Abstract
Objectives
Despite increasing research in obsessive compulsive disorder (OCD), a great deal still needs to be learned regarding how the disorder manifests in the juvenile population. This study sought to expound on previous research in adults to explore the characteristics of juveniles with OCD who are seeking help via the Internet, namely their OCD symptomology and its impact on disabilty and severity, and the value of a self-perception severity screener.
Methods
This study utilized a population of 157 juveniles who were accessing an online website for program-guided treatment of OCD (ages 7 to 17 years, M = 14.55, SD = 2.33).
Results
Results revealed that the most frequently reported subtype for juveniles was not just right (n = 73, 88.0%) followed by contamination (n = 58, 69.9%) OCD, almost half the participants 45% (n= 46) accurately reported their symptom severity, and over-reporting of symptom severity was associated with an increase in disability compared to both those who accurately reported [t(97) = −2.642, p = 0.010, r = .26] and under-reported [t(97) = −4.184, p < 0.001, r = .39] symptoms.
Conclusions
Clinical implications (e.g., OCD severity ratings, symptom categories, disability ratings and treatment implications), limitations (e.g., lack of confirmed diagnoses and self-reported data), and future directions (i.e., replication studies with juvenile specific measures) are discussed.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Obsessive compulsive disorder (OCD) is a chonic, debilitating mental illness that affects ~2% of the population (Ruscio et al. 2010). OCD is characterized by unwanted obsessions followed by repetitive rituals/compulsions (American Psychiatric Association 2013). OCD often manifests in childhood/adolescence (Pauls et al. 1995) and is more frequently diagnosed in boys, however the diagnosis equals out among gender groups by adulthood (Maj et al. 2002). OCD confers significant disability (Piacentini et al. 2003), and significantly impairs quality of life in children (Lack et al. 2009; Storch et al. 2018). Unfortunately, it often takes nine years for a proper OCD diagnosis and 17 years before effective treatment is received (Jenike 2004), which significantly influences the advancement of OCD severity.
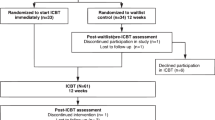
While previous studies have researched the utility of technology in the treatment of OCD more generally (Dettore et al. 2015), less is known about the use of technology with children and adolescents. Studies have addressed the use of technology to supplement traditional OCD treatment; Storch et al. (2011) studied the use of cognitive behavioral therapy (CBT) administered via webcam, and Brezinka (2013) supplemented treatment of children with a video game. Storch et al. (2011) found participants who received therapy via a webcam showed significant improvement compared to waitlist controls, thus suggesting enhancements in access to care, however Brezinka (2013) clearly states that the video game piloted in her study is a supplement not intended to replace the therapist. More recently, Lenhard et al. (2017) conducted a randomized controlled trial of internet-delivered cognitive behavioral therapy (ICBT). Their results showed significant improvement over waitlist controls at posttreatment and follow up.
Though previous research has documented the nature of OCD among treatment seeking clinical samples, virtually nothing is known about those who do not present to a clinician for treatment. We had the unique opportunity to explore OCD symptomology and its impact on disability and severity levels in a population of juveniles with OCD who were accessing an online portal seeking information and self-guided treatment for their OCD. Furthermore, although not a primary focus, no study to date has compared self-perception of symptom severity within a juvenile cohort to a standardized OCD severity measure. Recent research by McIngvale et al. (2017) revealed that adults were accurately able to rate their OCD severity level supporting the utility of a one-item severity screener. Consistent with recent calls in the field of psychological science for replication in research (Open Science Collaboration 2015), this secondary aim was to replicate the findings of McIngvale et al. (2017), to determine whether their findings extend to a juvenile sample. This knowledge would prove helpful in understanding the insight around illness severity of juveniles with OCD and to determine the utility of an internet self-help modality for juveniles.
Method
Participants
The present study included 157 participants ranging from 7 to 17 years of age (M = 14.55, SD = 2.33). The sample was slightly skewed toward female (59.4%), and a majority (75.8%) were Caucasian followed by participants who preferred not to disclose (5.1%) and participants who identified as multiracial (3.8%). The majority of participants identified as Christian (51.8%), followed by participants who preferred not to disclose (10.8%). All participants in the present study self-identified with OCD symptoms and visited the OCD Challenge website. The self-reported onset for OCD symptoms ranged from 1 to 17 years of age (M = 9.74, SD = 3.72). The most frequent method of referral to the OCD Challenge website was the internet (22.9%), followed by Google or a professional (both 19.7%), and a friend (15.3%).
Procedure
Data from The OCD Challenge (ocdchallenge.org/com) were used for this research study. The OCD Challenge is a free self-help website designed as an accessible tool for the management of OCD (McIngvale et al. 2015). The use of this source for data collection and this research project was approved by the institutional review board (IRB) at Baylor University. Participants in the present study were participants of the OCD Challenge program, but no recruitment specific to this study took place. Website users who accepted the terms of agreement (consenting for their data to be used for research), completed the assessments, and met the age criteria were included in this study.
Measures
Demographic data assessed through the OCD Challenge website used in this study included age, gender, ethnicity, religion, website referral source, age of onset of OCD symptoms, a single-item measure used to determine each users’ perception of their OCD severity and OCD symptom subtypes. Self-perception of OCD severity was evaluated before any formal severity measures were assessed by asking users to rate their OCD severity with selection options including: mild, moderate, severe, extreme, or would rather not say; results from this question were then compared to severity ratings calculated from the individual’s first Yale-Brown Obsessive-Compulsive Scale-Self-Report (Y-BOCS-SR) assessment score. Severity self-perception categories did not include the sub-clinical category that is included in the Y-BOCS-SR measurement so both the sub-clinical category and mild catergory were collapsed into the mild category for data analysis.
OCD symptom sub-types were determined through self-selection within the website, where subtypes are listed as challenge areas. Subtypes of OCD included in the website are Contamination, Harm to self, Harm to others, Scrupulosity/Morality, Not Just Right, Sexual Thoughts, Somatic, and Magical/Superstitious. Individuals can select one or multiple OCD subtypes that relate to their OCD by selecting “Yes” to one of the questions listed under the subtype. Some examples of questions found in the contamination subtype of OCD include: “are you excessively bothered by sticky things that you come into contact with?,” “are you excessively concerened or do you feel disgust about any bodily waste or secretions?,” and “are you excessively concerned or worried about dirt, germs, or certain illnesses?” Data analysis was conducted to examine the impact of OCD symptom subtypes on OCD severity and disability levels.
The Yale-Brown Obsessive-Compulsive Scale-Self-Report (Y-BOCS-SR; Goodman et al. 1989; Steketee et al. 1996) is a 10-item empirically supported measure developed to evaluate self-reported OCD severity levels, divided into two categories. Five questions focused on obsessions and five questions on compulsions. Total scores from the Y-BOCS-SR placed individuals into one of five severity ratings: sub-clinical (0–7), mild (8–15), moderate (16–23), severe (24–31), and extreme (32–40) (Goodman et al. 1989; Steketee et al. 1996). Participants’ first Y-BOCS-SR score completed in the assessment phase of the website was used for this research study. Internal consistency of the Y-BOCS-SR within our study sample was excellent with a Cronbach’s alpha of .92.
Disability was evaluated using the Sheehan Disability Scale (SDS; Sheehan et al. 1996). The SDS is a validated scale which determines disability across three domains: work/school, social, and family life. A likert scale is used with category selection for this scale including: not at all, mildly, moderately, markedly, and extreme (Sheehan et al. 1996). Internal consistency of the SDS within our sample was good with a Cronbach’s alpha of .87.
Motivation for change (regarding OCD) was determined through participants self-selecting various items on the motivation for change scale, which was developed by the OCD Challenge to assess participants feelings and beliefs about changing their OCD. This scale is divided into two categories: (1) why challenge/manage my OCD, and (2) why keep my OCD. Participants have the option to self-select supplied examples within each category, and are provided with an option to describe their own reasons to challenge/manage versus keep their OCD. Once the scale is completed, a bar graph is generated depicting users’ motivation levels for fighting versus keeping one’s OCD. This scale was used to assess motivation for change.
Data Analysis
Descriptive statistics were analyzed to determine the most frequently endorsed severity ratings on the Y-BOCS-SR and the one-item severity screener. Similarly, descriptive statistics were utilized to determine the frequency of subtypes endorsed by participants. Next, a series of one way analyses of variance (ANOVAs) were conducted to determine if juveniles endorsing various subtypes of OCD differed with regard to their level of disability on the SDS or severity on the Y-BOCS-SR. Next, Cohen’s Kappa was used to calculate the convergence of Y-BOCS-SR severity category to severity category on the one-item screener. Finally, Analyses of Covariance (ANCOVAs) were calculated to compare the means of participants who over-reported, under-reported, or accurately reported their symptoms after controlling for measured symptom severity category. This analysis used the Y-BOCS-SR severity categories (determined by total score) and the OCD severity self-perception category the individual selected to determine the relationship between self-perception and OCD severity per Y-BOCS-SR, along with relationship to disability and motivation for change in treatment (managing symptoms vs. keeping symptoms). Post hoc comparisons using a Bonferroni procedure were conducted.
Results
Severe was the most frequently endorsed self-rating of symptoms (40.6%) followed by moderate (39.1%) and extreme (11.7%). Participants reported experiencing between one and eight different subtypes of OCD (M = 4.59, SD = 2.09). Further descriptive statistics showed that of the 83 participants who completed subtype questionnaires, the most frequently endorsed subtype was Not Just Right (n = 73, 88.0%) followed by Contamination (n = 58, 69.9%) and Harm to Self (n = 51, 61.4%) (see Table 1 for complete list). Next, a series of one way analyses of variance (ANOVAs) were utilized to determine if juveniles endorsing various subtypes of OCD differed with regard to their level of disability on the SDS or severity on the Y-BOCS-SR. There were significant differences among participants endorsing scrupulosity and harm to others, with no significant differences for participants endorsing the contamination, harm to self, magical superstitious, somatic, and not just right subtypes. Participants endorsing scrupulosity (M = 17.54, SD = 6.73) rated their overall level of disability as significantly more severe than participants not endorsing (M = 13.59, SD = 7.10) scrupulosity [F(1, 82) = 6.73, p = .011]. More specifically, participants endorsing scrupulosity (M = 6.24, SD = 2.54) rated their level of social disability as significantly more severe than participants not endorsing (M = 4.84, SD = 2.85) scrupulosity [F(1, 82) = 5.59, p = .020]. Additionally, participants endorsing scrupulosity (M = 6.15, SD = 2.83) rated their level of family disability as significantly more severe than participants not endorsing (M = 4.51, SD = 2.63) scrupulosity [F(1, 82) = 7.32, p = .008]. There were no significant differences with regard to level of work disability [F(1, 82) = 2.65, p = .108]. Similarly, there were no significant differences as a function of the Y-BOCS-SR for overall severity [F(1, 82) = 2.33, p = .131], obsessions subscale score [F(1, 82) = 2.42, p = .124], or compulsions subscale score [F(1, 82) = 1.53, p = .220] (see Table 2).
Participants endorsing harm to others (M = 17.31, SD = 6.78) rated their overall level of disability as significantly more severe than participants not endorsing (M = 13.69, SD = 7.15) harm to others [F(1, 82) = 5.53, p = .021]. Similar to the results for scrupulosity, participants endorsing harm to others reported significant differences with regard to disability for both the social [F(1, 82) = 4.77, p = .032] and family domains [F(1, 82) = 5.71, p = .019]; however, no significant differences were demonstrated for the work domain [F(1, 82) = 2.26, p = .137] (see Table 3). Finally, participants endorsing harm to others had significantly higher levels of obsessions (M = 13.38, SD = 3.77) than participants not endorsing (M = 11.31, SD = 3.99) harm to others [F(1, 82) = 5.76, p = .019]. No significant differences were found for compulsions [F(1, 82) = 1.13, p = .290] or overall Y-BOCS-SR severity [F(1, 82) = 3.39, p = .069].
Comparisons of the one item self-reported severity perception level (severity perception) to measured Y-BOCS-SR scores (measured symptom severity) revealed that 45% (n= 46) of participants accurately reported severity ratings. Approximately one-third of participants under-reported the severity of their symptoms (n = 35, 34.3%), followed by those who over-reported (n = 21, 20.6%). Further breakdown of comparisons, presented in Table 4, shows that a rating of “severe” had the highest level of convergence (20.6%), followed by “moderate” (15.7%), “extreme” (4.9%), and finally “mild” (3.9%). Convergence was calculated using Cohen’s kappa, which revealed slight (McHugh 2012) agreement (Kappa = 0.20; p = 0.001).
Following the procedures set forth by McIngvale et al. (2017) to replicate the findings with juveniles, the groupings of participants who over-reported, under-reported, or accurately reported their symptoms were used, and comparisons of means were calculated using Analyses of Covariance (ANCOVAs) controlling for measured symptom severity category. Analyses examined motivations for change in treatment (managing symptoms vs. keeping symptoms) and disability and post hoc comparisons using a Bonferroni procedure were conducted.
The covariate, measured symptom severity, was significantly related to managing their symptoms [F(1,98) = 4.264, p= 0.042, r = .21]. However, there was no significant effect of illness severity perception on managing symptoms after controlling for measured symptom severity via Y-BOCS-SR [F(2,98) = .696, p= 0.501, partial η2 = .014]. Planned contrasts revealed no significant difference between those who over- and under-reported their symptoms [t(98) = −1.050, p = .296, r = .11] and those who accurately and over-reported their symptoms [t(98) = −.373, p = .710, r = .04]. The covariate, measured symptom severity was significantly related to the motivation for change construct of keeping their symptoms [F(1,98) = 5.299, p= 0.023, r = .23]. There was also no significant effect of illness severity perception on keeping symptoms after controlling for the effect of measured symptom severity via Y-BOCS-SR [F(2,98) = 1.862, p= 0.161, partial η2 = .037]. Planned contrasts revealed no significant difference between those who over- and under-reported symptoms [t(98) = −.006, p = .995, r = .00] and those who accurately and over-reported their symptoms [t(98) = 1.349, p = .181, r = .14] (see Table 5 for means and standard errors).
Disability was measured using the SDS, and was calculated using the total score, as well as the family, social, and work subscales. The covariate, measured symptom severity was significantly related to overall disability [F(1,97) = 97.968, p< 0.001, r = .71], as well as its subscales work [F(1,97) = 61.812, p< 0.001, r = .62], family [F(1,97) = 63.665, p< 0.001, r = .63], and social [F(1,97) = 71.684, p< 0.001, r = .65]. There was also a significant effect of illness severity perception on overall disability after controlling for measured symptom severity [F(2,97) = 8.866, p< 0.001, partial η2 = .155]. Similar significant results were found for the SDS subscales work [F(2,97) = 5.478, p= 0.006, partial η2 = .101], family [F(2,97) = 6.380, p= 0.002, partial η2 = .116], and social [F(2,97) = 6.261, p= 0.003, partial η2 = .114].
Planned contrasts for overall SDS revealed that over-reporting symptoms was significantly related to an increase in disability compared to both those who accurately reported [t(97) = −2.642, p = 0.010, r = .26] and under-reported [t(97) = −4.184, p < 0.001, r = .39] symptoms. This same pattern largely held true across SDS domains: work [under: t(97) = −3.181, p = 0.002, r = .31], family [accurate: t(97) = −2.216, p = 0.029, r = .22; under: t(97) = −3.546, p = 0.001, r = .34], and social [accurate: t(97) = −2.642, p = 0.010, r = .26; under: t(97) = −3.534, p = 0.001, r = .34]. As reported, the only non-significant difference was ratings on work disability between participants who over-reported and accurately [accurate: t(97) = −1.621, p = 0.108, r = .16] reported their symptoms (see Table 5 for means and standard errors).
Discussion
This study examined clinical characteristics of youth with OCD using internet self-help services. Overall, these individuals seemed to resemble those accessing care in clinical settings in terms of symptom presentation and impairment (Garcia et al. 2009; Geller et al. 2003; Storch et al. 2016). Symptom severity may have been comparable to clinical samples although it is not possible to tell this as no confirming diagnostic procedures were completed, and the Y-BOCS-SR has often been associated with under-reporting symptoms which could be the case herein (Storch et al. 2017).
The most frequently endorsed subtype selected by juveniles was “not just right,” which comports with the existing literature that adults most often endorsed the “not just right” subtype (McIngvale et al. 2015). It may be that these juveniles are seeking help online at high rates, potentially instead of accessing traditional care at a clinic. One speculative thought is that the absence of fear-evoking obsessions on the “not just right” subtype may somehow impact seeking care, perhaps because of diagnostic uncertainty (i.e., is this OCD if there is no fear?). Furthermore, juveniles endorsing the scrupulosity and harm to others subtypes endorsed the greatest levels of disability, which was particularly elevated in the social and family disability subscales. Scrupulosity symptoms have been associated clearly with high levels of impairment in other samples as well (McIngvale et al. 2017).
When compared to adults, juveniles in the present sample fared well rating the severity of their symptoms with roughly 45% accurately reporting their symptom severity. Adults were slightly better at accurately reporting (52 vs. 45%) while juveniles tended to under-report (34 vs. 27%) their symptoms (McIngvale et al. 2017). Over-reporting symptom severity was associated with an increased level of disability, consistent with findings from the adult sample (McIngvale et al. 2017). This finding indicates the potential feasibility of the use of a one-item screener to assess symptoms severity within a juvenile population while also noting the increased likelihood of this population under-reporting their symptoms severity. Its important to note, whether using a quick or validated OCD screener, their tendency to under-report symptom severity in addition to the increase in disability for those who over-report. Furthermore, this study showed that perceived symptom severity did not impact one’s motivation to keep or manage their OCD after controlling for actual severity. As such, participants who accurately reported, under-reported, and over-reported their symptoms, all had similar motivation levels for both managing and keeping their symptoms across groups.
Limitations and Future Research Directions
Several limitations must be noted. Our sample includes individuals who self-identify with OCD, which could not be verified by a clinician. Language and content (including assessments) used throughout the website are not specific to children/adolescents which may have posed a language/education barrier surrounding the content within the program. Specifically, the standard severity measurement used for children, the Children’s Yale-Brown Obsessive-Compulsive Scale (CY-BOCS; Scahill et al. 1997) was not utilized for the juvenile sample, as all participants received the same assessment battery as adults. Additionally, demographics and assessments were self-reported. Future studies should examine our findings through research given in a controlled setting including the use of formal clinician administered assessments specific to a juvenile population as well as parent perspective to confirm juvenile reports.
Within these limitations, there are several study implications. Over 150 children and teenagers took the initiative to log into a website and seek help for their OCD. These youth seemed to be similar in nature to those that present at clinical settings. This underscores the importance of access to care for this population, who in many instances, may not have the resources to receive services, or may be afraid to ask for help. Furthermore, the dearth of appropriate services available for adults seems abundent in comparison to those available to children, particularly those living outside of urban/metro areas or outside of the US. The lessons learned in this study should be utilized by practitioners as they continue to adapt services for juveniles and consider effective modalities to provide treatment to adolescents in a technological age.
References
American Psychiatric Association. (2013). Diagnostic and Statistical Manual of Mental Disorders (5th edn). Arlington: American Psychiatric Association.
Brezinka, V. (2013). Ricky and the Spider—a video game to support cognitive behavioural treatment of children with obsessive-compulsive disorder. Clinical Neuropsychiatry, 10(3), 6–12.
Dettore, D., Pozza, A., & Andersson, G. (2015). Efficacy of technology-delivered cognitive behavioural therapy for OCD versus control conditions, and in comparison with therapist-administered CBT: meta-analysis of randomized controlled trials. Cognitive Behaviour Therapy, 44(3), 190–211.
Garcia, A. M., Freeman, J. B., Himle, M. B., Berman, N. C., Ogata, A. K., Ng, J., & Leonard, H. (2009). Phenomenology of early childhood onset obsessive compulsive disorder. Journal of Psychopathology and Behavioral Assessment, 31, 104–111.
Geller, D. A., Biederman, J., Stewart, S. E., Mullin, B., Farrell, C., Wagner, K. D., & Carpenter, D. (2003). Impact of comorbidity on treatment response to paroxetine in pediatric obsessive-compulsive disorder: is the use of exclusion criteria empirically supported in randomized clinical trials? Journal of Child and Adolescent Pharmacology, 13(1), S19–29.
Goodman, W. K., Price, L. H., Rasmussen, S. A., Mazure, C., Fleischmann, R. L., Hill, C. L., & Charney, D. S. (1989). The Yale-Brown Obsessive Compulsive Scale. I. Development, use, and reliability. Archives of General Psychiatry, 46(11), 1006–1011.
Jenike, M. A. (2004). Clinical practice. Obsessive-compulsive disorder. New England Journal of Medicine, 350(3), 259–265.
Lack, C. W., Storch, E. A., Keeley, M. L., Geffken, G. R., Ricketts, E. D., Murphy, T. K., & Goodman, W. K. (2009). Quality of life in children and adolescents with obsessive-compulsive dsorder: base rates, parent-child agreement, and clinical correlates. Social Psyciatry and Psychiatric Epidemiology, 44, 935–942.
Lenhard, F., Andersson, E., Mataix-Cols, D., Rück, C., Vigerland, D., Högström, J., Hillborg, & Serlachius, E. (2017). Therapist-guided internet-delivered cognitive-behavioral therapy for adolescents with obsessive-compulsive disorder: a randomized controlled trial. Journal of the American Academy of Child & Adolescent Psychiatry, 56, 10–19.
Maj, M., Sartorius, N., Okasha, A. & Zohar, J. (Eds.) (2002). Obsessive-compulsive disorder (2nd edn). Hoboken: John Wiley & Sons.
McHugh, M. (2012). Interrater reliability: the kappa statistic. Biochemia Medica, 22, 276–282.
McIngvale, E., Rufino, K. A., Katz, J., & Hart, J. (2017). Value of a one item OCD severity perception assessment. Journal of Technology in Behavioral Science, 2(2), 88–93.
McIngvale, E., Bordnick, P. S., & Hart, J. (2015). A self-help website for obsessive compulsive disorder: who is accessing the website?. Journal of Technology in Human Services, 33(2), 191–203.
Open Science Collaboration. (2015). Estimating the reproducibility of psychological science. Science, 349, aac4716.
Pauls, D. L., Alsobrook, J. P., Goodman, W., Rasmussen, S., & Leckman, J. F. (1995). A family study of obsessive-compulsive disorder. American Journal of Psychiatry, 152, 76–84.
Piacentini, J., Bergman, R. L., Keller, M., & McCracken, J. (2003). Functional impairment in children and adolescents with obsessive-compulsive disorder. Journal of Adolescent Psychopharmacology, 13, S61–69.
Ruscio, A. M., Stein, D. J., Chiu, W. T., & Kessler, R. C. (2010). The epidemiology of obsessive-compulsive disorder in the National Comorbidity Survey Replication. Molecular Psychiatry, 15, 53–63.
Scahill, L., Riddle, M. A., McSwiggin-Hardin, M., Ort, S. I., King, R. A., Goodman, W. K., & Leckman, J. (1997). Children's Yale-Brown Obsessive-compulsive Scale: reliability and validity. Journal of the American Academy of Child and Adolescent Psychiatry, 36, 844–852.
Sheehan, D. V., Sheehan, K., & Raj, B. A. (1996). The measurement of disability. International Clinical Psychopharmacology, 11, 89–95.
Steketee, G., Frost, R., & Bogart, K. (1996). The Yale-Brown Obsessive Compulsive Scale: interview versus self-report. Behaviour Research and Therapy, 34, 675–684.
Storch, E. A., Caorino, N. E., Morgan, J. R., Lewin, A. B., Rojas, A., Brauer, L., & Murphy, T. K. (2011). Preliminary investigation of web-camera delivered cognitive-behavioral therapy for youth with obsessive-compulsive disorder. Psychiatry Research, 189, 407–412.
Storch, E. A., Nadeau, J. M., De Nadai, A. S., Cepeda, S. L., Reimann, B. C., Seibell, P., & Kay, B. (2017). Symptom correspondence between clinicians and patients on the Yale-Brown Obsessive Compulsive Scale. Comprehensive Psychiatry, 73, 105–110.
Storch, E. A., Small, B. J., McGuire, J. F., Murphy, T. K., Wilhelm, S., & Geller, D. A. (2018). Quality of life in children and youth with obsessive-compulsive disorder. Journal of Child and Adolescent Psychopharmacology, 28(8), 104–110.
Storch, E. A., Wilhelm, S., Sprich, S., Henin, A., Micco, J., Small, B. J., McGuire, J., & Geller, D. A. (2016). Efficacy of augmentation of cognitive behavior therapy with weight-adjusted D-Cycloserine vs placebo in pediatric obsessive-compulsive disorder: a randomized clinical trial. JAMA Psychiatry, 73, 779–788.
Author Contributions
K.A.R. analyzed the data and wrote parts of the paper. EM designed the study and wrote parts of the paper. E.A.S. collaborated in writing and editing the final manuscript.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of Interest
E.M. is on the board of directors for the International OCD Foundation and the Peace of Mind Foundation. E.A.S. receives research support from NIH and the International OCD Foundation. He has received royalties from Elsevier Publications, Springer Publications, American Psychological Association, Wiley, Inc, and Lawrence Erlbaum. He has served as a consultant for Rijuin Hospital, China and Levo Pharmaceuticals. He is on the Speaker’s Bureau and Scientific Advisory Board for the International OCD Foundation. The remaining author declares that she has no conflict of interest.
Ethical Approval
This study was approved by the IRB at Baylor University. No animals were used in this research.
Informed Consent
All participants provided informed consent prior to participation.
Additional information
Publisher’s note: Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
About this article
Cite this article
Rufino, K.A., McIngvale, E. & Storch, E.A. Internet Help-Seeking Juveniles with OCD: An Examination of Severity, Symptoms, Disability and Motivation. J Child Fam Stud 28, 1052–1058 (2019). https://doi.org/10.1007/s10826-019-01335-6
Published:
Issue Date:
DOI: https://doi.org/10.1007/s10826-019-01335-6