Abstract
Purpose
The modulation of the autonomic nervous system (ANS) has been shown to prevent myocardial ischemia-reperfusion injury (MIRI). Carotid baroreceptor stimulation modulates the ANS by sympathetic withdrawal and vagal activation. The aim of this study was to assess whether low-level carotid baroreceptor stimulation (LL-CBS) attenuated MIRI and test its underlying molecular mechanisms.
Methods
Forty adult healthy mongrel dogs were randomly assigned to three groups as follows: (1) I/R group (n = 15): left anterior descending artery (LAD) was occluded for 1 h and allowed for 1 h reperfusion; (2) LL-CBS group (n = 15): I/R plus LL-CBS; and (3) sham group (n = 10): sham surgery without stimulation. The voltage-reducing blood pressure by 5 % was defined as the threshold. LL-CBS was performed at a voltage that is 80 % below the threshold. Infarct size was assessed with Evans blue and TTC staining. The inflammatory cytokines, biomarker of oxidative stress and apoptosis, and connexin 43 (Cx43) expression were measured to assess the injury.
Results
The number of ventricular tachycardia/ventricular fibrillation (VT/VF) episodes was significantly decreased in the LL-CBS group compared with the I/R group (2.8 ± 0.8 vs. 7.0 ± 2.6, P < 0.05). LL-CBS reduced tumor necrosis factor α, interleukin (IL)-1, IL-6, and malondialdehyde levels but increased superoxide dismutase level compared with the I/R group (P < 0.05). Meanwhile, LL-CBS significantly decreased the percentage of terminal deoxynucleotidyl transferase-mediated dUTP-biotin nick end labeling assay (TUNEL)-positive cardiomyocytes (20 ± 8 vs. 47 ± 12, P < 0.05). Western blotting and real-time polymerase chain reaction (RT-PCR) in Cx43 revealed that LL-CBS caused an increase, respectively, compared with the I/R group (0.75 ± 0.3 vs. 0.3 ± 0.2 and 1.0 ± 0.3 vs. 0.4 ± 0.1, respectively, both P < 0.05).
Conclusions
LL-CBS exerted cardioprotective effects during ischemic reperfusion period potentially by inhibiting inflammation, oxidative stress, and apoptosis and modulating the Cx43 expression.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
1 Introduction
Coronary heart disease is the leading cause of death and disability worldwide [1]. Currently, timely myocardial reperfusion forms the cornerstone of acute myocardial infarction treatment. Although advances in percutaneous coronary intervention technology and the appropriate use of pharmacological agents to restore coronary flow have improved clinical outcomes, myocardial ischemia-reperfusion injury (MIRI) still occurs [2], which can also paradoxically counteract the beneficial results of myocardial reperfusion. Recently, autonomic nervous system (ANS) modulation has been shown to prevent MIRI [3–5].
Carotid baroreceptor stimulation can lower blood pressure (BP) by reducing the activity of the peripheral sympathetic nervous system [6] and can modulate the ANS by sympathetic withdrawal and vagal activation [7]. Reduced sympathetic drive and increased vagal tone are generally considered to preserve the left ventricular systolic function, limit the myocardial infarct size, and block the arrhythmic effect during acute ischemia-reperfusion injury [3–5]. Liao et al. demonstrated that low-level carotid baroreceptor stimulation (LL-CBS) inhibited the occurrences of ventricular arrhythmias during acute ischemia through ANS modulation in anesthetized dogs [8, 9]. However, the molecular mechanism of LL-CBS on ischemia-reperfusion injury remains unknown.
The process of myocardial reperfusion injury involves the activation of an inflammatory cascade and the imbalance of oxidative stress, and also, it induces cardiomyocyte apoptosis. Inhibition of inflammatory reaction and suppression of oxidative stress induced by MIRI could effectively reduce infarct size and attenuate cardiac dysfunction. Connexin43 (Cx43) is the primary gap junction protein responsible for conduction in the ventricles. Cx43 downregulation creates the substrate for arrhythmia and increases the arrhythmic risk after acute ischemia [10]. The reverse remodeling of impaired Cx43 expression can restore abnormal cardiac function and normalize electrical stability [11]. In the present study, using canine model, we test whether LL-CBS exerts cardioprotective effects against MIRI by anti-inflammation, anti-oxidative stress, and Cx43 modulation.
2 Materials and methods
2.1 Animal preparation
The animal protocol was approved by the Animal Care and Use Committee of Renmin Hospital of Wuhan University. All dogs were anesthetized with Na pentobarbital (30 mg/kg) and ventilated with room air using a positive pressure respirator (MAO01746, Harvard Apparatus Holliston, USA). Additional maintenance doses (2 mg/kg) were administered every other hour during the procedure. Normal saline (50–100 mL/h) was infused into femoral vein to replace spontaneous fluid losses. An arterial sheath was inserted into the right femoral artery to continuously monitor arterial blood pressure (BP). A computer-based laboratory system (Lead 2000B; Jingjiang Inc., China) was used to continuously record body electrocardiogram (ECG). The core body temperature of dogs was maintained at 36.5 ± 1.5 °C by the use of a heating pad during the whole treatment.
2.2 LL-CBS protocol
The right common carotid artery and internal carotid artery bifurcation from all dogs were isolated and exposed. A custom-made Ag-AgCl-stimulating electrode linked to a pulse generator (SEN-7103, Nihon Kohden, Tokyo, Japan) to deliver stimulation was implanted around the carotid sinus. The proper placement of the electrode was confirmed by three to four acute stimulation runs performed 1 to 3 min apart, each confirming an acute drop in BP and a reduction in HR, followed by a 15-min break. After BP and HR were restored to pre-stimulus levels, CBS was performed again. The voltage started at 1 V and was increased by 0.2 V every 5 min (50 Hz, 0.5-ms square wave) until BP and HR reduction was achieved. The voltage necessary to achieve BP and HR reduction by 5 % was used as the threshold for the LL-CBS settings in each experiment. The voltage used as the stimulation setting for LL-CBS was 80 % below the threshold, and the stimulation threshold was checked every 30 min to ensure the use of the appropriate LL-CBS setting [9, 12]. The pulse generator was programmed using the following parameters: 2.8–7.2 V, 50 Hz, and 0.5-ms pulse duration [13]. The stimulation was maintained until the end of the experiment.
2.3 Acute ischemia-reperfusion protocol
The chest of each dog was opened through a left thoracotomy at the fifth intercostal space, and the left anterior descending artery (LAD) was isolated after pretreatment. The LAD was occluded for 1 h by ligature (3–0 silk), which was positioned at approximately one third of the distance from the apex. Then, reperfusion was allowed for the following hour.
2.4 Experimental design
Forty healthy adult male mongrel dogs (body weight, 14 ± 4 kg) were supplied by the center of experimental animals at the medical college of Wuhan University. All of the dogs were randomly assigned to three groups. Dogs from the I/R group (n = 15) were subjected to 1 h ischemia and 1 h reperfusion without stimulation. The LL-CBS group (n = 15) underwent stimulation for 3 h plus ischemia 1 h and reperfusion 1 h. Dogs in the LL-CBS group performed pre-stimulation 1 h before LAD occlusion and 2 h stimulation when occlusion started. Sham group (n = 10) underwent sham surgery without LAD occlusion and stimulation (Fig. 1).
Schematic representation of the study protocols. The ischemic period (60 min) was induced by complete ligation of the LAD. The reperfusion period (60 min) was induced by LAD release. In the I/R group, canines underwent 1 h ischemia and following one reperfusion. In the LL-CBS group, LL-CBS (60 min) was given before LAD occlusion and continuously performed during ischemia-reperfusion period (120 min). Sham surgery and stimulation were given during the whole experiment in the sham group. LAD left anterior descending, LL-CBS low-level carotid baroreceptor stimulation
2.5 Assessment of ventricular arrhythmias
Ventricular arrhythmias observed in the ECG were classified according to the Lambeth Conventions criteria as premature ventricular contractions (PVCs), ventricular tachycardia (VT), or ventricular fibrillation (VF) [14]. Specifically, VT was defined as more than five consecutive PVCs. VF was characterized as a loss of the synchronicity of the electrocardiogram plus a decreased amplitude and a fall in the BP. In any cases of uncertainty, two blinded investigators were selected for electrocardiogram reading.
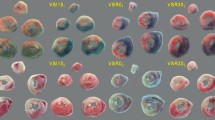
2.6 Infarct size determination
After reperfusion for 1 h, the LAD was reoccluded by ligature at the same position, and Evans blue dye was injected via the left atrial appendage. The dogs were killed, and the hearts were excised, sectioned, and stained with 2,3,5-triphenyltetrazolium chloride. The area at risk (AAR) was defined as the area not stained by Evans blue, and the infarcted area was defined as the area not stained by triphenyltetrazolium chloride [3]. Non-ischemic myocardium was stained blue, ischemic myocardium was stained red, while infarct size appeared white without staining. The infarct sizes were evaluated by Image Tool software version 3.0. The area ratio of infarct to AAR and of AAR to total ventricle were calculated and expressed as percentages.
2.7 Measurement of serum and myocardial inflammatory factors
Blood samples were collected from the femoral vein at baseline and after a 2-h ischemia-reperfusion period and taken in ice-chilled tubes coated with EDTA (BD Vacutainer K2E, BD Diagnostics, NJ). After resting in a supine position for at least 30 min, serum was separated by centrifugation at 4000 rpm for 15 min at 4 °C and was stored at −80 °C until assayed. Myocardial infarct tissue were thawed, weighed, and homogenized with Tris–HCl (5 mmol/L containing 2 mmol/L ethylene diamine tetraacetic acid (EDTA), pH 7.4). Homogenates were centrifuged (4000 rpm, 15 min, 4 °C), and the supernatants were used immediately for the assays of inflammatory cytokines [15]. Radioimmunoassay was performed using high-specific tumor necrosis factor (TNF-α; FT-630G, Nuclear Devices Factory, Beijing, China), interleukin 1 (IL-1), and interleukin 6 (IL-6) kits (R&D Systems, Abingdon, UK) according to the manufacturer’s information.
2.8 Measurement of MDA and SOD content in serum and myocardial tissue
The method of blood samples collection and serum centrifugation was the same as the above method. Aliquots of ischemic tissues were homogenized and centrifuged for 15 min at 10,000 rpm at 4 °C. The superoxide dismutase (SOD) and malondialdehyde (MDA) were measured using commercialized chemical assay kits according to the instructions of the manufacturer (Nanjing Jiancheng Bioengineering Institute, Nanjing City, China). SOD concentrations were measured by xanthine oxidase method [16], and MDA concentrations were measured according to the thiobarbituric acid (TBA) method with the spectrophotometric measurement. Myocardial SOD and MDA activity was expressed/milligram of protein.
2.9 TUNEL staining for myocardial apoptosis
Myocardial apoptosis was determined by terminal deoxynucleotidyl transferase-mediated dUTP-biotin nick end labeling assay (TUNEL) staining according to the manufacturer’s instructions (Roche Bio-chemicals, Mannheim, Germany) [17]. Briefly, the sections were deparaffinized and dehydrated with xylene and ethanol solutions. After being penetrated with a 1 % Triton X-100 transparent liquid at 37 °C for 5 min, sections were rinsed in phosphate-buffered saline (PBS) and treated with protease. After washing, the sections were incubated with TUNEL reaction solution in a humidified environment at 37 °C. After washing in PBS three times, sections were treated with 50 mL of converter-POD in a humidified environment at room temperature for 30 min. Fluorescence microscope (Nikon TE2000, Japan) at EX 450–500 nm/EM 515–565 nm was used to analyze stained sections. The TUNEL-positive cells were defined as the cells that exhibited condensed nuclei with an irregular form or split into brown particles. Each slide was examined under microscope to select three fields to detect cell death, and apoptotic index was calculated using the IPP 6.0 software.
2.10 Western blot
Membrane proteins were extracted as described previously [18]. Cx43 were detected with mouse monoclonal anti-pan-Cx43 antibodies (1/1000, Chemicon). Glyceraldehyde-3-phosphate dehydrogenases (GAPDH) were detected with mouse monoclonal anti-GAPDH (1/10,000, RDI) primary antibodies. Following the application of primary antibodies, membranes were incubated with anti-mouse (1/10,000, Santa Cruz Biotechnology) horseradish peroxidase-conjugated secondary antibodies. Signals were detected by chemiluminescence and quantified by video densitometry. Band intensities are expressed relative to GAPDH.
2.11 Real-time polymerase chain reaction of Cx43 expression
We acquired ventricular tissues from ischemic sites. Total cellular RNA was isolated from ventricular tissue, DNase treated, quantified, and quality controlled. PCR was performed with the following primer pair: forward 5′-AGA AAG AGG AGG AGC TCA AAG TTG-3′, reverse 5′-TTC AAT CTG CTT CAA GTG CAT GT-3′; β-actin: forward 5′-CGA TGA GGC CCA GAG CAA-3′, reverse 5′-TGA CGA TGC CGT GCT CAA-3′. β-Actin was used as an internal control. The synthesized primers were supplied by Shanghai BioAsia Biotech Company. Fluorescence signals were measured by a real-time quantitative PCR detection system (Applied Biosystems). The relative mRNA expression was determined by calculating 2−ΔCt. The details were described in a previous study [19].
2.12 Statistical analysis
The data was presented as the mean ± SD. The independent-samples t test was used to compare the mean of arrhythmias episodes between two groups. Statistical analysis was performed by one-way ANOVA among three groups, followed by post hoc analysis with the Tukey method to adjust multiple comparisons. Values of P < 0.05 were considered significant. Statistical program SPSS17.0 (SPSS, Inc, Chicago, IL) was used for data analysis.
3 Results
The heart rate and blood pressure were stable in all three groups during the entire period of the experiment.
3.1 Ventricular arrhythmias
Figure 2a shows examples of normal, PVC, VT, and VF ECG tracings. As shown in Fig. 2b, the 2-h continuous electrocardiogram recording revealed that the numbers of PVCs in the LL-CBS group were significantly decreased during the periods of ischemia and reperfusion when compared with those in the I/R group. Moreover, the number of VT/VF episodes was significantly decreased in the LL-CBS group compared with the I/R group (Fig. 2c). There was a significant decrease of VT/VF onset during the ischemic period in the LL-CBS group compared with the I/R group, whereas no changes were detected in time to VT/VF onset among the groups during reperfusion (Fig. 2d). In the sham group, there is no PVC, VT, or VF during ECG recording.
LL-CBS on the occurrence of cardiac arrhythmia during ischemia-reperfusion injury. a Examples of normal, PVC, VT, and VF ECG (lead I) tracings. b PVCs were markedly decreased in the LL-CBS group during the periods of ischemia and reperfusion compared with the control group. c The number of VT/VF episodes was significantly reduced in the LL-CBS group during ischemia and reperfusion. c The time to VT/VF episode onset was not significantly different between the groups during ischemia and reperfusion. *P < 0.05 vs. the I/R group. ECG electrocardiogram, LL-CBS low-level carotid baroreceptor stimulation, PVC premature ventricular contraction, VF ventricular fibrillation, VT ventricular tachycardia
3.2 Analysis of the area at risk and infarct size
The AAR (Fig. 3) in the LL-CBS group, expressing as a percentage of the total ventricle area, did not significantly change when compared with the I/R group. However, LL-CBS reduced the infarct size/area at risk (IS/AAR) ratio during acute ischemia-reperfusion injury (P < 0.05).
Assessment of the area at risk and infarct size. The AAR, expressed as the percentage of the total ventricular area, was not different among the groups. The myocardial IS, which was expressed as the percentage of the AAR, was significantly reduced by LL-CBS when compared with I/R group. *P < 0.05. AAR area at risk, NS not significant, IS infarct size
3.3 Effects of LL-CBS on inflammatory injury
Inflammation is one of the important mechanisms of myocardial ischemia-reperfusion injury. In order to test whether LL-CBS can inhibit inflammatory injury, herein, we measured serum and local tissue TNF-α, IL-1, and IL-6. All of the three inflammatory cytokines both in serum and myocardial tissue were significantly increased after 2 h ischemia-reperfusion injury when compared with baseline (P < 0.05, Fig. 4), whereas LL-CBS reduced high-level inflammatory cytokines induced by myocardial I/R injury. These results indicate that LL-CBS could inhibit inflammatory reaction during myocardial ischemia-reperfusion injury period.
Effects of LL-CBS on systemic and local inflammatory cytokines. Myocardial I/R injury induced excessive inflammatory cytokines release including TNF-α, IL-1, and IL-6. However, LL-CBS significantly attenuated the increases induced by I/R injury. *P < 0.05. IL-1 interleukin 1, IL-6 interleukin 6, TNF-α tumor necrosis factor α
3.4 Effects of LL-CBS on oxidative stress activity
Oxidative stress plays a critical role in myocardial ischemia-reperfusion injury and the activity of oxidative stress can be reflected by SOD and MDA concentrations in serum and myocardial ischemic tissues. SOD, an antioxidant biomarker, was significantly reduced after 2 h MIRI both in serum and myocardial ischemic tissue (P < 0.05). MDA, as a biomarker to assess the activity of pro-oxidative stress, showed a significant increase in serum as well as in myocardial ischemic tissues (P < 0.05). LL-CBS effectively increased SOD concentration and reduced MDA concentration when compared with the I/R group (Fig. 5, P < 0.05).
Effects of LL-CBS on oxidative stress in myocardium and serum. a, b Serum MDA and SOD concentrations were significantly increased in the I/R group compared with the sham group, whereas LL-CBS effectively reversed the increases. c, d Myocardial MDA and SOD levels were remarkably higher than the sham group, whereas LL-CBS effectively reduced this increase phenomenon. # P < 0.05 when compared with the other two groups; *P < 0.05 when compared with baseline. MDA myeloperoxidase, MPO malondialdehyde, SOD superoxide dismutase
3.5 Effects of LL-CBS on myocardial apoptosis
Apoptosis is the major mechanism of cell death induced by MIRI. Herein, myocardial apoptosis was assessed by TUNEL staining. TUNEL-positive cells were defined as the death of cells. In the MIRI group, the TUNEL-positive cells expressed as the percent of total nuclei were significantly increased when compared with the sham group. The percentage of TUNEL-positive cardiomyocytes was significantly lower in the LL-CBS group compared with the MIRI group (Fig. 6, P < 0.05).
Effects of LL-CBS on myocardiocytes apoptosis in infarction size detected with TUNEL staining. a Section from the sham group. b Section from the I/R group. c Section from the LL-CBS group. (Original magnification, ×200; brown indicates TUNEL-positive nucleus, whereas blue indicates non-apoptotic cells). d Apoptotic indexes among three groups. # P < 0.05 when compared with the other two groups; *P < 0.05 when compared with baseline. TUNEL terminal deoxynucleotidyl transferase-mediated dUTP-biotin nick end labeling assay
3.6 Effects of LL-CBS on Cx43 expression
Western blotting expression of Cx43 are shown in Fig. 7a, b. Figure 7a presents the representative western blots of the left ventricle homogenates from the three groups. Figure 7b shows that the relative expressions are presented as the ratio between proteins and GAPDH. Figure 7c shows the quantitative PCR analysis of Cx43 levels in the three groups. Myocardial I/R injury significantly induced ventricular Cx43 expression reduction, whereas LL-CBS caused an increase in the Cx43 protein level when compared with the I/R group (P < 0.05).
Effects of LL-CBS on Cx43 expression in western blot and RT-PCR. a Representative Western blots of left ventricle homogenates from the three groups. b Relative expressions are presented as the ratio between proteins and GAPDH. c Quantitative PCR analysis of Cx43 levels in the three groups. LL-CBS caused an increase in the Cx43 protein level compared with the I/R group. *P < 0.05. Cx43 connexin 43
4 Discussion
The present study demonstrates that LL-CBS protects the heart against acute ischemia-reperfusion injury. The modulation of the ANS by LL-CBS effectively reduced the occurrence of ventricular arrhythmias and limited the infarct size during acute ischemia-reperfusion period. Furthermore, the cardioprotective mechanisms of LL-CBS potentially involved the inhibition of inflammatory reaction, oxidative stress, and apoptotic reaction, as well as Cx43 expression modulation.
The carotid baroreceptors, one of the mechanoreceptor families located in the carotid sinus, are sensitive to stretch, i.e., to the distension of the carotid wall [20]. Studies have shown that the activation of the carotid baroreceptor reduced the sympathetic outflow and enhanced the vagal tone [7]. The occurrence and development of cardiovascular disease are mostly associated with the excessive activation of the sympathetic tone and increased vagal activation, exerting a protective effect in most cardiovascular diseases. It was reported that carotid sinus stimulation could be an effective treatment strategy for hypertension and heart failure [13, 21–23]. Liao et al. demonstrated that LL-CBS prevented ventricular arrhythmias during acute ischemic events by modulating the ANS in anesthetized dogs [9]. LL-CBS buffered the rise in LF/HF during ischemia-reperfusion and reduced the occurrence of ventricular arrhythmias. These findings further confirmed the previous work. Moreover, LL-CBS significantly decreased the occurrence of PVCs and the number of spontaneous VT/VF episodes; these effects are consistent with previous studies showing that vagus nerve stimulation, spinal cord stimulation, and renal denervation exerted anti-arrhythmic effects during ischemia-reperfusion [3–5]. These methods inhibited arrhythmias through reduced sympathetic outflow or enhanced vagal tone. These two effects worked simultaneously during LL-CBS to provide cardioprotection from acute ischemia-reperfusion injury. In addition, LL-CBS exerted cardioprotective effects without influencing the BP or HR, indicating that ANS modulation could be independent of BP and HR. This was also shown by Linz et al. in a pig model of acute ischemia-reperfusion injury and by Shinlapawittayatorn et al. in an investigation of low-amplitude vagus nerve stimulation [3].
In the present study, LL-CBS notably reduced the occurrence of ventricular arrhythmias compared with the I/R group, which confirmed the previous studies of acute ischemia [8, 9]. Meanwhile, infarct size induced by I/R injury also was significantly attenuated by LL-CBS treatment in this study. However, the previous study showed that 1 h LL-CBS treatment before the LAD occlusion did not significantly reduced infarct size in ischemic model. In our present study, using 2 h I/R model, dogs underwent 1 h pre-LL-CBS before LAD occlusion and 2 h LL-CBS during myocardial ischemic reperfusion period, totaling 3 h stimulation. This different results between the present and previous studies may be explained by stimulation time and sample size.
Ventricular arrhythmias are important causes of sudden cardiac death in acute myocardial infarction [24]. The reduced ventricular effective refractory period and slow conduction velocity are associated with altered electrophysiological properties in ventricular arrhythmias. The latter depends on cell-to-cell communications via gap junctions. In the adult heart, ventricular gap junctions are primarily formed by Cx43 protein; the remarkable reduction of Cx43 could be one component of the substrate that promotes lethal ventricular tachyarrhythmias during acute myocardial ischemia [10]. ANS modulation by LL-CBS reduced ischemia-reperfusion-induced ventricular arrhythmias and preserved Cx43 protein levels in the present study. Cx43 has been found not only at the plasma membrane, forming gap junctions and hemi-channels, but also at the inner mitochondrial membrane of cardiac subsarcolemmal mitochondria [25]. At the plasma membrane, Cx43 has been implicated as a cytoprotective effector by improving cell volume homeostasis [26]. Mitochondrial Cx43 hemi-channels can influence cell survival by modulating mitochondrial integrity. Mitochondrial Cx43 is required for the generation of mitochondrial reactive oxygen species, which are required for protective signal transduction, including the PKCε activation downstream of the diazoxide-sensitive mitochondrial KATP channel [27].
Myocardial ischemia-reperfusion injury is a complex process and several molecular mechanisms are involved in its pathogenesis. A great deal of evidence has shown that the reperfusion injury is partly induced by an excessive formation of reactive oxygen species (ROS) and free radicals [28, 29]. Free radicals finally trigger the inflammatory response. ROS and inflammatory cytokines consequently cause severe tissue damage and activate the program of cellular apoptosis, eventually leading to cell death. ROS could be attenuated by antioxidant mechanisms. MDA, as a biomarker to detect the activity of pro-oxidative stress, is an index of lipid damage by ROS. In our study, we found that MDA concentrations were significantly increased both in serum and myocardial tissue induced by reperfusion injury, whereas this increase phenomenon was reversed by LL-CBS. In addition, SOD, as a biomarker of antioxidant stress, provides a defense mechanism against ROS. We observed that myocardial ischemia-reperfusion injury induced a significantly reduce, whereas LL-CBS reversed the decrease caused by reperfusion injury. Koss et al. [30] demonstrated that autonomic nervous system stimulation effectively reduced ROS production induced by ischemic heart in a rat model. Furthermore, I/R injury also activates some pro-inflammatory cytokines, including TNF-α, IL-1, and IL-6, which could aggravate myocardial damage. In our study, we showed that TNF-α, IL-1, and IL-6 were significantly increased during ischemia-reperfusion period, but LL-CBS could effectively suppress inflammatory response. Zhang et al. [31] has shown that increased vagal tone could effectively inhibit systemic and local inflammatory responses to relieve myocardial I/R injury. Apoptosis is an important form for cell death in I/R injury myocardium and could be regulated by oxidative stress and inflammatory response [32]. We showed that LL-CBS could regulate myocardial apoptosis, as verified by the change of TUNEL-positive cells. Therefore, we indicated that the potential mechanisms of LL-CBS on cardiac protection against reperfusion damage might be involved in the suppression of oxidant stress, inflammatory reaction, and cellular apoptotic reactions.
4.1 Limitations
Recently, low-level neuromodulation, e.g., low-level vagus nerve stimulation (LL-VNS) [33–38] or LL-CBS [8, 9, 12], has emerged as an intriguing approach to prevent cardiac arrhythmias. It has been shown that decreasing sympathetic tone and increasing vagal tone both appear to be contributed to the cardioprotective effects of LL-VNS or LL-CBS [8, 9, 34, 35, 39, 40]. Future studies may employ atropine or other muscarinic blocker to further investigate which limb of the autonomic nervous system is primarily involved in the mechanisms underlying the cardioprotective effects of LL-CBS. All experiments were conducted under general anesthesia, which is known to alter the cardiac electrophysiological parameters. However, all interventions were compared in a similar background, and it is unlikely that anesthesia plays a meaningful role in the effects of LL-CBS. Our studies focused on the acute effects of LL-CBS on ischemia-reperfusion injury. However, the effects of chronic LL-CBS are also important, and these effects should be explored in future studies.
4.2 Clinical perspectives
During the past decades, CBS has emerged as a novel and promising treatment strategy for hypertension and heart failure, both of which are high-risk factors of acute myocardial infarction. The present study shows that LL-CBS provides a protective effect against acute ischemia-reperfusion injury. Therefore, LL-CBS may provide more benefits for acute myocardial infarction patients with hypertension and/or heart failure.
5 Conclusion
LL-CBS reduced the occurrence of ventricular arrhythmias and limited the infarct size. The potential molecular mechanisms of LL-CBS cardioprotection may involve the inhibition of oxidative stress and inflammatory response and the preservation of the loss of Cx43 through ANS modulation during acute ischemia-reperfusion injury.
References
Yasuda, S., & Shimokawa, H. (2009). Acute myocardial infarction: the enduring challenge for cardiac protection and survival. Circulation Journal, 73(11), 2000–2008.
Hausenloy, D. J., & Yellon, D. M. (2013). Myocardial ischemia-reperfusion injury: a neglected therapeutic target. Journal of Clinical Investigation, 123(1), 92–100.
Shinlapawittayatorn, K., Chinda, K., Palee, S., Surinkaew, S., Thunsiri, K., Weerateerangkul, P., et al. (2013). Low-amplitude, left vagus nerve stimulation significantly attenuates ventricular dysfunction and infarct size through prevention of mitochondrial dysfunction during acute ischemia-reperfusion injury. Heart Rhythm, 10(11), 1700–1707.
Odenstedt, J., Linderoth, B., Bergfeldt, L., Ekre, O., Grip, L., Mannheimer, C., et al. (2011). Spinal cord stimulation effects on myocardial ischemia, infarct size, ventricular arrhythmia, and noninvasive electrophysiology in a porcine ischemia-reperfusion model. Heart Rhythm, 8(6), 892–898.
Linz, D., Wirth, K., Ukena, C., Mahfoud, F., Poss, J., Linz, B., et al. (2013). Renal denervation suppresses ventricular arrhythmias during acute ventricular ischemia in pigs. Heart Rhythm, 10(10), 1525–1530.
Heusser, K., Tank, J., Engeli, S., Diedrich, A., Menne, J., Eckert, S., et al. (2010). Carotid baroreceptor stimulation, sympathetic activity, baroreflex function, and blood pressure in hypertensive patients. Hypertension, 55(3), 619–626.
Henderson, L. A., James, C., & Macefield, V. G. (2012). Identification of sites of sympathetic outflow during concurrent recordings of sympathetic nerve activity and fMRI. Anatomy Record (Hoboken), 295(9), 1396–1403.
Liao, K., Yu, L., He, B., et al. (2014). Carotid baroreceptor stimulation prevents arrhythmias induced by acute myocardial infarction through autonomic modulation. Journal of Cardiovascular Pharmacology, 64(5), 431–437.
Liao, K., Yu, L., Yang, K., et al. (2014). Low-level carotid baroreceptor stimulation suppresses ventricular arrhythmias during acute ischemia. PLoS One, 9(10), e109313.
Peters, N. S., Green, C. R., Poole-Wilson, P. A., & Severs, N. J. (1993). Reduced content of connexin43 gap junctions in ventricular myocardium from hypertrophied and ischemic human hearts. Circulation, 88(3), 864–875.
Fontes, M. S., van Veen, T. A., de Bakker, J. M., & van Rijen, H. V. (2012). Functional consequences of abnormal Cx43 expression in the heart. Biochimica et Biophysica Acta, 1818(8), 2020–2029.
Dai, M., Bao, M., Liao, J., Yu, L., Tang, Y., Huang, H., et al. (2015). Effects of low-level carotid baroreflex stimulation on atrial electrophysiology. Journal of Interventional Cardiac Electrophysiology, 43(2), 111–119.
Sabbah, H. N., Gupta, R. C., Imai, M., Irwin, E. D., Rastogi, S., Rossing, M. A., et al. (2011). Chronic electrical stimulation of the carotid sinus baroreflex improves left ventricular function and promotes reversal of ventricular remodeling in dogs with advanced heart failure. Circulation. Heart Failure, 4(1), 65–70.
Walker, M. J., Curtis, M. J., Hearse, D. J., Campbell, R. W., Janse, M. J., Yellon, D. M., et al. (1988). The Lambeth Conventions: guidelines for the study of arrhythmias in ischaemia infarction, and reperfusion. Cardiovascular Research, 22(7), 447–455.
Fu, J. H., Zheng, Y. Q., Li, P., Li, X. Z., Shang, X. H., & Liu, J. X. (2013). Hawthorn leaves flavonoids decreases inflammation related to acute myocardial ischemia/reperfusion in anesthetized dogs. Chinese Journal of Integrative Medicine, 19(8), 582–588.
Mao, G. X., Zheng, L. D., Cao, Y. B., Chen, Z. M., Lv, Y. D., Wang, Y. Z., et al. (2012). Antiaging effect of pine pollen in human diploid fibroblasts and in a mouse model induced by d-galactose. Oxidative Medicine and Cellular Longevity, 2012, 750963.
Wang, X., Zhao, Q., Huang, H., Tang, Y., Xiao, J., Dai, Z., et al. (2013). Effect of renal sympathetic denervation on atrial substrate remodeling in ambulatory canines with prolonged atrial pacing. PLoS One, 8(5), e64611.
Burstein, B., Comtois, P., Michael, G., Nishida, K., Villeneuve, L., Yeh, Y. H., et al. (2009). Changes in connexin expression and the atrial fibrillation substrate in congestive heart failure. Circulation Research, 105(12), 1213–1222.
Zhang, W., Ma, X., Zhong, M., Zheng, Z., Li, L., Wang, Z., et al. (2009). Role of the calpain system in pulmonary vein connexin remodeling in dogs with atrial fibrillation. Cardiology, 112(1), 22–30.
Biaggioni, I., Whetsell, W. O., Jobe, J., & Nadeau, J. H. (1994). Baroreflex failure in a patient with central nervous system lesions involving the nucleus tractus solitarii. Hypertension, 23(4), 491–495.
Scheffers, I. J., Kroon, A. A., Schmidli, J., Jordan, J., Tordoir, J. J., Mohaupt, M. G., et al. (2010). Novel baroreflex activation therapy in resistant hypertension: results of a European multi-center feasibility study. Journal of the American College of Cardiology, 56(15), 1254–1258.
Bisognano, J. D., Bakris, G., Nadim, M. K., Sanchez, L., Kroon, A. A., Schafer, J., et al. (2011). Baroreflex activation therapy lowers blood pressure in patients with resistant hypertension: results from the double-blind, randomized, placebo-controlled rheos pivotal trial. Journal of the American College of Cardiology, 58(7), 765–773.
Wustmann, K., Kucera, J. P., Scheffers, I., Mohaupt, M., Kroon, A. A., de Leeuw, P. W., et al. (2009). Effects of chronic baroreceptor stimulation on the autonomic cardiovascular regulation in patients with drug-resistant arterial hypertension. Hypertension, 54(3), 530–536.
Schomig, A. (1990). Catecholamines in myocardial ischemia. Systemic and cardiac release. Circulation, 82(3 Suppl), I13–I22.
Boengler, K., Stahlhofen, S., van de Sand, A., Gres, P., Ruiz-Meana, M., Garcia-Dorado, D., et al. (2009). Presence of connexin 43 in subsarcolemmal, but not in interfibrillar cardiomyocyte mitochondria. Basic Research in Cardiology, 104(2), 141–147.
Bhuiyan, M. I., Islam, M. N., Jung, S. Y., Yoo, H. H., Lee, Y. S., & Jin, C. (2010). Involvement of ceramide in ischemic tolerance induced by preconditioning with sublethal oxygen-glucose deprivation in primary cultured cortical neurons of rats. Biological and Pharmaceutical Bulletin, 33(1), 11–17.
Heinzel, F. R., Luo, Y., Li, X., Boengler, K., Buechert, A., Garcia-Dorado, D., et al. (2005). Impairment of diazoxide-induced formation of reactive oxygen species and loss of cardioprotection in connexin 43 deficient mice. Circulation Research, 97(6), 583–586.
Halladin, N. L. (2015). Oxidative and inflammatory biomarkers of ischemia and reperfusion injuries. Dan Medical Journal, 62(4), B5054.
Korthuis, R. J., Granger, D. N., Townsley, M. I., & Taylor, A. E. (1985). The role of oxygen-derived free radicals in ischemia-induced increases in canine skeletal muscle vascular permeability. Circulation Research, 57(4), 599–609.
Kong, S. S., Liu, J. J., Yu, X. J., Lu, Y., & Zang, W. J. (2012). Protection against ischemia-induced oxidative stress conferred by vagal stimulation in the rat heart: involvement of the AMPK-PKC pathway. International Journal of Molecular Sciences, 13(11), 14311–14325.
Zhang, R., Wugeti, N., Sun, J., Yan, H., Guo, Y., Zhang, L., et al. (2014). Effects of vagus nerve stimulation via cholinergic anti-inflammatory pathway activation on myocardial ischemia/reperfusion injury in canine. International Journal of Clinical Experimental Medicine, 7(9), 2615–2623.
Hamacher-Brady, A., Brady, N. R., & Gottlieb, R. A. (2006). The interplay between pro-death and pro-survival signaling pathways in myocardial ischemia/reperfusion injury: apoptosis meets autophagy. Cardiovascular Drugs and Therapy, 20(6), 445–462.
Gao, M., Zhang, L., Scherlag, B. J., Huang, B., Stavrakis, S., Hou, Y. M., et al. (2015). Low-level vagosympathetic trunk stimulation inhibits atrial fibrillation in a rabbit model of obstructive sleep apnea. Heart Rhythm, 12(4), 818–824.
Stavrakis, S., Humphrey, M. B., Scherlag, B. J., Hu, Y., Jackman, W. M., Nakagawa, H., et al. (2015). Low-level transcutaneous electrical vagus nerve stimulation suppresses atrial fibrillation. Journal of the American College of Cardiology, 65(9), 867–875.
Wang, Z., Yu, L., Wang, S., Huang, B., Liao, K., Saren, G., et al. (2014). Chronic intermittent low-level transcutaneous electrical stimulation of auricular branch of vagus nerve improves left ventricular remodeling in conscious dogs with healed myocardial infarction. Circulation. Heart Failure, 7(6), 1014–1021.
Sheng, X., Scherlag, B. J., Yu, L., Li, S., Ali, R., Zhang, Y., et al. (2011). Prevention and reversal of atrial fibrillation inducibility and autonomic remodeling by low-level vagosympathetic nerve stimulation. Journal of the American College of Cardiology, 57(5), 563–571.
Li, S., Scherlag, B. J., Yu, L., Sheng, X., Zhang, Y., Ali, R., et al. (2009). Low-level vagosympathetic stimulation: a paradox and potential new modality for the treatment of focal atrial fibrillation. Circulation. Arrhythmia and Electrophysiology, 2(6), 645–651.
Yu, L., Scherlag, B. J., Li, S., Sheng, X., Lu, Z., Nakagawa, H., et al. (2011). Low-level vagosympathetic nerve stimulation inhibits atrial fibrillation inducibility: direct evidence by neural recordings from intrinsic cardiac ganglia. Journal of Cardiovascular Electrophysiology, 22(4), 455–463.
Sha, Y., Scherlag, B. J., Yu, L., Sheng, X., Jackman, W. M., Lazzara, R., et al. (2011). Low-level right vagal stimulation: anticholinergic and antiadrenergic effects. Journal of Cardiovascular Electrophysiology, 22(10), 1147–1153.
Shen, M. J., Shinohara, T., Park, H. W., Frick, K., Ice, D. S., Choi, E. K., et al. (2011). Continuous low-level vagus nerve stimulation reduces stellate ganglion nerve activity and paroxysmal atrial tachyarrhythmias in ambulatory canines. Circulation, 123(20), 2204–2212.
Acknowledgments
This research was supported by grant numbers 81470597 and 81570460 from the National Natural Science Foundation of China, grant number 201115061 from the Natural Science Foundation of Jinlin Province, and grant number LY13H020003 from the Nature Science Foundation of Zhejiang Province. The authors hold no financial stake or interest in either of the commercially available diagnostic kits evaluated in this study or any others.
Author information
Authors and Affiliations
Corresponding authors
Ethics declarations
Conflict of interest
All authors declare that they have no conflict of interest.
Additional information
Xia Sheng, Mingxian Chen and Bing Huang contributed equally to this work.
Rights and permissions
About this article
Cite this article
Sheng, X., Chen, M., Huang, B. et al. Cardioprotective effects of low-level carotid baroreceptor stimulation against myocardial ischemia-reperfusion injury in canine model. J Interv Card Electrophysiol 45, 131–140 (2016). https://doi.org/10.1007/s10840-015-0094-1
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s10840-015-0094-1