Abstract
Background
Magnetic navigation system (MNS) ablation was suspected to be less effective and unstable in highly mobile cardiac regions compared to radiofrequency (RF) ablations with manual control (MC). The aim of the study was to compare the (1) lesion size and (2) stability of MNS versus MC during irrigated RF ablation with and without simulated mechanical heart wall motion.
Methods
In a previously validated myocardial phantom, the performance of Navistar RMT Thermocool catheter (Biosense Webster, CA, USA) guided with MNS was compared to manually controlled Navistar irrigated Thermocool catheter (Biosense Webster, CA, USA). The lesion dimensions were compared with the catheter in inferior and superior orientation, with and without 6-mm simulated wall motion. All ablations were performed with 40 W power and 30 ml/ min irrigation for 60 s.
Results
A total of 60 ablations were performed. The mean lesion volumes with MNS and MC were 57.5 ± 7.1 and 58.1 ± 7.1 mm3, respectively, in the inferior catheter orientation (n = 23, p = 0.6), 62.8 ± 9.9 and 64.6 ± 7.6 mm3, respectively, in the superior catheter orientation (n = 16, p = 0.9). With 6-mm simulated wall motion, the mean lesion volumes with MNS and MC were 60.2 ± 2.7 and 42.8 ± 8.4 mm3, respectively, in the inferior catheter orientation (n = 11, p = <0.01*), 74.1 ± 5.8 and 54.2 ± 3.7 mm3, respectively, in the superior catheter orientation (n = 10, p = <0.01*). During 6-mm simulated wall motion, the MC catheter and MNS catheter moved 5.2 ± 0.1 and 0 mm, respectively, in inferior orientation and 5.5 ± 0.1 and 0 mm, respectively, in the superior orientation on the ablation surface.
Conclusions
The lesion dimensions were larger with MNS compared to MC in the presence of simulated wall motion, consistent with greater catheter stability. However, similar lesion dimensions were observed in the stationary model.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
1 Introduction
Magnetic navigation system (MNS) allows remote guidance of ablation catheters during radiofrequency ablation for cardiac arrhythmias. Two powerful external magnets are used to navigate the magnetic-tipped catheter precisely to the destination [1]. The flexible, flaccid catheter navigates by virtue of magnetic pulling forces compared to pushing ones in conventional ablation. Consistent with this feature, MNS was reported to demonstrate a superior safety profile compared to conventional ablation, [2–5] with very low incidence of perforation [6].
However, the efficacy of MNS is debated [7–9]. The main concern has been the lack of adequate lesion creation [5], especially in the presence of cardiac wall motion. In the absence of a major randomized controlled trial comparing MNS with conventional ablation, the evidence base consists of case control and cohort studies, most of which found MNS to be as effective as conventional ablation in various arrhythmias [6, 10]. MNS had a benefit in ablations involving unstable regions of the heart including the papillary muscle, aortic cusp, outflow tracts as well as in hearts with abnormal anatomy such as in patients with congenital heart disease [3, 11]. Nonetheless, inferior outcomes had been reported especially in ventricular tachycardia (VT) ablation in patients with structural heart disease, atrial flutter ablations [2, 8] and atrial fibrillation (AF) ablation when acute end points and late recurrences were assessed [2].
Highly mobile cardiac structures causing lateral sliding movement of the catheter was shown as a cause of inadequate lesion formation during manual radiofrequency (RF) ablation [12]. The MNS catheter has a heavy tip, flexible shaft and is held to the ablation surface only by magnetic force. During rapid excursions such as might be evinced in highly mobile areas of the heart, it was considered a possibility that the catheter tip might skip away from the ablation surface due to inertial effects. However, some investigators claim MNS to be more stable in highly mobile regions and could negate the effects of local wall motion [1, 7]. This has not been demonstrated as yet [1]. The prolonged procedural time which is often cited as a drawback of MNS [4] could either be due to smaller lesion dimensions and hence the need for more number of ablations or it could be due to the operator learning curve associated with a novel system [9, 10]. Considering the fact that the tactile feedback from the catheter tip is absent, the adequacy of lesion size is often questioned [7–9], and the magnetic pulling force instead of pushing force which helps to reduce complications is suspected to limit lesion size as well [2, 3, 5, 8–10].
We hypothesized that lesion size could be smaller in MNS compared to MC ablation (irrigated Thermocool catheter) especially in the presence of simulated heart wall motion. The aims of this study were [1] to compare the lesion size in MNS and MC ablations and [2] to assess the stability of both catheters during simulated wall motion. The ablation dimensions were compared with the catheter in inferior orientation (simulating posterior wall ablation) and in superior orientation (simulating anterior wall ablation) with and without 6-mm simulating mechanical heart wall motion.
The ablations were performed in a previously described in vitro myocardial phantom/gel tank, which was validated by Chik et al. in animal studies [13]. This system comprised of a thermochromic sheet embedded in a solidified gel, which acted as an analogue for the myocardium and supernatant fluid, which provided an analogue for blood. The advantages were the real time visualization of lesion formation, accurate and precise delineation of lesion size and negation of the confounding effect of contact force, which is known to alter lesion size.
2 Methods
RF ablations were performed on the myocardial phantom (Fig. 1) with irrigated MNS and was compared to MC-irrigated RF ablation. Using each system, radiofrequency ablations were delivered under two different experimental settings including stationary phantom (upright and inverted) and with 6-mm simulated wall motion (upright and inverted). Lesion size (depth and width) was then measured for all ablations.
The myocardial phantom was prepared as previously described by Chik et al. [13]. In short, an agar substitute powder when heated up in saline and then allowed to cool formed a solid gel in which the thermochromic sheet was embedded. The impedance of the gel and supernatant fluid was similar to myocardium and blood, respectively. The fluid flow velocity of 55 ml/min and temperature of 37 °C simulated the characteristics of blood flow in vivo. The phantom was sensitive to temperatures between 50 and 75 °C and produced a hue (colour), which changed monotonically with temperature, enabling an isotherm of known temperature to be drawn. Images of the phantom were recorded by a camera (Canon 5DmkII, Canon Inc, Japan) with a 2× teleconverter (CAF BBAR MC-7, Tamron Inc, Japan) and macro lens (USM EF 100 mm, Canon, Japan) giving a sensor image resolution of 30 pixels per mm. Image analysis and hue to temperature assignment were performed using an in-house software (Fig. 2). Due to the presence of a strong magnetic field (0.1 T) in the MNS operating environment, the phantom was made of non-magnetic materials, and the camera and oscillation drive motor were mounted 1.2 m away from the magnetic field area.
2.1 Simulated wall motion
Simulating physiological cardiac wall movements, the ablation surface was able to move in a 6-mm diameter circular motion at 60–80 oscillations per minute (refer to supplementary video). The plane of the circle of motion was the same as the plane of the phantom gel sheet. The catheter support structure was arranged to stabilize the position of the catheter shaft and maintain it during oscillations of the ablation structure.
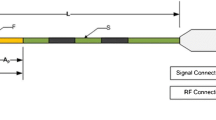
2.2 MNS versus MC radiofrequency ablation
RF ablations were delivered on the gel surface with the catheter tip positioned orthogonal to the surface, and in the plane of the gel sheet. Catheter positioning was confirmed by direct visualization. For the MNS ablations, a guide (Agilis, St Jude Medical) was used to introduce the catheter into the phantom with 120 mm of floating length unsupported by any structure. The MC was supported by Agilis sheath to within 50 mm of the distal tip. The MC was positioned manually whilst the MNS catheter was moved using the magnetic field.
All ablations were performed with a Stockert EP Shuttle Generator, with settings of 40 W power, 60 s duration and a temperature limit of 50 °C. Saline irrigation rate for the catheter tip was 30 ml/min for both systems.
2.3 Images of the ablation and lesion measurements and analysis
During RF ablations, images of the phantom were captured every 5 s. The 50 °C isotherm was drawn on the images by the custom image analysis software, and the isotherm was used to define lesion dimensions (depth and width). Lesion depth was measured from the electrode surface nearest to the ablation zone, to the isotherm of interest. Lesion width was defined as the maximal width of 50 °C isotherm parallel to the electrode gel surface. The volume of individual lesion was calculated using the formulae for half ellipsoid [14].
where v, w and d—volume, width and depth of the lesion, respectively.
2.4 Catheter stability
To measure the catheter stability during ablations on moving targets, the distance between the catheter tip and two fiducial points on the surface was measured at 40-ms intervals (each movie frame at 25 fps) of each ablation (superior and inferior catheter orientation with motion). The distance variation (range and SD) formed the metric used to assess stability (Fig. 3).
a Similar lesion volumes with MNS and MC ablation in the inferior catheter orientation (p = 0.6). b Similar lesion volumes with MNS and MC ablations in the superior catheter orientation (p = 0.9). c Increased lesion volume with MNS ablation compared to MC in the inferior catheter orientation with 6-mm lateral sliding due to the stable catheter position in MNS (p < 0.01*). d Increased lesion volumes with MNS ablations compared to MC in the superior catheter orientation with 6-mm lateral sliding due to the stable catheter position in MNS (p < 0.01*)
2.5 Statistical analysis
Parameters analyzed included lesion depth, width, volume and the extent of catheter lateral movement during simulated wall motion. SPSS 22 software was used to analyze all descriptive and analytical tests. Unpaired Students t test was used to compare the means between the groups.
3 Results
3.1 A total of 60 ablations were performed
In the stationary phantom, the mean lesion volumes with MNS and MC ablations was 57.5 ± 7.1 and 58.1 ± 7.1 mm3 (n = 23, p = 0.6), respectively, in the inferior catheter orientation and 62.8 ± 9.9 and 64.6 ± 7.6 mm3 (n = 16, p = 0.9), respectively, in the superior catheter orientation (Table 1) (refer to supplementary video). The lesion growth kinetics was similar in both catheter types in the stationary platform. The final width with MC and MNS was 5.45 ± 0.1 and 5.55 ± 0.1 mm (n = 23, p = 0.06) and depth was 3.5 ± 0.04 and 3.5 ± 0.1 mm (n = 23, p = 0.9), respectively.
During 6-mm simulated wall motion ablation, the MC catheter and MNS catheter moved 5.2 ± 0.1 and 0 mm, respectively, in inferior orientation and 5.5 ± 0.1 and 0 mm, respectively, in the superior orientation (refer to supplementary video). The mean lesion volume with MNS and MC was 60.2 ± 2.7 and 42.8 ± 8.4 mm3 (n = 11, p < 0.01*), respectively, in the inferior catheter orientation and 74.1 ± 5.8 and 54.2 ± 3.7 mm3 (n = 10, p < 0.01*), respectively, in the superior catheter orientation. The difference in mean lesion volume was due to shallow lesions in the conventional ablation during simulated wall motion both in inferior and superior catheter orientations. The lesion depth was 3.6 ± 0.2 and 2.1 ± 0.1 mm in the inferior catheter orientation, (n = 11, p < 0.001*) and was 3.9 ± 0.1 and 2.9 ± 0.1 mm in the superior catheter orientation with MNS and MC, respectively. On the contrary, the final lesion width was larger with MC. The lesion width was 6.1 ± 0.6 and 5.4 ± 0.1 mm in the inferior catheter orientation (n = 11, p = 0.04*) and was 6.3 ± 0.5 and 5.7 ± 0.2 mm in the superior catheter orientation (n = 10, p = 0.01*) for MC and MNS, respectively. Significant delay in lesion growth up to 20 s occurred in MC with simulated motion. Up to 60 s, the lesion dimensions did not plateau. Width and depth were 24 and 30 % larger at 60 s when compared to 30 s for both catheters (Fig. 4c, d).
a, b Lesion parameters plotted against time in stationary model. The growth curves were similar in both catheter types. The final width (p = 0.06) and depth (p = 0.9) were similar in MC and MNS. c, d Lesion parameters plotted against time in the simulated wall motion model. Significant delay in lesion growth in MC with simulated motion. The final width was larger (p = 0.04*), and the final depth was smaller with MC (p < 0.001*) compared to MNS
The lesion growth kinetics was similar with MNS ablation in both simulated wall motion and stationary models as the catheter was fixed to the surface due to magnetic force without any movement irrespective of the degree of surface sliding (Fig. 4a, b).
4 Discussion
The present findings demonstrate that MNS lesion sizes during simulated wall motion in both inferior and superior catheter orientations were superior to MC ablation owing to the better stability of the MNS catheter. During manual ablation, there was greater dispersion of RF energy on the gel interface due to increased catheter mobility thus creating shallower lesions. There was significant delay in lesion formation with MC during simulated wall motion. In the absence of wall motion, the lesion sizes were similar in the two systems studied (Fig. 5).
a No catheter movement at ablation surface with MNS catheter during RF ablation when 6-mm ablation surface sliding was applied in both inferior and superior catheter orientation. This is due to the strong magnetic pull of the MNS on the catheter approximating it to the ablation surface (Refer online video). b Significant catheter lateral sliding was observed with MC ablation when 6-mm simulated wall motion was applied. (Refer online video)
If MNS was compared to MC ablation in an in vivo setting as well, one could speculate that the MNS lesion size would not be inferior as it had been shown before that the measured contact force (CF) with MNS ablations was not significantly different to that with MC [15]. In majority of conventional ablations, the CF was measured to be between 10 and 20 g [16]. In the TOCATTA study for AF ablation, the mean CF of ablations was 14 g [16]. Using 0.15-T magnetic field, Faddis et al. demonstrated that the CF applied to the catheter tip with MNS was 26.8 g [17]. Thornton et al. also used only lower power with MNS to create similar-sized lesions as conventional ablation in an animal study [18]. This could probably be explained by the efficient energy delivery by virtue of stable contact (Fig. 6).
It had been shown previously that incremental contact force increases lesion size by tenting the endocardium thereby providing more electrode surface tissue contact to facilitate more energy delivery [1, 19]. The myocardial phantom model could not display the effect of varying contact forces on lesion size due to the nature of the gel providing a hard interfacing surface, which eliminated tenting. However, it provided an even platform for both systems (Fig. 7 online version). Even though one could not control for contact force, the similar lesion sizes in both systems without motion suggest that the contact forces were probably similar as well.
The lesion dimensions were similar with MNS and MC ablations without simulated wall motion. This was true in the inferior and superior catheter orientation positions with 40 W power, 30 ml/min irrigation for 60 s. In animal studies with non-irrigated MNS catheter, it was demonstrated that the MNS lesion size was similar to conventional ablation and also with less variability [18]. An AF ablation study by Luthje et al. found similar success rates with MNS and conventional ablation; however, MNS ablations needed more RF current compared to conventional ablation. This could be explained by the lower magnetic field strength of 0.08 T used as opposed to 0.1 T which is the standard practice now [20].
Kalman et al., with the help of intracardiac echocardiography, showed that more than 5 mm of lateral catheter sliding occurred in 18 % of MC ablations [12]. The lesion size was considerably smaller in ablations that showed significant lateral sliding. Lateral catheter sliding could not only affect efficacy of ablation but also could be a safety concern. Posterior tricuspid annulus, which is the ablation site for atrioventricular nodal reentrant tachycardia (AVNRT), had been shown to be a highly mobile area, and excessive catheter motion in this area could cause heart block by inadvertent ablation of the nearby His bundle. In the current study during lateral sliding of ablation surface, the MNS catheter was stable without any movement at the gel interface. This produced precise and larger lesions due to stable catheter contact. This explains Davies et al’s observation that MNS ablations of AVNRT had a lower mean temperature, less temperature variation and less time to junctional tachycardia [1]. It had been shown before in conventional ablation with force-sensing catheter that constant contact force lead to effective lesions [14]. This is consistent with the superior efficacy of MNS we demonstrated in the presence of lateral surface movement, when compared to MC ablations. However, with the MC catheter, lateral sliding resulted in lesions of smaller depth and therefore smaller volumes. Similar to AVNRT ablations, the necessity of precise ablations in other vital structures such as the outflow tracts cannot be overemphasized due to the concern of coronary artery injury [11]. The significant delay in lesion formation up to 20 s in our study with MC in the simulated wall motion model is probably due to dispersion of energy as a result of catheter sliding. The width of lesion eventually at 60 s was larger in MC with 6-mm sliding which could be proportional to the magnitude of simulated wall motion.
The possible reasons for the disparity between the perceived behaviour of lesion size in MNS and what we have shown might include the new advancements in MNS, such as introduction of irrigated catheter, upgrading from two to three magnet catheters and magnetic field strength increment from 0.08 to 0.1 T. All these factors could have contributed to more effective lesion formation in our study. Besides, initial use of MNS involves a significant learning curve of a new technique not only for the operator but also for the catheter lab staff [2, 5]. As lesion size is only one of the factors influencing efficacy of ablation, randomized study needs to be performed to assess parity or superiority of MNS compared to MC ablation.
4.1 Limitations
MNS ablation lesion size was measured only with the vector perpendicular to the surface of ablation, and other angles were not tested. However, in our clinical experience, a good proportion of the MNS in vivo ablations are performed with the vector perpendicular to the endocardium.
This is an in vitro and not an in vivo model; hence, effect of varying contact forces could not be studied. However, earlier studies with this phantom gel have shown that the lesion parameters correlated well with in vivo lesion sizes [13]. As explained above, the contact force measured with MNS was also not inferior to that with MC ablations.
The inverted gel tank model (superior catheter orientation) showed larger lesion sizes for both ablation types as compared to inferior catheter orientation. This was due to the impedance values being slightly lower, which is a consequence of the inverted system physical arrangement. In the upright system, supernatant fluid flows over one face of the gel well only, but in the inverted system, supernatant fluid flows over the upper and lower surface. The inverted model was therefore treated as a separate case in the analysis, and catheter types were compared against each other, which prevented bias.
4.2 Clinical implications
-
1
Owing to better stability, MNS could be particularly useful for precise ablations such as for AVNRT, parahisian accessory pathways, papillary muscle and ablations in close proximity to coronary arteries.
-
2
As the lesion dimensions with MNS ablation were similar or larger compared to that with MC, no augmentation of ablation parameters could be recommended for MNS.
-
3
MC ablations in highly mobile cardiac regions require prolonged ablation time as significant delay in lesion formation could result in ineffective lesions.
5 Conclusion
MNS provided a stable platform for ablations under all conditions tested, without any suggestion of inferior performance when compared with manual catheter ablation. In conditions of simulated wall motion, MNS created larger lesions, owing to its greater stability at the catheter-gel interface. However, as many other factors influence performance of an ablation system one could not speculate on the parity or superiority of MNS compared to manual ablation without randomized controlled trials.
Abbreviations
- MNS:
-
Magnetic navigation system
- MC:
-
Manual control
References
Davis, D. R., Tang, A. S. L., Gollob, M. H., Lemery, R., Green, M. S., & Birnie, D. H. (2008). Remote magnetic navigation-assisted catheter ablation enhances catheter stability and ablation success with lower catheter temperatures. Pacing & Clinical Electrophysiology, 31(7), 893–898.
Bradfield, J., Tung, R., Mandapati, R., Boyle, N. G., & Shivkumar, K. (2012). Catheter ablation utilizing remote magnetic navigation: a review of applications and outcomes. Pacing and Clinical Electrophysiology, 35(8), 1021–1034.
Bauernfeind, T., Akca, F., Schwagten, B., de Groot, N., Van Belle, Y., Valk, S., et al. (2011). The magnetic navigation system allows safety and high efficacy for ablation of arrhythmias. Europace, 13(7), 1015–1021.
Proietti, R., Pecoraro, V., Di Biase, L., Natale, A., Santangeli, P., Viecca, M., et al. (2013). Remote magnetic with open-irrigated catheter vs. manual navigation for ablation of atrial fibrillation: a systematic review and meta-analysis. Europace, 15(9), 1241–1248.
Shurrab, M., Danon, A., Lashevsky, I., Kiss, A., Newman, D., Szili-Torok, T., et al. (2013). Robotically assisted ablation of atrial fibrillation: a systematic review and meta-analysis. International Journal of Cardiology, 169(3), 157–165.
Chun, K. R. J., Wissner, E., Koektuerk, B., Konstantinidou, M., Schmidt, B., Zerm, T., et al. (2010). Remote-controlled magnetic pulmonary vein isolation using a new irrigated-tip catheter in patients with atrial fibrillation. Circulation Arrhythmia & Electrophysiology, 3(5), 458–464.
Schmidt, B., Chun, K. R. J., Tilz, R. R., Koektuerk, B., Ouyang, F., & Kuck, K. H. (2008). Remote navigation systems in electrophysiology. Europace, 10(3), 57–61.
Latcu, D. G., Ricard, P., Zarqane, N., Yaici, K., Rinaldi, J. P., Maluski, A., et al. (2009). Robotic magnetic navigation for ablation of human arrhythmias: initial experience. Archives of Cardiovascular Diseases, 102(5), 419–425.
Miyazaki, S., Shah, A. J., Xhaët, O., Derval, N., Matsuo, S., Wright, M., et al. (2010). Remote magnetic navigation with irrigated tip catheter for ablation of paroxysmal atrial fibrillation. Circulation. Arrhythmia and Electrophysiology, 3(6), 585–589.
Arya, A., Zaker-Shahrak, R., Sommer, P., Bollmann, A., Wetzel, U., Gaspar, T., et al. (2011). Catheter ablation of atrial fibrillation using remote magnetic catheter navigation: a case–control study. Europace, 13(1), 45–50.
Schwagten, B., Szili-Torok, T., Rivero-Ayerza, M., Jessurun, E., Valk, S., & Jordaens, L. (2009). Usefulness of remote magnetic navigation for ablation of ventricular arrhythmias originating from outflow regions. Netherlands Heart Journal, 17(6), 245–249.
Kalman, J. M., Fitzpatrick, A. P., Olgin, J. E., Chin, M. C., Lee, R. J., Scheinman, M. M., et al. (1997). Biophysical characteristics of radiofrequency lesion formation in vivo: dynamics of catheter tip–tissue contact evaluated by intracardiac echocardiography. American heart journal, 133(1), 8–18.
Chik, W. W. B., Barry, M. A., Thavapalachandran, S., Midekin, C., Pouliopoulos, J. I. M., Lim, T. W., et al. (2013). High spatial resolution thermal mapping of radiofrequency ablation lesions using a novel thermochromic liquid crystal myocardial phantom. Journal of Cardiovascular Electrophysiology, 24(11), 1278–1286.
Shah, D. C., Lambert, H., Nakagawa, H., Langenkamp, A., Aeby, N., & Leo, G. (2010). Area under the real-time contact force curve (force–time integral) predicts radiofrequency lesion size in an in vitro contractile model. Journal of Cardiovascular Electrophysiology, 21(9), 1038–1043.
Faddis, M. N., Chen, J., Osborn, J., Talcott, M., Cain, M. E., & Lindsay, B. D. (2003). Magnetic guidance system for cardiac electrophysiologya prospective trial of safety and efficacy in humans. Journal of the American College of Cardiology, 42(11), 1952–1958.
Reddy, V. Y., Shah, D., Kautzner, J., Schmidt, B., Saoudi, N., Herrera, C., et al. (2012). The relationship between contact force and clinical outcome during radiofrequency catheter ablation of atrial fibrillation in the TOCCATA study. Heart rhythm, 9(11), 1789–1795.
Faddis, M. N., Blume, W., Finney, J., Hall, A., Rauch, J., Sell, J., et al. (2002). Novel, magnetically guided catheter for endocardial mapping and radiofrequency catheter ablation. Circulation, 106(23), 2980–2985.
Thornton, A., De Castro, C. B., Van Deel, E., Van Beusekom, H., & Jordaens, L. (2010). An in vivo comparison of radiofrequency cardiac lesions formed by standard and magnetically steered 4 mm tip catheters. Netherlands Heart Journal, 18(2), 66–71.
Gallagher, N., Fear, E. C., Byrd, I. A., & Vigmond, E. J. (2013). Contact geometry affects lesion formation in radio-frequency cardiac catheter ablation. PloS One, 8(9), e73242.
Lüthje, L., Vollmann, D., Seegers, J., Dorenkamp, M., Sohns, C., Hasenfuss, G., et al. (2011). Remote magnetic versus manual catheter navigation for circumferential pulmonary vein ablation in patients with atrial fibrillation. Clinical Research in Cardiology, 100(11), 1003–1011.
Acknowledgments
This study was funded by the Westmead hospital research fund. We thank the staff of the cardiology department.
Conflicts of interest
None of the authors had any conflict of interests.
Author information
Authors and Affiliations
Corresponding author
Additional information
Tony Barry was the co-first author.
Electronic supplementary material
Below is the link to the electronic supplementary material.
(MP4 9984 kb).
(MP4 22677 kb).
(MP4 25800 kb).
(MP4 28206 kb).
Rights and permissions
About this article
Cite this article
Bhaskaran, A., Barry, M.A.(., I. Al Raisi, S. et al. Magnetic guidance versus manual control: comparison of radiofrequency lesion dimensions and evaluation of the effect of heart wall motion in a myocardial phantom. J Interv Card Electrophysiol 44, 1–8 (2015). https://doi.org/10.1007/s10840-015-0023-3
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s10840-015-0023-3