Abstract
Objective
To determine the effect of luteinized unruptured follicle (LUF) cycles on frozen thawed embryo transfer (FET).
Design
A retrospective analysis comparing the clinical outcomes after FET among 144 cases of luteinized unruptured follicle (LUF) cycles and 866 cases of ovulation cycles.
Setting
Reproductive medical center, Beijing China.
Patient(s)
Chinese infertile women who underwent FET.
Intervention(s)
None.
Main outcome measure(s)
Clinical pregnancy rate (PR), implantation rate.
Result(s)
The implantation rate, clinical pregnancy rate, on-going pregnancy rate and live birth rate in LUF group were 12.76% (49/384), 27.78% (40/144), 24.31% (35/144) and 19.44% (28/144), respectively, and in ovulation group, 14.74% (332/2251), 31.29% (271/866), 28.29% (245/866) and 22.23% (193/866), respectively (p > 0.05).
Conclusion(s)
LUF does not affect the clinical outcomes of FET. Patients of LUF should be included in FET treatment.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Luteinized unruptured follicle (LUF), a failure of ovulation due to luteinization of follicle under the action of luteinizing hormone (LH), is one of the major causes of infertility for women [1]. Like the women with ovulation cycles, women with LUF have normal menstrual period and biphase of basal body temperature (BBT): they exhibit similar cervical mucus and secretory changes to endometrium, and have almost the same ultrasonographic findings on endometrium as well as. Hence monitoring of follicle development and assessment of blood hormone were rarely conducted in clinical settings except for women with specific clinical indications. However, with the development of new diagnostic tools such as B type ultrasound, the diagnostic rate of LUF has been on the rise. In addition, recent data have shown that the endometrium proliferates more slowly in LUF cycles than in ovulation cycles, and women with LUF cycles have a shortened luteal phase, reduced P level and inadequate luteal function [2]. In spite of these new developments, to our knowledge, to date, there have been no reports in the world about the feasibility of FET in women having LUF cycle and many reproductive medical centers do not perform FET for women in LUF cycles.
It has been reported that the incidence of LUF is 11.2% in women with regular menstrual cycle [3], and 25% to 43% in women of infertility. The recurrent rate of LUF is much higher, ranges from 78.6% to 90% [4]: patients with recurrent LUF have to undergo repeated cancellation of FET leading to increased anxieties. It is therefore important to evaluate the effect of LUF cycles on FET. This study compares the clinical outcomes after FET between Chinese women in LUF cycles and women in ovulation cycles.
Materials and methods
Selection criteria
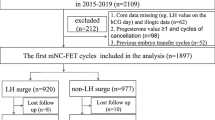
Included in the study were 1,016 infertile women with natural cycle (none of them was from induction of ovulation cycles) who had undergone FET treatment between January 2004 and December 2004 at Reproductive Medicine Center, Peking University Third Hospital. The subjects were categorized into either LUF group or ovulation group (144 and 866 cases, respectively) based on the criteria described below. On the day of FET and day 3 after FET, serum E2 and P level were measured and compared for patients performed FET between November 2004 and December 2004.
Diagnostic standards of ovulation
B type ultrasonography was used to monitor the process of ovulation starting at the time of the enlargement of follicles. If the midluteal P level was greater than 10 ng/ml (31.8 nmol/l) and a sudden disappearance of the preovulatory follicle or the follicle shrinking by 5 mm in diameter was observed, and/or the corpus luteum with or without the presence of fluid in the pelvic cavity was seen on ultrasound follow-up, the cycle was considered to be ovulatory.
Diagnostic standards of LUF
The following findings were diagnostic criteria of LUF [5, 6]: On ultrasonographic screening which a normal follicular development and a observation of a preovulatory follicle failed to rupture, instead: (1) continued to grow in size with an thickened follicular wall and increased internal resonance; meanwhile, extensive intrafollicular bright spots would be detected after 2 to 4 days; (2) rapidly enlargement to the size of 30 to 35 mm in diameter with strong internal resonance, persistent till the next cycle or even longer intrafollicular echoes might be (1) low, medium or high; (2) echoless; (3) diffuse and linear; (4) reticular or band-like. The presence of lowered cervical score, biphase of BBT, elevated serum LH, E2 and P level at the time together with the above findings established the diagnosis of LUF. The serum P level were >3 ng/ml (9.5 nmol/l) in LUF cycles [7].
Monitoring of ovulation
In the current study the patients were asked to monitor their follicles and sometimes cervical mucous score and serum E2 and P assessment to determine the day of ovulation and LUF. The size of follicles was assessed with transvaginal ultrasonography using 5.0 MHz section type testing probe. From the day 8 or day 10 of menstrual cycle, the size of follicles was measured continuously. Ovulation and LUF were established by ultrasonographic findings, the cervical mucous score and serum LH, E2, P level on the day of ovulation.
Luteal support
All the patients received the same luteal support by progesterone since the day of embryos transfer in which progesterone 20 mg were given daily from the day of ET.
FET therapy and evaluation of thawed embryos
Using slow freezing and rapid thawing protocol [8], all the frozen thawed embryos underwent 3 days culture in vitro. Embryos were assessed for quality from the following aspects [9]: morphology of cells, the number of cell and cellular debris. The embryos in G1 and G2 grade with no less than six blastomeres are defined as good quality embryos. Cumulative embryo score (CES) score was done in all patients according to embryonic morphology [10].
FET outcomes
The outcomes of FET were divided into two statuses: no pregnancy and clinical pregnancy. No pregnancy mean women whose blood HCG level was less than 35 IU/l. Clinical pregnancy mean women who had positive blood HCG, visible gestation cyst on ultrasound 30 days after FET or visible abortus. Clinical pregnancy was redefined into ongoing pregnancy (pregnancies continued over 20 gestation weeks) and embryonic diapause (women with empty gestational cysts by ultrasound on more than two consecutive observation, or presence of gestational sac without primary fetal heartbeat).
Statistical analysis
Statistical analysis was performed by using SPSS software, version 10.0 (SPSS, Inc., Chicago, IL, USA). χ 2 tests or Fisher exact tests were used for qualitative variables and nonparametric analysis of variance was used for the quantitative variables. The probability value used to identify significance was given a test of p < 0.05.
Results
Parameters of LUF and ovulation cycles
There were no significant differences between LUF and ovulation group in basic characteristics including age, course of infertility, infertility types, frozen time of embryos, the number of embryos transferred, the number of embryonic cells, mean number of cleavage cells, the number of top quality embryos between LUF and ovulation group (Table 1).
Relationship between outcomes of FET and pregnancy in LUF cycle
Out of the 1,016 Chinese infertile women included in the study 1,010 were followed up during their FET protocol, including 144 LUF patients and 866 ovulation patients (99.40% of the enrolled patients were followed up). A total of 2,635 embryos were transferred (384 in LUF group, and 2,251 in ovulation group), of which 369 (14.00%) embryos were implanted. As a result, 311 (30.79%) patients had clinical pregnancy. The pregnancy rate was 27.78% in LUF group (40/144 cases) and 31.29% in ovulation group (271/866 cases) and the implantation rate was 12.76% (49/384 cases) and 14.74% (332/2,251 cases) in LUF and ovulation group, respectively. Neither difference between the two groups was significant (for clinical pregnancy rate, p = 0.436; implantation rate, p = 0.346). There were no significant differences in ongoing pregnancy rate, term birth rate or premature delivery rate and late abortion rate between LUF and ovulation group. Also shown in Table 2 there was no significant difference in live birth rate from ongoing pregnancy between the two groups (19.44% vs. 22.23%, 28/144 cases vs. 193/866 cases, p = 0.514) noted in Table 2.
Endometrial ultrasonographic findings and serum hormone levels in LUF cycle
The ultrasonographic examination showed that there was no significant difference in the thickness of the endometrium between LUF group and ovulation group (1.01 ± 0.14 vs. 1.02 ± 0.14 cm, p = 0.534); There was no significant difference in the distribution of A type endometrial lining in LUF and ovulation group (46 vs. 625, 31.94% vs. 72.17%) but there were significantly more cases with B endometrial lining in LUF group than in ovulation group (98 vs. 241, 68.06% vs. 27.83%, p = 0.000).
The serum E2 and P level were measured for LUF patients undergoing FET between November 2004 and December 2004 on the day of FET and day 3 after FET, and the findings were compared with those in ovulation cycles. The comparison showed no significant differences in E2, P level and P/E2 ratio on the day of FET and day 3 after FET between LUF and ovulation group (Table 3).
Discussion
In 1975 Jewelwicz [11] first reported that well developed follicles could persisted unruptured and have the typically luteinization as observed in normal menstrual cycle. Marik and Hulka [12] demonstrated by laparoscope that in some individuals there failed to show cleavage for ovulation on the surface of the ovaries in the early luteal phase, indicating the process of luteinization didn’t necessarily result from ovulation. The mechanism of LUF was attributed to endocrinal and mechanical causes. The former referred to internal environmental factors leading to ovulation disorders, such as elevated level of cyclic adenosine monophosphate due to insufficient secretion of LH, reduced secretion of P, lowered activity of profibrinolysin activators, decreased fibrinolysis and autolysis of the wall of the ovaries leading to disorders in the maturation of follicles, cleavage and discharge oocytes [13]. LUF cycles might also result from such defects as collagens and vascularized graft, which usually lead to lowered P level [14, 15]. The later condition was also known as “false LUF”. It was usually caused by adhesion, thickening of pelvic soft tissues resulting from infarction of fallopian tube, endometriosis, pelvic surgeries or inflammation [16]. Other implicated causes of LUF included the use of certain non-steroid anti-inflammatory drugs, such as mezolin, meloxicam etc [17, 18]. The endocrinal mechanism of LUF has been gradually elucidated after numerous studies of the relationship between LUF and infertility. Westfahl [19] observed the absence of P surge and shortened P duration in animal experiments in LUF cycles, the level of androstenedione and testosterone rose and backed to basal level 48 h after HCG administration. A study on ovarian blood flow by ultrasonography, it demonstrated that intraovarian resistance indexes (RI) of LUF cycles was similar to those of anovulatory cycles but was much higher as compared with the ovulatory cycles [3, 20]. The high impedance of flow was partially caused by the defective corpus luteum formation and angiogenesis [21]. Yun et al. [22] reported that more than half of LUF cycles had luteal phase shorter than 11 days, suggesting inadequate luteal functions presenting in LUF cycle. There was evidence that the incidence of LUF in ovulation cycles were higher than that in natural cycle [23]. In a study, the incidence of LUF was reported 58.9% in ovulation induction cycle (clomiphene citrate cycle) [4]. But another study that monitored ultrasonographically 45 cycles of 40 infertile patients treated with clomiphene showed that no LUF occurrence [24]. Later study showed that after ovulation induction with CC/HMG/HCG, patients with LUF had similar ovulation development, the estrogen, LH and FSH levels before HCG administration were similar with those in ovulation cycles. But in LUF cycles the P level in mid-luteal phase was significantly lowered [25].
Inadequate luteal functions and retarded development of endometrium might influence the embryos implantation and their survival rate. Given the possible controversy effect on the application of FET in LUF cycles, some reproductive medical centers gave up performing FET in LUF cycles. But the recurrence of LUF was said to be as high as 90% [4], infeasibility of FET due to the recurrent LUF will lead to consumption of time, increasing mental and economical burdens. Assuming that by adopting luteal support protocols, we could increase the pregnancy and implantation rate of FET in LUF cycles. To reach this goal, luteal support protocols were given in LUF cycles to correct the possible inadequate luteal functions and facilitate the implantation and development of embryos; also the same luteal supports were given in ovulation cycles as control. The results of this study showed that the levels of blood hormones in LUF cycles were closed to that in ovulation cycles. Yimin and Hefeng [26] reported a case of FET in a LUF patient, that achieved a successful pregnancy and delivery and concluded that FET would be applicable to patients with intact endometrium and appropriate luteal support. But this assumption had not yet supported by experiments of larger sampling size. The present study reviewed the outcomes of FET in 144 Chinese LUF women. The results showed that no significant differences in serum E2, P and P/E2 measured on the day of transfer and day 3 after the transfer were noted between LUF group and ovulation group. Besides, no significant differences in implantation rate, clinical pregnancy rate, ongoing pregnancy rate and live birth rate between LUF and ovulation group were noted. In conclusion, our data suggest that FET might be a safe and workable procedure in LUF cycle if luteal phase support is given. Further study on FET for LUF patient with relapsing risks was warranted.
References
Summaria V, Speca S, Mirk P. Ovarian factor infertility. Rays 1998;23:709–26.
Lizhu Z, editor. Clinical reproductive endocrine and infertility. Beijing: Science; 2000. pp. 446–7.
Dal J, Vural B, Caliskan E, Ozkan S, Yucesoy I. Power Doppler ultrasound studies of ovarian, uterine, and endometrial blood flow in regularly menstruating women with respect to luteal phase defects. Fertil Steril. 2005;84:224–7.
Qublan H, Amarin Z, Nawasreh M, Diab F, Malkawi S, Al-Ahmad N, et al. Luteinized unruptured follicle syndrome: incidence and recurrence rate in infertile women with unexplained infertility undergoing intrauterine insemination. Hum Reprod. 2006;21:2110–3.
Check JH, Adelson HG, Dietterich C, Stern J. Pelvic sonography can predict ovum release in gonadotrophin-treated patients as determined by pregnancy rate. Hum Reprod. 1990;5:234–6.
Jie Q, Meizhi L. Analysis of the factors related with luteinized untrupture follicle syndrome of patients with polycystic ovarian syndrome after ovulation induction. Chin J Clin Obstet Gynecol. 2000;1:137–40.
Coulam CB, Hill LM, Breckle R. Ultrasonic evidence for luteinization of unruptured preovulatory follicles. Fertil Steril. 1982;37:524–9.
Testart J, Lassalle B, Belaisch-Allart J, Hazout A, Forman R, Rainhorn JD, et al. High pregnancy rate after early human embryo freezing. Fertil Steril. 1986;46:268–72.
Van Royen E, Mangelschots K, De Neubourg D, Valkenburg M, Van de Meerssche M, Ryckaert G, et al. Characterization of a top quality embryo, a step towards single-embryo transfer. Hum Reprod. 1999;14:2345–9.
Steer CV, Mills CL, Tan SL, Campbell S, Edwards RG. The cumulative embryo score: a predictive embryo scoring technique to select the optimal number of embryos to transfer in an in-vitro fertilization and embryo transfer programme. Hum Reprod. 1992;7:117–9.
Jewelewicz R. Management of infertility resulting from anovulation. Am J Obstet Gynecol. 1975;122:909–20.
Marik J, Hulka J. Luteinized unruptured follicle syndrome: a subtle cause of infertility. Fertil Steril. 1978;29:270–4.
Gumen A, Wiltbank MC. Length of progesterone exposure needed to resolve large follicle anovular condition in dairy cows. Theriogenology 2005;63:202–18.
Gottsch ML, Van Kirk EA, Murdoch WJ. Tumour necrosis factor alpha up-regulates matrix metalloproteinase-2 activity in periovulatory ovine follicles: metamorphic and endocrine implications. Reprod Fertil Dev. 2000;12:75–80.
Murdoch WJ, Gottsch ML. Proteolytic mechanisms in the ovulatory folliculo-luteal transformation. Connect Tissue Res. 2003;44:50–7.
Hamilton CJ, Wetzels LC, Evers JL, Hoogland HJ, Muijtjens A, de Haan J. Follicle growth curves and hormonal patterns in patients with the luteinized unruptured follicle syndrome. Fertil Steril. 1985;43:541–8.
Salhab AS, Amro BI, Shomaf MS. Further investigation on meloxicam contraceptivity in female rabbits: luteinizing unruptured follicles, a microscopic evidence. Contraception 2003;67:485–9.
Stone S, Khamashta MA, Nelson-Piercy C. Nonsteroidal anti-inflammatory drugs and reversible female infertility: is there a link? Drug Safety 2002;25:545–51.
Westfahl PK. Circulating sex steroids after induction of luteinized unruptured follicles in adult guinea pigs. Steroids 1988;51:101–14.
Merce LT, Garces D, Barco MJ, de la Fuente F. Intraovarian Doppler velocimetry in ovulatory, dysovulatory and anovulatory cycles. Ultrasound Obstet Gynecol. 1992;2:197–202.
Abulafia O, Sherer DM. Angiogenesis of the ovary. Am J Obstet Gynecol. 2000;182:240–6.
Yun F, Zijiang C, Zhongli Y. Luteinized unruptured follicle syndrome: clinical analysis of 30 cases. Acta Academic Medicine Shandong 1994;32:236–8.
Giannopoulos T, Sherriff E, Croucher C. Follicle tracking of women receiving clomiphene citrate for ovulation induction. J Obstet Gynaecol. 2005;25:169–71.
Randall JM, Templeton A. The effects of clomiphene citrate upon ovulation and endocrinology when administered to patients with unexplained infertility. Hum Reprod. 1991;6:659–64.
Coetsier T, Dhont M. Complete and partial luteinized unruptured follicle syndrome after ovarian stimulation with clomiphene citrate/human menopausal gonadotrophin/human chorionic gonadotrophin. Hum Reprod. 1996;11:583–7.
Yimin Z, Hefeng H. Successful clinical pregnancy after transfer of frozen–thawed embryo. Journal of Zhejiang University (Medical Sciences) 2000;29:14–5.
Acknowledgements
This research was supported by the Prospective Clinical and Basic Research in Obstetrics and Gynecology: 985 Disciplinary Development Project in China (grant number: 985-2-015-24).
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Wang, L., Qiao, J., Liu, P. et al. Effect of luteinized unruptured follicle cycles on clinical outcomes of frozen thawed embryo transfer in Chinese women. J Assist Reprod Genet 25, 229–233 (2008). https://doi.org/10.1007/s10815-008-9225-2
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s10815-008-9225-2