This study assessed the ability of minor life events to predict medical utilization among 141 low-income, predominantly African American family practice patients. Subjects completed one year of stress assessments including major and minor life events. Four years of prospective medical utilization was collected, including outpatient, inpatient, and emergency department visits. Hierarchical regressions were conducted to assess the predictive value of minor life events for utilization, after controlling for demographic variables and major life events. The impact of minor life events was a significant predictor of outpatient utilization, accounting for 3.6% of the variance. Minor life events were unrelated to emergency department and inpatient visits. The relationship between minor life events and some types of utilization suggests traditional stress management techniques may be beneficial in reducing utilization for some patients, although such conclusions are tempered by the modest relationship between stress and utilization.
Similar content being viewed by others
Explore related subjects
Discover the latest articles, news and stories from top researchers in related subjects.Avoid common mistakes on your manuscript.
INTRODUCTION
On average, Americans make approximately 3.5 outpatient medical visits annually, including visits to physicians' offices, hospital outpatient clinics, and emergency departments. In addition, nearly 120 per 1,000 individuals are admitted for medical inpatient care per year. Consequently, over $390 billion and $269 billion, respectively, are spent annually on hospital care and other physician and clinical services (National Center for Health Statistics, 2001). Due to the frequency of medical visits in the general population and the rising costs of health care services, researchers have paid increasing attention to factors associated with medical utilization.
Andersen and colleagues have formulated the most widely researched model of utilization, which includes predisposing factors (e.g., demographic variables, attitudes, beliefs), enabling factors (e.g., income, insurance), and need factors (e.g., symptoms, diagnoses) (Aday and Awe, 1997; Andersen and Newman, 1973). Despite the breadth and extensive research associated with this model, it accounts for only a modest proportion of the variance in utilization (Aday and Awe, 1997; Krause, 1988; Mechanic, 1979; Wolinsky, 1978). Thus, researchers have suggested examining other factors, such as stressful life events, for their potential relationship with medical utilization (Krause, 1988; Mechanic, 1979; Gortmaker et al., 1982).
Life stress could increase medical utilization for a number of reasons (Brantley and Ames, 2001). First, some individuals may take advantage of medical services as a means of coping with life stress (Mechanic and Volkart, 1961; Tessler et al., 1976). Second, stress negatively affects the symptoms of various medical conditions, including headaches (Benedittis and Lorenzetti, 1992; Fernandex and Sheffield, 1996; Sorbi et al., 1996), gastrointestinal conditions (Garrett et al., 1991; Searle and Bennett, 2001), diabetes (Aikens et al., 1992; Karamer et al., 2000), and cardiovascular conditions (Lindquis et al., 1997; Theorell and Emlund, 1993; Twisk et al., 1999). Third, stress has been associated with suppression of the immune system, leading to increased risk of infections (Brosschot et al., 1994; Cohen et al., 1991; Turner-Cobb and Steptoe, 1996). Finally, stress can indirectly affect health through changes in health behaviors, such as decreased medical compliance and decreased exercise (Hitchcock et al., 1990).
While early research with stressful life events focused on the effects of major life events (e.g., divorce, bereavement), subsequent research has examined the relationship between minor life events and health outcomes. Minor life events, or daily hassles, include everyday occurrences such as driving in heavy traffic, arguing with a spouse, etc. Research comparing the effects of major and minor stress suggests that minor stress demonstrates a stronger relationship to both physical and psychological outcomes (DeLongis et al., 1982; Kanner et al., 1981; Lazarus and Folkman, 1984; Ruffin, 1993). Compared to major stress, minor stress was a better predictor of symptoms in Crohn's Disease (Garrett et al., 1991), rheumatoid arthritis (Thomason et al., 1992), inflammatory bowel disease (Searle and Bennett, 2001), and headaches (Benedittis and Lorenzetti, 1992; Fernandex and Sheffield, 1996; Sorbi et al., 1996). Minor stress was also a better predictor of medical regimen compliance as compared to major life events (Hitchcock et al., 1990).
Minor stress may be a better predictor than major life events because minor events are more intimately tied to the manner in which a person handles stressful situations and demands (Kanner et al., 1981). The construct of minor life events, or daily hassles, includes both the environmental event as well as the individual's appraisal of that event and how it impacts his or her well-being (Lazarus, 1984). Further, Lazarus (1984) points out that major life events influence health by affecting individuals' daily routines, including minor life events and hassles. In this way, minor stressors may have a stronger influence on health because they have both independent effects on health as well as effects initiated by major life events. Identifying the role of minor life events is important because they are typically the focus of stress management programs (Brantley and Ames, 2001).
In light of such findings on stress and symptomatology, it is clear that stressful life events have the potential to increase medical utilization. Using self-report of daily stress and utilization, one early study found that high stress levels were associated with increased use of certain medical services, including increased rates of phone contact with physicians, emergency room visits, and visits to hospital outpatient clinics (Roghmann and Haggerty, 1973). Miranda and colleagues (Miranda et al., 1991) found major life stress to be associated with utilization through a more rigorously controlled study, although they did not address the role of minor life events. Only a handful of studies have examined both major and minor life stress in relation to medical utilization. Gortmaker et al. (1982) examined the effects of major and minor stress and found that utilization increased in the presence of both types of stress. The interaction of minor stress and heightened sensitivity to bodily sensations has been associated with increased medical utilization in patients suffering from heart palpitations, while major life stress showed no such relationship (Barsky et al., 1996). In a sample of Native American patients, major and minor stress were associated with subsequent hospital admissions, whereas outpatient visits were significantly related to minor stress only (Williams et al., 1992).
These studies provide valuable information on stress and medical utilization, but several shortcomings are common. First, many studies rely upon self-report of utilization (Gortmaker et al., 1982; Barsky et al., 1996) rather than a more objective method (e.g., chart reviews). Second, there has been a failure to measure the effects of minor stress on utilization (Mechanic and Volkart, 1961; Miranda et al., 1991; Pilisuk et al., 1987). Third, studies including minor stress have typically used unsophisticated measures of minor life stress. For example, Gortmaker et al. (1982) used an unvalidated measure of daily stress that focused on family and household stressors while ignoring other potential sources of stress. Fourth, few studies have taken more than one stress assessment (Krause, 1988; Miranda et al., 1991; Williams et al., 1992). Fifth, previous studies have utilized a retrospective design (Williams et al., 1992). Finally, there is a lack of research on medical services use among low income and uninsured individuals who depend increasingly on subsidized health care.
The objective of the current study was to determine the relationship between minor life events and medical utilization for family practice patients, while controlling for the influence of major life events and demographic variables. The current study attempted to address limitations of past research by including a prospective design over a four-year period of utilization, an objective measure of utilization obtained via chart review, and valid and reliable measures of life stress administered on several occasions. In addition, the current study included a sample of low-income, predominantly African American primary care patients.
METHOD
Participants
Adults were recruited from the waiting room of a family practice outpatient clinic at a public teaching hospital in the southeastern U.S. The hospital population is predominately low income, African American women who have no insurance coverage. Patients report receiving little if any care outside this hospital, which for all practical purposes represents a closed health delivery system. Patients who were at least 18-years-old and had access to a telephone (for follow-up assessments) were eligible for participation. Three hundred sixty patients were enrolled in the study. Of these, 295 completed the year of stress assessments. Any subjects who did not have complete utilization data for the four-year period (e.g., death, relocation) were excluded from analyses. However, the reason for patients' attrition was not available. One hundred forty-one subjects had complete data and were included in analyses, indicating a 52% attrition rate during the utilization period.
Measures
Life Experiences Survey (LES)
The LES (Sarason et al., 1978) is a 60-item inventory in which subjects indicate major stressors experienced during the past 6–12 months. Subjects also rate the intensity of each event's impact, with responses ranging from a value of –3 (extremely negative) to a value of +3 (extremely positive). Sarason et al. (1978) reported that the reliability of negative event scores ranged from .56 to .88. The reliability coefficients for total change (including both positive and negative events) ranged from .63 to .64.
Weekly Stress Inventory (WSI)
The WSI (Brantley et al., 1997) is an 87-item inventory of daily unpleasant events, in which respondents refer to events that occurred over the past week. Subjects indicate if each item occurred, and they rate the impact of each event on a scale ranging from 1 (happened but not stressful) to 7 (extremely stressful). The WSI reports both an event score (i.e., number of events that occurred) and an impact score (i.e., total perceived stressfulness of endorsed items). The WSI has shown high internal consistency, with coefficients ranging from .92 to .96, and high test-retest reliability during the same week (r = .83). Research indicates that five administrations of the WSI across a one-year period provide a highly stable measure of stress (Scarinci et al., 1999). The WSI correlates highly with a daily measure of stressful life events (Daily Stress Inventory) that has been linked to biochemical stress indices (Brantley et al., 1997).
Medical Utilization
Medical utilization data were collected by chart reviews, which resulted in four years of utilization data. Three doctoral graduate students, trained and provided with standardized protocol regarding classification of visits, conducted the chart reviews. Chart reviews obtained values for each patient's outpatient medical, emergency department, and inpatient visits. Inter-rater reliability checks were completed on 15% of the sample, and the intercorrelations ranged from .97 to 1.00 across the different types of medical visits.
Procedure
Subjects were randomly selected from patient appointment rosters and were approached in the family practice waiting room, where IRB-approved informed consent was obtained. Subjects also completed demographic questionnaires, the LES, and the WSI. Subjects were contacted every other month for one year via telephone to complete the WSI. The LES was also re-administered at month 6 and month 12. Participants were compensated a total of $160 for their participation (assessment visits and telephone calls). At month 12, a family practice physician conducted chart reviews to determine the number of diagnosed chronic illnesses. Chronic illnesses were defined as diseases and disorders continuing for six months or longer, such as diabetes, hypertension, and asthma. Four years after the termination of the stress assessments, a chart review was conducted to assess utilization.
Statistical Analysis
Primary outcome analyses were conducted using hierarchical multiple regressions, which assessed the ability of specified demographic variables and major and minor life events to predict utilization. Predictor variables were entered in steps, with variables from the previous step retained in subsequent steps. The first step included the number of chronic illnesses, age, gender, and ethnicity. The second step included LES impact scores, while the third step included WSI impact scores. Impact scores were used rather than event scores, since impact scores assess both the frequency of life stress and the individuals' appraisal of such events (Lazarus and Folkman, 1984). Separate regressions were conducted for each type of utilization, including outpatient, inpatient, and emergency department visits.
Prior to conducting the regressions, correlations between predictor and outcome variables were conducted. Additional analyses included descriptive statistics summarizing demographic information. Independent samples t-tests and chi square analyses were used to assess for differences between subjects who completed the study and those lost to attrition.
RESULTS
Sample Characteristics and Descriptive Statistics
A total of 141 participants remained enrolled as patients at the research site for the five-year study. Demographic characteristics of this sample are summarized in Table I. Table II includes descriptive statistics on subjects' stressful life events and utilization. Regarding minor life events, the WSI impact scores were similar to those obtained with community sample subjects of comparable age (Brantley et al., 1997). Regarding major life events, the LES impact scores were comparable to the scores found in a validation sample (Sarason et al., 1978). Participants attended a mean of 22 medical outpatient and emergency department visits over four years for an average of 5.5 visits per year. Compared to participants lost to attrition, participants completing the study did not differ on any assessed variables, including age, gender, ethnicity, number of chronic illnesses, LES impact scores, and WSI impact scores.
Correlations of Predictor and Criterion Variables
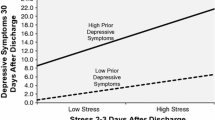
Intercorrelations of the predictor and criterion variables were computed prior to regression calculations (see Table III). Utilization of outpatient services and inpatient services were positively correlated with the number of chronic illnesses. Similarly, age was positively associated with outpatient and inpatient utilization. WSI impact scores were related to outpatient visits, such that individuals with higher minor stress scores demonstrated greater levels of utilization. Gender, ethnicity, and LES impact scores were unrelated to the utilization measures.
Predictors of Medical Utilization
For outpatient visits, step 1 of the regression accounted for a significant portion of the variance in utilization, (R 2 = .16, p < .001). The betas for the variables in this step showed that the number of chronic illnesses was the only significant predictor, (B = .30, p < .01). The impact of minor life events accounted for a significant amount of variance in outpatient medical visits, (R 2 Δ = .036, p < .02), while the impact of major life events failed to make a significant contribution in predicting outpatient visits (see Table IV).
The demographic variables in Step 1 of the regression were significantly predictive of inpatient utilization, (R 2 = .09, p < .02). Inspection of the individual betas indicated that age was the only variable responsible for this relationship, (B = .20, p < .05). The impact of major and minor stress was not related to inpatient utilization. For emergency department visits, none of the predictor variables were related to utilization.Footnote 1
DISCUSSION
The current study possesses several strengths building upon previous research on stress and utilization. First, this study assessed the relationship between minor life events and utilization, which has received considerably less attention than major life events. This study also included four years of utilization, which surpassed the time interval included in many projects. This is particularly important, as Pilisuk et al. (1987) found the effects of stress on utilization did not emerge until at least two years of utilization data had been collected, suggesting a limited time interval could be inadequate for such purposes. The current study also included several assessments of stressful life events, which likely provided a more reliable and valid measure of stress. Another asset was the inclusion of a predominantly minority, low-income sample, which has received less research attention in this area.
Current results suggest minor life events were a significant predictor of medical utilization in low-income, predominantly African American patients. Family practice patients who endorsed more stressful minor life events demonstrated greater rates of outpatient visits. Minor life events accounted for approximately 3.6% of the variance in outpatient visits. This influence of minor life events was significant even after accounting for the relationship between chronic illness and utilization. However, minor life events were unrelated to emergency department or inpatient visits, suggesting variability in the influence of minor stress on different types of utilization. Further, the impact of major life events failed to significantly predict any types of utilization.
There are several potential reasons why minor life events were related to certain types of hospital visits but not others. Patients may be more likely to present to the emergency room or be hospitalized for accidents and related injuries, which may be less influenced by chronic stress. In contrast, outpatient visits would typically include more elective-type procedures. Also, it may be important to consider the physician-patient relationship, as these family practice patients had access to the same primary care physician who managed their care. These patients may have developed relationships with their physician unlike emergency department or inpatient staff.
While minor stress accounted for a significant amount of variance in outpatient utilization, this relationship was relatively modest. However, previous research has found only a modest amount of variance in utilization accounted for by major life stress (Miranda et al., 1991) and by more comprehensive models of utilization (Aday and Awe, 1997; Wolinsky, 1978). In the current study, variables such as age and number of chronic illnesses accounted for only 15% of the variance in utilization. Thus, the 3–4% increase in explained variance accounted for by minor life events may be more important when considered in this context.
Since past research has uncovered a relationship between major life events and utilization, it is important to consider why no such relationship was found. Few studies have examined the relationship between utilization and stress in African American samples, and the effects of major stress that have been found with other populations may not be as pronounced in low-income, minority groups. Theories of medical utilization propose cultural factors as well as financial resources are significant contributors in utilization (Aday and Awe, 1997), providing further support for this argument. Also, this sample had a high level of chronic illness (i.e., over 40% had three or more chronic conditions), and the management of these chronic illnesses may have required more routine medical visits, which could have suppressed the effects of stress on utilization.
In summary, current results suggest minor life stress is modestly predictive of outpatient visits among predominantly low-income, ethnic minority patients. Since stress management techniques typically target patients' ability to cope with minor life events, this relationship highlights the possibility of implementing stress management procedures to reduce utilization rates. Further study is needed to determine if stress management strategies can positively influence utilization, determine which patients receive the most benefit from such strategies, and examine the cost utility of such procedures for utilization.
Notes
Examining the plots of the distributions raised questions about the normality of the utilization data distributions and residuals. The utilization data can be considered as count data, and indeed the plots were suggestive of an over-dispersed Poisson distribution. The analyses were repeated using the generalized model for Poisson regression (SAS v8 Proc GenMod). As all the results remained substantially the same, the more easily interpretable regression results are presented here.
REFERENCES
Aday, L. A., and Awe, W. C. (1997). Health services utilization models. In Gochman, D. S. (Ed.), Handbook of Health Behavior Research I: Personal and Social Determinants. Plenum: New York, pp. 153–172.
Aikens, J. E., Wallander, J. L., Bell, D. S., and Cole, J. A. (1992). Daily stress variability, learned resourcefulness, regimen adherence, and metabolic control in Type I diabetes mellitus. J. Consult. Clin. Psychol. 60: 113–118.
Anderson, R., and Newman, J. F. (1973). Societal and individual determinants of medical care utilization in the United States. Milbank Memorial Fund Quarterly: Health and Society 51: 95–124.
Barsky, A. J., Ahern, D. K., Bailey, E. D., and Delamater, B. A. (1996). Predictors of persistent palpitations and continued medical utilization. J. Fam. Pract. 42: 465–472.
Benedittis, G. D., and Lorenzetti, A. (1992). The role of stressful life events in the persistence of primary headache: Major events vs. daily hassles. Pain 51: 35–42.
Brantley, P. J., and Ames, S. C. (2001). Psychobiology of Health and Disease. In Sutker, P. B., and Adams, H. E. (Eds.), Comprehensive Handbook of Psychopathology. Plenum: New York, pp. 777–795.
Brantley, P. J., Jones, G. N., Boudreaux, E., and Catz, S. (1997). Weekly stress inventory. In Zalaquett C. P., and Wood R. J. (Eds.). Evaluating Stress: A Book of Resources. Scarecrow: Lanham. MD, pp. 405–420.
Brosschot, J. F., Benschop, R. J., Godaert, G., Olff, M., Smet, M., Heijnen, C. J., and Ballieux, R. E. (1994). Influence of life stress on immunological reactivity to mild psychological stress. Psychosom. Med. 56: 216–224.
Cohen, S., Tyrrell, D., and Smith, A. P. (1991). Psychological stress and susceptibility to the common cold. N. Engl. J. Med. 325: 606–612.
Fernande, E., and Sheffield, J. (1996). Relative contributions of life events versus daily hassles to the frequency and intensity of headaches. Headache 36: 595–602.
Garrett, V. D., Brantley, P. J., Jones, G. N., and McKnight, G. T. (1991). The relation between daily stress and Crohn's disease. J. Behav. Med. 14: 87–96.
Gortmaker, S. L., Eckenrode, J., and Gore, S. (1982). Stress and the utilization of health services: A time series and cross-sectional analysis. J. Health Soc. Behav. 2: 24–38.
Hitchcock, P. B., Brantley, P. J., Jones, G. N., and McKnight, G. T. (1990). Stress and social support as predictors of dietary compliance in hemodialysis patients. Behav. Med. 18: 13–20.
Kanner, A. D., Coyne, J. C., Schaefer, C., and Lazarus, R. S. (1981). Comparison of two modes of stress measurement: Daily hassles and uplifts versus major life events. J. Behav. Med. 4: 1–39.
Kramer, J. R., Ledolter, J., Manos, G. N., and Bayless, M. L. (2000). Stress and metabolic control in diabetes mellitus: Methodological issues and an illustrative analysis. Ann. Behav. Med. 22: 17–28.
Krause, N. (1988). Stressful life events and physician utilization. J. Gerontol. 43: 53–61.
Lazarus, R. S. (1984). Puzzles in the study of daily hassles. J. Behav. Med. 7: 375–389.
Lazarus, R. S., and Folkman, S. (1984). Stress, Appraisal, and Coping. Springer, New York.
Lindquist, T. L., Beilin, L. J., and Knuiman, M. W. (1997). Influence of lifestyle, coping, and job stress on blood pressure in men and women. Hypertension 29: 1–7.
Mechanic, D. (1979). Correlates of physician utilization: Why do major multivariate studies of physician utilization find trivial psychosocial and organizational effects? J. Health Soc. Behav. 20: 387–396.
Mechanic, D., and Volkart, E. H. (1961). Stress, illness behavior, and the sick role. Am. Socio. Rev. 26: 51–58.
Miranda, J., Perez-Stable, E. J., Munoz, R. F., Hargreaves, W., and Henke, C. J. (1991). Somatization, psychiatric disorder, and stress in utilization of ambulatory medical services. Health Psychol. 10: 46–51.
National Center for Health Statistics. (2001). Urban and Rural Health Chartbook: Health, United States. Hyattsville, MD.
Ogden, J., and Mtandabari, T. (1997). Examination stress and changes in mood and health related behaviors. Psychol. and Health 12: 289–299.
Pilisuk, M., Boylan, R., and Acredolo, C. (1987). Social support, life stress, and subsequent medical care utilization. Health Psychol. 6: 273–288.
Roghmann, K. J., and Haggerty, R. J. (1973). Daily stress, illness, and use of health services in young families. Pediatr. Res. 7: 520–526.
Ruffin, C. L. (1993). Stress and health: Little hassles vs. major life events. Aust. Psychol. 28: 201–208.
Sarason, I. G., Johnson, J. H., and Siegel, J. M. (1978). Assessing the impact of life changes: Development of the Life Experiences Survey. J. Consult. Clin. Psychol. 46: 932–946.
Scarinci, I. C., Ames, S. C., and Brantley, P. J. (1999). Chronic minor stressors and major life events experienced by low-income patients attending primary care clinics: A longitudinal examination. J. Behav. Med. 22: 143–156.
Searle, A., and Bennett, P. (2001). Psychological factors and inflammatory bowel disease: A review of a decade of literature. Psychol. Health, and Med. 6: 121–135.
Stetson, B. A., Rahn, J. M., Dubbert, P. M., Wilner, B. I., and Mercury, M. G. (1997). Prospective evaluation of the effects of stress on exercise adherence in community-residing women. Health Psychol. 16: 515–520.
Tessler, R., Mechanic, D., and Dimond, M. (1976). The effect of psychological distress on physician utilization: A prospective study. J. Health Soc. Behav. 17: 353–364.
Theorell, T., and Emlund, N. (1993). On physiological effects of positive and negative life changes—A longitudinal study. J. Psychosom. Res. 37: 653–659.
Thomason, B. T., Brantley, P. J., Jones, G. N., Dyer, H. R., and Morris, J. L. (1992). The relation between stress and disease activity in rheumatoid arthritis. J. Behav. Med. 5: 215–220.
Turner-Cobb, J. M., and Steptoe, A. (1996). Psychosocial stress and susceptibility to upper respiratory tract illness in an adult population sample. Psychosom. Med. 58: 404–412.
Twisk, J., Snel, J., Kemper, H., and Van Mechelen, W. (1999). Changes in daily hassles and life events and the relationship with coronary heart disease risk factors: A 2-year longitudinal study in 27–29-year-old males and females. J. Psychosom. Res. 46: 229–240.
Williams, R., Zyzanski, S. J., and Wright, A. L. (1992). Life events and daily hassles and uplifts as predictors of hospitalization and outpatient visits. Soc. Sci. Med. 34: 763–768.
Wolinsky, F. D. (1978). Assessing the effects of predisposing, enabling, and illness-morbidity characteristics on health service utilization. J. Health Soc. Behav. 19: 384–396.
ACKNOWLEDGMENTS
This study was funded by a grant (RO1MH51194) from the National Institute of Mental Health (NIMH). We would like to thank Steve Ames, Brad Applegate, Melanie Boyce, Shawn Jeffries, Daniel Mehan, and Isabel Scarinci for assistance in data collection.
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Brantley, P.J., Dutton, G.R., Grothe, K.B. et al. Minor Life Events as Predictors of Medical Utilization in Low Income African American Family Practice Patients. J Behav Med 28, 395–401 (2005). https://doi.org/10.1007/s10865-005-9001-z
Published:
Issue Date:
DOI: https://doi.org/10.1007/s10865-005-9001-z