Abstract
Objectives
Disruptive behaviors in children with Autism Spectrum Disorder (ASD) or developmental delay are common, persistent and cause distress to families. Parent–Child Interaction Therapy (PCIT) may be an effective intervention with emerging evidence to support its use for children with at-risk development. We aimed to investigate the effectiveness of standard PCIT for young children (2–4 years) with disruptive behaviors and signs of ASD and/or developmental delay, treated in a real-world clinical setting. We hypothesized that there would be a reduction in disruptive behaviors and for parents, a reduction in depressive symptoms.
Methods
This was a retrospective file-review study of 236 referrals to a toddler clinic over a 17-month period (January 2016 to May 2017). Disruptive child behavior (EBCI Intensity scale and ECBI Problem scale) and maternal depression (EDS score) severity were analyzed across two time conditions (pre-treatment and post-treatment) using linear mixed models with repeated measures, including time, child ASD risk status and their interaction as main effects. An identical linear mixed models with repeated measures analysis was subsequently conducted using clinician identified concern about the child’s development as the between subjects factor.
Results
Disruptive child behavior for children at-risk of autism (high SCQ score) and for those with low SCQ scores, improved on average into the non-clinical range. Parental EDS scores reduced in the both groups, but reduced by a greater degree in the children at-risk of autism (high SCQ) group.
Conclusions
This study suggests that children at-risk of autism and developmental delay should not be excluded from PCIT, an evidence-based intervention for disruptive behaviors, as there is potential benefit for both children and parents.
Highlights
-
Standard PCIT reduced disruptive behavior for children at-risk of autism or developmental delay.
-
Parental EDS scores reduced overall, by a greater degree for parents with a child at-risk of autism.
-
PCIT may be effective for children at-risk of autism or developmental delay, and for their parents’ depressive symptoms.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
The prevalence of disruptive child behaviors including aggression, irritability and non-compliance has been shown to be as high as 50% among children with Autism Spectrum Disorder (ASD) (Lecavalier 2006; Mazurek et al. 2013). Diagnosable behavioral disorders are also known to be common in this group, with a 2013 systematic review finding that 25% of youths with ASD meet diagnostic criteria for either Oppositional Defiant Disorder (ODD) or Conduct Disorder (CD) (Kaat and Lecavalier 2013). Without intervention, disruptive behaviors in children with ASD unfortunately tend to persist, in many cases developing into emotional and behavioral disorders later in childhood (Baker et al. 2003; Maire et al. 2017) and placing the child at increased risk of a range of negative outcomes including hospitalization (Mandell 2008) and greater medication use (Witwer and Lecavalier 2005). Disruptive behaviors in children with ASD can also cause significant levels of distress to families, above and beyond that caused by the child’s cognitive or physical limitations (Baker et al. 2002).
Among children with developmental delay, rates of disruptive behaviors are also high. Baker et al. (2002) found that compared to typically developing preschool children, those with delayed development were three to four times as likely to have a total Child Behavior Checklist (CBCL; Achenbach and Rescorla 2000) score in the clinical range, and their fathers’ were more likely to report higher scores for the externalizing and aggression scales. Conversely, in another study clinic-referred preschoolers with disruptive behaviors were found to be four times more likely to screen positive for developmental delay than preschoolers without disruptive behaviors (Szczepaniak et al. 2013). Significantly, a large population-wide study of 8000 children in the United States indicated that disruptive behaviors among children with developmental delay can commence from as early as 9 months and that they typically worsen as the child reaches school-age (Cheng et al. 2014). These behaviors in children with developmental disabilities have been shown to be associated with poor academic outcomes, psychiatric comorbidity, parental stress and out-of-home placement (Baker et al. 2002; Mcintyre et al. 2002; Swadi and Eapen 2000).
Promisingly, there is emerging evidence that Parent–Child Interaction Therapy (PCIT), a short-term, evidence-based parent-training program designed for children aged 2–7 years with externalizing behaviors (McNeil and Hembree-Kigin 2010; Niec 2018) may be an efficacious and accessible intervention for children with both ASD and/or developmental delay as well as disruptive behaviors. Drawing on attachment theory, social learning theory, and operant conditioning principles (Eyberg 1988), the overarching aim of PCIT is to strengthen the parent–child relationship by enhancing parental warmth and limit setting. The therapy program centers around dyadic parent–child play sessions, with the therapist providing the parent with live in vivo “coaching” through a one-way mirror and blue-tooth head-set microphone. The program is divided into two phases; Child-Directed Interaction (CDI), which aims to increase parental warmth and the quality of the parent–child relationship, and Parent-Directed Interaction (PDI), which aims to enhance child compliance by teaching the parent to give effective commands and follow through with consistent consequences. In the CDI phase, the parent is encouraged to follow the child’s lead, provide specific “labeled” praises for desirable behaviors, reflect the child’s appropriate verbalizations, imitate the child’s play, describe the child’s actions, and to enjoy the interaction. Simultaneously, the parent is encouraged to ignore inappropriate behaviors and to avoid critical statements, questions and commands when speaking with the child. During the PDI phase, the parent is coached to institute a time-out procedure for non-compliance, before gradually using this procedure in the home environment and eventually in public settings as well. Both phases are preceded by a teaching session where the format and expectations of the therapy, including regular daily “homework” practice sessions are emphasized.
Families complete the CDI phase when the clinician determines that the parent has met “mastery” criteria for the CDI skills (i.e., when the parent is observed in a 5-min period of parent–child interaction without coaching to use at least ten labeled praises, ten behavioral descriptions and ten reflections, and to use less than three criticisms, questions or commands). Families then typically move on to the PDI phase of the program. They are considered to have achieved “mastery” of PDI skills when, during a 5-min parent–child interaction, the parent is able to independently give 3–4 “effective” commands and to follow through with consistent consequences for compliance and non-compliance in 75% of cases. Families graduate from the program when they have successfully achieved mastery of CDI and PDI skills (or just CDI skills, if the PDI was not completed), when the parent reports feeling comfortable using the PCIT skills and when the child’s parent-reported behaviors are within the normal range on the Intensity subscale of the Eyberg Child Behavior Inventory (Eyberg and Funderburk 2011).
There is a wealth of evidence for PCIT’s effectiveness (Lieneman et al. 2017; Ward et al. 2016). One meta-analysis showed declines in child externalizing behavior and parental self-reported stress in 23 studies compared to active control and wait-list conditions as well an improvement in positive parent–child interactions (Thomas and Zimmer-Gembeck 2007). In a more recent review, Ward and colleagues reported some of the largest effect sizes in the realm of children’s mental health (i.e., d = 1.65). Importantly, while most of the published outcome data pertaining to PCIT has been conducted in university research clinic settings, there is also evidence for the use of PCIT in community child behavior clinics including a report by members of this team (Bjorseth and Wichstrom 2016; Phillips et al. 2008). A recognized limitation to the benefit of parent training programs is the presence of maternal depressive symptoms (Dempsey et al. 2016; Forgatch and Kjøbli 2016); in one study, PCIT was shown to improve the observed quality of interactions between depressed mothers and their children—despite the children’s behavior being rated as more severe at baseline—but it is unclear if there was any change in parental depressive symptoms (Timmer et al. 2011).
With the accumulation of such a strong empirical evidence base for PCIT, there has been a move in recent years to examine its efficacy in specific groups (Funderburk and Eyberg 2011), including that of children with ASD and developmental delay (McNeil et al. 2019). To date, there have been 11 published case studies demonstrating reductions in disruptive behaviors for children with ASD. This includes case studies of four children with high-functioning ASD and clinically significant externalizing behaviors who showed a reduction in externalizing behaviors with PCIT treatment (Hatamzadeh et al. 2010); three children in a study utilizing a multiple baseline design showed increased compliance and a reduction in disruptive behaviors (Masse et al. 2016); and three mother–child dyads with ASD and variable speech and IQ levels, all of whom showed a reduction in maternal stress as well as subjective reports of child disruptive behaviors (Agazzi et al. 2017). In the only randomized controlled trial of PCIT for children with ASD, 30 mother–child dyads with children aged 3–7 and confirmed ASD diagnosis were randomly allocated to receive the Child-Directed Interaction (CDI) phase of PCIT or to a wait-list control condition. Results showed a significant reduction in both child disruptive behavior and maternal distress for those who received PCIT (Ginn et al. 2017). However, no such benefits were shown in a waitlist control study of 19 young people with high-functioning autism who received PCIT modified to avoid circumscribed areas of interest, and to encourage cooperative play (Solomon et al. 2008).
Available evidence relating to the efficacy of PCIT for children with developmental delay tells an even stronger story. Bagner and Sheinkopf (2010) conducted an open trial of PCIT with 28 children at-risk for developmental delay through prematurity, and found evidence of clinically significant reductions in externalizing behavior problems and increases in compliance, with changes maintained at 4 months follow-up. In another trial of PCIT for 22 young children with mild or moderate intellectual delay, there was a reduction in disruptive behaviors and associated parenting stress, although not overall stress levels (Bagner and Eyberg 2007). In a re-analysis of these two studies, the key role of parental homework was emphasized for treatment efficacy, linking it to greater confidence, lower parenting stress and a reduction in problematic child behaviors (Ros et al. 2016).
Taken together, there is clearly a growing body of evidence to suggest that PCIT is an effective way to address behavioral problems in young children with ASD and developmental delay, with several limitations. First, studies to date have been limited largely to case studies and case series (Agazzi et al. 2013; Armstrong et al. 2014; Armstrong and Kimonis 2012; Lesack et al. 2014) and thus there is a need for outcome studies using larger samples and more robust designs. Second, many of the previously mentioned studies have modified PCIT procedures significantly, making it difficult to assess their fidelity to the original model, or to compare studies directly (Agazzi et al. 2017; Armstrong et al. 2014; Lesack et al. 2014; Solomon et al. 2008). In the larger, more robust studies to date, some have only used components such as the CDI phase (Ginn et al. 2017) or used a fixed number of CDI sessions rather than ensuring parents have mastered the necessary skills before progressing (Bagner and Sheinkopf 2010). Third, the majority of studies to date were conducted in university-based research settings and recruited from general community samples, rather than using referred clinical samples of young children, where there may be competing clinical demands for therapist time and limited resources to allocate to these particularly complex children and families (Bagner and Eyberg 2007; Ginn et al. 2017; Solomon et al. 2008). As such, the impressive effect sizes obtained in research to date may not be applicable to real-world clinical services, especially when the setting is outside of North America and involves children with comorbid disorders (Weisz et al. 2013). Finally, there are documented high rates of maternal depression and parenting stress among parents of children with ASD and/or developmental delay and behavioral issues (Eisenhower et al. 2005; Herring et al. 2006; Yirmiya and Shaked 2005). Only very limited research exists investigating the effects of general parent management training in alleviating depressive symptoms for similar parents (Iida et al. 2018; Tellegen and Sanders 2014), but it is likely there are reciprocal interactions between parental stress, depression, quality of parent–child interactions and parental responses to disruptive behaviors (Karst and Van Hecke 2012). It is important to examine the efficacy of interventions like PCIT in alleviating depressive symptoms for these parents—an avenue of research that to our knowledge has not yet been pursued.
To expand the current evidence base, this retrospective file-review study aimed to investigate the effectiveness of PCIT for young children (2–4 years) with disruptive behaviors and signs of ASD and/or developmental delay, treated in a real-world clinical setting. We hypothesized that (1) children with signs of ASD or developmental delay would show significant reductions in disruptive behavior symptom intensity and that this reduction would be comparable to that seen by children without ASD or developmental delay; (2) parents of children with signs of ASD or developmental delay would show significant improvements in depression symptom severity and that this reduction would be comparable to that seen by children without signs of ASD or developmental delay.
Methods
Participants
This study was conducted as a retrospective file review of children who attended the Karitane Toddler Clinic, a community-based treatment clinic for children aged 14 months to 4 years presenting with disruptive behaviors. All participants were referred to the service by a health professional. All participants received PCIT in unmodified form, conducted by experienced and certified PCIT clinicians (nurses, psychologists and social workers) who were under direct supervision of a PCIT International Level II trainer. The clinic specializes in the delivery of PCIT and provides treatment to a large number of families every year; in a previous publication the clinic was shown to deliver effective treatment (Phillips et al. 2008). The duration of treatment was determined by the family’s progression and mastery of skills, not limited to a set number of sessions. Treatment was delivered according to the PCIT protocol (Funderburk and Eyberg 2011), but due to the younger age of the children seen at the service, in many cases a decision was made to graduate the family after the CDI phase only, rather than completing the CDI and PDI phases, as recommended in the PCIT protocol.
Of the 236 families who completed an initial face-to-face assessment at the clinic during this given time frame, 5 were considered inappropriate for the PCIT intervention, 38 were considered appropriate for treatment but dropped out prior to attending any treatment sessions, and 191 commenced PCIT treatment. There were an additional two families who completed an assessment but were excluded from further analysis because the clinical file was unable to be located. Of the 191 families who commenced PCIT treatment, 55 (29%) commenced treatment but dropped out during the CDI phase of the program and a further 2 (1%) completed the CDI phase but dropped out during the PDI phase. The remaining 134 families met mastery criteria and “graduated” from the treatment program (55 who completed both the CDI and PDI phases and 79 who completed the CDI phase only). Of the 136 families who completed the CDI phase, the average number of CDI coaching sessions was 6.52 (SD = 3.90). Of the 55 families who went on to complete the PDI phase, the average number of PDI coaching sessions was 6.38 (SD = 2.48). Of the 236 families who completed an initial face-to-face assessment at the clinic, the average child age was 34 months (SD = 9.0 months), and 69.8% of children were boys. Around 3/4 of the children were the first born in the family. All of the children were born in Australia and around 70% percent of the children had parents who were in a married or de-facto relationship. Comparison of basic demographic and baseline scores on main study variables showed no significant differences between those who completed treatment and those who dropped out following the initial assessment session (ps < 0.05).
Procedures
The first study author extracted information from the clinical files of all children who accessed the service for a face-to-face initial assessment appointment during a 17-month period (January 2016 to May 2017) including demographic information such as the age of the child, number of siblings, parental relationship status and occupation; and clinician-identified concerns about developmental delay—documented as specific concerns about a child’s fine motor skills, gross motor skills, hearing or speech. Scores on standardized parent-report screening and assessment measures administered at pre- and post-treatment were also extracted, as were details regarding treatment outcome including the total number of sessions attended.
Measures
The Eyberg Child Behavior Inventory (ECBI; Eyberg and Pincus 1999) is a 36-item parent report measure of disruptive behaviors in children aged 2–7 years of age. The ECBI comprises an “Intensity” score that measures the frequency of disruptive child behaviors, and a “Problem” score that measures the number of behaviors that the parent views as problematic, with higher scores indicating a greater degree of conduct-disordered behavior (Intensity) and a greater impact on the parent (Problem). Raw scores of 131 or more on the Intensity scale (T-score of 60 or more) and 15 or more on the Problem scale (T-score of 60 or more) are considered to be clinically significant. The validity and reliability of the ECBI are well established (Eisenstadt et al. 1994; Funderburk et al. 2003).
The Social Communication Questionnaire (SCQ; Berument et al. 1999; Rutter et al. 2003) is a 40-item, parent-report screening measure based on the Autism Diagnostic Interview (ADI-R) and designed to screen for ASD symptomatology in children aged 2–6 years (Chandler et al. 2007; Charman et al. 2007). The SCQ is validated for children aged 2–6 years, but low specificity means it is not suitable as a diagnostic tool (Allen et al. 2007). A threshold raw score of 16 or more is recommended to minimize the risk of false negatives and indicates the need for a comprehensive evaluation but it has also been suggested that a cut-off of 11 or more may be more clinically useful (Allen et al. 2007; Eaves et al. 2006; Norris and Lecavalier 2010). For our clinic population, the SCQ was administered as a routine screening tool for entry into another study examining the effectiveness of PCIT for children with confirmed autism or callous/unemotional traits.
The Edinburgh Depression Scale (EDS; Cox et al. 1987) is a ten-item self-report measure, originally developed as an instrument to detect depression in the postnatal period, but now has also been validated for use with non-postnatal women with older children (Cox et al. 1996). For English speaking postnatal women, an EPDS score of 13 or more is considered indicative of a probable major depressive episode and a score of 10 or more is thought to indicate probable minor depression (Cox et al. 1987, 1996). It is used routinely as a depression screening tool in our clinical service.
Data Analyses
Bivariate correlations between demographics and main study variables were first conducted to test for covariates. Disruptive child behavior (EBCI Intensity scale and ECBI Problem scale) and maternal depression (EDS score) severity were then analyzed across two time conditions (pre-treatment and post-treatment) using linear mixed models with repeated measures, including time, child ASD risk status and their interaction as main effects. There were two levels of child ASD risk status: “low SCQ score” (children who received an SCQ score of 10 or less) and “high SCQ score” (children who received a SCQ score 11 or more). The model also included age, gender and total number of sessions as covariates. This procedure prevented listwise deletion due to missing data. An identical linear mixed models with repeated measures analysis was subsequently conducted using clinician identified concern about the child’s development as the between subjects factor (i.e., with two levels, “yes, clinician risk identified” and “no, clinician risk not identified”). Following a method described by Selya et al. (2012), effect sizes (Cohen's f2 values) were calculated for each outcome, namely f2 for the interaction effect (with main effects of time, group, child sex, age and sessions); for time (adjusting for group, child sex, age and sessions); and for group (adjusting for group, child sex, age and sessions). According to Cohen’s (1988) guidelines, f2 ≥ 0.02, f2 ≥ 0.15, and f2 ≥ 0.35 represent small, medium, and large effect sizes, respectively.
Results
Bivariate correlations between demographic and main study variables are shown in Table 1. As shown, baseline total SCQ score was not associated with any other study variable. Clinician identified developmental risk was associated with a higher post treatment ECBI Problem scale score. Older child age was associated with higher pre-treatment EDS score and higher pre-treatment ECBI Intensity score, and a higher pre-treatment EDS score was associated with a higher post-treatment EDS score and a higher pre-treatment ECBI Intensity score. There were positive associations between the ECBI Intensity and Problem scale scores at both time points. Given that older child age was positively correlated with pre-treatment EDS and pre-treatment ECBI Intensity scores, and that child gender was positively correlated with post-treatment ECBI Intensity score, the following variables were included as covariates in mixed models linear analyses: child age and child sex.
Of the 236 families who completed an initial face-to-face assessment at the clinic, 98 completed the SCQ. Of these, 78 (79.6%) were classified as having a “low SCQ score” (10 or less) and 20 (20.4%) were classified as having a “high SCQ score” (11 or more). Of the 236 families who completed an initial face-to-face assessment at the clinic, there was information in 162 of the files about whether or not the clinician did or did not have concerns about the child’s development. In 81 cases (50%) the clinician had identified concerns about the child’s development. Table 2 shows the mean ECBI Intensity, ECBI Problem and EDS scores in the low SCQ score group and the high SCQ score group, and of the group for which there was clinician identified developmental risk and the group for which there was no clinician identified developmental risk.
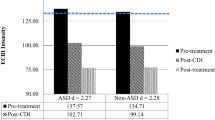
As shown in Table 3, comparison of children with high SCQ scores and children with low SCQ scores revealed significant main effects on all three outcome variables for Time, with large effects observed for both ECBI variables, and a small to moderate effect for EDS score. This indicates that regardless of whether or not the child scored above or below the threshold for possible ASD on the SCQ, at a group level, all children showed significant decreases in the intensity of disruptive child behaviors (moving into the non-clinical range). In addition, all parents improved in terms of the degree to which they found the child’s behaviors to be problematic, and in terms of their own levels of depressive symptomatology. The Time × SCQ group interaction effect was non-significant for the ECBI Intensity (Fig. 1) and ECBI Problem scales (Fig. 2) with negligible effect sizes, suggesting that there were no significant differences between the low SCQ and high SCQ groups in terms of the degree of change on these variables. In contrast, the Time × SCQ group interaction effect was significant for the EDS total score, with a medium effect size, indicating that the degree of change in EDS score shown by the parents of high SCQ scoring children was of a greater magnitude (see Fig. 3).
Similarly, when children with clinician identified developmental risk were compared to children without clinician identified developmental risk, there were significant main effects for time on all three of the study outcome variables, with a large effect size for both ECBI variables, and a small to moderate effect for the EDS (Fig. 4). This indicates that regardless of whether or not there were clinician-identified concerns about the child’s development, at a group level, all children showed significant decreases in the intensity of disruptive child behaviors and all parents had a reduction in terms of the degree to which they rated their child’s behaviors as problematic and their own levels of depressive symptomatology. The Time × Developmental risk interaction effect was non-significant for the ECBI Intensity (Fig. 5) and EDS scales (Fig. 4), with negligible effect sizes, suggesting that there were no significant differences between children who had possible developmental issues in terms of the degree of change on these variables. In contrast, the main effect for Developmental risk was significant for the ECBI problem scale, indicating that at a group level, the parents of children with developmental issues rated their child’s behavior as more problematic than did the parents of children without possible developmental issues, although the effect size was negligible (see Fig. 6).
Discussion
This study investigated the effectiveness of PCIT for children at risk for ASD and/or developmental delay, in a real-world clinic setting. Results showed that following PCIT treatment, children in this sample displayed significant reductions in the intensity of disruptive child behaviors into the non-clinical range, and the degree to which their parents reported these behaviors to be problematic, and their parents showed significant improvements in depressive symptomatology. There were no between group differences on these variables indicating that child behavior and maternal mood gains are not limited to children without possible ASD. Of particular note was the fact that in terms of maternal mood, the degree of change shown by the mothers of children with possible ASD was significantly greater than that shown by the mothers of children who were not identified as being at risk for ASD. In other words, on all domains examined, the children with possible ASD fared just as well as typically developing children, and the improvements were even greater for the high ASD risk group in the case of maternal mood.
Results for children with and children without clinician-identified developmental delay were slightly different to those of ASD. Specifically, while there were no differences in the degree of improvement seen in disruptive child behavior intensity and maternal mood between the children with and without possible developmental delay, parents of children with clinician identified developmental delay did rate their children’s behavior as more problematic. One possibility is that disruptive behaviors might add to the cumulative stress levels for these parents, already higher due to their children’s additional physical and emotional needs, and hence might be more problematic for these families. The effect size was not, however, large and so further research is needed to investigate this in more detail. It is difficult to interpret the significance of this result as the children with clinician-identified developmental delay may be diverse in terms of the severity and type of their delays. Further research might use a structured validated method for assessment of development, to explore the strengths and deficits of these children, capacity to engage in PCIT and the associated challenges for their parents.
Taken together, results of this study are significant because they suggest that PCIT in its standard form can be successfully delivered to children with possible ASD and/or possible developmental delay and that it can be an effective treatment for disruptive child behaviors, with benefits comparable to those seen for typically developing children. Many previous PCIT treatment studies have altered the PCIT treatment protocol to adapt them for children with developmental vulnerabilities, with the implicit assumption that standard PCIT would be ineffective (Holtz et al. 2009). Our findings oppose this view and suggest that standard PCIT can be effective, adding weight to conclusions made by Masse et al. (2007) who discussed the similarities between PCIT and established treatments for ASD such as prominent parental involvement in therapy, strengthening and enriching the parent–child relationship, and intensive systematic compliance training. Masse et al. (2007) suggested that standard PCIT may be a suitable initial treatment for children, which may facilitate further specialized therapy once child compliance has improved and disruptive behavior has lessened. It is important to note that our sample comprised children at-risk of ASD and at-risk for developmental delay. Children with confirmed ASD or severe developmental delays would likely require a range of additional treatments to support their development, in addition to the possible benefits of PCIT for their speech, communication and social skills.
The finding that mothers whose children were identified as being at “high risk” on the SCQ were more likely to show a larger degree of improvement in terms of depressive symptoms is also of note. This result suggests that even though the parents of these at-risk children were more depressed initially, after PCIT treatment, their mood had significantly improved and was to a similar level as the parents of normative children. The finding that initial depression was more severe in parents of children with possible ASD is consistent with other research findings that mothers of children with autism report significantly more parenting stress, even from as early as the toddler years (Eisenhower et al. 2005). Interestingly, other studies have found that the degree of parenting stress relates to the severity of externalizing behaviors rather than the severity of the child’s developmental delay itself (Baker et al. 2003).
The direction of the association between maternal depression/parental stress and child behavior is, however, unclear. As is the case for all children, disruptive child behaviors in children exist in a family and relational context, and are closely connected to the emotional wellbeing of parents (Hauser-Cram et al. 2001). While it can be difficult to tease apart the influence of the broader autism phenotype on parental depression, parents of children with autism do tend to have higher rates of mental disorders compared to parents of typically developing children and children with other disabilities (Yirmiya and Shaked 2005). Mothers and fathers of children with autism also report significantly more parenting stress during the toddler years, which is likely to enhance vulnerability to depression (Eisenhower et al. 2005; Herring et al. 2006). Our study implies that PCIT is an appropriate avenue of intervention for parental depression, even when associated with children’s developmental vulnerabilities and disruptive behavior.
Limitations
While this study has a number of strengths including utilization of a large clinical sample in a real world setting, there are a number of limitations that must be acknowledged. First, given that this was a retrospective file review of treatment delivered at a community based clinic, given the selection criteria for accepting referrals at the service, the sample was likely to be comprised of children without severe ASD or developmental issues. Although severe child developmental issues are not a definite exclusion from the service, those with concerns in multiple areas, especially when these concerns mean that they would be unable to play with their mothers, are typically declined and referred for comprehensive multidisciplinary assessment and specialized early intervention programs. A second limitation was the use of the SCQ as the screening test to identify children at-risk of ASD, rather than the gold-standard diagnostic tool for autism such as the ADOS and the use of clinician-identified developmental delay rather than a validated structured assessment tool. It is probable that some children assessed as at-risk for autism by the SCQ would be assessed as below the diagnostic threshold with a more specific measure such as the ADOS. Third, it is possible that some depressed parents sought individual treatment for their depression, which may have decreased their EDS scores in addition to any benefit from PCIT. However it would be unusual for only the parents of developmentally vulnerable children to seek out external treatment. Fourth, being a retrospective file review study there were several significant limitations to the data accessible. We extracted total scores for the measures obtained rather than item level data, and are unable to calculate Cronbach’s alphas to assess internal consistency for the measures. Also we do not have information about which families met mastery criteria specifically, apart from those who “graduated” from the treatment program after completing PDI. We were not able to objectively evaluate the integrity of the PCIT intervention delivery. PCIT is a standardized program and clinicians at the service typically follow the PCIT treatment protocol closely, but it is possible that individual clinicians strayed from this in some cases. However, this would apply to both groups and hence is unlikely to have influenced the study results.
These limitations notwithstanding, this study adds to the evidence-base for PCIT by investigating its effectiveness for children at-risk of autism and developmental delay, with improvements comparable to normative children in a real-world clinical setting. The improvement in children’s behavior also coincided with a reduction in severity of depressive symptoms in parents, despite higher EDS scores at baseline. This study suggests that PCIT, an evidence-based intervention for disruptive behaviors, should also be offered to children at-risk of autism and developmental delay, as there is potential benefit for both children and parents.
References
Achenbach, T., & Rescorla, L. (2000). Manual for the ASEBA preschool forms and profiles. Burlington: University of Vermont, Research Center for Children, Youth & Families.
Agazzi, H., Tan, R., & Tan, S. Y. (2013). A case study of parent-child interaction therapy in the treatment of autism spectrum disorder. Clinical Case Studies, 12(6), 428–442.
Agazzi, H., Tan, S. Y., Ogg, J., Armstrong, K., & Kirby, R. S. (2017). Does parent-child interaction therapy reduce maternal stress, anxiety, and depression among mothers of children with autism spectrum disorder? Child & Family Behavior Therapy, 39(4), 283–303.
Allen, C. W., Silove, N., Williams, K., & Hutchins, P. (2007). Validity of the social communication questionnaire in assessing risk of autism in preschool children with developmental problems. Journal of Autism and Developmental Disorders, 37(7), 1272–1278.
Armstrong, K., DeLoatche, K., Preece, K., & Agazzi (2014). Combining parent-child interaction therapy and visual supports for the treatment of challenging behavior in a child with autism and intellectual disabilities and comorbid epilepsy. Clinical Case Studies, 14(1), 3–14.
Armstrong, K., & Kimonis, E. (2012). Parent-child interaction therapy for the treatment of Asperger’s disorder in early childhood. Clinical Case Studies, 12(1), 60–72.
Bagner, D., & Sheinkopf, S. (2010). Parenting intervention for externalizing behavior problems in children born premature: an initial examination. Journal of Developmental and Behavioral Pediatrics, 31(3), 209–216.
Bagner, D. M., & Eyberg, S. M. (2007). Parent–child interaction therapy for disruptive behavior in children with mental retardation: a randomized controlled trial. Journal of Clinical Child & Adolescent Psychology, 36(3), 418–429.
Baker, B., Blacher, J., Crnic, K., & Edelbrock, C. (2002). Behavior problems and parenting stress in families of three-year-old children with and without developmental delays. American Journal of Mental Retardation, 107(6), 433–444.
Baker, B., McIntyre, L., Blacher, J., Crnic, K., Edelbrock, C., & Low, C. (2003). Pre-school children with and without developmental delay: behavior problems and parenting stress over time. Journal of Intellectual Disability Research, 47, 217–230.
Berument, S. K., Rutter, M., Lord, C., Pickles, A., & Bailey, A. (1999). Autism screening questionnaire: diagnostic validity. British Journal of Psychiatry, 175, 444–451.
Bjorseth, A., & Wichstrom, L. (2016). Effectiveness of parent-child interaction therapy (PCIT) in the treatment of young children’s behavior problems. A randomized controlled study. PLoS ONE, 11(9), 1–19.
Chandler, S., Charman, T., Baird, G., Simonoff, E., Loucas, T., Meldrum, D., & Pickles, A. (2007). Validation of the social communication questionnaire in a population cohort of children with autism spectrum disorders. Journal of the American Academy of Child & Adolescent Psychiatry, 46(10), 1324–1332.
Charman, T., Baird, G., Simonoff, E., Loucas, T., Chandler, S., Meldrum, D., & Pickles, A. W. (2007). Efficacy of three screening instruments in the identification of autistic-spectrum disorders. British Journal of Psychiatry, 191, 554–559.
Cheng, E. R., Palta, M., Kotelchuck, M., Poehlmann, J., & Witt, W. P. (2014). Cognitive delay and behavior problems prior to school age. Pediatrics, 134(3), e749–e757.
Cohen, J 1988). Statistical power analysis for the behavioral sciences. 2nd ed. Hillsdale, NJ: Lawrence Erlbaum Associates.
Cox, J., Holden, J., & Sagovsky, R. (1987). Detection of postnatal depression. Development of the 10-item Edinburgh postnatal depression scale. British Journal of Psychiatry, 150, 782–786.
Cox, J. L., Chapman, G., Murray, D., & Jones, P. (1996). Validation of the Edinburgh postnatal depression scale (EPDS) in non-postnatal women. Journal of Affective Disorders, 39(3), 185–189.
Dempsey, J., McQuillin, S., Butler, A. M., & Axelrad, M. E. (2016). Maternal depression and parent management training outcomes. Journal of Clinical Psychology in Medical Settings, 23(3), 240–246.
Eaves, L., Wingert, H., Ho, H., & Mickelson, E. (2006). Screening for autism spectrum disorders with the social communication questionnaire. Journal of Developmental and Behavioral Pediatrics, 27(Supplement 2), S95–S103.
Eisenhower, A. S., Baker, B. L., & Blacher, J. (2005). Preschool children with intellectual disability: syndrome specificity, behavior problems, and maternal well-being. Journal of Intellectual Disability Research, 49(9), 657–671.
Eisenstadt, T., McElreath, L., Eyberg, S., & McNeil, C. (1994). Interparent agreement on the Eyberg child behavior inventory. Child & Family Behavior Therapy, 16(1), 21–27.
Eyberg, S. (1988). Parent-child interaction therapy. Child & Family Behavior Therapy, 10(1), 33–46.
Eyberg, S., & Funderburk, B. (2011). Parent-child interaction therapy protocol. Gainesville, FL: PCIT International.
Eyberg, S. M., & Pincus, D. (1999). Eyberg child behavior inventory and Sutter–Eyberg student behavior inventory—revised. Odessa: Psychological Assessment Resources.
Forgatch, M. S., & Kjøbli, J. (2016). Parent management training Oregon model: adapting intervention with rigorous research. Family Process, 55(3), 500–513.
Funderburk, B., & Eyberg, S. (2011). Parent-child interaction therapy. In J. Norcross, G. VandenBos & D. Freedheim (Eds), History of psychotherapy: continuity and change (pp. 415–420). Washington, DC: American Psychological Association.
Funderburk, B., Eyberg, S., Rich, B., & Behar, L. (2003). Further psychometric evaluation of the Eyberg and Behar rating scales for parents and teachers of preschoolers. Early Education and Development, 14(1), 67–81.
Ginn, N. C., Clionsky, L. N., Eyberg, S. M., Warner-Metzger, C., & Abner, J.-P. (2017). Child-directed interaction training for young children with autism spectrum disorders: parent and child outcomes. Journal of Clinical Child & Adolescent Psychology, 46(1), 101–109.
Hatamzadeh, A., Pouretemad, H., & Hassanabadi, H. (2010). The effectiveness of parent-child interaction therapy for children with high functioning autism. Procedia—Social and Behavioral Sciences, 5(2), 994–997.
Hauser-Cram, P., Warfield, M. E., Shonkoff, J. P., Krauss, M., Sayer, A., & Upshur, C. (2001). Children with disabilities: a longitudinal study of child development and parent well-being. Monographs of the Society for Research in Child Development, 66, 1–126.
Herring, S., Gray, K. M., Taffe, J., Tonge, B., Sweeney, D., & Einfeld, S. (2006). Behavior and emotional problems in toddlers with pervasive developmental disorders and developmental delay: associations with parental mental health and family functioning. Journal of Intellectual Disability Research, 50(12), 874–882.
Holtz, C., Carrasco, J., Mattek, R., & Fox, R. (2009). Behavior problems in toddlers with and without developmental delays: comparison of treatment outcomes. Child & Family Behavior Therapy, 31(4), 292–311.
Iida, N., Wada, Y., Yamashita, T., Aoyama, M., Hirai, K., & Narumoto, J. (2018). Effectiveness of parent training in improving stress-coping capability, anxiety, and depression in mothers raising children with autism spectrum disorder. Neuropsychiatric Disease and Treatment, 14, 3355–3362.
Kaat, A. J., & Lecavalier, L. (2013). Disruptive behavior disorders in children and adolescents with autism spectrum disorders: a review of the prevalence, presentation, and treatment. Research in Autism Spectrum Disorders, 7(12), 1579–1594.
Karst, J. S., & Van Hecke, A. V. (2012). Parent and family impact of autism spectrum disorders: a review and proposed model for intervention evaluation. Clinical Child and Family Psychology Review, 15, 247–277.
Lecavalier, L. (2006). Behavioral and emotional problems in young people with pervasive developmental disorders: relative prevalence, effects of subject characteristics, and empirical classification. Journal of Autism and Developmental Disorders, 36, 1101–1114.
Lesack, R., Bearss, K., Celano, M., & Sharp, W. (2014). Parent-child interaction therapy and autism spectrum disorder: adaptations with a child with severe developmental delays. Clinical Practice in Pediatric Psychology, 2(1), 68–82.
Lieneman, C. C., Brabson, L. A., Highlander, A., Wallace, N. M., & McNeil, C. B. (2017). Parent-child interaction therapy: current perspectives. Psychology Research and Behavior Management, 10, 239–256.
Maire, J., Galera, C., Meyer, E., Salla, J., & Michel, G. (2017). Is emotional lability a marker for attention deficit hyperactivity disorder, anxiety and aggression symptoms in preschoolers? Child and Adolescent Mental Health, 22(2), 77–83.
Mandell, D. S. (2008). Psychiatric hospitalization among children with autism spectrum disorders. Journal of Autism and Developmental Disorders, 38, 1059–1065.
Masse, J., McNeil, C., Wagner, S., & Chorney, D. (2007). Parent-child interaction therapy and high functioning autism: a conceptual overview. Journal of Early and Intensive Behavior Intervention, 4(4), 714–735.
Masse, J. J., McNeil, C. B., Wagner, S., & Quetsch, L. B. (2016). Examining the efficacy of parent–child interaction therapy with children on the autism spectrum. Journal of Child and Family Studies, 25(8), 2508–2525.
Mazurek, M. O., Kanne, S. M., & Wodka, E. L. (2013). Physical aggression in children and adolescents with autism spectrum disorders. Research in Autism Spectrum Disorders, 7, 455–465.
Mcintyre, L. L., Blacher, J., & Baker, B. L. (2002). Behavior/mental health problems in young adults with intellectual disability: the impact on families. Journal of Intellectual Disability Research, 46(3), 239–249.
McNeil, C., & Hembree-Kigin, T. (2010). Parent-child interaction therapy. New York, NY: Springer.
McNeil, C., Quetsch, L. B. & Anderson, C. M. (Eds) (2019). Handbook of parent-child interaction therapy for children on the autism spectrum. New York, NY: Springer.
Niec, L. (Ed.) (2018). Handbook of parent-child interaction therapy—innovations and applications for clinical practice. New York, NY: Springer.
Norris, M., & Lecavalier, L. (2010). Screening accuracy of level 2 autism spectrum disorder rating scales. A review of selected instruments. Autism, 14(4), 263–284.
Phillips, J., Morgan, S., Cawthorne, K., & Barnett, B. (2008). Pilot evaluation of parent-child interaction therapy delivered in an Australian community early childhood clinic setting. Australian and New Zealand Journal of Psychiatry, 42, 712–719.
Ros, R., Hernandez, J., Graziano, P. A., & Bagner, D. M. (2016). Parent training for children with or at risk for developmental delay: the role of parental homework completion. Behavior Therapy, 47(1), 1–13.
Rutter, M., Bailey, A., & Lord, C. (2003). The social communication questionnaire: manual. Torrance, CA: Western Psychology Services.
Selya, A., Rose, J., Dierker, L., Hedeker, D., & Mermelstein, R. (2012). A practical guide to calculating Cohen's f(2), a measure of local effect size, from PROC MIXED. Frontiers in Psychology, 3, 111.
Solomon, M., Ono, M., Timmer, S., & Goodlin-Jones, B. (2008). The effectiveness of parent-child interaction therapy for families of children on the autism spectrum. Journal of Autism and Developmental Disorders, 38(9), 1767–1776.
Swadi, H., & Eapen, V. (2000). A controlled study of psychiatric morbidity among developmentally disabled children in the United Arab Emirates. Journal of Tropical Pediatrics, 46(5), 278–281.
Szczepaniak, D., McHenry, M., Nutakki, K., Bauer, N., & Downs, S. (2013). The prevalence of at-risk development in children 30-60 months old presenting with disruptive behaviors. Clinical Pediatrics, 52(10), 942–949.
Tellegen, C. L., & Sanders, M. R. (2014). A randomized controlled trial evaluating a brief parenting program with children with autism spectrum disorders. Journal of Consulting and Clinical Psychology, 82(6), 1193–1200.
Thomas, R., & Zimmer-Gembeck, M. J. (2007). Behavioral outcomes of parent-child interaction therapy and triple P-positive parenting program: a review and meta-analysis. Journal of Abnormal Child Psychology, 35(3), 475–495.
Timmer, S. G., Ho, L. K., Urquiza, A. J., Zebell, N. M., Fernandez Y Garcia, E., & Boys, D. (2011). The effectiveness of parent-child interaction therapy with depressive mothers: the changing relationship as the agent of individual change. Child Psychiatry and Human Development, 42(4), 406–423.
Ward, M. A., Theule, J., & Cheung, K. (2016). Parent-child interaction therapy for child disruptive behavior disorders: a meta-analysis. Child Youth Care Forum, 45, 675–690.
Weisz, J. R., Kuppens, S., Eckshtain, D., Ugueto, A. M., Hawley, K. M., & Jensen-Doss, A. (2013). Performance of evidence-based youth psychotherapies compared with usual clinical care. JAMA Psychiatry, 70(7), 750.
Witwer, A., & Lecavalier, L. (2005). Treatment incidence and patterns in children and adolescents with autism spectrum disorders. Journal of Child and Adolescent Psychopharmacology, 15(4), 671–681.
Yirmiya, N., & Shaked, M. (2005). Psychiatric disorders in parents of children with autism: a meta-analysis. Journal of Child Psychology and Psychiatry and Allied Disciplines, 46(1), 69–83.
Author Contributions
P.M. designed and executed the study, assisted with the data analyses and wrote the paper. J.K. collaborated with the design, analyzed the results and collaborated in the writing of the paper. V.E. collaborated with the design of the study, writing and editing of the manuscript.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of Interest
The authors declare that they have no conflict of interest.
Additional information
Publisher’s note Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
About this article
Cite this article
McInnis, P., Kohlhoff, J. & Eapen, V. Real-world Outcomes of PCIT for Children at Risk of Autism or Developmental Delay. J Child Fam Stud 29, 1701–1711 (2020). https://doi.org/10.1007/s10826-020-01699-0
Published:
Issue Date:
DOI: https://doi.org/10.1007/s10826-020-01699-0