Abstract
The disadvantages of human amniotic membrane (hAM), used for ocular surface reconstruction, necessitate the development of standardized alternatives. Keratin-derived-films (KF) have been indicated as transferable substrate for cell cultivation and tissue engineering. The impact of different sterilization procedures on KF and surgical feasibility were investigated. Human hair KF were prepared and sterilized; optical, biomechanical properties, in vitro cell seeding efficiency and proliferation of human corneal epithelial cells were studied and compared with hAM. Surgical feasibility was tested on enucleated porcine eye. Sterilized KF showed higher light transmission and significantly higher E-modulus than hAM; cell-seeding-efficiency and proliferation rate were not affected. Although KF could be surgically handled, suture placement was more difficult compared to hAM. Plasma treatment seems the best sterilization method for KF; it does not affect cell biology or optical and biomechanical properties. However material modifications are requested before KF may represent a feasible alternative for ocular surface reconstruction.
Similar content being viewed by others
Explore related subjects
Discover the latest articles, news and stories from top researchers in related subjects.Avoid common mistakes on your manuscript.
1 Introduction
Cornea-related blindness affects millions of people world-wide. Congenital, degenerative, nutrient, neoplastic and immunological disorders, as well as trauma, can lead to ocular surface breakdown, resulting in temporary discomfort, superficial punctate keratopathy and permanent loss of corneal transparency and vision. Primary ocular surface diseases (OSD) include Stevens Johnson syndrome, ocular mucous membrane pemphigoid, graft versus host disease and chemical burns. Secondary OSD can result from lid anomalies, severe dry eye or neurotrophic disease. Since medical therapy often fails, surgical methods, such as corneal or human amniotic membrane (hAM) transplantation, are currently used to stabilize the ocular surface [1]. In particular, hAM transplantation has been found to be effective in the treatment of corneal ulcers [2–8] and as a substrate to expand limbal epithelial cells and transfer them as a graft to restore the ocular surface in cases of limbal stem cell deficiency [9–11]. Transmission of systemic disease with graft material is in principle possible although rare. In fact—to the best of our knowledge—no such transmission has been reported for transplantation of stored hAM so far. Such tissue routinely undergoes quality controls including HIV, hepatitis B, C and HTLV tests of donor serum at the time of harvesting the membrane and often 6 months later again to exclude late seroconversion of donors. However, as reported by Eberle et al. [12] samples of fresh donor material, in this case a single droplet of serum, can transmit serious disease such as HIV and fresh unpreserved hAM is also used quite commonly in the developing world and is certainly associated with a higher risk of disease transmission [13–15]. Unfortunately, preservation processes have been also responsible for hAM morphology and biochemical composition change. Cryopreserved hAM presents epithelial vacuolar degeneration and stromal edema [16, 17], while lyophilized hAM is thinner but also shows epithelial vacuolar degeneration and flattening of the epithelial surface [18]. It is well known that hAM has limited transparency, reduced biomechanical resistance [19] and carries a risk of infection. Moreover, its characteristics, such as thickness and composition, have interdonor and intradonor variations [14, 18, 20–23].
Keratins belong to the group of structural proteins that are formed in the epithelial cells of higher vertebrates. These cysteine-rich proteins can be found in hard or filamentous structures, such as hair, nails, horns, hoofs or feathers. They exhibit high mechanical strength due to a large number of disulfide bonds and are water-insoluble. In general, chemical reduction of the disulfide bonds is needed to obtain water-soluble proteins that can be used directly or after further chemical modifications, such as methylation or oxidation, which results in variable product properties [24, 25]. Although other groups have reported human hair keratin (KF) as an option for regenerative medicine [26–31] its successful use as a transferable substrate for corneal epithelial cells has been recently reported by our group [32]. These films were made by mixing aqueous keratin dialysate, which contains keratinous nanoparticles, and alkaline keratin dialysate. The transparent KF possessed a higher light transmission than hAM and showed similar substrate properties to human corneal epithelial cells, as compared to hAM. The biomechanical properties of KF could be adjusted and optimized by varying process parameters, such as keratin dialysate composition, content of the softening agent (glycerol) and curing temperature and duration.
Prior to bringing the KF from the in vitro state to animal testing, a standardized sterilization procedure is required, as well as an understanding of their suturability using routine ophthalmological surgical suture material. The aim of this study was to investigate the impacts of various sterilization methods on the optical and biomechanical properties of the KF as well as the cell proliferation behavior. In addition, the feasibility of suturing KF was studied in a porcine ex vivo model to find the optimized KF for subsequent animal studies.
2 Methods
2.1 Materials
Sodium dodecyl sulfate (SDS), urea, thiourea, 2-amino-2-hydroxymethyl-propane-1,3-diol (Tris), sodium hydroxide and 2-mercaptoethanol were purchased from Roth (Karlsruhe, Germany). Dulbecco’s modified Eagle’s medium (DMEM), Ham’s F12 medium, fetal calf serum (FCS), insulin, and epidermal growth factor (EGF) were obtained from Biochrom (Berlin, Germany). Phosphate-buffered saline (PBS) was purchased from MP Biomedicals (Solon, US). Dimethyl sulfoxide (DMSO) and glycerol were obtained from Sigma (Deisenhofen, Germany). The trypsin–EDTA, an antibiotic/antimycotic solution and MycoTrace kit were obtained from PAA (Linz, Austria). Spectra/Por® 1 dialysis membrane (MWCO 6–8,000 Da) was purchased from Spectrum (Rancho Dominguez, US). Tissue culture flasks and polystyrene 24-well cell culture plates were obtained from TPP (Trasadingen, Switzerland). Vivaspin® was purchased from Sartorius (Goettingen, Germany), and polyethylene terephthalate (PET) foil was obtained from LTS Lohmann (Andernach, Germany). PureVision™ soft contact lenses were obtained from Bausch&Lomb (Rochester, New York, US), and PrecisionUV® soft contact lenses were obtained from CIBA Vision (Duluth, Minnesota, US). Monofil 10–0 polyamide suture material Ethilon™ (Ethicon™) was purchased from Johnson & Johnson (Norderstedt, Germany). All other chemicals were of analytical grade. All solutions were formulated using double-distilled water.
The method for securing human tissue was performed according to the tenets of the Declaration of Helsinki. Samples of human amniotic membrane were obtained at the time of an elective caesarean section. Intact amnion was stripped from the chorion by blunt dissection and sutured onto 7.5 × 7.5 cm sterile sponge sheets (Katena, New Jersey, US). All operations were performed under sterile conditions. The hAM was cryopreserved at −80 °C in a mixture of 50 % DMEM and 50 % glycerol [7]. This method of preservation is reported in almost 95 % of the current literature on utilizing hAM for ocular surface reconstruction [33] and, based on the results of recent studies, it has been demonstrated that long-term storage of hAM in cell culture media with 50 % glycerol does not significantly impair its sterility, histology, or biological properties [34] and that it is preferable over lyophilization which seems to cause greater reduction in total protein amount and growth factor concentration [18]. Porcine eyes were obtained from a local slaughterhouse. They were removed within 30 min of death, transported in physiologic sodium chloride solution and used within 24 h for the suture studies.
2.2 Keratin film preparation
Human hair keratin was extracted as described by Nakamura et al. [35], and the KF were prepared according to a method previously reported by Reichl et al. [32]. Briefly, hair was mixed with an extraction medium, which is an aqueous solution (pH 8.5) containing 25 mM Tris, 2.6 M thiourea, 5 M urea and 5 % 2-mercaptoethanol, and was incubated at 50 °C for 72 h. The mixture was centrifuged and the supernatant was filtered using filter paper with a pore size of 2.5 μm. The filtrate, termed “Shindai extract”, was immediately used or stored at −20 °C and thawed prior to use. The Shindai extract was exhaustively dialyzed against water using a MWCO 6–8,000 Da cellulose membrane at 20 °C. The keratin dialysate, termed “aqueous keratin dialysate,” was centrifuged to remove coarse aggregates and immediately used to prepare the KF. In another phase of dialysis, the same amount of Shindai extract was dialyzed against 0.25 M sodium hydroxide solution in the same manner as described above, at 4 °C. This dialysate was concentrated via ultrafiltration using Vivaspin® 20 concentrators with a MWCO of 5,000 Da. The filtrates were discarded and the supernatant was diluted several times with 0.05 μM NaOH to generate the alkaline keratin dialysate.
KF were prepared by mixing the aqueous keratin dialysate with portions of alkaline keratin dialysate (at ratios of 100, 90/10 and 80/20, respectively; e.g., a 90/10 film consists of 90 % aqueous and 10 % alkaline keratin dialysate). Glycerol was added at a concentration of 1 % as a softening agent. Thereafter, the keratin dialysate mixture was cast on hydrophobic coated PET sheets and allowed to dry overnight in air. Biomechanically stable films were achieved by performing a subsequent curing procedure that involves dry heat. By varying the curing temperature, the mechanical properties of the film can be adjusted. In general, the films were cured at 110 °C for 2 h. All film preparation steps were performed under aseptic conditions.
2.3 Sterilization methods
To study the possible influence of sterilization on the material properties, KF were treated by three different sterilization procedures. For these experiments, KF 100 cured at 110 °C for 2 h were used. KF were sterilized by incubation in 70 % ethanol for 2 h, by steam sterilization in PBS at 121 °C for 15 min or by plasma sterilization of dry KF using H2O2 in a Sterrad® 100S plasma sterilizer (ASP, Irvine, California, US). The success of these methods was evaluated by sterility testing.
2.4 In vitro assessment of sterilized keratin films
2.4.1 Light transmission
Total light transmission of KF 100 samples (untreated; 70 % ethanol-treated, plasma-sterilized and autoclaved) was measured using a spectrophotometer (UV multi-plate reader Powerwave XS, Biotek) with a wavelength rage from 300 to 800 nm. After 24 h of water equilibration, the specimens were clamped within a self-constructed two-ring arrangement of suitable size in order to fix the films during the experiment and provide a standardized area (0.332 cm²) of exposure (Fig. 1). The samples were positioned in a 24-well plate containing 1 mL of water per well. The extinction was measured and the light transmission was calculated. The measurements were performed with a resolution of 1 nm and a blank correction. Two types of therapeutic soft contact lenses (Bausch&Lomb PureVision™ BC 8.6 PWR 0.00 and Ciba Vision PrecisionUV® BC 8.7 PWR 0.00) and hAM samples served as references.
2.4.2 Tensile testing
The biomechanical properties of KF both untreated and after sterilization, were examined by means of a Zwicki-Line Z 0.5 static material testing machine (Zwick, Ulm, Germany) with a 10 N load. KF 100 and 90/10 samples were incubated in water for 24 h and punched out using an S3 film cutting device (Zwick) to yield standardized (35 mm) dumbbell specimens. The measurements were conducted with a test speed of 1 mm/min for E-modulus (Young’s modulus) determination and 5 mm/min for tensile strength testing. Both, E-Modulus (EM) and ultimate strength (US) values were calculated from the stress–strain curves obtained using the testXpert® II software.
2.4.3 Cell culture
The SV40-immortalized human corneal epithelial cell line HCE-T was obtained from the RIKEN cell bank (Tsukuba, Japan) and used to study the substrate properties of sterilized KF. This cell line was introduced by Araki-Sasaki et al. [36]. The cells were cultivated in 1:1 DMEM/Ham’s F12 medium supplemented with 5 % FCS, 5 μg/mL insulin, 10 ng/mL EGF, 0.5 % DMSO and 1 % antibiotic/antimycotic solution in 25 cm2 tissue culture flasks at 37 °C in a humidified atmosphere containing 5 % CO2 as recommend by the providing cell bank. The growth medium was replaced three times per week. The absence of mycoplasma contamination was confirmed by PCR (MycoTrace). Before starting the cell culture experiments, the KF were intensively washed in sterile water, which was replaced twice daily for seven days. An even growth area and fixation of the substrate on the bottom of the cell culture well were achieved by punching out KF in circles (diameter 11 mm) and clamping of the circles within the same two-ring arrangement as described in 2.4.1 (Fig. 1). Before cell seeding, the KF were equilibrated in growth medium for 6 h.
2.4.4 Seeding efficiency
In order to evaluate the seeding efficiency, the cells (150,000 cells/cm²) were seeded and incubated for 10 h. After rinsing with PBS and detaching the cells by a trypsin–EDTA-procedure, the cells were counted using a Z2 Coulter counter (Beckman Coulter, Krefeld, Germany). The seeding efficiency was calculated by dividing the number of cells attached by the number of cells that were seeded. The measurements were performed in triplicate.
2.4.5 Proliferation studies
Proliferation studies were performed in polystyrene 24-well plates using HCE-T cells. Cells were seeded at a density of 30,000 cells/cm² and incubated for 14 days. At fixed time intervals, cells were detached using trypsin–EDTA and counted as described above. The number of cells (mean ± standard deviation; n = 3 wells) was semi-log plotted against culture time. The culture growth parameters (lag time, population doubling time (PDT), saturation density) were calculated from the sigmoidal proliferation curves.
2.5 Suture experiments
2.5.1 In vitro suture tear-out
The material testing machine described in 2.4.2 was used for the in vitro suture tear-out experiments. In this set-up, KF and hAM were punched in standard 12 mm diameter disc specimens and equilibrated in water for 24 h. A 10–0 polyamide suture with a tape pointed needle was passed through the geometrical center of the samples. The test material was clamped with the lower third of the sample in the lower clamping jaw, while the suture was fixed in the upper clamping jaw. The test speed for suture tear-out force testing was set at 5 mm/min. The maximum force (Fmax) that was required to pull out the suture from the center to the periphery was determined. Six samples each of unsterilized KF 100 and 90/10 containing 1 % glycerol and cured for 2 h at temperatures ranging from 70 to 110 °C were tested to assess the impact of curing temperature on film stability during the suture procedure. Furthermore, KF 100, which was prepared under standard conditions (110 °C, 2 h), was tested as an untreated sample as well as after sterilization.
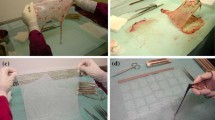
2.5.2 Ex vivo surgical assessment
The surgical feasibility of KF was assessed by seven surgeons, who were asked to suture the films onto enucleated porcine eyes. All procedures were performed under a microscope (Zeiss, Oberkochen, Germany). Porcine eyes were placed on a specially designed, self-constructed plastic material support, and intraocular pressure set to 20 mm Hg by connecting the globe via a cannula with a bottle of saline solution placed at a 100 cm height from the working plane. The ocular surface and KF were kept wet with a second cannula fixed 15 cm above the globe and delivery of three drops of saline solution per minute. A 7.5 mm diameter superficial keratectomy of approximately 100–200 μm in depth was manually performed on all eyes by the same surgeon before the remaining participating surgeons sutured the 8 mm diameter implants into the defects with 8 radial single polyamide 10–0 sutures.
Each surgeon first sutured one human amniotic membrane specimen and then seven samples of KF 90/10 cured at 100 °C for 2 h. This composition of film was chosen because films containing a higher content of alkaline dialysate were found to be too soft and unable to be sutured or handled during the suture tear-out force measurements and KF 100 was found be too stiff and to break easily. Once each transplant had been fixed with eight sutures, digital photographs were taken through the microscope using a standard setting. The percentage of tight sutures, “small tears”, which were defined as a small linear break within the implant, “tears including margin”, which were defined as large linear breaks extending to the margin of the implant, “small breaks”, which were defined as <1/4 of the implant missing and the percentage of “large breaks”, which were defined as ≥1/4 of implant missing, were registered. Furthermore, the time per KF needed for suturing was determined.
A subgroup of three surgeons repeated the experiment in similar settings by suturing KF 90/10 (100 °C, 2 h) that had undergone different methods of sterilization. For each subgroup of films, the surgeon was requested to suture five samples.
2.6 Statistical analysis
All experimental data were evaluated using MS Excel 2007. The ANOVA test was used to test for a significant difference within the subgroups, while a t test with Bonferroni correction was used to test for a significant difference between subgroups. Values of P < 0.05 were considered statistically significant.
3 Results
3.1 In vitro studies
KF exhibit distinctly higher transparency than the amniotic membrane as shown in Fig. 1. The optical impression was confirmed by the results of light transmission experiments, which are shown in Fig. 2. As expected, light transmission was nearly 100 % between 400 and 800 nm for both therapeutic contact lenses. On the contrary, hAM transmitted only approximately 35 % of the light at 400 nm and approximately 70 % of the light at 800 nm. The light transmission for untreated KF 100 samples was considerably higher, with values at approximately 80 % at 400 nm, 90 % at 500 nm and 97 % at 800 nm. The sterilization methods showed only small influences on KF light transmission. After ethanol treatment, light transmission was only marginally altered compared to untreated films, and autoclaving reduced the light transmission slightly, most notably in the wavelength range of 300–600 nm. In contrast, plasma-sterilized films showed higher light transmission than untreated films at wavelengths between 300 and 700 nm, while light transmission at wavelengths between 700 and 800 nm was comparable for plasma-sterilized films and untreated KF.
The impact of sterilization on the biomechanical properties (i.e., ultimate strength (US) and E-modulus (EM)) of KF 100 and 90/10 was tested in comparison to untreated films and hAM (Figs. 3 and 4). As observed in a previous study of untreated KF [32], the values for EM and US decreased with an increasing level of alkaline dialysate. This effect can also be detected with sterilized films. No significant changes of US were observed for sterilized KF compared to untreated films in either KF 100 or KF 90. A trend towards higher tensile strength of KF after ethanol treatment was detected (P = 0.19), whereas plasma-sterilized and autoclaved films remained unaffected (P = 0.14 and P = 0.29, respectively). Compared to hAM, the US of KF 100 untreated or sterilized and KF 90/10 ethanol-treated were in the same range, while KF 90/10 untreated and plasma or autoclaved showed reduced US values. The E-modulus of KF was affected by the sterilization procedures. While the autoclaving process influenced EM only marginally, the ethanol treatment resulted in higher values and made the films stiffer. On the other hand, plasma sterilization reduced the EM compared to untreated films, resulting in softer films. Compared to hAM, KF 100, untreated or sterilized, exhibited considerably higher EM values. However, KF 90/10 especially when plasma sterilized, had an EM values which were in the range of hAM.
Ultimate strength of KF 100 and 90/10, respectively, untreated and having undergone ethanol treatment, plasma and steam sterilization (autoclaving) as well as amniotic membrane, mean ± SD, n = 8–13. * From Ref. [32]
E-Modulus of KF 100 and 90/10, respectively, untreated or having undergone ethanol treatment or plasma and steam sterilization (autoclaving) as well as amniotic membrane, mean ± SD, n = 8–13. * From ref. [32]
The seeding efficiency of HCE-T cells on untreated KF 100 was found to be 63.8 % [32] (Table 1). Ethanol treatment and autoclaving did not alter the seeding efficiency significantly (P = 0.93 and P = 0.55, respectively). After plasma sterilization seeding efficiency was 86 % which was not different as with hAM [32] (P = 0.9). HCE-T cells exhibited a slightly extended lag-phase after seeding on keratin substrates in comparison to hAM, especially in the case of ethanol-treated KF, whereas the lag-phase of autoclaved and plasma-sterilized KF did not differ from untreated films. The population doubling times of HCE-T cells on KF were in the same range as reported for hAM [32], only autoclaved films showed a prolonged PDT. Autoclaving and plasma sterilization did not affect the saturation density of HCE-T cells on the substrates. Only ethanol treatment resulted in a threefold decrease of saturation density compared to untreated KF or hAM.
3.2 Suture experiments
The impact of the curing temperature (70–110 °C, 2 h) on KF material properties, regarding the resistance against suture tear-out, was tested in vitro and compared with the hAM to evaluate the best KF for further ex vivo and animal studies (Fig. 5). The mean tear-out force (Fmax) measured for hAM was 0.26 N. At different curing temperatures, Fmax values ranged between 0.02 N (70 °C) and 0.33 N (110 °C) for KF 100 and between 0.02 N and 0.1 N for KF 90/10. In KF 100, an increase in curing temperature was associated with an increase in suture tear-out force, while KF 90/10 showed no relationship between Fmax and curing temperature. In general, KF obtained at 70 °C appeared to be too soft for both KF 90/10 and KF 100. The statistical analysis showed a significant difference within both KF 100 and KF 90/10 groups for various curing temperature. In addition, statistically significant differences were found between KF 100 cured at 70 °C and KF 100 cured at temperatures between 80 and 110 °C (P < 0.005) and between KF 90/10 cured at 70 and 100 °C (P < 0.005). Compared with hAM, KF 90/10 showed significantly lower resistance against tear-out over the entire temperature range (P < 0.005). KF 100 were significantly weaker than the hAM at 70 °C (P < 0.005). Figure 6 depicts the suture tear-out experiment, including sterilized specimens. The average Fmax values of ethanol-treated and autoclaved KF 100 samples were marginally reduced compared to untreated films, and were in the same range as those of the hAM. Only the plasma-sterilized KF exhibited a significant reduction in Fmax.
KF 100 seemed to be the material of choice for further ex vivo suturing experiments, however when fitting the films to the corneal surface of porcine eyes we invariably found that KF 100 did not mould into shape with the recipient but showed stiff, wave like dehiscence in its peripheral circumference. In contrast KF 90/10 could easily fit the recipient corneal curvature.
Hence the latter construct was used for further surgical assessment of KF in particular we choose sample cured at 100 °C for 2 h. In all cases, the surgeons were able to place eight single sutures as requested (Fig. 7). The mean time needed to suture a KF (16.7 ± 1.3 min) was not significantly longer than the time needed to suture an amniotic membrane (13.7 ± 3.5 min) (P = 0.27). There was a trend for shorter surgical time from the first (20.3 ± 6.7 min) to the final KF (16.1 ± 3.7 min), which was not significant (P = 0.15) (Fig. 7a). More importantly, the percentage of tight sutures securing the implant to the corneal tissue was invariably and substantially higher for hAM (100 ± 0 %) compared to KF (58 ± 28 %; P = 0.0002; Fig. 7b). Again, the percentage of tight sutures tended to improve from the first (48.2 %) to the seventh KF (62.5 %); however, this difference did not reach statistical significance (P = 0.44). Finally, we did not detect any small tears or tears including the margin within hAM. On KF, these defects were encountered in 65 % (P = 0.002 compared to hAM) and 12 % (P = 0.2 compared to hAM) of the cases, respectively (Fig. 7c, d). Neither small nor large breaks were detected for hAM or KF, respectively. None of the KF sterilization methods used in this study significantly altered the results of fixation with interrupted sutures (P = 0.8, data not shown), although the surgeons subjectively described plasma-sterilized films as softer and ethanol-treated films as harder than untreated KF.
Ex vivo surgical assessment of KF relative to AM. The experiments were performed by seven different surgeons on seven independent KF samples (KF 90/10 cured at 100 °C for 2 h) and amniotic membrane, mean ± SD. a The average time needed to suture the AM and KF onto an enucleated porcine eye. The time registered to suture the AM was shorter than that needed for the other KF, but the difference was statistically significant only when comparing the AM to the first KF (P = 0.02). b The percentage of tight sutures on the AM and KF; the difference between AM and KF was statistically significant. c, d The percentages of small tears and tears including margin, respectively, occurring on both the AM and KF. Small tears were registered statistically significantly more often on KF than on AM. On the contrary, tears including margin, even if more recurrent on KF than on AM, were not statistically higher compared to AM
4 Discussion
Over the last decade, some films and scaffolds based on keratin have been proposed as a new biomaterial for cell culture and tissue engineering applications [26, 37–42]. A novel technology allowed for the preparation of stable and transparent films that represent an excellent growth substrate for corneal epithelial cells [32]. Due to the light transmission of KF being comparable to that of contact lenses, the tensile strength of KF being potentially higher than that of hAM and the possibility to cultivate corneal epithelial cells on KF, it was suggested as an alternative to amniotic membrane for ocular surface reconstruction [32]. The presented study evaluated appropriate sterilization methods and their impact on optical, biomechanical and cell culture properties in comparison to untreated films and hAM, as a further step towards the use of KF in animal studies and clinical application of KF. In addition, it includes the first ex vivo experiments investigating the surgical feasibility of this material. One limitation of our study is the limited number of samples available for testing of tear-out (n = 6) and the surgical feasibility (n = 7) that together with tissue variation is likely to result in the substantial standard deviation.
Clinically, the most important limitation to hAM transplantation is the membrane’s poor transparency, although it has been established that the amniotic sac distal to the placenta offers the greatest transparency [43]. Freeze-dried and rehydrated hAM provides an increased level of transparency over a freeze–thaw method of preservation. For clinically applied cryopreserved hAM, light transmission values are 60–70 % for wavelengths in the range of 400–700 nm [43 42]. These values are similar to our data for hAM and are distinctly lower than those measured for untreated or sterilized KF 100. The KF showed light transmission values ranging between 65 and 97 % at 400–700 nm, indicating that these films are considerably more transparent than hAM. The ethanol treatment and plasma sterilization methods seem to have only a marginal effect on light transmission, likely because they work at low temperatures, and they did not result in ultrastructural changes of the film. On the other hand, autoclaving led to decreased transparency, which could be explained by the higher temperature and possible subsequent protein denaturation, which would reduce light transmission. However, even after steam sterilization, light transmission is still considerably higher than for hAM. In contrast, the biomechanical properties of KF remained unaffected by steam sterilization. Ethanol treatment resulted in stiffening and reduced elasticity of the films. A similar effect has been reported for silk protein films [44]. This finding is not surprising given that ethanol leads to structural protein alteration by dehydration, making it widely used in tissue fixation procedures for histological studies. Plasma sterilization resulted in a slight but insignificant decrease in tensile strength and a more pronounced decrease in the E-modulus. Plasma sterilization is able to chemically modify protein, which could reduce some of the bonding forces within the KF, making the material more elastic. Compared to hAM, KF 100 showed an equal ultimate strength and KF 90/10 showed a reduced ultimate strength. The EM of KF was markedly higher than that detected for hAM, with the exception of plasma-sterilized KF 90/10, which was found to have similar elasticity as hAM after plasma sterilization.
Our results obtained with an immortalized corneal epithelial cell line (HCE-T) demonstrate that the sterilization methods did not significantly alter the cell seeding efficiency. While ethanol-treated and autoclaved KF showed the same seeding efficiency as untreated KF, which is lower than that detected for hAM [32], plasma sterilization resulted in an improved seeding efficiency of KF, which was similar to that of hAM. Plasma treatment led to enhanced epithelial cell attachment to the keratin surface, which can be explained by surface modification through enhanced surface hydrophilicity and roughness. The same effect has been observed by Rafat et al. [45]. The investigators detected improved attachment of corneal epithelial cells on an argon plasma-treated collagen-based artificial cornea in comparison to untreated substrate [45]. Regarding corneal cell proliferation, plasma-sterilized KF possessed the same behavior as untreated films, while ethanol treatment and steam sterilization resulted in some alterations. Moreover, the HCE-T cells exhibited markedly reduced proliferation on ethanol-treated KF. In summary, the in vitro experiments indicate that plasma treatment is the best sterilization method for KF because it did not negatively impact light transmission, cell attachment or proliferation. The decreased ultimate strength and E-modulus observed for plasma-sterilized KF were within acceptable ranges. On the contrary, autoclaving and ethanol treatment slightly reduced the light transmission or increased the film stiffness and reduced cell proliferation.
The in vitro suture experiments confirmed the previous results of tensile strength testing [32], which indicated that tensile strength and stiffness are dependent upon the content of alkaline dialysate in the KF and the curing temperature. Hence, KF 90/10 exhibited a low tear-out force (Fmax), even with an increasing curing temperature, when compared to KF 100 and hAM. However, a partial alkaline keratin dialysate composition seemed to provide the KF with more elasticity [32]. The ex vivo pilot use of KF 100 confirmed that it did not adapt well to the corneal curvature because of its inherent stiffness. KF 80/20 was better adapted to the corneal curvature, but it was too soft to be suitable for sutures, which is in agreement with the low Fmax values. Therefore, an ex vivo surgical feasibility assessment was conducted with KF 90/10 cured at 100 °C for 2 h. The surgical assessment showed that the KF can be sutured into a corneal defect by surgeons with variable experience in a time that was clinically but not statistically different from hAM. The use of a pointed needle rather than a spatula needle tears KF more easily than it tears hAM, and hence it seems to be less elastic. The high rate of loose sutures in KF should be of concern given that loose sutures in vivo would result in poor adaptation of the membrane to the surface and may cause irritation and corneal neovascularization. Hence, material modification to increase elasticity or alternative surgical techniques, such as suture-free implantation, should be considered for further in vivo evaluations.
5 Conclusion
Keratin films from human hair have been reported to support the growth of corneal epithelial cells in vitro. Our data show that this material can be plasma sterilized with no negative impact on light transmission, cell attachment or proliferation. The decreased ultimate strength and E-modulus observed for plasma-sterilized KF were within acceptable ranges. However the difficulties observed with suture placement and surgical tissues adaptation could in vivo lead to irritation and corneal neovascularization. If these could be overcome by material modifications KF could offer a promising alternative for ocular surface reconstruction.
References
Dua HS, Gomes JA, King AJ, Maharajan VS. The amniotic membrane in ophthalmology. Surv Ophthalmol. 2004;49:51–77.
Lee SH, Tseng SC. Amniotic membrane transplantation for persistent epithelial defects with ulceration. Am J Ophthalmol. 1997;123:303–12.
Chen HJ, Pires RT, Tseng SC. Amniotic membrane transplantation for severe neurotrophic corneal ulcers. Br J Ophthalmol. 2000;84:826–33.
Hanada K, Shimazaki J, Shimmura S, Tsubota K. Multilayered amniotic membrane transplantation for severe ulceration of the cornea and sclera. Am J Ophthalmol. 2001;131:324–31.
Rodríguez-Ares MT, Touriño R, López-Valladares MJ, Gude F. Multilayer amniotic membrane transplantation in the treatment of corneal perforations. Cornea. 2004;23:577–83.
Tsubota K, Satake Y, Ohyama M, et al. Surgical reconstruction of the ocular surface in advanced ocular cicatricial pemphigoid and Stevens–Johnson syndrome. Am J Ophthalmol. 1996;122:38–52.
Tseng SC, Prabhasawat P, Lee SH. Amniotic membrane transplantation for conjunctival surface reconstruction. Am J Ophthalmol. 1997;124:765–74.
Nakamura T, Inatomi T, Sekiyama E, Ang LPK, Yokoi N, Kinoshita S. Novel clinical application of sterilized, freeze-dried amniotic membrane to treat patients with pterygium. Acta Ophthalmol Scand. 2006;84:401–5.
Tsai RJ, Li LM, Chen JK. Reconstruction of damaged corneas by transplantation of autologous limbal epithelial cells. N Eng J Med. 2000;343:86–93.
Rama P, Bonini S, Lambiase A, et al. Autologous fibrin-cultured limbal stem cells permanently restore the corneal surface of patients with total limbal stem cell deficiency. Transplantation. 2001;72:1478–85.
Shimazaki J, Aiba M, Goto E, Kato N, Shimmura S, Tsubota K. Transplantation of human limbal epithelium cultivate on amniotic membrane for the treatment of severe ocular surface disorders. Ophthalmology. 2002;109:1285–90.
Eberle J, Habermann J, Gürtler LG. HIV-1 infection transmitted by serum droplets into the eye: a case report. AIDS. 2000;14(2):206–7.
Gündüz K, Uçakhan OO, Kanpolat A, Günalp I. Nonpreserved human amniotic membrane transplantation for conjunctival reconstruction after excision of extensive ocular surface neoplasia. Eye. 2006;20:351–7.
Gicquel JJ, Dua HS, Brodie A, et al. Epidermal growth factor variations in amniotic membrane used for ex vivo tissue constructs. Tissue Eng Part A. 2009;15:1919–27.
Rahman I, Said DG, Maharajan VS, Dua HS. Amniotic membrane in ophthalmology: indications and limitations. Eye. 2009;23:1954–61.
Kruse FE, Joussen AM, Rohrschneider K, et al. Cryopreserved human amniotic membrane for ocular surface reconstruction. Graefe’s Arch Clin Exp Ophthalmol. 2000;238:68–75.
Rama P, Giannini R, Bruni A, Gatto C, Tiso R, Ponzin D. Further evaluation of amniotic membrane banking for transplantation in ocular surface diseases. Cell Tissue Bank. 2001;2:155–63.
Rodríguez-Ares MT, López-Valladares MJ, Touriño R, et al. Effects of lyophilization on human amniotic membrane. Acta Ophthalmol. 2009;87:396–403.
Dua HS, Rahman I, Miri A, Said DG. Variations in amniotic membrane: relevance for clinical applications. Br J Ophthalmol. 2010;94:963–4.
Hopkinson A, McIntosh RS, Tighe PJ, James DK, Dua HS. Amniotic membrane for ocular surface reconstruction: donor variations and the effect of handling on TGF-beta contents. Investig Ophthalmol Vis Sci. 2006;47:4316–22.
Bourne GL. The microscopic anatomy of the human amnion and chorion. Am J Obstet Gynecol. 1960;79:1070–3.
Koizumi N, Inatomi T, Sotozono C, Fullwood NJ, Quantock AJ, Kinoshita S. Growth factor mRNA and protein in preserved human amniotic membrane. Curr Eye Res. 2000;20:173–7.
López-Valladares MJ, Rodríguez-Ares MT, Touriño R, Gude F, Silva MT, Couceiro J. Donor age and gestational age influence on growth factor levels in human amniotic membrane. Acta Ophthalmol. 2010;88:211–6.
Hill P, Brantley H, Van Dyke M. Some properties of keratin biomaterials: kerateines. Biomaterials. 2010;31:585–93.
Schrooyen PM, Dijkstra PJ, Oberthür RC, Bantjes A, Feijen J. Partially carboxymethylated feather keratins. 2. Thermal and mechanical properties of films. J Agric Food Chem. 2001;49:221–30.
Verma P, Ray P, Ray AR. Preparation of scaffolds from human hair proteins for tissue-engineering applications. Biomed Mater. 2008;3:25007.
Tachibana A, Kaneko S, Tanabe T, Yamauchi K. Rapid fabrication of keratin-hydroxyapatite hybrid sponges toward osteoblast cultivation and differentiation. Biomaterials. 2005;26:297–302.
Sierpinski P, Garrett J, Ma J, et al. The use of keratin biomaterials derived from human hair for the promotion of rapid regeneration of peripheral nerves. Biomaterials. 2008;29:118–28.
Chen Y, Dong WR, Xiao YQ, Zhao BL, Hu GD, An LB. Preparation and bioactivity of human hair keratin-collagen sponge, a new type of dermal analogue. Nan Fang Yi Ke Da Xue Xue Bao. 2006;26:131–8.
Dias G, Peplow P, McLaughlin A, Teixeira F, Kelly R. Biocompatibility and osseointegration of reconstituted keratin in an ovine model. J Biomed Mater Res Part A. 2010;92:513–20.
de Guzman RC, Merrill MR, Richter JR, Hamzi RI, Greengauz-Roberts OK, Van Dyke ME. Mechanical and biological properties of keratose biomaterials. Biomaterials. 2011;32:8205–17.
Reichl S, Borrelli M, Geerling G. Keratin films for ocular surface reconstruction. Biomaterials. 2011;32:3375–86.
Riau AK, Beuerman RW, Lim LS, Mehta JS. Preservation, sterilization and de-epithelialization of human amniotic membrane for use in ocular surface reconstruction. Biomaterials. 2010;31:216–25.
Thomasen H, Pauklin M, Noelle B, Geerling G, Vetter J, Steven P, Steuhl KP, Meller D. The effect of long-term storage on the biological and histological properties of cryopreserved amniotic membrane. Curr Eye Res. 2011;36:247–55.
Nakamura A, Arimoto M, Takeuchi K, Fujii T. A rapid extraction procedure of human hair proteins and identification of phosphorylated species. Biol Pharm Bull. 2002;25:569–72.
Araki-Sasaki K, Ohashi Y, Sasabe T, et al. An SV40-immortalized human corneal epithelial cell line and its characterization. Invest Ophthalmol Vis Sci. 1995;36:614–21.
Yamauchi K, Maniwa M, Mori T. Cultivation of fibroblast cells on keratin-coated substrata. J Biomater Sci Polym Ed. 1998;9:259–70.
Tachibana A, Furuta Y, Takeshima H, Tanabe T, Yamauchi K. Fabrication of wool keratin sponge scaffolds for long-term cell cultivation. J Biotechnol. 2002;93:165–70.
Reichl S. Films based on human hair keratin as substrates for cell culture and tissue engineering. Biomaterials. 2009;30:6854–66.
Yamauchi K, Hojo H, Yamamoto Y, Tanabe T. Enhanced cell adhesion on RGDS-carrying keratin film. Mater Sci Eng C. 2003;23:467–72.
Srinivasan B, Kumar R, Shanmugam K, Sivagnam U, Reddy N, Sehgal P. Porous keratin scaffold-promising biomaterial for tissue engineering and drug delivery. J Biomed Mater Res Part B Appl Biomater. 2010;92:5–12.
Rouse JG, Van Dyke ME. A review of keratin-based biomaterials for biomedical applications. Materials. 2010;3:999–1014.
Connon CJ, Doutch J, Chen B, et al. The variation in transparency of amniotic membrane used in ocular surface regeneration. Br J Ophthalmol. 2010;94:1057–61.
Mandal B, Kundu S. Non-bioengineered silk gland fibroin protein: characterization and evaluation of matrices for potential tissue engineering applications. Biotechnol Bioeng. 2008;100:1237–50.
Rafat M, Griffith M, Hakim M, et al. Plasma surface modification and characterization of collagen-based artificial cornea for enhanced epithelialization. J Appl Polym Sci. 2007;106:2056–64.
Acknowledgments
The authors would like to thank Dr. K. Araki-Sasaki (Kagoshima, Japan) for his generous gift of the HCE-T cell line, and Dr. Meyer (Department of Ophthalmology, University of Würzburg, Germany) for help with the statistical analysis. Furthermore, special thanks are given to Drs. T. Klink, R. Guthoff and H. Sold (Department of Ophthalmology, University of Würzburg, Germany) for their time spent in the laboratory participating in the surgical feasibility tests, as well as Lucia Albrecht and Gesa Grobe (Technische Universität Braunschweig, Germany) for their technical assistance in the cell culture studies and tensile strength testing. This work was supported by the Deutsche Forschungsgemeinschaft, DFG grants Re 2596/3-1 and Ge 895/7-1.
Author information
Authors and Affiliations
Corresponding author
Additional information
Maria Borrelli and Stephan Reichl contributed equally to this study.
Rights and permissions
About this article
Cite this article
Borrelli, M., Reichl, S., Feng, Y. et al. In vitro characterization and ex vivo surgical evaluation of human hair keratin films in ocular surface reconstruction after sterilization processing. J Mater Sci: Mater Med 24, 221–230 (2013). https://doi.org/10.1007/s10856-012-4774-4
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s10856-012-4774-4