Abstract
Purpose
To estimate the prevalence of chromosomally abnormal related miscarriages in an infertile population.
Methods
Retrospective analysis of cytogenetics obtained by chorionic villi harvesting of the first miscarriage cycle of infertile patients at our center from 2001–2010 were reviewed. Abnormal results were characterized as trisomy, monosomy X, structural, or other. Age, # of eggs, #2PN, # embryos transferred, day of transfer, and performance of intracytoplasmic sperm injection (ICSI) were recorded.
Results
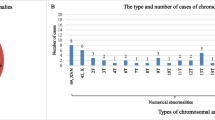
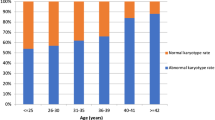
In a study population of 299 patients with a mean age of 38.0 ± 4.5 y, 276(92 %) patients had some form of assisted reproductive technologies (ART), and 244(82 %) had IVF. Of all results, 71.6 % had an abnormal karyotype. Patients with abnormal cytogenetics were older (38.6 ± 4.1 vs. 36.3 ± 4.9, p < 0.001), and more likely to have a day 3 transfer (age < 38 ( 20.7 %) vs. age 38 (46.3 %), p = <0.001) with more embryos transferred (3.0 ± 1.2, vs. 2.3 ± 0.9, p < 0.001). The performance of ICSI did not affect the rate of cytogenetically abnormal products of conception (ICSI 68.3 % vs. no ICSI 70.7 %). In comparing patients, monosomy X was more common in <38 y. Rates of trisomy, although not statistically significant, were higher in older patients.
Conclusions
The classic associations between advancing age and chromosomal abnormalities, and younger age and monosomy X, are affirmed in our infertile population. There was no increase in chromosomal abnormalities in cycles where ICSI was performed. Older patients are more likely to have day 3 transfers and more embryos transferred. Our chromosomal abnormality rates are higher than classic estimates but comparable to recent studies. The limitation of this study was a lack in uniformity among practitioners in recommending all patients have a Dilation and Curettage (D&C) at time of diagnosis. Such information may serve to improve the counseling of patients after miscarriage.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
In the general population, spontaneous abortion accounts for approximately 15 % of first trimester pregnancy losses. The risk of chromosomal abnormalities in spontaneous pregnancy loss is approximately 50 % in the general population based upon original work in 1980 [6]. In couples undergoing assisted reproductive technologies (ART) the risk of spontaneous abortion and karyotypic abnormalities are less clearly identified. This selected patient group is often counseled based on well established risks calculated for the general, otherwise fertile, population. However, studies have concluded that patients seeking infertility treatment have higher rates of chromosomally abnormal products of conceptions compared to age matched controls [3]. Furthermore, it has been speculated that the risk of cytogenetically abnormal products of conception may depend on the type of assisted reproductive technologies utilized [1, 4, 7].
The techniques employed for analysis of products of conception are important when reporting chromosomal abnormalities. Specifically, if care is not taken to avoid maternal cell contamination this could result in an inflated number of normal female karyotypes. This would lead to false reassurance of couples seeking explanation for first trimester miscarriages.
In this study we sought to estimate the prevalence of chromosomally abnormal miscarriages in an infertile population after assisted reproductive technologies. Our secondary objective was to minimize maternal cell contamination with a laboratory protocol for short term culture of dissected chorionic villus. With this information we hope to more effectively counsel patients and potentially devise better treatment plans.
Materials & methods
This was a retrospective cohort study. All infertile patients age 22–51 undergoing dilation and curettage at our center for first trimester singleton spontaneous abortions after ovulation induction, in vitro fertilization, spontaneous pregnancy, natural cycles, frozen embryo transfer, donor egg recipient, pre-implantation genetic diagnosis, and frozen donor egg recipients were identified from billing records between 2001 to 2010. First trimester losses were defined by the absence of fetal cardiac activity prior to 12 weeks of gestation. These records were then cross matched with the Society for Assisted Reproductive Technologies (SART) databases. Patients that elected for cytogenetic analysis of products of conception were included in this study. Only the first miscarriage at our center for each patient was included, and all multiple gestations and repeat cycles were excluded from this study. Only patients who underwent dilation and curettage with chromosomal analysis were included in this study. The age of the donor was included for donor egg recipient cycles. A pregnancy test and ultrasound were performed and patients were offered dilation and curettage depending upon the recommendation of their primary physician.
Cytogenetic studies were obtained with a laboratory protocol for short-term culture of dissected chorionic villi (CV) from products of conception received in their entirety following D&C [10]. Briefly, CV and gestational sac are separated from placental tissues, washed in sterile saline, and meticulously cleaned in Dulbecco’s Modified Eagle Medium (Life Technologies) under a dissecting microscope with sterile surgical blades and needles to remove maternal decidua, blood clots and other non-villous material. Approximately 30 mg of the cleaned CV are dissociated with trypsin for 1 h and then collagenase for 1–2 h. The digested cells are centrifuged and split into three flasks for culture in Chang Medium D (Irvine Scientific). Cleaned sac (~20 mg) is minced finely crosswise with scalpel blades and set up in one flask for culture in Delbecco’s MEM supplemented with 20 % fetal bovine serum (Life Technologies). Following short-term culture, typically 5–6 days, cells were harvested for routine G-band chromosome analysis. To further reduce reporting of normal female cells due to maternal cell contamination, in cases with a normal female karyotype, optimally 10 cells were analyzed from two independent CV and one sac culture (if sac failed to grow, three CV cultures were examined). Specimens were considered indeterminate and likely of non-fetal origin that did not meet the above criteria; included are those with inadequate material noted at specimen receipt or with very slow culture growth.
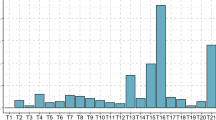
Abnormal results were characterized as trisomy, monosomy X, structural, or other. Trisomy was defined as a single chromosome in three copies. Monosomy X was defined as a single X chromosome in a single copy with no second sex chromosome. Structural abnormalities included all balanced or unbalanced chromosomal rearrangements. All additional chromosomal abnormalities not included in the aforementioned categories were categorized as other (i.e. triploidy).
Patient information from SART databases was recorded. Demographic information included patient age, and diagnosis of infertility. Cycle information collected included type of assisted reproductive technology, number of eggs retrieved, number of fertilized oocytes (2PN), number of embryos transferred, day of transfer, and performance of ICSI. All results were analyzed using chi squared tests and statistical analysis was performed using the SPSS statistical program. For all test thresholds a value of p < 0.05 was used for significance.
Results
A total of 299 patients with a mean age of 38 ± 4 (range 22–51) underwent dilation and curettage for spontaneous abortion at our center from 2001–2010. Two hundred seventy-six (92 %) patients had some form of assisted reproductive techniques and 244 (82 %) had in vitro fertilization (Table 1). Of all results, 73 % had an abnormal karyotype. Patients with abnormal cytogenetics were older (38.6 ± 4.1 vs. 36.3 ± 4.9, p < 0.001), and more likely to have a day 3 transfer (age <38 20.7 % vs. age ≥38 46.3 %, p = <0.001) with more embryos transferred (3.0 ± 1.2, vs. 2.3 ± 0.9, p < 0.001). Monosomy X was only seen in patients younger than 38 years old. Rates of trisomy, although not statistically significant were higher in older patients (Table 2).
Thirty-four cases were initially diagnosed as normal females by our cytogenetics laboratory. Further analysis revealed that 22 of these cases were likely of fetal origin and 12 likely maternally derived based on our established protocol to minimize maternal cell contamination. When eliminating the 12 patients (categorized as likely maternal) from our overall database, the number of patients with cytogenetically abnormal products of conception was 76 % (217/287.) In cycles where ICSI (87) was performed there was no statistical difference in percentage of chromosomally abnormal products of conception, 69 % vs. 72 %.
Six patients of average age 36.5 (32–42) underwent pre-implantation genetic diagnosis (PGD) prior to in-vitro fertilization. The specific chromosomes tested for were identified by fluorescence in situ hybridization (FISH) as shown in Table 3. Four out of six had karyotypically normal products of conception. One of these patients had a 46,XX karyotype that could not be ruled out due to maternal cell contamination, and two patients had abnormal chromosomes that were not specifically tested for during pre-implantation genetic diagnosis. (Table 3).
Two hundred eighteen cases of IVF were examined based on day of embryo transfer, for this analysis cases that involved PGD or frozen cycles were excluded. These cycles were grouped according to day of transfer with 82 cleavage stage and 136 blastocyst embryo transfers. Chi squared analysis was then performed to determine if there was any statistical difference in rates of chromosome abnormalities between these groups. As shown in Table 4 there was a higher percentage of chromosomally normal products of conception in the blastocyst transfer group (30.9 % compared to 20.7 %) although this did not achieve statistical significance (p = 0.12).
Discussion
Infertile patients had a 76 % rate of chromosomal abnormalities in our study population. This is higher than classical estimates of 50 %, but affirms recently published data in infertility cohorts that report a higher rate of chromosomal abnormalities [1]. Classic associations between advancing age and chromosomally abnormal products of conception are demonstrated in this group. The link between younger age and monosomy X is reaffirmed in our study population [5]. Assisted reproduction technologies, such as ICSI, have been suggested to lead to higher rates of chromosomal abnormalities, however in this study ICSI (69 % vs. 72 % p = 0.76) did not affect the rate of genetically abnormal products of conception [2, 7]. In our study it is possible that no difference in miscarriage risk was detected in the ICSI group secondary to comprehensive preconceptual screening at initial visit or biases in criteria to perform ICSI. Patients who are referred to our center often request ICSI as part of their IVF protocol when they do not fit stringent criteria to warrant use of this technique. Additionally, it has been proposed that day of embryo transfer may affect the results of pregnancy outcome, and in our study we found a higher percentage of chromosomally normal products of conception in blastocyst transfers but no statistical difference from cleavage stage transfers. This may be secondary to a small sample size.
Chorionic villi harvesting (CVH) in conjunction with a protocol to reduce maternal contamination of specimens is an important adjunct to cytogenetic analysis [8, 10]. While newer techniques such as microarrays are useful in detecting subtle unbalanced chromosomal abnormalities, they have limitations in comparison to CVH. In particular, standard clinical microarrays are unable to detect triploidy and polyploidy.
In cycles where PGD was performed FISH was used to detect chromosomally normal embryos prior to transfer. In recent years, the validity of FISH to detect chromosomal abnormalities has been questioned secondary to the poor predictive value associated with this test. Specifically, FISH is unable to detect embryo mosaicism, and is an invasive method that can negatively impact the embryo. In response to these limitations, our center now uses comparative genomic hybridization microarray technology and has had no subsequent aneuploidy related miscarriages (Grifo, unpublished data).
In future studies it would be useful to offer all patients with infertility and first trimester losses a D&C for cytogenetic analysis. This would allow for a larger cohort to define the incidence of cytogenetic abnormalities in first trimester losses, which could lead to research analyzing chromosomal reasons for unexplained infertility. In addition, it would be constructive to identify a current control population for comparison, rather than using a historical control population.
Our study results indicate that patients seeking fertility treatment have a higher risk of karyotypic abnormalities than classic estimates (63.7 %–78.9 % vs. 30–40 %) and counseling should reflect this information. As the risk of chromosomal abnormalities is high, cytogenetic analysis of products of conception can be a useful component of the fertility work-up. The results from karyotypic analysis of first trimester losses can enhance diagnostic evaluation, and this information may help in counseling infertile couples for future cycles [9].
References
Bettio D, Venci A, Levi Setti PE. Chromosomal abnormalities in miscarriages after different assisted reproduction procedures. Placenta. 2008;29(Suppl B):126–8.
Brandes M, Verzijden JC, Hamilton CJ, et al. Is the fertility treatment itself a risk factor for early pregnancy loss? Reprod Biomed Online. 2011;22:192–9.
Campana M, Serra A, Neri G. Role of chromosome aberrations in recurrent abortion: a study of 269 balanced translocations. Am J Med Genet. 1986;24:341–56.
Causio F, Fischetto R, Sarcina E, Geusa S, Tartagni M. Chromosome analysis of spontaneous abortions after in vitro fertilization (IVF) and intracytoplasmic sperm injection (ICSI). Eur J Obstet Gynecol Reprod Biol. 2002;105:44–8.
Hagman A, Wennerholm UB, Kallen K, et al. Women who gave birth to girls with Turner syndrome: maternal and neonatal characteristics. Hum Reprod. 2010;25:1553–60.
Hassold T, Chen N, Funkhouser J, et al. A cytogenetic study of 1000 spontaneous abortions. Ann Hum Genet. 1980;44:151–78.
Kim JW, Lee WS, Yoon TK, et al. Chromosomal abnormalities in spontaneous abortion after assisted reproductive treatment. BMC Med Genet. 2010;11:153.
Morales C, Sanchez A, Bruguera J, et al. Cytogenetic study of spontaneous abortions using semi-direct analysis of chorionic villi samples detects the broadest spectrum of chromosome abnormalities. Am J Med Genet A. 2008;146A:66–70.
Northrop LE, Treff NR, Levy B, Scott Jr RT. SNP microarray-based 24 chromosome aneuploidy screening demonstrates that cleavage-stage FISH poorly predicts aneuploidy in embryos that develop to morphologically normal blastocysts. Mol Hum Reprod. 2010;16:590–600.
Schmidt-Sarosi C, Schwartz LB, Lublin J, Kaplan-Grazi D, Sarosi P, Perle MA. Chromosomal analysis of early fetal losses in relation to transvaginal ultrasonographic detection of fetal heart motion after infertility. Fertil Steril. 1998;69:274–7.
Acknowledgements
Alan Berkeley, MD
Nicole Noyes, MD
Frederick Licciardi, MD
David L. Keefe, MD
M. Elizabeth Fino, MD
Lisa M. Kump-Checchio, MD
The NYU School of Medicine and Departments of Fertility, Pathology, and Obstetrics and Gynecology
Funding
None.
Author information
Authors and Affiliations
Corresponding author
Additional information
Capsule
The incidence of fetal chromosal abnormalities in an infertile population are higher than for the general population, as evidenced by analysis of products of conception.
Rights and permissions
About this article
Cite this article
Werner, M., Reh, A., Grifo, J. et al. Characteristics of chromosomal abnormalities diagnosed after spontaneous abortions in an infertile population. J Assist Reprod Genet 29, 817–820 (2012). https://doi.org/10.1007/s10815-012-9781-3
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s10815-012-9781-3