Abstract
Purpose
We aimed to explore how patients make decisions regarding use of preimplantation genetic testing for aneuploidy (PGT-A) for in vitro fertilization (IVF).
Methods
This is a cross-sectional survey at an academic medical center. Three hundred subjects initiating an IVF cycle over 8 weeks were asked to complete a validated survey to determine how they decided whether or not to pursue PGT-A. All patients were previously counseled that the primary goal of PGT-A is to maximize pregnancy rates per embryo transfer. Survey responses were compared between those who elected PGT-A and those who did not with a chi-squared or t test.
Results
Of 191 subjects who completed the survey, 117 (61%) planned PGT-A, while 74 (39%) did not. Among those who decided to undergo PGT-A, 56% stated their primary reason was to have a healthy baby, while 18% chose PGT-A to reduce the incidence of birth defects, and 16% aimed to decrease the risk of miscarriage. Patients who decided not to pursue PGT-A stated they prioritized avoiding the scenario in which they might have no embryos to transfer (36%) or reducing cost (31%). Both groups rated physicians as the single most important source of information in their decision-making (56% vs 68%, p = NS).
Conclusions
Patients who chose to undergo PGT-A have different priorities from those who do not. Many patients planning PGT-A do so for reasons that are not evidence-based. While patients cite physicians as their primary source of information in the decision-making process, rationales for selecting PGT-A are inconsistent with physician counseling.
Similar content being viewed by others
Explore related subjects
Discover the latest articles, news and stories from top researchers in related subjects.Avoid common mistakes on your manuscript.
Introduction
Preimplantation genetic testing for aneuploidy (PGT-A) by analysis of 24-chrosome copy number has been increasingly adopted [1] despite controversy surrounding its utility [2,3,4]. While several studies have suggested the use of PGT-A with blastocyst trophectoderm biopsy increases clinical pregnancy and live birth rates in select populations [5, 6], the Practice Committee of the American Society for Reproductive Medicine (ASRM) asserts that the limited nature of these data leaves the value of PGT-A as a universal screening test undetermined [7]. In theory, transfer of genetically screened euploid embryos should result in increased pregnancy and live birth rates and decreased rates of spontaneous pregnancy loss and viable trisomies [8]. Unfortunately, while genetic testing platforms have advanced considerably [9, 10], there are currently limited data supporting the proposed benefits of blastocyst trophectoderm biopsy with 24-chromosome analysis for PGT-A.
Shared decision-making is a pillar of the provider-patient relationship. However, it hinges on not only the presentation of accurate data on risks and benefits of interventions, but also an understanding of patient preferences [11]. Providers disagree as to the relative benefits of PGT-A with an attendant wide variety in recommendations for or against the use of this technology [12]. As a result, it is likely that patients are receiving conflicting recommendations surrounding the use or disuse of this technology. Furthermore, there are no data describing patient preferences when weighing perceived risks and benefits of PGT-A. We sought to understand how patients make decisions regarding the use of PGT-A in a high-volume academic medical center’s assisted reproductive technology (ART) practice.
Methods
The cross-sectional survey was created at the University of California San Francisco (UCSF) and assessed for clarity and validity by a research group with experience in survey methodology. It was then trialed on 10 patients from the UCSF Center for Reproductive Health for readability and content validity, or the degree to which the survey accurately assessed the factors involved in decision-making surrounding the use of PGT-A. The final survey contained 12 questions and was designed to take no more than 5 min to maximize participation and survey completion. The survey included questions addressing whether or not a subject planned to pursue PGT-A, where/from whom information was obtained to make this decision, their perceived level of knowledge surrounding the use of PGT-A, and how influential various factors were in their decision-making process (rated on a visual scale from not influential/0 to extremely influential/100). Ultimately, subjects were asked to select the decisive factor from a list of potential considerations in their decision-making process.
This 12-question survey was distributed on paper to 300 consecutive patients over an 8-week period at the time of their IVF baseline ultrasound or during an IVF injection class just prior to a planned IVF cycle.
All patients were previously counseled on the benefits, risks, and alternatives of PGT-A on at least three different occasions: (1) in a physician-led seminar, (2) in an individual consultation with their physician, and (3) in an appointment with an in-house genetic counselor. The information given was that PGT-A technology afforded the opportunity to select embryos with the potential to maximize pregnancy rates per embryo transfer. We further emphasized that PGT-A does not confirm a healthy baby or minimize birth defects. Patients planning IVF with or without PGT-A were included while those planning oocyte cryopreservation were excluded. Each subject was invited to participate only once. As the survey was available only in English, non-English speakers were excluded. The study was approved by the UCSF Committee on Human Research.
Statistical analyses were performed using STATA version 14 (Stata Corp., College Station, TX). Statistical significance was defined by two-sided p values < 0.05. Survey responses were compared between those who elected PGT-A and those who did not with a chi-squared or t test, where appropriate.
Results
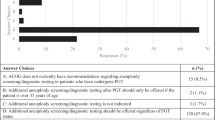
Of 300 patients approached, 191 subjects (64%) completed the survey. One hundred seventeen (61%) planned PGT-A, while 74 (39%) did not. The mean age was identical between groups at 38 ± 5 years. Patients who elected to undergo PGT-A rated themselves more knowledgeable surrounding the technology when compared with those who did not (58 vs 47 on scale 0 to 100, p = 0.02). Patients planning PGT-A rated a desire to have a healthy baby, reduce miscarriage risk, and reduce incidence of birth defects as more influential when compared to those who did not plan to pursue PGT-A. Those forgoing PGT-A rated highly a motivation to reduce time to pregnancy and avoid having no embryos for transfer (Table 1). Among those who decided to undergo PGT-A, 56% stated their primary reason was to have a healthy baby, while 18% chose PGT-A to reduce the incidence of birth defects, and 16% aimed to decrease the risk of miscarriage (Fig. 1). Patients who decided not to pursue PGT-A stated they prioritized avoiding the scenario in which they might have no embryos to transfer (36%) or reducing cost (31%) (Fig. 2). Both groups rated physicians as the single most important source of information in their decision-making surrounding the use of PGT-A (56% PGT-A vs 68% no PGT-A, p = NS).
Discussion
We demonstrate that patients who choose to undergo PGT-A have different priorities from those who do not and that many patients planning PGT-A do so for reasons that are not evidence-based. Furthermore, while patients cite physicians as their primary source of information in the decision-making process, rationales for selecting PGT-A at our institution are inconsistent with the counseling provided by physicians and genetic counselors.
It has been well-documented that patients retain only a fraction of the information imparted by medical providers [13, 14]. This has been demonstrated across medical specialties, despite attempts to improve retention of information by patients with interventions targeting providers [15] and patients alike [16, 17]. While information recall by patients is low, information that is “recalled” is often inaccurate or misconstrued [18]. In the field of reproductive medicine, knowledge about reproductive health has been demonstrated to be suboptimal among patients attending fertility clinics [19]. Reasons for poor retention of medical information include both clinician- and patient-related factors [20]. Poor communication skills by physicians and the use of medical terminology likely exacerbate inattention, fundamental lack of understanding, or preconceived notions held by patients. Regardless of the reason, there is an ethical imperative for clinicians to counsel patients in a manner that they can understand so that patients may be informed consumers of medical services. In the fee-for-service environment of assisted reproduction, this is particularly critical.
Despite explicit counseling that PGT-A does not afford an opportunity to obtain offspring free of genetic disease, three quarters of all patients who selected PGT-A indicated they did so to either have a healthy baby or reduce the risk of birth defects. While the use of PGT-A with transfer of an euploid embryo has the theoretical potential to reduce the incidence of aneuploid live birth from ART, this outcome is relatively uncommon [21] and has not been studied with respect to the use of PGT-A. Certainly, substantially more factors are responsible for the health of a neonate than chromosomal copy number. Furthermore, aneuploidy testing, even if perfectly accurate, does not assess for birth defects nor has it been demonstrated to guarantee a healthy live birth. Improved counseling of patients regarding differences between assessment of chromosome copy number and testing for genetic/non-genetic disease, as well as the multi-factorial etiology for many birth defects, may be needed to reinforce this point.
Approximately one in six individuals planning to undergo PGT-A did so with a stated desire to reduce miscarriage risk. Early pregnancy loss is largely due to aneuploidy, providing biologic plausibility for the use of PGT-A among patients desiring to avoid miscarriage. However, data have not yet demonstrated an association between its use and this outcome. Among patients with recurrent pregnancy loss, one retrospective study demonstrated similar clinical pregnancy and miscarriage rates between individuals who underwent PGT-A and those electing expectant management [22]. Providers need to acknowledge the difference between this theoretical benefit of PGT-A and what the data have shown thus far with respect to PGT-A and miscarriage risk. Additionally, patients undergoing PGT-A rated a desire to reduce time to pregnancy as more important in the decision-making process when compared to those who elected not to use PGT-A and some rated this as the single most important factor influencing their decision. Unfortunately, while time to live birth is the ideal outcome measure, it has not yet been assessed in an RCT [23]. Thus, while PGT-A may improve the chances of live birth per transfer, patients need to understand the difference between this and time to live birth per cycle start.
Patients declined PGT-A for a variety of reasons. Most commonly, these patients cited wanting to avoid the possibility of having no embryo for transfer. The reliance of prior RCTs on randomization at the blastocyst stage [6, 24] precludes a true understanding of how the requirement of blastocyst culture for PGT-A with trophectoderm biopsy impacts live birth rates. Additionally, some patients indicated they chose not to pursue PGT-A due to cost. While the technology is associated with cost, it is unclear if its use affords a cost-savings by reducing transfer number. Additional data are needed to inform patients of the cost-effectiveness of PGT-A [7]. Finally, a minority of patients indicated they did not pursue PGT-A primarily due to concern regarding harm of biopsy to the embryo. However, a non-selection study in which half of embryos were biopsied with subsequent transfer without influence from PGT-A results indicated that blastocyst biopsy did not appear to reduce implantation potential [25], suggesting this concern lacks a basis in evidence.
The current study is limited by the closed nature of the survey questions. While subjects were allowed to write-in additional factors influencing their decision-making surrounding the use of PGT-A, it is possible that respondents did not avail themselves of this opportunity. As a result, additional factors may have played a role but are not discussed. Additionally, while survey content was validated prior to implementation, it is possible that some of the offered rationales for pursuing PGT-A were misunderstood. Pursuing PGT-A to “have a healthy baby” was the most common selection in open-ended questioning during the validation phase of this survey and was thus included in the final survey. While we acknowledge that all patients would likely select a technology that offered a chance to increase the probability of having a healthy baby, it is our practice to explicitly counsel patients that PGT-A does not provide this outcome. This should be clarified in counseling with patients to indicate that PGT-A has not been shown to reduce the incidence of genetic/non-genetic disease.
While the second iteration of PGT-A with 24-chromosome copy number screening offers many theoretical benefits, more RCTs are needed to guide counseling and assist with identification of the appropriate patient population for use of this technology. Furthermore, as demonstrated by this survey, enhanced scrutiny of provider counseling and patient understanding is needed given the discrepancy between the stated content of counseling by providers and patient interpretation. Finally, patient preferences are likely to remain paramount where clinical equipoise exists.
References
De Rycke M, Goossens V, Kokkali G, Meijer-Hoogeveen M, Coonen E, Moutou C. ESHRE PGD Consortium data collection XIV-XV: cycles from January 2011 to December 2012 with pregnancy follow-up to October 2013. Hum Reprod. 2017;32(10):1974–94.
Gleicher N, Barad DH. A review of, and commentary on, the ongoing second clinical introduction of preimplantation genetic screening (PGS) to routine IVF practice. J Assist Reprod Genet. 2012;29(11):1159–66.
Mastenbroek S, Repping S. Preimplantation genetic screening: back to the future. Hum Reprod. 2014;29(9):1846–50.
Paulson RJ. Every last baby out of every last egg: the appropriate goal for fertility treatment in women older than 40 years. Fertil Steril. 2016;105:1443–4.
Yang Z, Liu J, Collins GS, Salem SA, Liu X, Lyle SS, et al. Selection of single blastocysts for fresh transfer via standard morphology assessment alone and with array CGH for good prognosis IVF patients: results from a randomized pilot study. Mol Cytogenet. 2012;5:24.
Scott RT, Upham KM, Forman EJ, Hong KH, Scott KL, Taylor D, et al. Blastocyst biopsy with comprehensive chromosome screening and fresh embryo transfer significantly increases in vitro fertilization implantation and delivery rates: a randomized controlled trial. Fertil Steril. 2013;100:697–703.
Practice Committee of the American Society for Reproductive Medicine. The use of preimplantation genetic testing for aneuploidy (PGT-A): a committee opinion. Fertil Steril. 2018;109:429–36.
Geraedts J, Sermon K. Preimplantation genetic screening 2.0: the theory. Mol Hum Reprod. 2016;22(8):839–44.
Capalbo A, Treff NR, Cimadomo D, Tao X, Upham K, Ubaldi FM, et al. Comparison of array comparative genomic hybridization and quantitative real-time PCR-based aneuploidy screening of blastocyst biopsies. Eur J Hum Genet. 2015;l23:901–6.
Fiorentino F, Bono S, Biricik A, Nuccitelli A, Cotroneo E, Cottone G, et al. Application of next-generation sequencing technology for comprehensive aneuploidy screening of blastocysts in clinical preimplantation genetic screening cycles. Hum Reprod. 2014;29(12):2802–13.
Stiggelbout AM, Van der Weijden T, De Wit MPT, Frosch D, Legare F, Montori VM, et al. Shared decision making: really putting patients at the centre of healthcare. BMJ. 2012;344:e256. https://doi.org/10.1136/bmj.e256.
Sermon K, Capalbo A, Cohen J, Coonen E, De Rycke M, De Vos A, et al. The why, the how and the when of PGS 2.0: current practices and expert opinions of fertility specialists, molecular biologists, and embryologists. Mol Hum Reprod. 2016;22(8):845–57.
Godwin Y. Do they listen? A review of information retained by patients following consent for reduction mammoplasty. Br J Plast Surg. 2000;53:121–5.
Turner P, Williams C. Informed consent: patients listen and read, but what information do they retain? N Z Med J. 2001;115(1164):U218.
Naini P, Lewis J, Rajanna K, Weir AB 3rd. Evaluation of a method to improve the consent process: improved data retention with stagnant comprehension. J Cancer Educ. 2013;28(1):38–42.
Langdon IJ, Hardin R, Learmonth ID. Informed consent for total hip arthroplasty: does a written information sheet improve recall by patients? Ann R Coll Surg Engl. 2001;84(6):404–8.
Ruiz JG, Andrade AD, Anam R, Lisigurski M, Karanam C, Sharit J. Computer-based programmed instruction did not improve the knowledge retention of medication instructions of individuals with type 2 diabetes mellitus. Diabetes Educ. 2014;40(1):77–88.
Anderson JL, Dodman S, Kopelman M, Fleming A. Patient information recall in a rheumatology clinic. Rheumatol Rehabil. 1979;18:244–55.
Bennett LR, Wiweko B, Bell L, Shafira N, Pangestu M, Adayana IB, et al. Reproductive knowledge and patient education needs among Indonesian women infertility patients attending three fertility clinics. Patient Educ Couns. 2015;98(3):364–9.
Ley P. Memory for medical information. Br J Soc Clin Psychol. 1979;18:245–55.
Hassold T, Hunt P. To err (meiotically) is human: the genesis of human aneuploidy. Nat Rev Genet. 2001;2:280–91.
Murugappan G, Shahine LK, Perfetto CO, Hickok LR, Lathi RB. Intent to treat analysis of in vitro fertilization and preimplantation genetic screening versus expectant management in patients with recurrent pregnancy loss. Hum Reprod. 2016;31:1668–74.
Cedars MI. Fresh versus frozen: initial transfer or cumulative cycle results: how do we interpret results and design studies? Fertil Steril. 2016;106(2):251–6.
Forman EJ, Hong KH, Ferry KM, Tao X, Taylor D, Levy B, et al. In vitro fertilization with single euploid blastocyst transfer: a randomized controlled trial. Fertil Steril. 2013;100:100–7.
Treff NR, Ferry KM, Zhao T, Su J, Forman EJ, Scott RT. Cleavage stage embryo biopsy significantly impairs embryonic reproductive potential while blastocyst biopsy does not: a novel paired analysis of cotransferred biopsied and non-biopsied sibling embryos. Fertil Steril. 2011;96:52.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
The study was approved by the UCSF Committee on Human Research.
Rights and permissions
About this article
Cite this article
Quinn, M.M., Juarez-Hernandez, F., Dunn, M. et al. Decision-making surrounding the use of preimplantation genetic testing for aneuploidy reveals misunderstanding regarding its benefit. J Assist Reprod Genet 35, 2155–2159 (2018). https://doi.org/10.1007/s10815-018-1337-8
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s10815-018-1337-8