Abstract
Purpose
The purpose of this matched-cohort study was to assess endometrial receptivity to blastocyst implantation in fresh embryo transfer by comparing implantation outcomes of fresh embryo transfer with frozen embryo transfer, where two blastocysts of good quality were transferred in good prognosis patients.
Method(s)
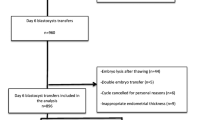
Fresh embryo transfer from intracytoplasmic sperm injection cycles and artificial frozen embryo transfer cycles performed from January 2012 to December 2013 at a private clinic were retrospectively analyzed and the pregnancy, clinical pregnancy, and implantation rates statistically compared. Cycles were stratified and matched according to the blastocyst expansion grade (grade 2, 3, 4, or 5) of the two blastocysts transferred. Five hundred ninety-eight fresh embryo transfer cycles were matched with 545 frozen embryo transfer cycles across four blastocyst cohorts.
Result(s)
In this study of 1143 blastocyst transfer cycles, fresh embryo transfer resulted in reduced pregnancy, clinical pregnancy, and fetal heart implantation rates in all four blastocyst cohorts. The fetal heart implantation rates for fresh embryo transfer ranged from 16.7 % in the grade 2 to 47.3 % in the grade 5 cohort, compared to 23.1 % in the grade 2 to 57.4 % in the grade 5 cohort for frozen embryo transfer. The trends in increasing pregnancy outcomes relative to increasing blastocyst expansion were similar in fresh embryo transfer and frozen embryo transfer.
Conclusion(s)
Blastocysts of good quality transferred in frozen embryo transfer had a significantly greater chance of implantation and clinical pregnancy compared to blastocysts of matched quality transferred in fresh embryo transfer, suggesting reduced endometrial receptivity in fresh embryo transfer.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
After four decades of human-assisted reproductive technology (ART) research and development, a relatively low embryo implantation rate still remains a major point of study. The increasing use of single embryo transfer (SET) to avoid the iatrogenic complications of multi-embryo transfers has increased the importance of achieving optimal embryo implantation. A major part of any in vitro fertilization (IVF) treatment is controlled ovarian stimulation (COS). The purpose of COS is to induce multi-follicular ovarian development to produce oocyte cohorts of suitable size and maturity, thereby promoting the chances of favorable embryo culture and pregnancy outcomes. However, multi-follicular development and final oocyte maturation induction with exogenous hormones may also have adverse consequences for reproductive outcomes because of the altered endogenous hormone conditions produced and the flow-on effect on endometrial development and function [1–6].
Although the effect of elevated estrogen levels may only be circumstantial, the combined supra-physiological levels of progesterone and estrogen often reached at the time of ovulation induction may have significant implications for reproduction outcomes [6]. A premature rise (>1.5 ng/mL) in progesterone may occur in spite of using GnRH agonist or antagonist for pituitary suppression during COS and is often associated with increased ovarian response (i.e., high estrogen levels and follicle numbers). Although the exact cause-and-effect mechanisms of a premature progesterone rise is not fully understood, it has been suggested to involve the advancement of endometrial development and in altered endometrial gene expression [7–10]. In some studies, cycles with elevated progesterone levels before ovulation induction have been associated with reduced pregnancy and live birth outcomes, suggestive of reduced endometrial receptivity and placentation [3, 5].
An instinctual strategy would be to circumvent the complications associated with COS by cryopreserving all embryos, deferring fresh embryo transfer (ET), and using subsequent natural or artificial cycles with frozen-thawed embryo transfer (FET). However, FET pregnancy rates have historically been inferior to those of fresh ET, which relegated FET to a lesser, supportive-only role in most ART programs [11]. The last decade has, however, seen significant improvements in cryopreservation technologies [11, 12]. Moreover, the use of FET increased through necessity during this time, i.e., the increased need for cohort cryopreservation for ovarian hyper-stimulation syndrome (OHSS) prevention and for time to allow to genetically screen embryos, as well as the need for cumulative SET pregnancy rates to be comparable to multi-embryo transfer rates. These changes in attitude and technology saw significant improvement in post-thaw embryo survival and developmental competence, and a concomitant increase in FET pregnancy and live birth outcomes [13–16]. The Society for Reproductive Technology (SART) IVF success rate reports for 2003 and 2011 graphically illustrate these historical changes. The pregnancy rates from FET and fresh ET performed with non-donor oocytes in the 35–37-year female age group increased from 28.3 % (2.7 embryos per transfer) to 35.7 % (1.8 embryos per transfer) and 36.9 % (2.9 embryos per transfer) to 38.4 % (2.1 embryos per transfer), respectively, during the period (http://www.sart.org/, accessed on 8/1/2014). In addition, there was a 102 % increase in FET numbers compared to only a 7.4 % increase in fresh ET numbers over the period 2003 to 2011.
A number of comparative studies, using the fresh vs frozen-thawed ET model to investigate the effects of COS on endometrial receptivity and embryo implantation have been performed [13–16]. The results from the studies suggest that patients undergoing ART may in some cases benefit from deferring fresh ET, cryopreserving all embryos, and performing FET in subsequent cycles [14]. The goal of this study was to add to the evidence that reproductive outcomes of fresh ET were compromised, probably as a result of the use of COS. In this comparatively large retrospective matched-cohort study, pregnancy outcomes in fresh ET were compared with artificial cycle FET in which two matched blastocysts of good quality (grades 2 to 5) were transferred in good prognosis patients.
Materials and methods
Study details
This study was conducted as a retrospective observational study on the pregnancy outcomes from fresh ET and artificial FET cycles, performed during the period January 2012 to December 2013. The study was initiated following the implementation of vitrification as the routine method for cryopreservation in June 2011, and as more than 90 % of the subsequent vitrified-warmed transfers were double blastocyst transfers, only double blastocyst transfers were included in the study. The study was approved by the IRB and ethics committee of the Akdeniz University, Medical Faculty (reference no. 443/2014). The clinical procedures performed in the study were all performed by three resident clinicians. The patient cycles with written consent were extracted without patient identifiers from the ART database of Antalya IVF, with a patient only included once in a group and all patients having no intrauterine abnormalities. Thirty-eight patients who had a failed fresh ET cycle were also included in the FET group, as they met the study inclusion criteria and deemed not to introduce a significant autocorrelation bias. Only cycles where at least two day 5 blastocysts were available for fresh ET and where at least two day 5 blastocysts survived warming for FET were included in the analysis. The selected fresh ET and FET cycles were stratified and matched according to the blastocyst expansion grade (grade 2, 3, 4, or 5) of the two blastocysts transferred (i.e., 2:2 vs 2:2 or 3:3 vs 3:3, etc.), with inner cell mass grade of A or B and trophectoderm grade of A or B (i.e., AA, AB, BA, or BB). For example, the grade 2 cohort included the following blastocyst transfer combinations: 2AB/2AB, 2AA/2AB, 2AB/2BA, and 2BB/2BB.
Ovarian stimulation and embryo culture
Controlled ovarian stimulation (COS) was performed using a GnRH antagonist (0.25 mg, Cetrotide, Merck Serono, Turkey) co-treatment protocol with a combination of rFSH (Gonal-F, Merck Serono, Turkey) and hMG (Menopur, Ferring Pharmaceuticals, India). A transvaginal ultrasound-guided oocyte pickup (OPU) procedure was performed 36 h after ovulation induction with human chorionic gonadotropin (hCG; 250 μg/0,05 mL, Ovidrel, Merck, Serono, Turkey) or a combination of hCG and gonadotropin-releasing hormone agonist (GnRHa; 0.2 mg, Gonapeptyl®, Ferring Pharmaceuticals, India). In cycles of oocyte collection, embryo culture was performed using Sydney IVF (COOK Medical, USA) media. All inseminations were performed using ICSI [17]. Incubation conditions were set at 6 % CO2, 5 % O2, and 37.0 °C (K-Systems, Kivex Biotec ltd, Denmark), and embryos cultured in micro-droplets of media overlayed with light mineral oil. All embryos were cultured to at least the 5th day after OPU for transfer and/or cryopreservation.
Blastocysts were scored according to the three-part grading system proposed by Gardner and Schoolcraft [18, 19]: blastocyst expansion on a scale of 1 (early blastocyst) to 6 (hatched blastocyst), the inner cell mass (ICM) on a scale of A to C, according to the number and degree of compaction of the cells, and the trophectoderm (TE) on a scale of A to C, according to the number, size, shape, and contiguous arrangement of the trophectoderm cells. Blastocysts with grade C inner cell mass and trophectoderm scores were selected for fresh ET, but none were vitrified and therefore were not included in the analysis. Day 5 grade 1 blastocysts were not included in the analysis, as these were cultured to day 6 for transfer and or cryopreservation selection.
Vitrification and warming of blastocysts
Vitrification and warming of blastocysts was performed as described in the manufacturer’s methodology insert (Cryotop, Kitazato BioPharma Co. Ltd, Japan). The method utilizes high concentration cryoprotectants with ultra-rapid vitrification and warming rates. Equilibration, vitrification, thawing, diluent, and washing solutions required for the procedures were all provided in the commercially available Cryotop Safety Kits. Briefly, blastocysts were taken through an equilibration step and a vitrification step at room temperature before being placed on a Cryotop strip and plunged into liquid nitrogen. No more than two blastocysts were placed on a strip, with a minimal volume of medium. The Cryotop strip was placed in a cap under liquid nitrogen and stored in a cryo-tank. For warming, a capped Cryotop container was removed from the cryo-tank and the strip removed from the cap under liquid nitrogen. The strip was taken from the liquid nitrogen and plunged into warming solution. Recovered blastocysts were taken through a diluent and two wash steps all at 37 °C. Following the washing steps, the blastocysts were placed in culture droplets covered with light mineral oil and placed in an incubator for an equilibration period of at least 2 h. The warmed blastocysts were assessed for survival and had their morphologies re-scored after the equilibration period. These post-equilibration blastocyst scores were used in the matching. The blastocyst survival rate during the period of the study was 89.1 % (2096/2353). All blastocysts that survived warming and were assessed as viable, but not transferred, were re-vitrified. The blastocysts selected for transfer were prepared for FET after the 2-h equilibration period.
FET programming
All FET cycles were performed after endometrial preparation and synchronization using a scheduled supplementation of estrogen (Estrofem, Novo Nordisk, Turkey) and progesterone (Crinone, Merck Serono, Turkey). Endometrial preparation was performed using a step-up regime of estrogen (2 to 8 mg/day) supplementation. A transvaginal ultrasound scan (TVUS) was performed on day 14 to measure endometrial thickness, and blood was taken to check the progesterone concentration. If the endometrium was >7 mm and there was no evidence of progesterone rise (>2 ng/mL progesterone), estrogen supplementation was continued at 6 mg/day and progesterone (8 % twice a day) supplementation started the next day (day 15). The blastocyst warming and transfer was scheduled to be performed on the 6th day of progesterone supplementation.
Blastocyst transfer and luteal phase support
All blastocyst transfer procedures were performed using a Hamilton syringe (50 μL, Hamilton Company, USA) attached to an embryo replacement catheter (Wallace, Smiths Medical International, UK) and transabdominal ultrasound guidance. The same luteal phase support of estrogen and progesterone supplementation was followed for fresh ET and FET, with supplementation continuing for at least 9 weeks of gestation, if pregnant.
Outcomes and statistics
Pregnancy outcomes were defined as follows: a day 14 βhCG value of >30 IU/L was defined as a pregnancy, fetal heart with normal cardiac activity observed by ultrasound between the 6th and the 8th week of gestation was defined as a clinical pregnancy. The fetal heart implantation rate was determined from the ratio, total number of fetal hearts divided by the total number of blastocysts transferred. MedCalc version 13.0.6 was used for statistical analysis and to obtain the confidence intervals (95 % CI) and relative risk (RR). Descriptive statistics were presented as the mean and standard deviation for continuous data and as percentages for the categorical data. The independent samples t test was used to compare the means, and the chi-square or Fisher exact test was used to determine statistical significance between percentages. A p <0.05 was considered to be significant.
Results
Five hundred and ninety-eight fresh double blastocyst ET cycles and 545 double blastocyst FET cycles satisfied the inclusion criteria, were stratified according to their day 5 blastocyst expansion (grade 2 to 5), and matched between fresh ET and FET. The patient fertility characteristics of the cycles included in the fresh ET and FET groups are presented in Table 1. The mean patient age, infertility duration, BMI, and endometrial thickness outcomes were all non-significantly different between the two groups. The endometrial thickness measures which were not significantly different (9.58 vs 9.45 mm; p = NS) were done within 1 day of ovulation induction in fresh ET cycles and on the 14th day of estrogen supplementation in the FET cycles. The parity (0.20 vs 0.19; p = 0.03) and antral follicle count (AFC; 21.4 vs 31.0; p < 0.0001) were, however, significantly different. The higher AFC outcome from the FET cycles was not unexpected, as the majority (91 %) of the cryopreserved blastocysts used in the FET cycles was from fresh cycles with supernumerary blastocysts. The reduced parity observed in the FET group may suggest patients with previous failed fresh ET. The etiology classification proportions were also not significantly different between the two groups, with male infertility and unexplained infertility as the primary reasons (≈55 %) for treatment (Table 1). OHSS, a risk factor for reduced pregnancy outcomes in fresh ET, only occurred in eight (1.34 %) of the fresh ET cycles.
The oocyte number collected at the respective OPU and the pregnancy outcomes for the four blastocyst expansion grade fresh ET and FET cohorts are presented in Table 2. The oocyte number variable was included in Table 2 to represent the difference in AFC observed between the fresh ET and FET groups. In all four matched-cohort comparisons, the pregnancy, clinical pregnancy, and fetal heart implantation rates were lower for fresh ET. The RR for blastocyst implantation in fresh ET was lower in grade 2 (RR, 0.72; 95 % confidence interval (CI), 0.347–1.5032) and grade 3 (RR, 0.86; 95 % CI, 0.701–1.061) cohorts and significantly lower in grade 4 (RR, 0.65; 95 % CI, 0.563–0.759) and grade 5 (RR, 0.82; 95 % CI, 0.708–0.960) cohorts. The fetal heart implantation rate increased from 16.7 % for grade 2 to 47.3 % for grade 5 blastocysts in fresh ET cohorts, compared to 23.1 to 57.4 % in FET cohorts. The measured pregnancy outcomes observed in the different cohorts of both fresh ET and FET confirms the association between embryo quality and pregnancy outcome (i.e., increasing embryo quality results in increased pregnancy). The oocyte number was statistically lower in fresh ET compared to FET in each of the cohorts (Table 2). The data in Table 2 also indicates a possible association between oocyte number and blastocyst expansion.
The sub-group analysis presented in Table 3 was performed because of the statistical differences observed between the AFC and oocyte numbers obtained for fresh ET and FET. In this analysis, the cycles analyzed were restricted to those cycles with between 8 and 28 oocytes at OPU. Notwithstanding, the re-stratification of the cycles oocyte number still remained statistically lower in fresh ET (16.9 vs 17.8; p = 0.0298). The data was not further stratified according to blastocyst expansion, because 88.4 % of fresh ET and 82.5 % of FET were with blastocysts that had expansion grades >3. The pregnancy outcomes and the differences observed between fresh ET and FET resembled those obtained in the overall grade 4 cohort analysis. The pregnancy (RR, 0.82; 95 % CI, 0.7569–0.887), clinical pregnancy (RR, 0.78; 95 % CI, 0.704–0.869), and fetal heart implantation rates (RR, 0.79; 95 % CI, 0.708–0.882) were all significantly lower in fresh ET.
Discussion
More and more clinical studies are suggesting that COS may significantly and adversely affect implantation [6, 20]. In this comparatively large matched-cohort study, we examined pregnancy outcomes in good prognosis patients after the transfer of day 5 blastocysts of similar quality (grade ≥2) in fresh ET and FET. The patient and blastocyst selection criteria were deliberately chosen in an attempt to limit bias related to patient fertility and blastocyst developmental competence (i.e., reduced implantation of slow developing blastocyst because of endometrial asynchrony), therefore isolating the peri-implantation conditions of fresh ET and FET as the primary differential. The outcomes of the present study showed that artificial cycle FET resulted in higher pregnancy, clinical pregnancy, and fetal heart implantation rates, independent of the expansion grade of the blastocysts transferred. The fetal heart implantation rates of fresh ET ranged from 16.7 % in the grade 2 to 47.3 % in the grade 5 blastocyst cohort, compared to the 23.1 % in grade 2 to 57.4 % in grade 5 blastocyst cohort of FET. The trend of increasing pregnancy with increasing blastocyst expansion was similar in fresh ET and FET with a similar difference in pregnancy at each blastocyst expansion grade between fresh ET and FET. The reduced pregnancy outcomes in fresh ET observed in the present study confirms the outcomes of recent publications demonstrating the possible negative impact of hormone therapies, such as COS on reproductive outcomes [6, 13, 15, 16, 21]. The results from their study prompted Zhu et al. [21] to ask the question, “is it time for a new embryo transfer strategy?” The present study echoes this sentiment and suggests that a freeze-all strategy may certainly benefit reproductive outcomes in selected patient groups.
The biases related to embryo quality that have been cited in fresh vs frozen comparative studies are based on suppositions, such as mainly secondary embryos are cryopreserved and only the best embryos survive cryopreservation. In this study, the post-equilibration morphological scores of the vitrified-warmed blastocysts were matched with blastocyst scores at the time of fresh ET. While there was no a priori evidence to suggest that this would ensure developmental competency equivalence, the very similar trends in pregnancy outcomes (i.e., increasing pregnancy with increasing blastocyst expansion) observed for fresh ET and FET in this study certainly suggests that the cryopreservation methodology used delivered blastocysts with very similar competency. Moreover, the survival rates of 89 % obtained in this study and the 96 % [12] and 94 % [16] obtained in two other studies using Cryotop technology indicate that the presumption that only the best embryos survive may no longer be a plausible argument. The significant advances in cryopreservation may therefore have significantly reduced bias in terms of embryo competency in frozen-thaw cycles. Other biases in the present study were related more to patient fertility characteristics (i.e., AFC and parity). While the potential for bias from the parity difference was questionable, the AFC difference (21.4 vs 31.0) was of greater significance and was therefore investigated for any attributed bias. The decision to perform a sub-analysis was based on the results of the present study and that of Stone et al. [22] which showed that as oocyte yields rise, the average grades and the implantation potential of selected blastocysts increase, even though a previous large meta-analysis found AFC only to be predictive of ovarian response [23]. In the sub-analysis, the pregnancy, clinical pregnancy, and fetal heart implantation rates of fresh ET and FET mirrored those obtained in the initial cohort analyses; therefore, the AFC difference may unlikely have attributed any measurable bias to FET outcomes. We therefore believe that the outcomes of the present study mainly reflect differences in endometrial competence between fresh ET and FET.
Taking advantage of the improvements in cryopreservation survival outcomes, a number of studies have tested the hypothesis that higher implantation rates could be obtained by deferring fresh transfer and rather transferring embryos in natural or artificial FET cycles [13, 15, 16]. The pivotal challenge in these investigations has been the ability to compare like with like by suitably matching patient and cycle covariates, and especially the embryo quality variable. Shapiro et al. [15, 24, 25] used three different fresh vs frozen study designs to compare endometrial receptivity between fresh ET and FET. In all three studies, the implantation and pregnancy outcomes were found to be reduced in fresh cycles, as compared to FET cycles. In three recent SET studies, the fresh ET and FET cohorts were matched as follows: Shapiro et al. [15] matched embryo quality according to blastocyst diameter, inner cell mass size, and trophectoderm cell count; Feng et al. [13] compared the transfer of blastocysts graded ≥3BB; and Roy et al. [16] matched blastocysts graded as grades I and II, according to their morphology and developmental stage. In the study by Shapiro et al. [15], the ongoing pregnancy rate was found to be non-significantly higher in the FET cohort for day 5 blastocysts (61 vs 57 %). In the study by Feng et al. [13], a non-significantly lower implantation rate (47 vs 52 %) was obtained in the FET cohort, and in the study by Roy et al. [16], non-significantly different live birth rates were obtained between the grade 1 cohorts (53 vs 55 %) and between the grade II cohorts (35 vs 30 %).
Similar trends in pregnancy, clinical pregnancy, and implantation rates were observed within the fresh ET and the FET cohort groups of the present study, with regard to blastocyst expansion grades (grades 2 to 5). Similarly, the study by Ahlstrom et al. [26] found blastocyst expansion to be a significant predictor of live birth. The outcomes observed in the present study indicate that pregnancy outcomes were mostly dependent on blastocyst expansion grade and endometrial receptivity. While blastocysts with an expansion grade >3 had the highest probability of pregnancy (≈86 %), transferring these blastocysts in fresh ET rather than FET would mean a reduction of ≈10 % in pregnancy. In the past, the best embryos have always been preferentially transferred in fresh ET, because of the increased risk for embryo competence loss through cryopreservation [27]. The results of this study and other studies using vitrification technology demonstrate that a greater use of elective FET may not be out of order, based on current vitrification-warming survival and developmental competence rates [12, 13, 16, 21].
A limitation of the present study is its retrospective design; it therefore suffers from the usual biases inherent to retrospective studies. In addition, the broad cycle selection criteria resulted in the inclusion of cycles in the FET group that were different to those in the fresh ET group in terms of ovarian response and probably blastocyst utilization. However, we still believe the outcomes presented in our study to be of clinical value. The main reasons being the number of cycles included, the manner in which the cycles were matched (i.e., day 5 blastocysts only and the morphological score of two blastocysts), the use of vitrification for blastocyst cryopreservation, and the results showing that there was no bias forthcoming from the AFC differences observed. The use of vitrification not only ensured a high survival rate but also ensured a high blastocyst developmental competence retention rate. In conclusion, this large and selectively matched study demonstrates that blastocyst FET results in higher pregnancy, implantation, and clinical pregnancy rates as compared to fresh blastocyst ET in good prognosis patients. Whether FET will replace fresh ET for the reasons of better peri-implantation outcomes [20] in all patients will require further studies that will include patients with poor fertility prognosis and slow developing blastocysts.
References
Bourgain C, Devroey P. The endometrium in stimulated cycles for IVF. Hum Reprod Update. 2003;9:515–22.
Oehninger S. Revealing the enigmas of implantation: what is the true impact of ovarian hyperstimulation? Fertil Steril. 2008;89:27–30.
Bosch E, Labarta E, Crespo J, Simόn C, Remohi J, Jenkins J, et al. Circulating progesterone levels and ongoing pregnancy rates in controlled ovarian stimulation cycles for in vitro fertilization—analysis of over 4000 cycles. Hum Reprod. 2010;25:2092–100.
Humaidan P, Papanikolaou EG, Kyrou D, Alsbjerg B, Polyzos NP, Devroey P, et al. The luteal phase after GnRH-agonist triggering of ovulation: present and future perspectives. Reprod BioMed Online. 2012;24:134–41.
Xu B, Li Z, Zhang H, Jin L, Li Y, Ai J, et al. Serum progesterone level effects on the outcome of in vitro fertilization in patients with different ovarian response: an analysis of more than 10,000 cycles. Fertil Steril. 2012;97:1321–7.
Evans J, Hannan NJ, Edgell TA, Vollenhoven BJ, Lutjen PJ, Osianlis T, et al. Fresh versus frozen embryo transfer: backing clinical decisions with scientific and clinical evidence. Hum Reprod Update. 2014;20:808–21.
Papanikolaou EG, Bourgain C, Kolibianakis E, Tournaye H, Devroey P. Steroid receptor expression in late follicular phase endometrium in GnRH antagonist IVF cycles is already altered, indicating initiation of early luteal phase transformation in the absence of secretory changes. Hum Reprod. 2005;20:1541–7.
Van Vaerenbergh I, Van Lommel L, Ghislain V, In’t Veld P, Schuit F, Fatemi HM, et al. In GnRH antagonist/rec-FSH stimulated cycles, advanced endometrial maturation on the day of oocyte retrieval correlates with altered gene expression. Hum Reprod. 2009;24:1085–91.
Labarta E, Martınez-Conejero JA, Alama P, Horcajadas JA, Pellicer A, Simon C, et al. Endometrial receptivity is affected in women with high circulating progesterone levels at the end of the follicular phase: a functional genomics analysis. Hum Reprod. 2011;26:1813–25.
Humaidan P, Van Vaerenbergh I, Bourgain C, Alsbjerg B, Blockeel C, Schuit F, et al. Endometrial gene expression in the early luteal phase is impacted by mode of triggering final oocyte maturation in recFSH stimulated and GnRH antagonist co-treated IVF cycles. Hum Reprod. 2012;27:3259–72.
Edgar DH, Gook DA. A critical appraisal of cryopreservation (slow cooling versus vitrification) of human oocytes and embryos. Hum Reprod Update. 2012;18:536–54.
Cobo A, de los Santos MJ, Castello D, Gamiz P, Campos P, Remohí J. Outcomes of vitrified early cleavage-stage and blastocyst-stage embryos in a cryopreservation program: evaluation of 3,150 warming cycles. Fertil Steril. 2012;98:1138–46.
Feng G, Zhang B, Zhou H, Shu J, Gan X, Wu F, et al. Comparable clinical outcomes and live births after single vitrified-warmed and fresh blastocyst transfer. Reprod BioMed Online. 2012;25:466–73.
Roque M, Lattes K, Serra S, vSola I, Psych B, Geber S, et al. Fresh embryo transfer versus frozen embryo transfer in in vitro fertilization cycles: a systematic review and meta-analysis. Fertil Steril. 2013;99:156–62.
Shapiro BS, Daneshmand ST, Restrepo H, Garner FC, Aguirre M, Hudson C. Matched-cohort comparison of single-embryo transfers in fresh and frozen-thawed embryo transfer cycles. Fertil Steril. 2013;99:389–92.
Roy TK, Bradley CK, Bowman MC, McArthur SJ. Single-embryo transfer of vitrified-warmed blastocysts yields equivalent live-birth rates and improved neonatal outcomes compared with fresh transfers. Fertil Steril. 2014;101:1294–301.
Ferraretti AP, Goossens V, Mouzon J, Bhattacharya S, Castilla JA, Korsak V, et al. The European IVF-monitoring (EIM), and Consortium, for the European Society of Human Reproduction and Embryology (ESHRE) assisted reproductive technology in Europe, 2008: results generated from European registers by ESHRE. Hum Reprod. 2012;27:2571–84.
Gardner DK, Schoolcraft WB. In vitro culture of human blastocysts. In: Jansen R, Mortimer D, editors. Toward reproductive certainty: fertility and genetics beyond 1999. London: Parthenon Publishing; 1999. p. 378–88.
Gardner DK, Schoolcraft WB. Culture and transfer of human blastocysts. Curr Opin Obstet Gynecol. 1999;11:307–11.
Weinerman R, Mainigi M. Why we should transfer frozen instead of fresh embryos: the translational rationale. Fertil Steril. 2014;102:10–8.
Zhu D, Zhang J, Cao S, Zhang J, Heng BC, Huang M, et al. Vitrified-warmed blastocyst transfer cycles yield higher pregnancy and implantation rates compared with fresh blastocyst transfer cycles—time for a new embryo transfer strategy. Fertil Steril. 2011;95:1691–5.
Stone BA, March CM, Ringler GE, Baek KJ, Richard P, Marrs RP. Casting for determinants of blastocyst yield and of rates of implantation and of pregnancy after blastocyst transfers. Fertil Steril. 2014;102:1055–64.
Broer SL, van Disseldorp J, Broeze KA, Dolleman M, Opmeer BC, Bossuyt P, et al. Added value of ovarian reserve testing on patient characteristics in the prediction of ovarian response and ongoing pregnancy: an individual patient data approach. Hum Reprod Update. 2013;19:26–36.
Shapiro BS, Daneshmand ST, Garner FC, Aguirre M, Hudson C, Thomas S. Evidence of impaired endometrial receptivity after ovarian stimulation for in vitro fertilization: a prospective randomized trial comparing fresh and frozen–thawed embryo transfer in normal responders. Fertil Steril. 2011;96:344–8.
Shapiro BS, Daneshmand ST, Forest C, Garner FC, Aguirre M, Hudson C, et al. Evidence of impaired endometrial receptivity after ovarian stimulation for in vitro fertilization: a prospective randomized trial comparing fresh and frozen-thawed embryo transfers in high responders. Fertil Steril. 2011;96:516–8.
Ahlstrom A, Westin C, Reismer E, Wikland M, Hardarson T. Trophectoderm morphology: an important parameter for predicting live birth after single blastocyst transfer. Hum Reprod. 2011;26:3289–96.
Imbar T, Kol S, Francine Lossos F, Bdolah Y, Hurwitz A, Haimov-Kochman R. Reproductive outcome of fresh or frozen–thawed embryo transfer is similar in high-risk patients for ovarian hyperstimulation syndrome using GnRH agonist for final oocyte maturation and intensive luteal support. Hum Reprod. 2012;27:753–9.
Study funding/competing interest(s)
The study was performed and manuscript prepared with no known conflicts of interest and with no financial support.
Trial registration number
N/A
Author information
Authors and Affiliations
Corresponding author
Additional information
Capsule Reproductive outcomes of fresh ET were reduced in comparison to outcomes of artificial FET.
Rights and permissions
About this article
Cite this article
Özgür, K., Berkkanoğlu, M., Bulut, H. et al. Higher clinical pregnancy rates from frozen-thawed blastocyst transfers compared to fresh blastocyst transfers: a retrospective matched-cohort study. J Assist Reprod Genet 32, 1483–1490 (2015). https://doi.org/10.1007/s10815-015-0576-1
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s10815-015-0576-1