2006a, b) indicated that, among other findings, (a) all participants assessed understood the purpose, procedure, and format of the LAS; (b) the LAS was highly correlated with alternative measures tapping into satisfaction with life; and (c) the LAS was characterized by high test–retest stability.
Perceived health status
Perceived health status was measured using a similar LAS, now graded with indicators ranging from 0 (worst imaginable health) to 100 (best imaginable health). Participants were asked to rate their overall health by marking a point on this scale.
Depressive symptoms
Depressive symptoms were measured with the 20-item Center for Epidemiologic Studies Depression Scale (Bouma et al., 1995). Each item asks how often participants had experienced symptoms of depression during the past week, using a 4-point scale from 0 (seldom) to 3 (most of the time or always). A scale score was calculated by summing all items (range 0–60), with higher scores indicating more frequent symptoms of depression. A sample item reads “During the last week, I felt depressed”. Cronbach’s alphas at Times 1–3 were .89, .89, and .91, respectively.
Loneliness
Loneliness was assessed with the 8-item version of the UCLA Loneliness Scale (Roberts et al., 1993). Participants responded to each item using a 5-point scale ranging from 1 (strongly disagree) to 5 (strongly agree). A scale score was calculated by averaging all the items (range 1–5), with higher scores indicating higher levels of loneliness. A sample item reads: “I feel isolated from others”. Cronbach’s alphas at Times 1–3 were .81, .84, and .86, respectively.
Paternal and maternal support
Parental support was assessed using the responsiveness subscale (with 7 items) of the Child Report of Parent Behavior Inventory (Schludermann & Schludermann, 1988). Adolescents responded using a 5-point scale, from 1 (strongly disagree) to 5 (strongly agree). A sample item reads: “My mother/father makes me feel better after talking over my worries with her/him”. Scale scores were calculated by averaging all the respective items (range 1–5), with higher scores indicating higher levels of support. Cronbach’s alphas at Times 1–3 were .91, .90, and .91, respectively, for mothers, and .91, .92, and .93, respectively, for fathers.
Plan of analysis
Cross-lagged path analysis using observed variables was applied from a structural equation modelling approach to examine the direction of effects over time. Figure 1 illustrates a cross-lagged design with two variables (variables X and Y) assessed at three measurement points. In our cross-lagged design, all six study variables were measured at three points in time, yielding estimates of synchronous (as indicated with a in Fig. 1), autoregressive or stability (as indicated with b and c), and cross-lagged relations (as indicated with d and e). Association a refers to the association between different variables at each point in time; associations b and c refer to the prediction of a variable by its level at previous time points; and associations d and e refer to the prediction of a variable at Time t + 1 by another variable that has been measured at Time t, controlling for the Time t level of the predicted variable. Hence, these latter cross-lagged coefficients can be interpreted as variable X assessed at Time t predicting relative changes (i.e., relative increases or decreases) in variable Y assessed at Time t + 1 (or vice versa). To evaluate model fit, we used the Chi-squared index, which should be as small as possible; the Root Mean Square Error of Approximation (RMSEA), which should be less than .08; the Comparative Fit Index (CFI), which should exceed .90; and the Standardized Root Mean Square Residual (SRMR) should be less than .09 (Kline, 2006).
Cross-lagged analysis proceeded in three steps. First, all paths included in the model were freely estimated (i.e., the unconstrained model). Second, we constrained the unstandardized cross-lagged paths to be equal across both intervals (i.e., coefficients d in Fig. 1 were set equal and coefficients e were set equal across Times 1–2 and Times 2–3), hence resulting in a more parsimonious model producing more reliable estimates of the different cross-lagged coefficients (i.e., the stationarity-assumed model). If the stationarity-assumed and unconstrained models provide equivalent fit to the data, then the assumption of stationarity can be retained. The stationarity assumption would be statistically rejected if the difference in χ2 (Δχ2), relative to the degrees of freedom, between both models would be significant at p < .05. Third, using multi-group analyses, we tested whether cross-lagged coefficients could be constrained as equal for boys versus girls (e.g., the path from depressive symptoms to quality of life was set equal for boys and girls), indicating that the paths of interest would not be moderated by gender.
Results
Sample characteristics
The sample at Time 1 consisted of 229 boys and 200 girls, with a mean age of 15.75 years. The primary heart defect was categorized using a modified version of the scheme developed by the CONCOR (CONgenital COR Vitia) project (Vander Velde et al., 2005); the modifications are detailed elsewhere (Moons et al., 2009). Patients were categorised according to their disease complexity by using the classification of the Task Force 1 of the 32nd Bethesda conference: simple, moderate, or complex (Warnes et al., 2001). This classification takes the primary diagnosis, any procedures, and residua into account. A total of 40.6 % of patients had a simple heart defect and 11.9 % had a complex heart defect; 46.6 % received cardiac surgery in the past. With respect to family structure, 77.1 % of adolescents had parents who were married or living together. Demographic and clinical characteristics are detailed in Table 1.
Preliminary mean-level and correlational analyses
Table 2 displays means and standard deviations for all study variables at Times 1–3. A series of univariate analyses of variance (ANOVA) were conducted to investigate whether sex and complexity of heart defect were related to the study variables at Times 1–3. As detailed in Table 2, these ANOVAs pointed to mean differences based on sex and complexity of heart defect. Girls scored higher on depressive symptoms at Times 1–3 as compared to boys. Adolescents with a complex heart defect scored lowest on perceived health status at Times 1 and 3 and on quality of life at Time 1. All effects reported were accompanied by a small effect size, as indicated by values for η2 below .059 (Cohen, 1988). Further, age was negatively related to perceived health status (r = −.11, p < .05) and maternal support (r = −.10, p < .05) at Time 1. Hence, sex, disease complexity, and age were included in the cross-lagged analyses as control variables by estimating paths from these variables to all study variables.
Table 3 presents the correlations among the study variables at Times 1–3. All variables were significantly interrelated at the different time points. Depressive symptoms and loneliness were negatively and maternal and paternal support were positively related to perceived health status and quality of life. Maternal and paternal support were negatively related to depressive symptoms and loneliness. In the next set of analyses, cross-lagged analysis was used to determine directionality of effect over time.
Cross-lagged analyses
In a first set of cross-lagged analyses, we examined how perceived health status, quality of life, depressive symptoms, and loneliness predicted one another over time. The cross-lagged model including all within-time correlations, all stability coefficients, all cross-lagged paths among the study variables at Times 1–3, and additional paths from the control variables (i.e., age, sex, and disease complexity) had an excellent fit to the data (df = 12; χ2 = 12.26, p = .42; RMSEA = .007; CFI = 1.000; SRMR = .015). The control variables were substantially related to the study variables in line with the results reported earlier in the univariate ANOVAs and, hence, these associations are not reiterated here. Next, the stationarity-assumed model in which all cross-lagged paths were constrained as equal over time was estimated (df = 24; χ2 = 18.02, p = .80; RMSEA = .000; CFI = 1.000; SRMR = .015) and was favored over the less parsimonious unconstrained model (Δχ2 (12) = 5.73, p = .93). As can be seen in Fig. 2, perceived health status predicted relative increases in quality of life over time, depressive symptoms predicted decreases in perceived health status and quality of life and increases in loneliness over time. Loneliness, in turn, predicted increases in depressive symptoms and decreases in quality of life over time. Table 4 contains all significant coefficients for the stability and cross-lagged paths.
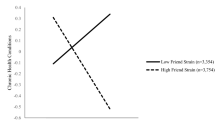
In a second set of cross-lagged analyses, all non-significant cross-lagged paths were trimmed from the previous stationarity-assumed model and maternal and paternal support were added to the model to examine temporal sequences involving parental support, again resulting in an excellent fit to the data (df = 68; χ2 = 85.33, p = .08; RMSEA = .024; CFI = 0.995; SRMR = .030). As detailed in Table 4, paternal support predicted increases in perceived health status and quality of life and decreases in depressive symptoms and loneliness over time. Finally, ancillary multigroup analyses indicated that the cross-lagged paths were not moderated by gender (Δχ2 (16) = 17.42, p = .36). Hence, the temporal sequences identified applied equally well to boys and girls.
Discussion
The present longitudinal study investigated how internalizing symptoms (i.e., depressive symptoms and loneliness), parental support, perceived health status, and quality of life predicted one another over time in a large sample of adolescents with congenital heart disease. Before we turn to discussing the important temporal sequences obtained, it needs to be emphasized that, as expected, girls with congenital heart disease scored higher than boys on depressive symptoms. Further, although not consistently replicated across all three time points, adolescents with a complex heart defect scored somewhat lower on perceived health status and, to a lesser extent, quality of life as compared to other adolescents with a simple or moderate defect. Of crucial importance, however, the longitudinal findings were obtained after controlling for these relatively limited mean-level differences. Further, ancillary analyses indicated that these longitudinal findings were not moderated by sex. Put differently, the directionality of effects and the strength of the different paths involved were highly similar for both boys and girls.
Readers should note that some of the cross-lagged coefficients were rather small, but that these coefficients were obtained when simultaneously controlling for all within-time associations and autoregressive paths. Further, such relatively modest coefficients could be expected given that the variables under study are potentially determined by additional variables not assessed in the present study. This being said, important temporal sequences were obtained which potentially provided information for prevention and intervention efforts targeting psychosocial functioning in adolescents with congenital heart disease and, potentially, other chronic diseases, as detailed below. First, in line with recent longitudinal research in community samples, loneliness and depressive symptoms were found to predict one another over time, constituting a negative vicious circle. These findings confirm and, at the same time, substantially extend recent cross-sectional findings in a sample of adults with congenital heart disease, demonstrating that loneliness functioned as an important correlate of depressive symptoms (Kovacs et al., 2009). Although this previous study proved to be highly informative, the present study is the first to demonstrate that depressive symptoms and loneliness reinforce one another over time in patients with congenital heart disease. Hence, for clinical interventions to be successful in the long run, they need to focus on both internalizing symptoms simultaneously because, due to their developmental interdependence, changes in any of both constructs must be reinforced by corresponding changes in the other construct.
Second, despite the fact that both perceived maternal and paternal support were related to all study variables at all three time points, especially paternal support proved to be the most consistent predictor of over-time changes in depressive symptoms and loneliness. These findings need to be emphasized given that the majority of studies on parent–child relationships in clinical samples focused on maternal involvement and, hence, somewhat overlooked the unique contribution fathers can have on their children’s development. Especially during adolescence, fathers can become increasingly important given that they tend to encourage—potentially more so than mothers do—adolescents’ self-reliance and individuation (Seiffge-Krenke, 2002). Such a pattern could partially explain why fathers in the present study tend to have a unique impact on psychosocial functioning. Although mothers have been found to be generally more involved with the management of their offspring’s disease (Seiffge-Krenke, 2002) and to report more distress with respect to congenital heart disease (Spijkerboer et al., 2007), congenital heart disease is not necessarily the most salient aspect of adolescents’ daily life. Hence, encouraging adaptive levels of both maternal and paternal involvement in the management of pediatric chronic diseases remains of the utmost importance during adolescence (Casey et al., 1996; Wysocki & Gavin, 2006), but parents need to stay attuned to their children’s developmental needs as well in order for their children to flourish in the challenging transition to adulthood. Perceived maternal and paternal support, in turn, were predicted by adolescents’ level of depressive symptoms. Hence, in line with a growing body of evidence indicating that parents and chronically ill adolescents mutually influence one another’s functioning (Chaney et al., 1997), important reciprocal processes were found in the present study. As such, the present findings have important clinical implications in that the total family system has to be taken into account to break detrimental vicious circles that can put adolescents with congenital heart disease on a pathway to ill-being and suboptimal functioning.
Finally, these previous variables in tandem (i.e., depressive symptoms, loneliness, and parental support) were found to predict quality of life over time, whereas quality of life was not found to predict changes in any of these variables. Hence, the present study supported the theoretical hypothesis prevailing in the congenital heart disease literature that generic psychosocial functioning substantially affects quality of life in these patients, even when taking into account the influence of disease complexity and perceived health status (Kovacs et al., 2009). Although perceived health status proved to be a significant predictor of quality of life in the present analyses, the importance of psychosocial issues should not be overlooked in clinical practice. Indeed, depressive symptoms were also found to lead to a worsening of perceived health status over time, again emphasizing the need to attend to internalizing symptoms in this population.
Summarizing across the present findings and taking previous research efforts in the literature into account, Fig. 2 could provide a framework for (a) researchers interested in examining psychosocial issues in adolescents with congenital heart disease and other chronic diseases and (b) clinicians interested to tackle these issues in their contacts with these youngsters. However, such psychosocial issues are generally not attended to in detail in the training of cardiologists (Kovacs et al., 2005). Nonetheless, adolescents with congenital heart disease will benefit from an increased awareness of and attention towards these issues, further testifying to the need for a strong multidisciplinary input (e.g., cardiologist, nurse, and psychologist) into routine clinical care (Utens et al., 1998). It should be noted that, for most adolescents in the present sample, the magnitude of internalizing symptoms did not meet the threshold for being labelled as psychopathology. However, the fact that these symptom scores represented rather normal variants does not downgrade the importance of our findings. Apparently, intra-individual changes in internalizing symptoms outside the clinical range also have the potential to influence variables such as quality of life. In addition, subclinical levels of internalizing symptoms could hinder adolescents from mastering normative developmental tasks and render them vulnerable for developing psychopathology later in life (Petersen et al., 1993).
Limitations and suggestions for future research
The present study has some limitations which provide suggestions for future research. First, all primary study variables were self-reported by the adolescents with congenital heart disease. Although adolescent self-report is the most valid measure to assess perceptions of parental support because it captures how adolescents subjectively experience such support, future research would be strengthened by using data from multiple sources. Such future research should also include additional and more extensive measures tapping into quality of life and perceived health, as these constructs were measured by a single item in the present study. In addition, although the present took into account disease complexity (which is mainly based on initial CHD diagnosis and any procedures used) in all primary analyses, future studies should include current functional status and physical health as potential predictors of psychosocial functioning (Chen et al., 2011).
Second, the single-center setting and the specific nature of the study population also reduced the generalizability of the findings. However, the proportion of patients with a simple, moderate, or complex heart defect in the present study corresponds to the reported prevalence in the literature (Moons et al., 2010). The composition of our sample can therefore be considered as representative for the population of adolescents with congenital heart disease. Furthermore, patients were recruited from the database of one university hospital, but received follow-up in different hospitals across the country.
Third, although the present manuscript did not provide information on mean-level developmental trends and trajectories over time, the present study is embedded in a larger longitudinal project in which a total of four measurement waves will be collected spanning nearly 3 years. Hence, future research reports based on this project will allow for charting developmental trajectories of the variables under study.
Finally, although participation rates were very high at each time point resulting in large sample sizes of adolescents with congenital heart disease, some attrition is inevitable in longitudinal studies which could potentially affect study results. However, attrition analyses pointed to no systematic pattern in these missing data and, hence, a systematic attrition bias is unlikely to affect the present study results.
Despite these limitations, the present study was the first to demonstrate that internalizing symptoms mutually predict one another over time and actually predict quality of life in adolescents with congenital heart disease, using a strong methodological design. Further, findings again emphasized the need to focus on paternal involvement in addition to maternal involvement in studies on children and adolescents with chronic diseases. We hope that the present findings could inform future longitudinal studies on psychosocial functioning in chronic disease in an attempt to set up a knowledge base for designing prevention and intervention efforts.
References
Barber, B. K., Stolz, H. E., & Olsen, J. A. (2005). Parental support, psychological control, and behavioral control: Assessing relevance across time, method, and culture. Monographs of the Society for Research in Child Development, 70(4, Serial No. 281).
Berg, C. A., Butler, J. M., Osborn, P., King, G., Palmer, D. L., Butner, J., et al. (2008). Role of parental monitoring in understanding the benefits of parental acceptance on adolescent adherence and metabolic control of type 1 diabetes. Diabetes Care, 31, 678–683.
Blatt, S. J. (1990). Interpersonal relatedness and self-definition: Two personality configurations and their implications for psychopathology and psychotherapy. In J. Singer (Ed.), Repression: Defense mechanisms and personality (pp. 299–335). Chicago: University of Chicago Press.
Bouma, J., Ranchor, A. V., Sanderman, R., & van Sonderen, E. (1995). Het meten van symptomen van depressie met de CESD: Een handleiding [The measurement of symptoms of depression with the CESD: A manual]. Groningen, The Netherlands: Noordelijk Centrum voor Gezondheidsvraagstukken.
Casey, F. A., Sykes, D. H., Craig, B. G., Power, R., & Mulholland, H. C. (1996). Behavioral adjustment of children with surgically palliated complex congenital heart disease. Journal of Pediatric Psychology, 21, 335–352.
Chaney, J. M., Mullins, L. L., Frank, R. G., Peterson, L., Mace, L. D., Kashani, D. A., et al. (1997). Transactional patterns of child, mother, and father adjustment in insulin-dependent diabetes mellitus: A prospective study. Journal of Pediatric Psychology, 22, 229–244.
Chen, C. A., Liao, S. C., Wang, J. K., Chang, C. I., Chiu, I. S., Chen, Y. S., et al. (2011). Quality of life in adults with congenital heart disease: Biopsychosocial determinants and sex-related differences. Heart, 97, 38–43.
Cohen, J. (1988). Statistical power analyses for the behavioral sciences (2nd ed.). Hillsdale, NY: Erlbaum.
Coyne, J. C. (1976). Toward an interactional description of depression. Psychiatry: Interpersonal and Biological Processes, 39, 28–40.
Dillman, D. A. (1983). Mail and other self-administered questionnaires. In P. H. Rossi, J. D. Wright, & A. B. Anderson (Eds.), Handbook of survey research (pp. 359–377). New York: Academic Press.
Enders, C. K. (2010). Applied missing data analysis. New York: Guilford.
Fredriksen, P. M., Diseth, T. H., & Thaulow, E. (2009). Children and adolescents with congenital heart disease: Assessment of behavioural and emotional problems. European Child and Adolescent Psychiatry, 18, 292–300.
Karsdorp, P. A., Everaerd, W., Kindt, M., & Mulder, B. J. M. (2007). Psychological and cognitive functioning in children and adolescents with congenital heart disease: A meta-analysis. Journal of Pediatric Psychology, 32, 527–541.
Kline, R. B. (2006). Principles and practices of structural equation modeling (2nd ed.). New York: Guilford Press.
Kovacs, A. H., Saidi, A. S., Kuhl, E. A., Sears, S. F., Silversides, C., Harrison, J. L., et al. (2009). Depression and anxiety in adult congenital heart disease: Predictors and prevalence. International Journal of Cardiology, 137, 158–164.
Kovacs, A. H., Sears, S. F., & Saidi, A. S. (2005). Biopsychosocial experiences of adults with congenital heart disease: Review of the literature. American Heart Journal, 150, 193–201.
Little, R. J. A. (1988). A test of missing completely at random for multivariate data with missing values. Journal of the American Statistical Association, 83, 1198–1202.
Luyckx, K., Goossens, E., Missotten, L., & Moons, P. (2011a). Adolescents with congenital heart disease: The importance of perceived parenting for psychosocial and health outcomes. Journal of Developmental and Behavioral Pediatrics, 32, 651–659.
Luyckx, K., Goossens, E., Van Damme, C., & Moons, P. (2011b). Identity formation in adolescents with congenital cardiac disease: A forgotten issue in the transition to adulthood. Cardiology in the Young, 21, 411–420.
Luyckx, K., Missotten, L., Goossens, E., & Moons, P. (2012). Individual and contextual determinants of quality of life in adolescents with congenital heart disease. Journal of Adolescent Health, 51, 122–128.
Mitchell, S. C., Korones, S. B., & Berendes, H. W. (1971). Congenital heart disease in 56,109 births. Incidence and natural history. Circulation, 43, 323–332.
Moons, P., Bovijn, L., Budts, W., Belmans, A., & Gewillig, M. (2010). Temporal trends in survival to adulthood among patients born with congenital heart disease from 1970–1992 in Belgium. Circulation, 122, 2264–2272.
Moons, P., Budts, W., & De Geest, S. (2006a). Critique on the conceptualisation of quality of life: A review and evaluation of different conceptual approaches. International Journal of Nursing Studies, 43, 891–901.
Moons, P., Sluysmans, T., De Wolf, D., Massin, M., Suys, B., Benatar, A., et al. (2009). Congenital heart disease in 111,225 births in Belgium: Birth prevalence, treatment and survival in the 21st century. Acta Paediatrica, 98, 472–477.
Moons, P., Van Deyk, K., De Bleser, L., Marquet, K., Raes, E., De Geest, S., et al. (2006b). Quality of life and health status in adults with congenital heart disease: A direct comparison with healthy counterparts. European Journal of Cardiovascular Prevention and Rehabilitation, 13, 407–413.
Moons, P., Van Deyk, K., Marquet, K., Raes, E., De Bleser, L., Budts, W., et al. (2005). Individual quality of life in adults with congenital heart disease: A paradigm shift. European Heart Journal, 26, 298–307.
Mussatto, K. (2006). Adaptation of the child and family to life with a chronic illness. Cardiology in the Young, 16, 110–116.
Muthén, L. K., & Muthén, B. O. (2002). Mplus user’s guide. Los Angeles, CA: Muthén & Muthén.
Petersen, A. C., Compas, B. E., Brooks-Gunn, J., Stemmler, M., Ey, S., & Grant, K. E. (1993). Depression in adolescence. American Psychologist, 48, 155–168.
Roberts, R. E., Lewinsohn, P. M., & Seeley, J. R. (1993). A brief measure of loneliness suitable for use with adolescents. Psychological Reports, 72, 1379–1391.
Schludermann, E. H., & Schludermann, S. M. (1988). Children’s report on parent behavior (CRPBI-108, CRPBI-30) for older children and adolescents. Technical report. Winnipeg, MB, Canada: University of Manitoba, Department of Psychology.
Seiffge-Krenke, I. (2002). “Come on, say something, dad!”: Communication and coping in fathers of diabetic adolescents. Journal of Pediatric Psychology, 27, 439–450.
Shorer, M., David, R., Schoenberg, M., Levavi-Lavi, I., Phillip, M., & Meyerovitch, J. (2011). Role of parenting style in achieving metabolic control in adolescents with type 1 diabetes. Diabetes Care, 34, 1735–1737.
Spijkerboer, A. W., Helbing, W. A., Bogers, A. J. J. C., Van Domburg, R. T., Verhulst, F. C., & Utens, E. M. W. J. (2007). Long-term psychological distress and styles of coping in parents of children who underwent invasive treatment for congenital cardiac disease. Cardiology in the Young, 17, 638–645.
Utens, E. M., Verhulst, F. C., Duivenvoorden, H. J., Meijboom, F. J., Erdman, R. A., & Hess, J. (1998). Prediction of behavioural and emotional problems in children and adolescents with operated congenital heart disease. European Heart Journal, 19, 801–807.
van der Linde, D., Konings, E. E. M., Slager, M. A., Witsenburg, M., Helbing, W. A., Takkenberg, J. J. M., et al. (2011). Birth prevalence of congenital heart disease worldwide. Journal of the American College of Cardiology, 58, 2241–2247.
Vander Velde, E. T., Vriend, J. W., Mannens, M. M., Uiterwaal, C. S., Brand, R., & Mulder, B. J. (2005). CONCOR, an initiative towards a national registry and DNA-bank of patients with congenital heart disease in The Netherlands: Rationale, design, and first results. European Journal of Epidemiology, 20, 549–557.
Vanhalst, J., Klimstra, T. A., Luyckx, K., Scholte, R. H. J., Engels, R. C. M. E., & Goossens, L. (2012). The interplay of loneliness and depressive symptoms across adolescence: Exploring the role of personality traits. Journal of Youth and Adolescence, 41, 767–787.
Warnes, C. A., Liberthson, R., Danielson, G. K., Dore, A., Harris, L., Hoffman, J. I. E., et al. (2001). Task force 1: The changing profile of congenital heart disease in adult life. Journal of the American College of Cardiology, 37, 1170–1175.
Wysocki, T., & Gavin, L. (2006). Paternal involvement in the management of pediatric chronic diseases: Associations with adherence, quality of life, and health status. Journal of Pediatric Psychology, 31, 501–511.
Acknowledgments
Funding was provided through grant OT/11/033 from the Research Fund-Catholic University of Leuven (Belgium).
Conflict of interest
The authors have no conflict of interest to disclose.
Author information
Authors and Affiliations
Corresponding author
Additional information
This study is conducted on behalf of the i-DETACH investigators.
Rights and permissions
About this article
Cite this article
Luyckx, K., Goossens, E., Rassart, J. et al. Parental support, internalizing symptoms, perceived health status, and quality of life in adolescents with congenital heart disease: influences and reciprocal effects. J Behav Med 37, 145–155 (2014). https://doi.org/10.1007/s10865-012-9474-5
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s10865-012-9474-5