Abstract
To evaluate evidence for motor impairment specificity in autism spectrum disorder (ASD) and attention deficit/hyperactivity disorder (ADHD). Children completed performance-based assessment of motor functioning (Movement Assessment Battery for Children: MABC-2). Logistic regression models were used to predict group membership. In the models comparing typically developing and developmental disability (DD), all three MABC subscale scores were significantly negatively associated with having a DD. In the models comparing ADHD and ASD, catching and static balance items were associated with ASD group membership, with a 1 point decrease in performance increasing odds of ASD by 36 and 39 %, respectively. Impairments in motor skills requiring the coupling of visual and temporal feedback to guide and adjust movement appear specifically deficient in ASD.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Movement impairment is a common co-occurring symptom in children with developmental disorders, including autism spectrum disorders (ASD) and attention-deficit/hyperactivity disorder (ADHD). For instance, Green et al. (2009) found that 79 % of children with ASD demonstrated movement impairments on performance-based assessment (i.e., Movement Assessment Battery for Children: M-ABC). Additionally, Jansiewicz et al. (2006) found high positive (82.2 %) and negative (87.5 %) predictive power of motor assessment (using the Physical and Neurological Exam for Subtle Signs: PANESS) in differentiating between children with ASD and typically developing (TD) children. Lower prevalence of motor impairment is described for children with ADHD, with 36 % of children with ADHD demonstrating significant motor impairment on the M-ABC, with an additional 28 % scoring in the borderline range (Wang et al. 2011). Other reports have purported that up to 55 % of children with ADHD meet criteria for Developmental Coordination Disorder (DCD; Watemberg et al. 2007), which may be more evident for children with the inattentive subtype (64.3 % compared with 11 % for the hyperactive/impulsive type). Though somewhat inconsistent with the greater body of literature describing the presence of motor impairments in ADHD, recent report (Papadopoulos et al. 2012) suggested that when screening out children with ADHD plus autism symptomatology (i.e., examining a group of children with pure ADHD), motor impairments are not evident, and thus reflect the overlap between ADHD and ASD. Contrary to this, MacNeil and Mostofsky (2012) found that both children with ADHD and children with ASD show impairment in basic motor control as assessed by the PANESS.
While motor skill impairments are described in both ASD and ADHD, it remains unclear whether there is evidence for specificity of motor impairment within different clinical groups. For instance, using the M-ABC, children with Asperger’s syndrome have been shown to demonstrate greater impairments in throwing and catching while children with DCD demonstrate greater impairments in balance and dexterity (Green et al. 2002). Similarly, Whyatt and Craig (2012, 2013) consistently found that children with autism exhibit particular deficits in catching a ball on the MABC-2, suggesting that motor skill deficits in children with autism may be specific to perception–action coupling, or the ability to integrate visual spatial and temporal characteristics of an action, rather than general motor abilities; in these studies, additional impairments in balance and manual dexterity were respectively identified. Impairment in tasks involving visual-motor feedback has been further supported in the literature (Fulkerson and Freeman 1980; Minshew et al. 1997; Stieglitz Ham et al. 2008) using measures other than the M-ABC. Additionally, Haswell et al. (2009) reported that in learning an internal model of the novel tool, children with ASD placed an excessive association between self-generated motor commands and proprioception, and a less than normal association between the same motor commands and the visual feedback.
Motor impairments described for children with ADHD appear less specific. For instance, Wang et al. (2011) reported that children with ADHD exhibited poorer motor ability on all three domains of the M-ABC compared to typically developing (TD) children. Other examination supports the notion of more widespread motor deficits in ADHD. Kooistra et al. (2009) found that children with ADHD performed in the clinical range on the Clinical Observations of Motor and Postural Skills (COMPS), a measure assessing subtle perceptuo-motor problems using six motor tasks: slow (ramp) movements, rapid forearm rotation (dysdiadochokinesis), finger–nose touching, prone extension posture, asymmetrical tonic neck reflex, and supine flexion. Taken together, the literature suggests that children with ADHD have a more general impairment in basic motor abilities.
While there is substantial evidence indicating motor impairment in both ASD and ADHD, few studies have simultaneously compared the motor profiles for these populations using a comprehensive measure of motor functioning. Two studies examined basic motor control as well as ideomotor praxis (performance of skilled motor gestures) among children with ASD, ADHD and TD children, with one of those studies also including a fourth developmental coordination disorder (DCD) group. In both studies, investigators found that both children with ASD and ADHD had significantly impaired motor coordination skills, but only children with ASD exhibited generalized impairment in gestural performance (MacNeil and Mostofsky 2012; Dewey et al. 2007). While these studies did reveal differences in motor functioning between children with ASD and children with ADHD, these differences were specific to praxis. For both studies, overall levels of basic motor control were found to be similar in children with ASD and ADHD; however, neither study included a detailed, item-specific analysis of motor control or coordination.
Another study comparing motor functioning among children with ASD, ADHD, and TD children found that both children with ASD and ADHD had poorer gross motor skills compared to TD children (Pan et al. 2009). In addition, both groups performed poorer on subtests assessing locomotor skills (run, gallop, hop, leap, horizontal jump, skip, and slide) and object control skills (two-hand strike, stationary bounce, catch, kick, and overhand throw), with the ASD group performing poorer than the ADHD group (Pan et al. 2009). Though this study highlights some motor deficits seen in children with ASD and ADHD and provides evidence for greater impairment in children with ASD, it does not indicate what specific types of motor deficits differ between the two diagnostic groups.
A final study examined predictors of motor impairment and associations between motor impairment and daily living skills in children with ASD, ADHD, and DCD, but did not compare the motor profiles of these diagnostic categories (Kopp et al. 2010). Therefore, additional research is needed to further determine motor impairment specificity in children with ASD and ADHD.
The present study aims to compare motor functioning among three groups: children with ASD, children with ADHD, and TD children in order to better define motor deficits in these clinical groups and understand whether motor deficits assist in distinguishing between clinical groups. Building on findings from the few prior studies of motor function in children with ASD and ADHD, we sought to examine the specific profile of impairments in basic motor control and coordination. It was hypothesized that children with ASD and children with ADHD would show greater impairment in motor functioning compared to the TD children, with more pronounced impairment in the ASD group. Specifically, given evidence that children with ASD tend to discount visual feedback during motor learning (Haswell et al. 2009; Izawa et al. 2012) it was predicted that tasks relying more heavily on visual-motor feedback (e.g., catching) would be more impaired in children with ASD than ADHD. Similarly, it was further hypothesized that these tasks involving visual-motor feedback would best discriminate between children with ASD and ADHD.
Methods
Participants
A total of 200 children, ages 8–13 years, participated in the present study: 56 children with ASD (mean age = 10.27, SD = 1.28; 8 girls), 63 children with ADHD (mean age = 9.98, SD = 1.34; 9 girls), and 81 TD children (mean age = 10.31, SD = 1.18; 12 girls). Participants were recruited from a variety of sources including local schools, pediatricians’ offices, outpatient clinics at the [Kennedy Krieger Institute], advertisements posted in local community centers, local Autism Society of America chapters, local chapters of Children and Adults with Attention-Deficit Hyperactivity Disorder, and by word of mouth.
Children with ASD met the Diagnostic and Statistical Manual of Mental Disorders, Fourth Edition (DSM-IV) criteria (American Psychiatric Association 2000). The Autism Diagnostic Interview-Revised (ADI-R; Lord et al. 1994), the Autism Diagnostic Observation Schedule-G, Module 3 (ADOS-G; Lord et al. 2000)/Autism Diagnostic Observation Schedule-Second Edition, Module 3 (ADOS-2; Lord et al. 2012), and clinical judgment were used to establish ASD diagnoses. All participants had to meet on the basis of clinical judgment and diagnostic criteria on the ADI-R, ADOS-G/ADOS-2, or both. If there was a history of known etiology for autism (e.g., fragile X syndrome, tuberous sclerosis, phenylketonuria, or congenital rubella) or a history of documented prenatal or perinatal insult, then children were excluded from the ASD group.
Children with ADHD met the DSM-IV criteria. The Diagnostic Interview for Children and Adolescents-IV (DICA-IV; Reich et al. 1997) was used to establish ADHD diagnoses. Children were also required to have positive scores on at least one of the parent rating scales (i.e., T-score of 65 or higher on the Inattentive or Hyperactive-Impulsive scale) on the Conners’ Parent Rating Scales-Revised (CPRS-R; Conners 1997) or scores of 2 or 3 on at least 6 of the 9 items on the Inattentive or Hyperactivity/Impulsivity scales on the ADHD Rating Scale-IV, home and school versions (ADHDRS; DuPaul et al. 1998). Children were excluded from the ADHD group if they met criteria for conduct, mood, generalized anxiety, separation anxiety, or obsessive–compulsive disorders on the DICA-IV. Diagnoses of oppositional defiant disorder (ODD) and simple phobias were allowed. While findings from previous studies suggest that ADHD associated with conduct disorder may be a distinct subtype, this is not the case for ADHD associated with ODD (Biederman et al. 1992; Faraone et al. 1995).
In addition, extensive telephone interviews were performed to screen for social problems and autism symptoms, and all children were evaluated by a psychology associate and a child neurologist (with extensive experience in diagnosing children with neurodevelopmental disorders, particularly ASD and ADHD) prior to inclusion. Children included in the ADHD group had no reported history of ASD and did not present with behaviors associated with ASD when evaluated by the psychology associate and child neurologist.
Participants were not eligible for the group of TD children if, based on the DICA-IV, they had a history of a developmental or psychiatric disorder. They were also excluded if they had an immediate family member with autism or another pervasive developmental disorder.
Children were excluded from all three groups if there was prior documented history of a definitive neurological disorder (including seizures, tumors, traumatic brain injury, stroke, or lesions), a severe chronic medical disorder, visual impairment, substance abuse or dependence, or childhood schizophrenia or psychosis. Potential participants were screened and excluded appropriately after gathering information during a phone screening.
The ADHD sample included 26 children with comorbid diagnoses (25 with ODD and 5 with a simple and/or social phobia). The ASD sample included 40 children with comorbid diagnoses (31 with ADHD, 16 with ODD, 12 with a simple and/or social phobia, six with generalized anxiety disorder, one with separation anxiety disorder, one with major depressive disorder, one with dysthymic disorder, two with obsessive compulsive disorder, and two with a history of major depressive disorder or a major depressive episode). Comorbidities were determined using the DICA-IV.
Forty-three children with ADHD were taking stimulant medications. Children with ADHD taking long acting medications, such as atomoxetine, guaneficine, and clonidine, were excluded. Children with ASD were not excluded on the basis of any specific medications, unless the medication related to an exclusionary comorbid disorder. Thirty-eight children with ASD were taking psychoactive medications (24 were taking stimulants; 11 anti-depressants; 8 sympatholytic medication; 3 neuroleptics; 1 mood stabilizer; and 1 N-Methyl-d-aspartate receptor antagonist). In addition, parents of children (both children with ASD and ADHD) taking stimulants were asked to withhold the child's medication the day prior to and the day of each study visit. All other medications were taken as prescribed. Children in the control group were not taking any psychotropic medications.
For all groups, intellectual functioning was evaluated using the Wechsler Intelligence Scale for Children-Fourth Edition (WISC-IV; Wechsler 2003). Generally, children were eligible to participate if they had a Full Scale IQ greater than 80. However, if this criterion was not met and there was a 12-point or greater discrepancy between index scores, children were eligible if their Verbal Comprehension Index (VCI) or Perceptual Reasoning Index (PRI) was greater than 80 and the lower of the two was at least 65. One child was included in this study that did not meet the above intellectual functioning criteria, but was still considered to be high functioning. This child had a VCI of 79 and a PRI of 86 (but did not have a 12-point or greater discrepancy between index scores). Demographics for ASD, ADHD, and TD participants are shown in Table 1.
Procedures
The [Johns Hopkins University School of Medicine] Institutional Review Board approved this study. Written consent was obtained from a parent or legal guardian and assent was obtained from every child. Parents completed telephone interviews regarding their child’s behavior, developmental, and medical history prior to their research appointment. Children were administered the WISC-IV and the Movement Assessment Battery for Children, Second Edition (MABC-2; Henderson et al. 2007). These measures were administered as part of larger, ongoing projects examining motor development in both children with ASD and ADHD.
Measures
Movement Assessment Battery for Children: Second Edition (MABC-2; Henderson et al. 2007)
The MABC-2 is a performance-based assessment evaluating motor skill ability. For the present sample, the second (ages 7–10) and the third (ages 11–16) age bands were administered. Both age bands consist of 11 item and three subtest scores: Manual Dexterity, Balance, and Ball Skills. Higher scores indicate better functioning. Item and subtest standard (scaled) scores based on the normative sample were examined in analyses.
Statistical Analysis
Statistical analyses were completed in R (R Core Team 2013). To compare group differences in motor functioning, a series of conditional logistic regression models was used (McCullagh and Nelder 1989) (see Figs. 1, 2). The first logistic model compared motor functioning between TD children and children with a developmental disorder, either ASD or ADHD. The second logistic model compared motor functioning between children with ADHD and children with ASD, controlling for Conners inattention and hyperactivity-impulsivity scores. The final logistic model compared motor functioning of children with ASD and comorbid ADHD to children with ASD who did not have a comorbid diagnosis of ADHD, controlling for Conners inattention and hyperactivity-impulsivity scores and ADOS total score. In this model, gender and PRI were also controlled for, as significant differences in gender and PRI between groups were identified.
a (Model 1) Coefficients and 95 % confidence intervals for models comparing TD children and children with DD. Coefficients and confidence intervals are given as odds ratios, where the outcome of interest is DD. The coefficients reflect the association between a 1-point decrease in mABC score and the odds of DD. The solid gray line corresponds to an odds ratio equal to 1, indicating no relationship between mABC score and the odds of DD. Significant relationships (before correcting for multiple comparisons) are shown in solid black, while non-significant relationships are shown in dashed black. b (Model 2) Coefficients and 95 % confidence intervals for models comparing children with ASD and children with ADHD. Coefficients and confidence intervals are given as odds ratios, where the outcome of interest is ASD. The coefficients reflect the association between a 1-point decrease in mABC score and the odds of ASD. The solid gray line corresponds to an odds ratio equal to 1, indicating no relationship between mABC score and the odds of ASD. Significant relationships (before correcting for multiple comparisons) are shown in solid black, while non-significant relationships are shown in dashed black. c (Model 3) Coefficients and 95 % confidence intervals for models comparing children with ASD with and without comorbid ADHD. Coefficients and confidence intervals are given as odds ratios, where the outcome of interest is comorbid ADHD. The coefficients reflect the association between a 1-point decrease in mABC score and the odds of comorbid ADHD. The solid gray line corresponds to an odds ratio equal to 1, indicating no relationship between mABC score and the odds of comorbid ADHD. Significant relationships (before correcting for multiple comparisons) are shown in solid black, while non-significant relationships are shown in dashed black
For each of the outcomes described above, two models were fit: a subscale-level model and an item-level model. The subscale-level model included as predictors total scores for each MABC subscale (Manual Dexterity, Aiming and Catching, and Balance). The item-level model included as predictors all individual MABC items. We conducted a t test at a significance level of 0.05, adjusting for multiple comparisons using Bonferroni correction within each model.
As MABC item scores within each subscale were highly correlated, sequential orthogonalization was employed to reduce multi-collinearity for the item-level regression models. Items within each subscale were ordered by strength of association with the outcome. The most important item within each subscale was left unchanged, and the less important items were orthogonalized with respect to all the items in the same subscale with stronger association with the outcome. This approach is known as stepwise orthogonalization (Forina et al. 2007), dominant component analysis (Šoškic et al. 1996), and SELECT (Kowalski and Bender 1976), and is used to reduce collinearity while preserving predictor variable interpretability.
Results
Group Differences on the MABC-2
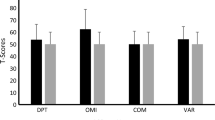
A univariate analysis of variance for the MABC-2 total standard score indicated that there was a significant main effect of group [F (2, 197) = 62.04, p < 0.001]. The Bonferroni post hoc test was used to examine potential differences in MABC-2 score between diagnostic groups. Bonferroni pair-wise comparisons among the diagnostic groups revealed the following: There was a statistically significant difference in total MABC-2 score between the TD group (M = 8.90, SD = 2.52) and both the ADHD (M = 6.38, SD = 2.67) and ASD groups (M = 4.14, SD = 2.19). There was also a statistically significant difference in total MABC-2 score between the ADHD and ASD group (Table 2).
Group Classification Using the MABC
Tables 3, 4, 5 shows point estimates, 95 % confidence intervals (95 % CIs) and p values for the coefficients of the subscale-level and item-level models for each outcome. While significance levels are Bonferroni-corrected for multiple comparisons, confidence intervals and p values are reported uncorrected. Coefficient estimates and confidence intervals are given as odds ratios. Confidence interval endpoints were obtained by exponentiating the endpoints of the 95 % CIs for the model coefficients.
In the subscale-level model comparing TD children and children with a developmental disorder, all three MABC subscale scores (Manual Dexterity, Aiming and Catching, and Balance) were significantly negatively associated with having a DD (Table 3A). Every 1-point decrease in MABC subscale score was associated with an increase in the odds of DD by 30.3 % (95 % CI 11.7, 52.0 %; p = 0.001) for the manual dexterity subscale; 19.7 % (CI 5.6, 35.8 %; p = 0.005) for the ball skills subscale; and 21.6 % (CI 6.5, 39.0 %; p = 0.004) for the balance subscale. In the item-level model, manual dexterity item 1 (pegboard), catching, and balance item 2 (dynamic balance) were significantly associated with having a DD (Table 3B). Every 1-point decrease in item score was associated with an increase in the odds of DD by 25.9 % (CI 8.0, 46.7 %; p = 0.003) for manual dexterity item 1; 24.3 % (CI 9.3, 41.4 %; p = 0.001) for catching; and 21.5 % (CI 9.3, 35.2 %; p < 0.001) for balance item 2.
In the subscale-level model comparing children with ADHD and children with ASD, the Aiming and Catching and Balance subscale scores were significantly associated with having ASD as the primary diagnosis (Table 4A). Every 1-point decrease in the Aiming and Catching score was associated with a 32.3 % (CI 10.6, 58.3 %; p = 0.002) increase in the odds of ASD, while a 1-point decrease in the Balance score was associated with a 34.7 % (CI 10.3, 64.5 %; p = 0.004) increase in the odds of ASD. In the item-level model, catching (and static balance were significantly associated with ASD as compared to ADHD, with every 1-point decrease in catching score being associated with a 35.9 % (CI 13.1, 63.4 %; p = 0.001) increase in the odds of ASD and every 1-point decrease in balance item 1 score being associated with a 39.1 % (CI 12.0, 72.7 %; p = 0.003) increase in the odds of ASD as compared to ADHD (Table 4B). While no manual dexterity item was significant after Bonferroni correction, manual dexterity item 3 (tracing task) was significantly associated with ADHD before correction, with every 1-point decrease in item score being associated with a 20.2 % (CI 1.6, 42.2 %; p = 0.031) increase in the odds of ADHD as compared to ASD. Furthermore, balance item 3 was significantly associated with ASD before correction, with every 1-point decrease in item score being associated with a 17.5 % (CI 0.2, 37.8 %; p = 0.048) increase in the odds of ASD as compared to ADHD.
In the subscale-level and item-level models comparing children with ASD and comorbid ADHD to children with ASD without comorbid ADHD, no subscale or item scores were significantly associated with having comorbid ADHD (Table 5).
Discussion
This study examined the specificity of motor impairments identified in children diagnosed with ASD and ADHD compared to TD children. As hypothesized and consistent with previous literature (e.g., Green et al. 2009; Wang et al. 2011; Watemberg et al. 2007), both the ASD and the ADHD groups in this study evidenced motor impairment compared to the TD group based on overall performance on the MABC-2. In addition, the first hypothesis was further supported in that children in the ASD group demonstrated greater overall motor impairment compared to children with ADHD. These findings are generally consistent with previous reports suggesting that motor impairment is more severe in ASD than ADHD (Green et al. 2009; Wang et al. 2011), and may be more strongly associated with social symptomatology uniquely seen in ASD (Papadopoulos et al. 2012; Dziuk et al. 2007; Dowell et al. 2009). With that said, in this sample children with ADHD showed significant deficits as compared to typically developing children on performance-based motor assessment. As such, it appears that there are clear motor deficits evidenced in each disorder that do not appear exclusively related to social features of ASD.
Also consistent with previous reports (e.g., Whyatt and Craig 2012), performance on the catching task and a task that taxes ability to maintain balance (so called “static balance”) were the most robust predictors of ASD diagnosis when differentiating between ASD and ADHD (i.e., by each point decrease on the catching and balance tasks, the odds of having ASD versus ADHD was increased by about 36 and 39 %, respectively). In addition, while overall performance on manual dexterity, balance, and ball skills activities were associated with having either ASD or ADHD, only the catching and balance items remained significant when differentiating between ASD and ADHD. These findings suggest that multiple deficits in motor functioning may be related to having a neurodevelopmental disability; however, deficits in tasks involving visual feedback and static balance are most aligned with having an ASD. These tasks share a demand for integrating spatial and temporal characteristics of movement (Whyatt and Craig 2012), requiring in-the-moment adjustments for successful completion. These in-the-moment adjustments are required for coordinating whole body movements such as walking, running, and playing sports. Such deficits may be associated with abnormal gait in children with ASD. In contrast, performance on manual dexterity tasks appeared more strongly related to ADHD group membership, as decreased performance on a tracing task was more strongly associated with ADHD vs. ADHD diagnosis (each point decrease resulted in 20 % increase in odds of ADHD). These deficits in manual dexterity may translate into difficulty holding and manipulating small objects, as is necessary to handwriting, cutting with scissors, and performing a variety of dressing skills. Taken together, these findings reflect some degree of specificity of impairment in perception–action coupling for children with ASD, even for those children with ASD and comorbid ADHD. As such, it remains critical to examine component tasks of the MABC2 rather than subscales, particularly when describing deficits realized by children with ASD (e.g., as only deficits are demonstrated on static as compared to dynamic balance tasks).
The findings of specific ASD-associated impairment on the catching task, requiring rapid integration of visual feedback, is in line with previous work suggesting that children with ASD are less likely to rely on visual feedback when learning a novel movement pattern, instead showing a bias towards reliance on proprioceptive feedback (Haswell et al. 2009; Izawa et al. 2012). Additionally, Izawa et al. (2012) found that children with ADHD showed a motor learning pattern indistinct from TD children, establishing some specificity for this atypical bias in sensory-motor integration in autism. Further, this bias towards reliance on proprioceptive, rather than visual, feedback was robustly correlated with core social impairments of autism as well as impairments in imitation and praxis (Haswell et al. 2009). It follows that limited visual-motor integration, reflected in poor catching, may be associated with autism-associated difficulties with learning social skills through imitation of others’ actions. The brain basis for these impairments may lie in altered patterns of connectivity. There is evidence suggesting that autism is associated with a pattern of over-connectivity within/between neighboring brain regions and long-range under-connectivity (Herbert et al. 2004; Happé and Frith 2006). Taken together, poor catching, combined with findings described above outlining deficits specific to ASD in motor learning, suggest that motor difficulties in autism may be associated with abnormalities in frontal-posterior connectivity. The cerebellum is also crucial to sensory-motor integration, and deficits in motor coordination and visual feedback control have been linked to impaired cerebellar functioning (Ogawa et al. 2006; Salmi et al. 2010); as such, this difficulty with efficient visual-motor integration in children with ASD may alternatively be due to cerebellar dysfunction. Linking these neurological findings to impairment in motor tasks involving visual feedback offers insight into the phenotypic presentation of ASD, whereby children have difficulty with visual aspects of socialization, including imitation and appreciation nonverbal cues, exhibiting both a motor and social dyspraxia.
Our findings suggest that the presence of ADHD, including in children with ASD, may particularly impact performance of manual dexterity tasks. While the mABC2 manual dexterity tasks also require visual guidance, the requirement for visual integration is not as strenuous as it is in ball-catching which requires rapidly altering hand motion based on a moving stimulus (in contrast to the stationary stimuli used for manual dexterity tasks). Rather, manual dexterity tasks require high degrees of facile control and selection of motor actions. Children with ADHD are known to have particular difficulty with efficient response selection and control, including impaired motor inhibition (MacNeil and Mostofsky 2012; Gilbert et al. 2011; Wu et al. 2012), and in contrast to children with ASD, they do not appear to discount visual feedback during motor learning (Izawa et al. 2012). It therefore appears most likely that ADHD-associated inefficient response selection might impact the ability to effectively execute the motor control necessary to perform the tracing task under the manual dexterity component of the MABC-2. Additionally, children with ADHD and deficient response inhibition may have been more likely to sacrifice accuracy for speed on this task, resulting in lower performance.
In conclusion, through performance comparison on a frequently used measure of motor impairment (MABC-2) among clinical groups (ASD and ADHD), specificity of motor impairment in ASD and possibly ADHD was identified. While previous research has suggested that impairments in catching and “static” balance are present in ASD, findings from the present study suggest that these deficits are somewhat specific to ASD and are robust in predicting ASD diagnosis from other developmental disorders evidencing motor impairment (i.e., ADHD).
Limitations to this study include the restricted age range of our clinical sample as well as the restricted range in functioning. Due to these range restrictions, it is more difficult to generalize the findings of this study to the larger autism population. Given our findings, future research is warranted to further describe the specificity of motor impairments in a less restricted sample of children with ASD, particularly with more severe autism and cognitive impairments, or younger/older. Additional research should also examine motor functioning using kinematic motor tasks, which provide a more sensitive assessment of movement and may highlight more subtle differences in motor functioning in children with ASD and ADHD. Further defining the specificity of motor impairment in the broader ASD population will potentially allow for a better understanding of the etiology and impact of these impairments and help to improve interventions targeting acquisition of skills necessary to motor, as well as social, functioning.
References
American Psychiatric Association. (2000). Diagnostic and statistical manual of mental disorders (4th ed., text rev.). Washington, DC: Author.
Biederman, J., Faraone, S. V., Keenan, K., Benjamin, J., Krifcher, B., Moore, C., et al. (1992). Further evidence for family-genetic risk factors in attention deficit hyperactivity disorder: Patterns of comorbidity in probands and relatives in psychiatrically and pediatrically referred samples. Archives of General Psychiatry, 49(9), 728.
Conners, C. K. (1997). Conners’ Parent Rating Scales-Revised. New York, NY: Multi-Health Systems.
Dewey, D., Cantell, M., & Crawford, S. G. (2007). Motor and gestural performance in children with autism spectrum disorders, developmental coordination disorder, and/or attention deficit hyperactivity disorder. Journal of the International Neuropsychological Society, 13, 246–256.
Dowell, L. R., Mahone, E. M., & Mostofsky, S. H. (2009). Associations of postural knowledge and basic motor skill with dyspraxia in autism: Implication for abnormalities in distributed connectivity and motor learning. Neuropsychology, 23(5), 563–570.
DuPaul, G. J., Power, T. J., Anastopoulos, A. D., & Reid, R. (1998). ADHD Rating Scale—IV: Checklists, norms, and clinical interpretation. New York, NY: Guilford Press.
Dziuk, M. A., Larson, J. C., Apostu, A., Mahone, E. M., Denckla, M. B., & Mostofsky, S. H. (2007). Dyspraxia in autism: Association with motor, social, and communicative deficits. Developmental Medicine and Child Neurology, 49(10), 734–739.
Faraone, S. V., Biederman, J., Chen, W. J., Milberger, S., Warburton, R., & Tsuang, M. T. (1995). Genetic heterogeneity in attention-deficit hyperactivity disorder (ADHD): Gender, psychiatric comorbidity, and maternal ADHD. Journal of Abnormal Psychology, 104(2), 334.
Forina, M., Lanteri, S., Casale, M., & Cerrato Oliveros, M. (2007). Stepwise orthogonalization of predictors in classification and regression techniques: An “old” technique revisited. Chemometrics and Intelligent Laboratory Systems, 87(2), 252–261.
Fulkerson, S. C., & Freeman, W. M. (1980). Perceptual-motor deficiency in autistic children. Perceptual and Motor Skills, 50(1), 331–336.
Gilbert, D. L., Isaacs, K. M., Augusta, M., Macneil, L. K., & Mostofsky, S. H. (2011). Motor cortex inhibition: A marker of ADHD behavior and motor development in children. Neurology, 76(7), 615–621.
Green, D., Baird, G., Barnett, A. L., Henderson, L., Huber, J., & Henderson, S. E. (2002). The severity and nature of motor impairment in Asperger’s syndrome: A comparison with specific developmental disorder of motor function. Journal of Child Psychology and Psychiatry, 43(5), 655–668.
Green, D., Charman, T., Pickles, A., Chandler, S., Loucas, T., Simonoff, E., et al. (2009). Impairment in movement skills of children with autistic spectrum disorders. Developmental Medicine and Child Neurology, 51(4), 311–316.
Happé, F., & Frith, U. (2006). The weak coherence account: Detail-focused cognitive style in autism spectrum disorders. Journal of Autism and Developmental Disorders, 36(1), 5–25.
Haswell, C. C., Izawa, J., Dowell, L. R., Mostofsky, S. H., & Shadmehr, R. (2009). Representation of internal models of action in the autistic brain. Natural Neuroscience, 12(8), 970–972.
Henderson, S. E., Sugden, D. A., & Barnett, A. L. (2007). Movement Assessment Battery for Children—Second Edition [Movement ABC-2]. London, UK: The Psychological Corporation.
Herbert, M. R., Ziegler, D. A., Makris, N., Filipek, P. A., Kemper, T. L., Normandin, J. J., et al. (2004). Localization of white matter volume increase in autism and developmental language disorder. Annals of Neurology, 55(4), 530–540.
Izawa, J., Pekny, S. E., Marko, M. K., Haswell, C. C., Shadmehr, R., & Mostofsky, S. H. (2012). Motor learning relies on integrated sensory inputs in ADHD, but over-selectively on proprioception in autism spectrum conditions. Autism Research, 5(2), 124–136.
Jansiewicz, E. M., Goldberg, M. C., Newschaffer, C. J., Denckla, M. B., Landa, R., & Mostofsky, S. H. (2006). Motor signs distinguish children with high functioning autism and Asperger’s syndrome from controls. Journal of Autism and Developmental Disorders, 36(5), 613–621.
Kooistra, L., Ramage, B., Crawford, S., Cantell, M., Wormsbecker, S., Gibbard, B., et al. (2009). Can attention deficit hyperactivity disorder and fetal alcohol spectrum disorder be differentiated by motor and balance deficits? Human Movement Science, 28(4), 529–542.
Kopp, S., Beckung, E., & Gillberg, C. (2010). Developmental coordination disorder and other motor control problems in girls with autism spectrum disorder and/or attention-deficit/hyperactivity disorder. Research in Developmental Disabilities, 31, 350–361.
Kowalski, B. R., & Bender, C. F. (1976). An orthogonal feature selection method. Pattern Recognition, 8(1), 1–4.
Lord, C., Risi, S., Lambrecht, L., Cook, E. H, Jr, Leventhal, B. L., DiLavore, P. C., et al. (2000). The Autism Diagnostic Observation Schedule—Generic: A standard measure of social and communication deficits associated with the spectrum of autism. Journal of Autism and Developmental Disorders, 30(3), 205–223.
Lord, C., Rutter, M., DiLavore, P. C., Risi, S., Gotham, K., & Bishop, S. L. (2012). Autism diagnostic observation schedule (2nd ed.). North Tonawanda, NY: Multi-Health Systems Inc.
Lord, C., Rutter, M., & Le Couteur, A. (1994). Autism Diagnostic Interview-Revised: A revised version of a diagnostic interview for caregivers of individuals with possible pervasive developmental disorders. Journal of Autism and Developmental Disorders, 24(5), 659–685.
MacNeil, L. K., & Mostofsky, S. H. (2012). Specificity of dyspraxia in children with autism. Neuropsychology, 26(2), 165–171.
McCullagh, P., & Nelder, J. A. (1989). Generalized linear models. London: Chapman and Hall.
Minshew, N. J., Goldstein, G., & Siegel, D. J. (1997). Neuropsychological functioning in autism: Profile of a complex information processing disorder. Journal of the International Neuropsychological Society, 3(4), 303–316.
Ogawa, K., Inui, T., & Sugio, T. (2006). Separating brain regions involved in internally guided and visual feedback control of moving effectors: An event-related fMRI study. NeuroImage, 32, 1760–1770.
Pan, C. Y., Tsai, C. L., & Chu, C. H. (2009). Fundamental movement skills in children with autism spectrum disorders and attention deficit hyperactivity disorder. Journal of Autism and Developmental Disorders, 39, 1694–1705.
Papadopoulos, N., Rinehart, N. J., Bradshaw, J. L., Taffe, J., & McGinley, J. (2012). Is there a link between motor performance variability and social-communicative impairment in children with ADHD-CT: A kinematic study using an upper limb Fitts’ aiming task. Journal of Attention Disorders. doi:10.1177/1087054712454569.
R Core Team. (2013). R: A language and environment for statistical computing. R Foundation for Statistical Computing, Vienna, Austria. http://www.R-project.org/.
Reich, W., Welner, Z., & Herjanic, B. (1997). The Diagnostic Interview for Children and Adolescents-IV. North Towanda Falls, NY: Multi-Health Systems Inc.
Salmi, J., Pallesen, K. J., Neuvonen, T., Brattico, E., Korvenoja, A., Salonen, O., et al. (2010). Cognitive and motor loops of the human cerebro-cerebellar system. Journal of Cognitive Neuroscience, 22, 2663–2676.
Šoškic, M., Plavšic, D., & Trinajstic, N. (1996). Link between orthogonal and standard multiple linear regression models. Journal of Chemical Information and Computer Sciences, 36(4), 829–832.
Stieglitz Ham, H., Corley, M., Rajendran, G., Carletta, J., & Swanson, S. (2008). Brief report: Imitation of meaningless gestures in individuals with Asperger syndrome and high-functioning autism. Journal of Autism and Developmental Disorders, 38(3), 569–573.
Wang, H. Y., Huang, T. H., & Lo, S. K. (2011). Motor ability and adaptive function in children with attention deficit hyperactivity disorder. Kaohsiung Journal of Medical Sciences, 27(10), 446–452.
Watemberg, N., Waiserberg, N., Zuk, L., & Lerman-Sagie, T. (2007). Developmental coordination disorder in children with attention-deficit-hyperactivity disorder and physical therapy intervention. Developmental Medicine and Child Neurology, 49(12), 920–925.
Wechsler, D. (2003). Wechsler Intelligence Scale for Children-Fourth Edition (WISC-IV). San Antonio, TX: The Psychological Corporation.
Whyatt, C. P., & Craig, C. M. (2012). Motor skills in children aged 7–10 years, diagnosed with autism spectrum disorder. Journal of Autism and Developmental Disorders, 42(9), 1799–1809.
Whyatt, C. P., & Craig, C. M. (2013). Sensory-motor problems in autism. Frontiers in Integrative Neuroscience, 7(51), 1–12.
Wu, S. W., Gilbert, D. L., Shahana, N., Huddleston, D. A., & Mostofsky, S. H. (2012). Transcranial magnetic stimulation measures in attention-deficit/hyperactivity disorder. Pediatric Neurology, 47(3), 177–185.
Acknowledgments
This research was supported by Autism Speaks and by NIH: R01NS048527, R01 MH085328, R01 MH078160, the Johns Hopkins University School of Medicine Institute for Clinical and Translational Research, and NIH/NCRR CTSA Program, UL1-RR025005.
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Ament, K., Mejia, A., Buhlman, R. et al. Evidence for Specificity of Motor Impairments in Catching and Balance in Children with Autism. J Autism Dev Disord 45, 742–751 (2015). https://doi.org/10.1007/s10803-014-2229-0
Published:
Issue Date:
DOI: https://doi.org/10.1007/s10803-014-2229-0