Abstract
Background
Catheter ablation of atrial fibrillation (AF) is an established therapeutic rhythm approach in symptomatic patients. Obesity is a dominant driver of AF recurrence after ablation. However, being both overweight and underweight drives long-term cardiac and general health risks. Long-term data are needed to understand the influence of body mass index (BMI) on outcomes after ablation in regard to arrhythmia recurrence and cardiovascular outcomes.
Methods
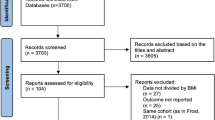
All patients who underwent an index ablation with a BMI recorded and at least 3 years of follow-up were included (n = 1558). The group was separated and compared by index ablation BMI status (≤20, 21–25, 26–30, >30 kg/m2). Long-term outcomes included AF recurrence, stroke/TIA, heart failure (HF) hospitalization, and death.
Results
Patients with advancing BMI status were more likely to be male and have hypertension, a smoking history, diabetes, HF, and a prior cardioversion. Patients with a BMI ≤20 were more likely to have a moderate-high congestive heart failure, hypertension, age >75, diabetes, stroke (CHADS2) score. At 3 years, recurrence rates of AF increased significantly with increasing BMI status (p = 0.02); paradoxically, there was a trend for increased stroke risk with decreasing BMI (p = 0.06). Long-term death rates tended to increase inversely with BMI status, and HF rates were greatest in the highest and lowest BMI groups.
Conclusions
Lower weight at AF ablation lowers arrhythmia recurrence risk. However, AF ablation patients who are normal or underweight remain at high risk of other cardiovascular outcomes including increased stroke risk with less AF burden.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
1 Introduction
Atrial fibrillation (AF) continues to increase globally in a manner not completely accounted for by aging or traditional cardiovascular risk factors [1, 2]. There are other global trends that may account for a large portion of the increased AF incidence, such as obesity, sedentary lifestyles, and lack of exercise [3, 4].
Many of the traditional risk factors for AF and heart disease are largely the result of lifestyle choices such as high blood pressure, dyslipidemia, and noninsulin dependent diabetes. Obesity is often secondary to lifestyle choices that are complex and affect diet, activity, occupation, quality of sleep, and exercise [5–7].
Current therapies, both pharmacologic and nonpharmacologic, remain suboptimal, and with long-term follow-up, AF recurrences are common [8–12]. In light of these suboptimal outcomes, recent focus has been on enhancing the likelihood of success of current treatments or preventing the disease all together. One way to do this is to modify the risk factors related to lifestyle that are driving surging trends of AF [13–16]. In patients who undergo aggressive lifestyle interventions with serial follow-up, the burden and severity of AF are reduced, and in those who undergo ablation, success rates are improved [13–16]. Given these sentinel studies regarding the impact of lifestyle modification of AF, it is reasonable to anticipate a potential inverse linear relationship between weight or body mass index (BMI) and AF success rates after ablation.
However, cardiovascular outcomes seldom follow a linear relationship with weight or BMI. In fact, most often, a U-shaped curve has been reported in that the highest risks are observed in both the underweight and overweight [17, 18]. As such, understanding the role of baseline BMI on long-term AF ablation outcomes and AF-related comorbidities may help in regard to patient counseling and management before and after catheter ablation.
2 Methods
2.1 Patient population
A total of 1558 patients who were ≥18 years of age, underwent their index AF ablation at LDS Hospital (Salt Lake City, UT) or Intermountain Medical Center (Murray, UT), and had at least 3 years of follow-up were studied. The patients were stratified into four BMI-based strata (≤20, 21–25, 26–30, >30 kg/m2). The Intermountain Healthcare Central Institutional Review Board approved this study.
2.2 Demographics and clinical assessments
In addition to index ablation BMI category, clinical characteristics were collected, including diabetes status (diabetes mellitus: fasting blood glucose >125 mg/dL, clinical diagnosis of diabetes mellitus, or anti-diabetic medication use; insulin resistance: fasting glucose between 110 and 125 mg/dL; and normal: fasting glucose <110 mg/dL), hypertension (systolic blood pressure ≥140 mmHg, diastolic ≥90 mmHg, or anti-hypertensive use), and hyperlipidemia (total cholesterol ≥200 mg/dL, LDL ≥130 mg/dL, or cholesterol-lowering medication use). Smoking was defined as an active smoker or those with a >10 pack-year history. Prior stroke, transient ischemic attack (TIA), and myocardial infarction (MI) were physician-reported or determined by previous ICD-9 discharge diagnosis codes. AF subtype (paroxysmal, persistent, or permanent) was physician-reported at ablation hospitalization. Discharge medications (i.e., statin, other lipid-lowering medications, ACE inhibitors [ACEI], angiotensin receptor blocker [ARB], beta-blocker, diuretic, digoxin, plavix) were also available. All patients were placed on warfarin for a minimum of 3 months after the ablation unless contraindicated. Within our system, in patients with a congestive heart failure, hypertension, age >75, diabetes, stroke (CHADS2) score of ≥2, long-term anti-coagulation is recommended regardless of AF ablation outcome. However, the use of long-term anti-coagulation was dependent upon the patient’s need, as determined by their primary care physician and cardiologist. Direct oral anti-coagulants are now routinely used; however, in this population, which required at least 3 years of follow-up, post-ablation anti-coagulation was with warfarin. Within our system, it is recommended that all patients fail an anti-arrhythmic drug before proceeding to ablation unless there is a clear indication that the drug may pose harm or risk in addition to that expected with ablation. The use of an anti-arrhythmic drug at the time of ablation was sought to list amongst the baseline demographics.
The ablation approach including extent of ablation, use of additional ablation beyond pulmonary vein isolation, anti-coagulation strategy, catheter-tip technology, and mapping guidance was based upon individual operator choice and not from system-wide guidelines.
2.3 Patient follow-up and event assessment
Clinical outcomes were evaluated at 3 years and included death, heart failure hospitalization, dementia, stroke, TIA, and atrial flutter or AF recurrence. All outcomes, except death and AF recurrence, were determined by ICD-9 codes and were defined as heart failure (HF) hospitalization: ICD-9 code 428, 398.91, 402.01, 402.11, 402.91, 404.01, 404.03, 404.11, 404.13, 404.91, or 404.93; stroke: ICD-9 codes 436, 433._1, and 434._1; TIA: ICD-9 code 435. Atrial flutter or AF recurrences were documented through review of the AF ablation registry with ambulatory heart monitors performed at 3, 6, 9, and 12 months post-ablation and then thereafter based upon recurrence of clinical symptoms excluding a 3-month blanking period. All electrocardiograms and/or any ordered ambulatory monitor performed after 12 months from both routine and cardiovascular assessment were also reviewed for arrhythmia recurrence and available through the system-wide healthcare network electrocardiogram database. Recurrences of AF were considered significant for this endpoint and collected from the index procedure rather than the last procedure performed. Deaths were determined by telephone survey, hospital records, and Utah State Health Department records (death certificates) and were verified through Social Security death records. Patients not listed as deceased in any registry were considered to be alive.
2.4 Statistical analysis
The chi-square statistic, Fisher’s exact test, and analysis of variance were used to evaluate baseline and clinical characteristics among the patient groups. Demographics were collected at the time of the ablation procedure. Initial evaluation to endpoints by BMI categories utilized the chi-square statistic, the Fisher’s exact test, and the Kaplan-Meier survival estimates and the log-rank test. To confirm associations determined by univariable analysis, multivariable Cox hazard regression (SPSS, version 22.0; Chicago, IL) was performed to determine hazard ratios (HRs) for 5 unit BMI increments. Final models entered the significant (p < 0.05) and confounding (10 % change in HR) baseline covariables. Two-tailed p values of ≤0.05 were designated to be nominally significant.
3 Results
The baseline demographics of the 1558 patients who underwent an index ablation for symptomatic AF are shown in Table 1. Patients who were considered overweight (BMI >26 kg/m2) or obese (BMI >30 kg/m2) comprised most of our AF population [≤20, 30 (1.9 %); 21–25, 296 (19.0 %); 26–30, 541 (34.7 %); >30, 691 (44.4 %)]. The majority of the underweight (BMI <20) were women. The underweight group had the highest rates of diagnosed chronic obstructive pulmonary disease. Risk factors that increased with BMI quartile included hypertension, dyslipidemia, and sleep apnea. Risk factors that were the highest in the underweight and overweight groups included heart failure and diabetes. The ablation approach, specifically the addition of left-sided linear ablation, and anti-arrhythmic drug therapy before and after the ablations are shown in Table 2.
The long-term event rates are shown in Table 3. At 3 years, rates of AF and atrial flutter recurrence increased with increasing baseline BMI. Total and cardiovascular death rates were similar at 1 and 3 years amongst BMI groups.
Heart failure admission rates were highest in the lightest and heaviest groups, which is consistent with their higher rates of baseline heart failure. Despite relatively higher rates of AF/atrial flutter and heart failure in the heavier groups, stroke rates were lowest in this group.
The Kaplan-Meier survival curve for freedom from recurrent AF and atrial flutter is shown in Fig. 1. There was a trend of worse outcomes with higher BMI values that was not statistically significant after multivariable adjustment (p = 0.20). The multivariable 3-year HR for AF/atrial flutter compared to normal weight (BMI = 21–25) was as follows: ≤20: adjusted HR = 1.08 (0.64, 1.81), p = 0.77, 26–30: adjusted HR = 1.22 (1.01, 1.48), p = 0.04, and >30: adjusted HR = 1.16 (0.96, 1.40), p = 0.13. Figure 2 shows the Kaplan-Meier survival-free curve for major adverse cardiac events, which is the composite of death, heart failure admission, and stroke/TIA. The highest risks were estimated in the highest and lowest BMI groups.
In the obese population (BMI >30 kg/m2), AF/atrial flutter outcomes based upon weight change were compared in three categories (1: lost >3 % of weight at 3 years, n = 141, 2: maintained weight ±3 % of weight at 3 years, n = 147, 3: gained >3 % of weight at 3 years, n = 119) (Fig. 3). Those who gained weight or maintained their weight had a higher multivariable adjusted risk of AF/atrial flutter at 3 years compared to those who lost weight, HR = 1.27 (0.85, 1.85), p = 0.24, and 1.37 (0.91, 2.02), p = 0.12, respectively. However, neither of these HRs was statistically significant after multivariate adjustment.
Kaplan-Meier survival curve for 3-year atrial fibrillation or flutter reoccurrence in obese (BMI >30 kg/m2) patients who underwent an index ablation procedure for atrial fibrillation compared by weight trends during the follow-up period. Those who lost >3 % of their baseline weight had lower rates of arrhythmia recurrence (p = 0.09)
4 Discussion
This study had several important findings. First, lower weight at the time of ablation confirms early and long-term benefits in regard to arrhythmia recurrences. In those who are obese at ablation, subsequent maintenance of weight loss can favorably influence outcomes. Second, stroke mechanisms post-ablation are multifactorial and not just a manifestation of clinical arrhythmia recurrence. Finally, we observed the risk of outcomes to be U-shaped suggestive of unique risk of being overweight and underweight.
This study adds to many prior studies that have explored the predictive role of BMI at the time of catheter ablation negatively and arrhythmia-based outcomes. Obesity has a significant impact on adverse structural remodeling of the atrium and as such would be anticipated to consistently negatively influence outcomes after ablation [19]. Many of these prior studies have shown mixed results [20–23]. In a meta-analysis of six observational studies, in aggregate, patients classified as overweight had a 27 % increased risk of AF compared to normal-weight patients [24]. However, the majority of these studies comprise post-ablation outcomes with 1 year of less follow-up and specifically evaluate the role of being overweight. In this study, we show that the adverse impact of BMI extends to 3 years and would find that being underweight did not convey risk for arrhythmia recurrence.
These data also highlight the potential pervasive value in maintenance of weight loss in obese patients as they relate to arrhythmia-related outcomes. Weight loss in obese patients has a powerful influence on arrhythmia risk before and after ablation [13–15]. However, an optimal approach to weight loss involves a dedicated center that can provide the long-term follow-up necessary to prompt compliance to healthy lifestyle choices [13, 14]. This study did not involve the active use of a lifestyle medication clinic, as it was retrospective, and as such shows outcomes of weight trends that were not necessarily targeted for modification. However, given that the majority of patients that undergo ablation are overweight or obese, high volume AF ablation centers should consider developing programs that involve lifestyle counseling, exercise prescriptions, dietary support, and recources that allow long-term follow-up and patient interactions regarding these core concepts.
Next, despite higher rates of AF in the obese groups, stroke rates did not parallel this trend. Stroke rates were highest in the normal-weight group and higher in the underweight group than the overweight group. This finding suggests that post-ablation mechanisms of stroke may be multifactorial and not solely dependent on AF recurrence. Given the study design, we were unable to explore specific mechanisms outside of less AF detected. However, one of the most striking unique stroke risk factors in the lower-weight groups was the high prevalence of female gender. Meta-analysis work supports female sex as an independent stroke risk factor [25] and as such has been added in the congestive heart failure, hypertension, age >75, diabetes, stroke, vascular disease, age >65, female sex (CHADS2-VASc) risk score [26]. There was also a trend toward more pre-ablation strokes in the less heavy groups, which is a significant predictor of recurrent strokes. However, in comparison, the overweight group had a higher rate of moderate CHADS2 scores, hypertension, diabetes, renal failure, heart failure, and higher recurrence rates and still had the lowest stroke rates.
Finally, when examining major adverse cardiac events in aggregate, we observed a 3-year U-shaped curve with higher risk in the lightest and heaviest groups. These groups are discrete in baseline demographics. However, this type of U-shaped curve found in analysis of long-term cardiac outcomes has been shown in much larger populations and highlights, in some disease states, the potential detriment and benefit with weight. As observed in our population, underweight patients have different disease states. However, they often have less muscle mass, which is a known predictor of mortality [27, 28]. Finally, adipose tissue is for energy storage. In responding to disease states that are energy demanding, such as COPD and heart failure, additional weight can allow response to acute injuries or stress that takes additional energy such as pneumonia or other infections or underlying disease exacerbations. Striking in these data is that the highest cardiovascular mortality rates were observed in the underweight with major risk factors for this mode of death, stroke, and heart failure, occurring frequently in the underweight.
5 Study limitations
This study has several important limitations to consider in the data interpretation. First, it is an observational long-term analysis. This limits the strengths of the conclusions as the compared groups are subject to confounding variables that can influence outcomes. We have highlighted in Sect. 4 the clear differences in baseline demographics among the BMI groups. Next, the AF ablation protocol was not standardized, so we cannot draw conclusions on the impact of approach or outcomes. The first-year approach to routine assessment for clinical and subclinical arrhythmias is fairly standardized with routine use of extended ambulatory monitoring; after 1 year, there is marked variability. However, the same trends that we observed in the 1-year rates were also observed in the 3-year rates. A lack of uniform approach to patients after 1 year may not only lead to an underdiagnosis of the outcomes that we studied, but can also influence treatments that influence outcomes and risks. Anti-coagulation use and compliance, a measure that we cannot track in the entire cohort, may have impacted the outcomes. As a heart rhythm team, we strongly recommended anti-coagulation in all patients post-ablation with long-term use independent of ablation outcome in those patients with a CHADS2 or CHADS2-VASc score ≥2. Finally, the underweight cohort population who underwent index ablation was relatively small compared to the other groups, and as such, the general characteristics can be influenced by the sample size alone. Also, in this group, we often observe the greatest differences in outcomes; however, statistical significance was often not seen given the relatively small number of patients.
6 Conclusion
Lower weight at AF ablation lowers arrhythmia recurrence risk that is maintained up to 3 years. However, AF ablation patients who are normal or underweight remain at high risk of other cardiovascular outcomes including increased stroke risk with less AF burden, highlighting the unique risk factors of these groups and the multivariable nature of stroke post-ablation. Long-term adverse outcomes are highest in the lightest and heaviest populations as measured by BMI, which is consistent with prior observational studies that have examined general cardiovascular outcomes and mortality.
References
Chugh SS, Havmoeller R, Narayanan K, Singh D, Rienstra M, Benjamin EJ, et al. Worldwide epidemiology of atrial fibrillation: a global burden of disease 2010 study. Circulation. 2014;129(8):837–47.
Brunner KJ, Bunch TJ, Mullin CM, May HT, Bair TL, Elliot DW, et al. Clinical predictors of risk for atrial fibrillation: implications for diagnosis and monitoring. Mayo Clin Proc. 2014;89(11):1498–505.
Healy GN, Winkler EA, Owen N, Anuradha S, Dunstan DW. Replacing sitting time with standing or stepping: associations with cardio-metabolic risk biomarkers. Eur Heart J. 2015;36(39):2643–9.
Nalliah CJ, Sanders P, Kottkamp H, Kalman JM. The role of obesity in atrial fibrillation. Eur Heart J. 2015.
Saydah S, Bullard KM, Cheng Y, Ali MK, Gregg EW, Geiss L, et al. Trends in cardiovascular disease risk factors by obesity level in adults in the United States, NHANES 1999–2010. Obesity. 2014;22(8):1888–95.
Duncan MJ, Vandelanotte C, Caperchione C, Hanley C, Mummery WK. Temporal trends in and relationships between screen time, physical activity, overweight and obesity. BMC Public Health. 2012;12:1060.
Troost JP, Rafferty AP, Luo Z, Reeves MJ. Temporal and regional trends in the prevalence of healthy lifestyle characteristics: United States, 1994–2007. Am J Public Health. 2012;102(7):1392–8.
Bunch TJ, May HT, Bair TL, Jacobs V, Crandall BG, Cutler M, et al. The impact of age on 5-year outcomes after atrial fibrillation catheter ablation. J Cardiovasc Electrophysiol. 2016;27(2):141–6.
Bunch TJ, Crandall BG, Weiss JP, May HT, Bair TL, Osborn JS, et al. Patients treated with catheter ablation for atrial fibrillation have long-term rates of death, stroke, and dementia similar to patients without atrial fibrillation. J Cardiovasc Electrophysiol. 2011;22(8):839–45.
Wilber DJ, Pappone C, Neuzil P, De Paola A, Marchlinski F, Natale A, et al. Comparison of antiarrhythmic drug therapy and radiofrequency catheter ablation in patients with paroxysmal atrial fibrillation: a randomized controlled trial. JAMA: J Am Med Assoc. 2010;303(4):333–40.
Cosedis Nielsen J, Johannessen A, Raatikainen P, Hindricks G, Walfridsson H, Kongstad O, et al. Radiofrequency ablation as initial therapy in paroxysmal atrial fibrillation. N Engl J Med. 2012;367(17):1587–95.
Oral H, Pappone C, Chugh A, Good E, Bogun F, Pelosi Jr F, et al. Circumferential pulmonary-vein ablation for chronic atrial fibrillation. N Engl J Med. 2006;354(9):934–41.
Pathak RK, Elliott A, Middeldorp ME, Meredith M, Mehta AB, Mahajan R, et al. Impact of CARDIOrespiratory FITness on arrhythmia recurrence in obese individuals with atrial fibrillation: the CARDIO-FIT study. J Am Coll Cardiol. 2015;66(9):985–96.
Pathak RK, Middeldorp ME, Meredith M, Mehta AB, Mahajan R, Wong CX, et al. Long-term effect of goal-directed weight management in an atrial fibrillation cohort: a long-term follow-up study (LEGACY). J Am Coll Cardiol. 2015;65(20):2159–69.
Pathak RK, Middeldorp ME, Lau DH, Mehta AB, Mahajan R, Twomey D, et al. Aggressive risk factor reduction study for atrial fibrillation and implications for the outcome of ablation: the ARREST-AF cohort study. J Am Coll Cardiol. 2014;64(21):2222–31.
Abed HS, Wittert GA, Leong DP, Shirazi MG, Bahrami B, Middeldorp ME, et al. Effect of weight reduction and cardiometabolic risk factor management on symptom burden and severity in patients with atrial fibrillation: a randomized clinical trial. JAMA: J Am Med Assoc. 2013;310(19):2050–60.
Romero-Corral A, Montori VM, Somers VK, Korinek J, Thomas RJ, Allison TG, et al. Association of bodyweight with total mortality and with cardiovascular events in coronary artery disease: a systematic review of cohort studies. Lancet. 2006;368(9536):666–78.
Roh L, Braun J, Chiolero A, Bopp M, Rohrmann S, Faeh D, et al. Mortality risk associated with underweight: a census-linked cohort of 31,578 individuals with up to 32 years of follow-up. BMC Public Health. 2014;14:371.
Mahajan R, Lau DH, Brooks AG, Shipp NJ, Manavis J, Wood JP, et al. Electrophysiological, electroanatomical, and structural remodeling of the atria as consequences of sustained obesity. J Am Coll Cardiol. 2015;66(1):1–11.
Letsas KP, Siklody CH, Korantzopoulos P, Weber R, Burkle G, Mihas CC, et al. The impact of body mass index on the efficacy and safety of catheter ablation of atrial fibrillation. Int J Cardiol. 2013;164(1):94–8.
Chilukuri K, Dalal D, Gadrey S, Marine JE, Macpherson E, Henrikson CA, et al. A prospective study evaluating the role of obesity and obstructive sleep apnea for outcomes after catheter ablation of atrial fibrillation. J Cardiovasc Electrophysiol. 2010;21(5):521–5.
Jongnarangsin K, Chugh A, Good E, Mukerji S, Dey S, Crawford T, et al. Body mass index, obstructive sleep apnea, and outcomes of catheter ablation of atrial fibrillation. J Cardiovasc Electrophysiol. 2008;19(7):668–72.
Mohanty S, Mohanty P, Di Biase L, Bai R, Dixon A, Burkhardt D, et al. Influence of body mass index on quality of life in atrial fibrillation patients undergoing catheter ablation. Heart Rhythm. 2011;8(12):1847–52.
Guijian L, Jinchuan Y, Rongzeng D, Jun Q, Jun W, Wenqing Z. Impact of body mass index on atrial fibrillation recurrence: a meta-analysis of observational studies. Pacing Clin Electrophysiol: PACE. 2013;36(6):748–56.
Wagstaff AJ, Overvad TF, Lip GY, Lane DA. Is female sex a risk factor for stroke and thromboembolism in patients with atrial fibrillation? A systematic review and meta-analysis. QJM. 2014;107(12):955–67.
Lip GY, Nieuwlaat R, Pisters R, Lane DA, Crijns HJ. Refining clinical risk stratification for predicting stroke and thromboembolism in atrial fibrillation using a novel risk factor-based approach: the euro heart survey on atrial fibrillation. Chest. 2010;137(2):263–72.
Wannamethee SG, Shaper AG, Whincup PH, Lennon L, Papacosta O, Sattar N. The obesity paradox in men with coronary heart disease and heart failure: the role of muscle mass and leptin. Int J Cardiol. 2014;171(1):49–55.
Wannamethee SG, Shaper AG, Lennon L, Whincup PH. Decreased muscle mass and increased central adiposity are independently related to mortality in older men. Am J Clin Nutr. 2007;86(5):1339–46.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Funding
None
Rights and permissions
About this article
Cite this article
Bunch, T.J., May, H.T., Bair, T.L. et al. Long-term influence of body mass index on cardiovascular events after atrial fibrillation ablation. J Interv Card Electrophysiol 46, 259–265 (2016). https://doi.org/10.1007/s10840-016-0142-5
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s10840-016-0142-5