Abstract
Purpose
To assess the efficiency of IVM in patients with repeated ART failure due to resistant ovary syndrome or due to deficient oocyte maturation.
Methods
Clinical and laboratory data were obtained retrospectively from 28 patients who underwent 49 cycles of IVM between 2010 and 2017; nine patients had resistant ovary syndrome and 19 patients had repeated deficient oocyte maturation.
Results
Nine patients with resistant ovary syndrome underwent 24 IVM cycles. In those, an average of 11.5 ± 10.4 cumulus-oocyte complexes (COC) was retrieved, and IVM resulted in 3.4 ± 3.1 mature oocytes. After ICSI and transfer of 23 cleavage-stage embryos, eight pregnancies were obtained, resulting in five healthy live births. The live birth rate was 16.7% per started cycle and 33.3% per patient.
Nineteen patients with a history of deficient oocyte maturation underwent 25 IVM cycles. An average of 10.6 ± 9.2 COC was retrieved, and after IVM, 1.3 ± 2.1 oocytes were mature. No mature oocytes were obtained in 11 cycles. In ten cycles with mature oocytes, none of them fertilized after ICSI. Out of four cycles with fertilized oocytes, only one good-quality embryo was obtained. No live births were obtained after IVM in patients with a history of deficient oocyte maturation.
Conclusions
Based on our experience, IVM is a valuable approach in patients with resistant ovary syndrome, but should not be recommended for patients with deficient oocyte maturation.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
In vitro maturation (IVM) of oocytes is an alternative approach to conventional methods of artificial reproductive technologies (cART). The concept of IVM revolves around the capacity of immature oocytes to resume meiosis and acquire developmental competence in vitro, upon release from their antral follicular environment [1]. Both semantically and physiologically, “IVM” implies the incubation in vitro of immature cumulus-oocyte complexes (COC) collected from antral follicles, although variations of the existing definition of IVM have been developed, including the administration of hCG or GnRH agonists as ovulatory trigger in vivo [2], with the objective of enhancing pregnancy and live birth rates after IVM. Although these variations have been the subject of much debate among the scientific community [3, 4] and although hCG administration before the oocyte retrieval may enhance maturation rates in IVM cycles [5], there is no conclusive evidence that hCG priming has an effect on live birth, pregnancy, or miscarriage rates in patients who undergo IVM of immature COC collected from antral follicles [6]. Because of the avoidance of gonadotropin-related side effects, patients with high antral follicle counts with or without a diagnosis of polycystic ovarian syndrome (PCOS) have historically been considered suitable candidates for IVM treatment [7]. Indeed, ovarian hyperstimulation syndrome (OHSS), whether mild, moderate, or severe, has never been reported after IVM, nor has ovarian torsion. Nevertheless, IVM treatment in these patients using currently available IVM culture systems is less efficient than cART, most likely because monophasic IVM systems are suboptimal and a substantial proportion of oocytes that reach metaphase II (MII) stage in vitro do not acquire full cytoplasmic maturation allowing proper embryo development [8].
Some patients present with ovaries that appear to be unresponsive to endogenous and exogenous FSH and constitute a category of patients for whom cART offers poor perspectives. The condition in these patients has been referred to as “resistant ovary syndrome,” a rare disorder characterized by elevated serum levels of FSH and LH, in spite of normal levels of AMH and normal antral follicle counts [9]. The etiology of this heterogeneous condition is potentially genetic or immunologic [10, 11] but remains often unexplained [12]. Reports of IVM in patients with resistant ovary syndrome are scarce and only two live births after non-hCG-triggered IVM for this specific indication have been described [13, 14].
Although controlled ovarian stimulation (COS) will yield mature oocytes in the majority of infertile patients, there are distinct categories of patients in whom mature oocytes cannot be obtained using cART. For the majority of these patients, the prospect of childbirth after cART is poor and oocyte donation or adoption are often the only options. More specifically, some patients produce an unusually high rate of immature oocytes retrieved after COS. These patients exhibit infertility based on an oocyte maturation defect or the so-called oocyte factor causing meiosis to become arrested at various stages of oocyte maturation. Some authors have suggested that these oocyte maturation problems may be related to dysfunctional development of the oocyte in advanced stages of follicular development; therefore, IVM of oocytes has been proposed as a shortcut method to “rescue” the oocytes from the follicular environment [15]. Others have cultured germinal vesicle (GV)-stage oocytes, free from their surrounding cumulus cells, as an alternative strategy for patients showing a high number of immature oocytes after COS (sometimes referred to as “rescue IVM” but often erroneously termed IVM) [16].
In our center, IVM has been applied since 2010, predominantly in patients with PCOS [17], but also, to a much lesser extent, as last-resort treatment in patients with resistant ovary syndrome or with poor oocyte maturation rates after cART. We here describe our experience with IVM for these uncommon indications in order to discuss whether IVM is a realistic approach in these poor prognosis patients.
Material and methods
This is a retrospective case series illustrating our experience with IVM for patients with resistant ovary syndrome and deficient oocyte maturation from 2010 to 2017.
Infertile patients undergoing ART were given the diagnosis of resistant ovary syndrome if they had either (i) normal or elevated serum FSH levels and ovaries that were unresponsive to ovarian stimulation with gonadotropins in spite of a normal antral follicular count (AFC) (≥ 12 AFC) [18] and normal (> 1.1 ng/mL) serum anti-Müllerian hormone (AMH) levels [18] or (ii) elevated serum FSH levels in spite of a normal antral follicular count (AFC) (≥ 12 AFC) [19] and normal (> 1.1 ng/mL) serum anti-Müllerian hormone (AMH) levels. Reference ranges for serum concentrations of AMH and baseline FSH were 0.69–2.27 μg/L [20] and 3.5–12.5 IU/L (Elecsys FSH kit insert, Roche Diagnostics), respectively. Patients with decreased ovarian reserve were excluded.
The diagnosis of “oocyte maturation deficiency” was assigned to patients with at least one previous cART cycle with no mature oocytes or at least two previous cART cycles with 80% or more immature oocytes at oocyte retrieval. We searched our patient database for all IVM cycles in patients with resistant ovary syndrome or maturation deficiency since the start of our IVM program in 2010 and we excluded IVM cycles performed in cancer patients referred for fertility preservation. The so-called rescue IVM cycles (of cumulus cell-free oocytes that have failed to become mature after COS in a cART cycle) were also excluded from this analysis.
The study was approved by the hospital Institutional Review Board (IRB) - B.U.N. 143201835921.
Stimulation protocol
Patients with resistant ovary syndrome
In patients with resistant ovary syndrome and baseline serum FSH levels > 15 IU/L, no ovarian stimulation was performed. Instead, one of the following approaches was selected:
-
(A)
Artificial endometrial preparation was given using oral tablets of 17-beta-estradiol valerate (Progynova; Bayer Schering Pharma, Belgium), followed by a bolus of 5000 or 10,000 IU of hCG (Pregnyl, MSD, The Netherlands), as soon as the endometrium thickness was deemed adequate, as previously described by Grynberg et al. [13].
-
(B)
In a number of cycles, artificial endometrial preparation was given as above, but no ovulation trigger was administered. Briefly, 17-beta-estradiol valerate was administered orally at 2 mg twice daily for 6 days, then increased to 2 mg three times a day for 7 days. Endometrial thickness was measured on day 13 of estradiol valerate administration. If the endometrial thickness reached 7 mm, daily administration of 600 mg micronized vaginal progesterone (Utrogestan, Besins, Belgium) was started on the next day. This type of hormonal preparation is commonly referred to as hormone replacement therapy (HRT).
-
(C)
In some cycles of patients with resistant ovary syndrome, no hormonal preparation was given: follicle aspiration was performed at the patient’s convenience and good-quality embryos ensuing from IVM and ICSI were eventually vitrified. Artificial endometrial priming was subsequently administered to accommodate frozen embryo transfer.
-
(D)
In patients with ovaries resistant to exogenous FSH but normal baseline serum FSH levels (< 15 IU/L), ovarian stimulation with gonadotropins (highly purified human menotropin, Menopur, Ferring, Saint-Prex, Switzerland (HP-hMG) or recombinant FSH (rFSH)) was performed. In a limited number of patients, an ovulation trigger was given.
A detailed description of the stimulation protocol of each patient is presented in Table 3.
Patients with deficient oocyte maturation
Ovarian stimulation was performed according to previously described protocols [17]. In the majority of patients, administration of HP-hMG was started on cycle day 3 of the menstrual period or 5 days after discontinuation of a combined contraceptive pill. Patients were generally given a short course of approximately 3 days of HP-hMG treatment, and in the majority of patients, no exogenous ovulation trigger was given. Some patients had no ovarian stimulation. In a small number of patients, an ovulation trigger of 5000 IU or 10,000 IU hCG (Pregnyl, MSD, Oss, The Netherlands) was used 34–36 h before oocyte retrieval. In all patients described in this study, oocyte retrieval was planned with the diameter of the largest follicle being less than 12 mm. A detailed description of the stimulation protocol of each patient is presented in Table 4.
Oocyte retrieval
Transvaginal oocyte retrieval was performed under local anesthesia using ultrasound guidance with a 17-gauge single-lumen aspiration needle (Cook, Bloomington, USA) with a reduced aspiration pressure of 70 mmHg, as previously described [17]. All visible antral follicles were drained without flushing. The follicular fluid (FF) was collected in culture tubes. COC were isolated from the FF by filtration (70-μm mesh, Falcon), rinsed, and collected in Flushing Medium (Medicult, Origio, Copenhagen, Denmark).
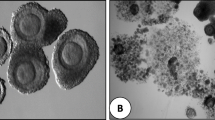
In vitro maturation, ICSI, embryo culture, and vitrification
Cumulus-oocyte complexes were washed in LAG medium (IVM System, Medicult, Origio) and incubated in IVM medium (IVM System, Medicult, Origio) supplemented with 75 mIU/mL HP-hMG (Menopur, Ferring), 100 mIU/mL hCG (Pregnyl, MSD), and 10 mg/mL HSA (Vitrolife, Västra Frölunda, Sweden) for 30 or 40 h in a four-well dish with oil overlay (Ovoil, Vitrolife) in an incubator containing 6% CO2 in air at 37 °C. After denuding, mature oocytes were fertilized by intracytoplasmic sperm injection (ICSI). After ICSI, the oocytes were cultured in sequential media formulations under oil (Ovoil, Vitrolife) until day 3 after ICSI. The cycles were performed in Quinn’s Advantage series (SAGE, Origio) or in Origio sequential series (Origio). Sixteen to 18 h post-insemination, fertilization was assessed by the presence of two pronuclei. On day 3 after ICSI, embryo transfer was performed or, alternatively, all embryos of good morphology were vitrified, using the Vitrification kit media (Irvine Scientific, Santa Ana, USA) and high-security straws (VHS Kit, CryoBiosystem, L’Aigle, France).
Luteal support
Progesterone luteal support with vaginal tablets containing three times 200 mg of micronized progesterone daily (Utrogestan, Besins, Paris, France) was started on the day of fertilization. Luteal support continued until the day of the hCG test and, if pregnant, until 10 weeks of pregnancy.
The pregnancy test was performed routinely on day 12 after embryo transfer. A viability ultrasound scan was performed during the seventh week of gestation. Pregnancy outcome was assessed for each case.
Results
Between 2010 and 2017, 28 patients fulfilling our inclusion criteria underwent at least one IVM treatment cycle in our center, completing 49 IVM cycles in total. The patients’ mean age was 30.6 ± 3.7 years, with 23 (82.1%) patients suffering from primary infertility. Four out of nine patients (44.4%) with resistant ovary syndrome had secondary infertility, whereas all patients with deficient oocyte maturation had primary infertility. The majority of the patients in this study had multiple previous unsuccessful cART treatment cycles. The patients’ baseline characteristics are presented in Tables 1 and 2.
Patients with resistant ovary syndrome
Nine patients presented with resistant ovary syndrome. Nevertheless, four of these nine patients had conceived naturally before the diagnosis of ovarian resistance to FSH was made. The remaining five patients had primary infertility, with no known history or biochemical clues of an autoimmune condition (Table 1). Two patients had a regular cycle of 28 days, three had oligomenorrhea, and four patients presented with secondary amenorrhea. Five out of nine patients had elevated baseline FSH levels ranging from 18.3 to 85.5 IU/L (Table 3) and hence the follicles in these patients were resistant to endogenous FSH. In a further subset of four patients, endogenous FSH levels were normal or only moderately elevated (< 15 IU/L FSH) and ovarian stimulation for ovulation induction or cART had previously been performed. In two of those, ovarian stimulation had initially resulted in follicular growth, oocyte retrieval, and embryo transfer without implantation. Yet subsequent attempts of high-dose stimulation with gonadotropins did not result in any ovarian response. In the remaining two patients, follicle growth did not occur in spite of exogenous gonadotropin administration.
In five patients with ovarian resistance to FSH, cytogenetic analysis showed a normal constitutional female karyotype: 46,XX. Screening for genetic variation (polymorphisms or inactivating mutations) of FSHR using PCR amplification and sequencing of the coding portions of the FSHR gene with self-designed primers was performed in two patients, according to the method used in our center and already described by Santos-Ribeiro et al. [21] (nos. 7 and 9, Table 1); no FSHR variants were identified in patient no. 7, whereas two variants in the FSHR gene were identified in patient no. 9, more specifically c.457G> A, p.Asp153Asn and c.617T> C, p.Leu206Ser. It is unclear whether these variants contribute to the clinical profile of this patient; hence, the findings were classified as variants of unknown significance. In patient no. 8, a diagnosis of polyglandular autoimmune syndrome type 2 was suspected based on the presence of anti-thyroperoxidase, anti-adrenal, and anti-pancreatic antibodies (GADA).
The group of nine patients with ovarian resistance to FSH underwent 24 IVM cycles in total. All patients had normal AFC ranging from 16 to 50 antral follicles and normal or high AMH levels ranging from 1.4 to 8.6 μg/L. Our choice of clinical protocol in patients with resistant ovary syndrome has changed over time, in accordance with published literature and with our own clinical practice. In one cycle, clinical protocol A was performed, as described above, whereas in five cycles (four patients) protocol B was chosen. In five further patients (nine cycles), protocol C was performed, and in the remaining three patients (nine cycles), protocol D was chosen, encompassing three to 11 consecutive days of gonadotropin stimulation because the patients presented with baseline FSH levels below 15 IU/L, but no follicle growth ensued; hCG was administered in two patients (three cycles) 36 h prior to antral follicle aspiration.
On average, egg collection yielded 11.5 ± 10.4 (mean ± SD) COC. In one cycle (one patient), no oocytes were identified. After non-hCG-triggered IVM, on average, 3.5 ± 3.0 mature oocytes were available in 19 cycles (seven patients), and in these patients, the mean oocyte maturation rate was 27.5% (66 MII/240 COC). In hCG-triggered IVM cycles, we observed a maturation rate of 44.4% (16 MII/36 COC) in 4 cycles of three patients. This resulted in an overall maturation rate of 29.7% in our patients with resistant ovary syndrome.
In total, 30 good-quality embryos were obtained on day 3 after ICSI in the 24 IVM cycles. Of those, seven were transferred freshly and 16 were transferred after vitrification warming. This resulted in six clinical pregnancies out of which three resulted in a healthy singleton live birth at term. One further twin pregnancy resulted in live birth of healthy twins who were delivered by cesarean section at 31 weeks’ gestation because of placental abruption. One singleton live birth and the twin live birth originate from non-hCG-triggered IVM, whereas two live births originate from hCG-triggered IVM. Two embryos are still cryopreserved and four embryos did not survive the vitrification warming process (Table 3).
Patients with deficient oocyte maturation
Nineteen patients with a history of deficient oocyte maturation after cART underwent 25 IVM cycles in total. Of those, 18 had primary infertility and one patient had a previous child, after spontaneous conception. Four patients had had an embryo transfer in previous cART treatment, but no pregnancy had been established (Table 2). In four cycles (three patients), IVM treatment was performed according to the protocol described by Vitek et al. [22]. In two cycles, no hormonal priming was given. In 19 cycles (16 patients), ovarian stimulation was performed with daily injections of 75–225 IU HP-hMG between 2 and 10 days, followed by hCG trigger in two cycles and agonist trigger in one cycle. The average oocyte retrieval rate was 10.2 ± 9.6 COC. After incubation in IVM media and denudation, on average, 1.5 ± 2.3 oocytes were at the metaphase II stage, conferring a maturation rate of 13.6% (32 MII/235 COC) in non-hCG-triggered IVM and on average 0.3 ± 0.5 MII oocytes or a maturation rate of 5.0% (1 MII/20 COC) in hCG-triggered IVM, resulting in an overall maturation rate of 12.9%. In 11 out of 25 cycles, no mature oocytes were obtained (Table 4). In the cohort of 14 cycles with mature oocytes after IVM, there was a complete failure of fertilization in ten cycles. Fertilization and embryo development were achieved in four cycles (three patients, non-hCG-triggered IVM). In one of these cycles only, the embryo quality on day 3 after ICSI met the criteria for cryopreservation [23, 24]. However, the only single embryo that was vitrified did not survive the thawing process. Hence, in this series of 25 cycles of IVM of immature COC collected from antral follicles that were performed on indication of suspected deficient oocyte maturation, none of the 19 IVM patients had an embryo transfer.
Discussion
To our knowledge, this is the largest series of well-defined poor prognosis patients in whom IVM treatment was attempted as a last resort in patients with resistant ovary syndrome or deficient oocyte maturation. Ovarian stimulation is the cornerstone of ART; although repeated failure to achieve a live birth after cART is not uncommon in patients of advancing age, poor embryo quality, or implantation failure, there is a subset of infertile patients with an apparently normal antral follicle count who constitute a particular challenge for fertility doctors, because ovarian stimulation in these patients does not result in adequate follicle growth and/or maturation of oocytes. Not only do these patients often undergo multiple fruitless attempts of treatments, a specific diagnosis cannot be identified in the majority of these patients adding up to increased levels of psychological distress. The high degree of perplexity surrounding these rare cases and the perseverance of these patients has resulted in the referral of these poor prognosis patients to our clinic for IVM treatment. IVM has proven to be successful in two cases of poor prognosis patients with empty follicle syndrome where eventually one had a live birth after IVM [15]. In the study presented here, patients with a history of empty follicle syndrome were not included.
The association of primary amenorrhea, gonadotropin levels in the menopausal range, and the presence of a normal number of antral follicles as documented on ultrasound scan or serum analysis of AMH levels has previously been described as resistant ovary syndrome [25] or Savage syndrome [9] and should not be confounded with primary ovarian insufficiency, which is characterized by a low number of antral follicles and low or undetectable serum levels of AMH. The etiology remains often unknown, but the condition is heterogeneous as illustrated by the case series reported here, as none of the patients presented with primary amenorrhea, some had normal baseline FSH levels, and some had secondary infertility. In four out of nine patients with FSH resistance, this condition emerged after a previous spontaneous conception and live birth, which may point towards an acquired problem, possibly of immunological origin, in these patients. Nevertheless, all nine patients exhibited resistance to gonadotropin stimulation while having normal AFC and normal or high AMH serum levels. In patients with elevated baseline serum levels of FSH and LH, the diagnosis of ovarian resistance to FSH can be made at an early stage, but patients with normal baseline levels of FSH often undergo long treatment trajectories. This is illustrated by patient 8, who was 36 years old when she was referred to our center for the evaluation and treatment of primary infertility. This patient had oligomenorrhea, an AFC of 40, and a baseline serum AMH of 2.11 μg/L. She had previously undergone a series of failed attempts of ovarian stimulation for artificial insemination that had been canceled because of absent ovarian response. She had autoimmune thyroid pathology with a suspicion of polyglandular autoimmune syndrome type 2 and she was being treated with DHEA 50 mg/day and hydrocortisone (10-5-5 mg). Seven cycles of immature oocyte retrieval followed by IVM were conducted in this patient, resulting in three fresh embryo transfers, with the last embryo transfer resulting in a live birth. Among the nine patients with resistance to FSH, four patients had primary infertility, with no known history or biochemical clues of an autoimmune condition.
Only two live births after IVM in patients with resistant ovary syndrome have been reported so far [13, 14]. Grynberg described a protocol that combines oocyte retrieval from small antral follicles with HRT for priming of the endometrium, so as to enable fresh embryo transfer. Although satisfactory clinical outcomes have been reported using a similar protocol for IVM in infertile patients without a history of FSH resistance [22], a protocol based on estrogen priming instead of FSH stimulation has not been widely used in IVM clinics because of the suppressive action of estrogen on follicle growth. We adopted the HRT protocol in six cycles (five patients) with FSH resistance, but in a modified version in the majority of cases (without hCG trigger), which resulted in one live birth (which was achieved in the only HRT cycle with hCG trigger). Our concerns with the administration of hCG as ovulation trigger, more specifically the aspiration of a heterogenous cohort of oocytes at different stages of meiotic resumption, reviewed by De Vos et al. [4] led us to omit this hCG bolus in five cycles (four patients); moreover, in view of the successful clinical outcomes of vitrified embryo transfer after IVM [17], we performed egg collection without hormonal pretreatment in nine cycles (five patients). The latter minimal approach strategy, without ovarian stimulation, resulted in one live birth (patient number 7), and a second pregnancy in patient number 9 was a twin gestation that resulted in live birth of healthy twins. One further live birth was achieved after mild HP-hMG pretreatment and hCG-triggered IVM (patient 8). Our results seem to suggest that IVM protocols with hCG triggering and without hCG triggering can both be applied in patients with resistant ovary syndrome, although the number of cases in our series is too small to advocate the preferential use of one approach above another.
In contrast with the reports of Grynberg et al. and Yu Li et al., who described oocyte maturation rates of 80% and 60% respectively [13, 14], the average maturation rate in our series of nine patients is low (29.7%), which could at least in part be due to the absence of an hCG trigger in the majority of our patients. Van Tol et al. identified the presence of FSH receptors, but not of LH receptors, on the somatic compartment of the COC derived from small antral follicles, in normogonadotropic patients [26], which may contribute to meiotic resumption when these COC are incubated in IVM media supplemented with FSH. However, there is no information regarding FSH action in vitro in COC from patients with FSH resistance; moreover, historical observations of Edwards have illustrated that immature oocytes are capable of spontaneous meiotic resumption and maturation upon release from the follicle environment [1] without FSH supplementation in vitro. Recent developments of enhanced in vitro maturation systems that include a pre-maturation phase may boost the efficiency of IVM [27] in patients with resistant ovary syndrome and even in patients suitable for IVM treatment in general.
In sharp contrast with the encouraging results obtained in patients with resistant ovary syndrome, clinical outcomes of IVM cycles in patients with deficient oocyte maturation were disappointingly poor. The complex process of oocyte maturation requires a coordinated cascade of endocrine, molecular, and genetic events, and this process may be impaired by a multitude of different etiologies, resulting in deficient oocyte maturity at any stage in the cascade [15, 28]. From the unreferenced perspective that the precocious release of an immature oocyte from a presumably “hostile” or inhibitory follicular environment may result in proper oocyte maturation in vitro, in patients with a deficient oocyte maturation after cART, these poor prognosis patients have been referred, or self-referred, to the IVM clinic, as a last resort for their hope of own genetic offspring. However, in view of the very poor maturation (overall 12.9%) and fertilization rates in the sample reported here, we believe that IVM in these patients should be attempted with a lot of caution for false hope. Even in those rare cases when an embryo was obtained after IVM, the embryo quality was very poor and none of the 12 cycles included in this report resulted in embryo transfer. These results are in line with previous studies, showing very poor results even with extended oocyte culture [15, 29]. We agree with assumption of other authors that these cases represent intrinsic oocyte problems not influenced by the follicular environment and in vitro maturation media cannot be designed to overcome intrinsic causes of maturation arrest [15]. Although mature oocytes can be obtained after extended in vitro culture of denuded GV oocytes in patients with a high proportion of immature and meiotically resistant oocytes after COS and hCG triggering, this so-called rescue IVM strategy should be considered with caution, as oocytes that reach metaphase II after rescue IVM have a significantly higher percentage of spindle abnormalities and misaligned chromosomes [30].
Our study has a number of limitations. Patient characteristics were not homogeneous and four different protocols of IVM cycles have been used. Moreover, details of previous ovarian stimulation protocols were missing in the medical records of a number of patients with a history of deficient oocyte maturation, although we do not believe that this lack of information would have precluded a correct diagnosis of ovarian resistance to FSH or deficient oocyte maturation in any of the patients. Furthermore, we acknowledge that we did not scrutinize the incidence and etiologies of deficient oocyte maturation; the majority of these poor prognosis patients will proceed to oocyte donation and skip the option of IVM. Hence, we realize that this sample of 19 patients with uncategorized deficient oocyte maturation may not be representative of the total group of patients with deficient oocyte maturation, which precludes firm conclusions regarding the role of IVM in this patient population. The same is true for patients with resistant ovary syndrome because we only described our approaches and outcomes, but not etiologies. Constitutional karyotyping was performed in five out of nine patients and FSHR mutation analysis was performed in two patients only. Further research is needed to unravel the etiologies of this rare condition.
Conclusion
Based on our data, the use of IVM in patients who present with resistant ovary syndrome should be encouraged. On the other hand, IVM should not be recommended for patients with deficient oocyte maturation.
References
Edwards RG. Maturation in vitro of mouse, sheep, cow, pig, rhesus monkey and human ovarian oocytes. Nature. 1965;208:349–51.
Lin YH, Hwang JL, Huang LW, Mu SC, Seow KM, Chung J, et al. Combination of FSH priming and hCG priming for in-vitro maturation of human oocytes. Hum Reprod. 2003;18:1632–6.
Dahan MH, Tan SL, Chung J, Son WY. Clinical definition paper on in vitro maturation of human oocytes. Hum Reprod. 2016;31:1383–6.
De Vos M, Smitz J, Thompson JG, Gilchrist RB. The definition of IVM is clear - variations need defining. Hum Reprod. 2016;31:2411–5.
Chian RC, Buckett WM, Tulandi T, Tan SL. Prospective randomized study of human chorionic gonadotrophin priming before immature oocyte retrieval from unstimulated women with polycystic ovarian syndrome. Hum Reprod. 2000;15:165–70.
Reavey J, Vincent K, Child T, Granne IE. Human chorionic gonadotrophin priming for fertility treatment with in vitro maturation. Cochrane Database Syst Rev. 2016;11:CD008720.
Trounson A, Wood C, Kausche A. In vitro maturation and the fertilization and developmental competence of oocytes recovered from untreated polycystic ovarian patients. Fertil Steril. 1994;62:353–62.
Gilchrist RB, De Vos M, Smitz J, Thompson JG. IVM media are designed specifically to support immature cumulus-oocyte complexes not denuded oocytes that have failed to respond to hyperstimulation. Fertil Steril. 2011;96(2):e141 author reply e142.
Jones GS, De Moraes-Ruehsen M. A new syndrome of amenorrhae in association with hypergonadotropism and apparently normal ovarian follicular apparatus. Am J Obstet Gynecol. 1969;104:597–600.
Haller-Kikkatalo K, Salumets A, Uibo R. Review on autoimmune reactions in female infertility: antibodies to follicle stimulating hormone. Clin Dev Immunol. 2012;2012:762541.
Conway GS, Conway E, Walker C, Hoppner W, Gromoll J, Simoni M. Mutation screening and isoform prevalence of the follicle stimulating hormone receptor gene in women with premature ovarian failure, resistant ovary syndrome and polycystic ovary syndrome. Clin Endocrinol. 1999;51:97–9.
Huhtaniemi I, Alevizaki M. Gonadotrophin resistance. Best Pract Res Clin Endocrinol Metab. 2006;20:561–76.
Grynberg M, Peltoketo H, Christin-Maître S, Poulain M, Bouchard P, Fanchin R. First birth achieved after in vitro maturation of oocytes from a woman endowed with multiple antral follicles unresponsive to follicle-stimulating hormone. J Clin Endocrinol Metab. 2013;98:4493–8.
Li Y, Pan P, Yuan P, Qiu Q, Yang D. Successful live birth in a woman with resistant ovary syndrome following in vitro maturation of oocytes. J Ovarian Res. 2016;9:1–6.
Hourvitz A, Maman E, Brengauz M, Machtinger R, Dor J. In vitro maturation for patients with repeated in vitro fertilization failure due to “oocyte maturation abnormalities”. Fertil Steril. 2010;94:496–501.
Reichman DE, Politch J, Ginsburg ES, Racowsky C. Extended in vitro maturation of immature oocytes from stimulated cycles: an analysis of fertilization potential, embryo development, and reproductive outcomes. J Assist Reprod Genet. 2010;27:347–56.
De Vos M, Ortega-Hrepich C, Albuz FK, Guzman L, Polyzos NP, Smitz J, et al. Clinical outcome of non-hCG-primed oocyte in vitro maturation treatment in patients with polycystic ovaries and polycystic ovary syndrome. Fertil Steril. 2011;96:860–4 e1.
Ferraretti A, La Marca A, Fauser BC, Tarlatzis B, Nargund G, Gianaroli L, et al. ESHRE consensus on the definition of “poor response” to ovarian stimulation for in vitro fertilization: the Bologna criteria. Hum Reprod. 2011;26(7):1616–24.
Melo MA, Garrido N, Alvarez C, Bellver J, Meseguer M, Pellicer A, et al. Antral follicle count (AFC) can be used in the prediction of ovarian response but cannot predict the oocyte/embryo quality or the in vitro fertilization outcome in an egg donation program. Fertil Steril. 2009;91(1):148–56.
Anderson RA, Anckaert E, Bosch E, Dewailly D, Dunlop CE, Fehr D, et al. Prospective study into the value of the automated Elecsys antimüllerian hormone assay for the assessment of the ovarian growing follicle pool. Fertil Steril. 2015;103(4):1074–80.
Santos-Ribeiro S, Polyzos NP, Stouffs K, De Vos M, Seneca S, Tournaye H, et al. Ovarian hyperstimulation syndrome after gonadotropin-releasing hormone agonist triggering and “freeze-all”: in-depth analysis of genetic predisposition. J Assist Reprod Genet. 2015;32:1063–8.
Vitek W, Robins JC. In vitro maturation. The Obstetrician & Gynaecologist. 2013;15:215–9.
Van Landuyt L, Van de Velde H, De Vos A, Haentjens P, Blockeel C, Tournaye H, et al. Influence of cell loss after vitrification or slow-freezing on further in vitro development and implantation of human day 3 embryos. Hum Reprod. 2013;28(11):2943–9.
ALPHA Scientists In Reproductive Medicine; ESHRE Special Interest Group Embryology. Istanbul consensus workshop on embryo assessment: proceedings of an expert meeting. Reprod BioMed Online. 2011;22(6):632–46.
de Moraes-Ruehsen M, Jones GS. Premature ovarian failure. Fertil Steril. 1967;18:440–61.
Van Tol HT, Van Eijk MJT, Mummery CL, Van Den Hurk R, Bevers MM. Influence of FSH and hCG on the resumption of meiosis of bovine oocytes surrounded by cumulus cells connected to membrana granulosa. Mol Reprod Dev. 1996;45:218–24.
Sánchez F, Lolicato F, Romero S, De Vos M, Van Ranst H, Verheyen G, et al. An improved IVM method for cumulus-oocyte complexes from small follicles in polycystic ovary syndrome patients enhances oocyte competence and embryo yield. Hum Reprod. 2017;32:2056–68.
Feng R, Sang Q, Kuang Y, Sun X, Yan Z, Zhang S, et al. Mutations in TUBB8 and human oocyte meiotic arrest. N Engl J Med. 2016;374:223–32.
Hartshorne G, Montgomery S, Klentzeris L. A case of failed oocyte maturation in vivo and in vitro. Fertil Steril. 1999;71:567–70.
Lu Y, Ferrer-Buitrago M, Popovic M, Neupane J, De Vos WH, Lierman S, et al. Patients with a high proportion of immature and meiotically resistant oocytes experience defective nuclear oocyte maturation patterns and impaired pregnancy outcomes. Reprod BioMed Online. 2018;36:396–407.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
The study was approved by the hospital Institutional Review Board (IRB) - B.U.N. 143201835921.
Conflict of interest
A.G., I.S., and J.S. have no conflict of interest. M.D.V. received honoraria for lectures from MSD, Cook Medical, Besins, and Ferring and he is the principal investigator of a research program funded by the FWO Board and the Board of Trustees of the F.R.S.-FNRS (application no. 30443682 submitted as part of the “Excellence of Science - EOS” Call 2017). H.T. reports grants from Cook, during the conduct of the study; grants from Merck Serono; grants from MSD; grants from Goodlife; grants from Roche; grants from Besins; other from Finox; other from Abbott; other from ObsEva, grants from Ferring; grants from Research Fund of Flanders (FWO); and grants from Ferring, outside the submitted work.
Rights and permissions
About this article
Cite this article
Galvão, A., Segers, I., Smitz, J. et al. In vitro maturation (IVM) of oocytes in patients with resistant ovary syndrome and in patients with repeated deficient oocyte maturation. J Assist Reprod Genet 35, 2161–2171 (2018). https://doi.org/10.1007/s10815-018-1317-z
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s10815-018-1317-z