Abstract
There have been few studies of psychopathology in adult with autism. This study examined psychiatric co-morbidity in 147 adults with intellectual disability (ID) and autism and 605 adults with ID but without autism. After controlling for the effects of gender, age, psychotropic medication and level of ID, people with autism and ID were no more likely to receive a psychiatric diagnosis than people with ID only. People with autism were less likely to receive a diagnosis of personality disorder. These findings cast doubts on the hypothesis that adults with ID and autism are more vulnerable to certain psychiatric disorders than non-autistic adults with ID.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
AutismFootnote 1 often co-exists with Intellectual Disability (ID) (Fombonne, Mazaubrun, Cans, & Grandjean, 1997; Gillberg, 1999). Although the increased incidence of psychiatric disorders in ID has been well documented (Deb, Mathews, Holt, & Bouras, 2001; Deb, Thomas, & Bright, 2001) it is unclear whether people with ID and autism are more prone to psychiatric disorders than people with ID only.
It has been often suggested that people with autism are more vulnerable to certain psychiatric disorders. For example, common interpersonal and cognitive impairments in autism and schizophrenia have historically contributed to a controversy on whether the two disorders were the same (Eisenberg & Kanner, 1958) or whether autism per se is a risk factor for later psychosis (Clarke, LittleJohns, Corbett, & Joseph, 1989; Petty, Ornitz, Michelman, & Zimmerman, 1984). This hypothesis has not received empirical support (Mouridsen, Rich, & Isager, 1999; Volkmar & Cohen, 1991). A large study by Volkmar and Cohen (1991) found the schizophrenia rate in people with autism to be similar to that expected in the general population. Correspondingly, Mouridsen et al. (1999) in a 22-year follow-up study of 38 people with autism found no one to have schizophrenia or any other psychotic disorder. There is some emerging evidence that affective disorders, especially depression, are the most common psychiatric disorders in people with autism. Rates of depression have been found to be increased among close relatives of people with autism (Piven & Palmer, 1999) and a number of studies have shown an increased rate of affective disorders and anxiety among first-degree relatives of people with autism compared to people with Down syndrome (Bolton, Pickles, Murphy, & Rutter, 1998; Lainhart, 1999). Bolton et al. (1998) found that both autistic-like symptoms and affective disorders were elevated among the relatives of people with autism compared to the relatives of people with Down syndrome. However, there was no correlation between measures of the broader autistic phenotype and affective disorders suggesting that affective disorders might not be part of the broader autistic phenotype. Increased carer burden cannot be excluded as potential contributing factor, especially considering emotional and psychosocial aspects of raising a child with autism.
Rates of depression are also increased among children and adolescents with autism, and with Asperger syndrome (Ghaziuddin, Ghaziuddin, & Greden, 2002; Gillberg & Billstedt, 2000). A systematic review of follow-up studies from childhood to adulthood (Howlin, 2000) has concluded that depression, often associated with severe anxiety, is the most common psychiatric disorder in high-functioning adults with autism. It is possible that high-functioning adults with autism might be more prone to such disorders, in part perhaps because of their greater insight into their deficits and greater sensitivity to social stigma, handicap and discrimination.
Recently, Morgan, Roy, and Chance (2003) reported the prevalence of psychiatric disorders based on ICD-10 criteria in a large sample of adults with ID and autism. Depressive disorders were more common in adults with ID and autism as compared to adults with ID but without autism, although there were no other psychopathology differences. These results suggest an increased vulnerability to depression in people with autistic spectrum disorders and ID. Unfortunately, potentially confounding variables such as age, gender, level of ID, and psychotropic medication were not controlled for. As a result, it remains unclear whether the obtained levels of psychiatric co-morbidity in the autistic sample were due to true differences or due to some confounding variables. Bradley, Summers, Wood, and Bryson (2004) studied psychopathology in adolescents with ID and autism and found that not only depression but most psychiatric disorders were elevated in people with autism compared to a matched control group, although in this study the sample size was small (N = 12).
These studies have suggested that people with ID and autism are at greater risk for psychopathology, and perhaps especially depression, than people with ID alone. However, the studies were limited by small sample sizes and failure to control for potential confounding variables. Therefore, the aims of the present study were first, to examine whether a variety of psychiatric disorders or depression alone are increased in people with ID and autism; second, to assess the possible contribution of other variables, such as gender, age, level of ID, psychotropic medication, that could account for any relationship between psychopathology between autism.
Method
Participants
There were 147 people with autism and ID and 605 people with ID and without autism between 16 and 84 years old (mean = 33.3, SD = 13.2), 60% were males and 40% females. They were referred for assessment to a Specialist Mental Heath Service of South-East London between 1983 and 2001 (Bouras, Cowley, Holt, Newton, & Sturmey, 2003) and represented 19.5% of the total referrals to the Service for that period. The largest proportion of referrals came from Primary Care (47.5%) followed by Generic Mental Health Services (37.4%) and Social Services (15.2%). The degree of ID was coded on ICD-criteria into mild (F70), moderate (F71) or severe (F72–73). The diagnosis of pervasive developmental disorder (F84, ICD-10) was made by a psychiatrist following clinical interviews with key informants and the patients as part of delivering clinical service. Two experienced psychiatrists agreed on the diagnosis by using ICD-10 clinical criteria. Historical details of early social and communication problems were obtained from past medical records. The same procedure was followed for the assessment of psychopathology. The eligibility criteria for the study were identical with the referral criteria, i.e., IQ below 70 and significant social impairment.
The service includes outpatient clinics, outreach work, inpatient assessment and treatment, and consultation with community agencies. The clinical team consists of psychiatrists, community psychiatric nurses and administrative staff, and has a regular interface with clinical psychologists and behavioural support practitioners. There are three phases in providing clinical services: assessment, intervention and follow-up. Therapeutic interventions are based on multidisciplinary work and include medication and environmental manipulation, as well as psychological treatments such as anxiety management and cognitive behaviour therapy.
Data Recording and Analysis
The data were recorded at initial assessment using a specially devised assessment and information rating profile and were then entered in a spreadsheet. The six variables that were recorded were age, gender, psychiatric diagnosis, epilepsy, degree of intellectual disability, and medication. Psychiatric diagnosis was coded to the following major ICD-10 categories: schizophrenia spectrum disorder (F20–27), personality disorder (F60–69), anxiety (F40–48), depressive disorder (F32–39), adjustment reaction (F43), and dementia (F00–03). The two patient groups were defined on the basis of the presence or absence of pervasive developmental disorder (F84). The data were analysed by chi-square tests to examine whether there were any statistically significant differences between the autistic and non-autistic group. Data were analysed using the Statistical Package for Social Sciences, 11th Version (SPSS 11).
Multi-variate Analyses
In order to control statistically for the contribution of potentially confounding demographic variables, while assessing each diagnostic category as an independent predictor of autism, a binary logistic regression was performed using a stepwise forward method. The variables were added successively according to their magnitude of the correlation with the dependent variable, and then were successively removed until the predictive ability of the regression model, indexed by the model chi-square, was not significantly improved.
Before the analysis, dummy variables were created where there were more than one category for each variable, coded as presence or absence. The presence of autism was the dependent measure. The parameters gender, age (≥35 or <35), ID level (severe/non-severe), medication (presence/absence), as well as the psychiatric categories, (schizophrenia spectrum disorder, personality disorder, anxiety, depressive disorder, adjustment reaction, and dementia), each coded as a binary variable, were entered in the equation as predictor variables.
PAS-ADD Sample
A subgroup of 224 participants, 55 of whom were diagnosed with autism spectrum disorders ID and 172 were diagnosed with ID only were also assessed with the Psychopathology Assessment Schedule for Adults with Developmental Disabilities Checklist (PAS-ADD Checklist). The PAS-ADD Checklist is a reliable measure of psychopathology for people with ID (Moss, Prosser, Costello, Simpson, & Patel, 1998). A key informant, such as a family or staff member completed the PAS-ADD Checklist for each individual. The assessing psychiatrist was blind to the PAS-ADD Checklist score at assessment, and the key informant was blind to the psychiatric diagnosis. The PAS-ADD Checklist has 29 items (scored from 0 to 2) tapping a range of psychiatric symptoms, and gives three total scores: Affective/Neurotic, Possible Organic and Psychotic Disorders.
Results
Table 1 presents the proportion of participants by gender, age, and level of ID for the two groups. People with autism and ID were younger than people with ID only (χ2 = 3.41, df = 5, P < .0001), and were more likely to have moderate or severe ID (χ2 = 33.44, df = 2, P < .0001). The gender differences between the two groups did not reach significance (χ2 = 3.41, df = 1, P = .06).
The proportion of psychiatric diagnosis and epilepsy is presented in Table 2. Psychiatric disorder were less frequent in the autistic group (χ2 = 20.07, df = 6, P < .001. There were no significant differences between the two groups in the rate of epilepsy (P > .30).
The proportion of people with autism and ID, and those with ID only, by type of medication is presented in Table 3. There were significant differences in the proportion of patients with autism who were in receipt of medication (χ2 = 21.44, df = 5, P < .001). Specifically, people with autism were more likely to take psychotropics (χ2 = 13.06, df = 1, P < .001) and less likely to take anti-convulsants (χ2 = 6.14, df = 1, P < .01).
Multi-variate Analyses
Table 4 summarises the logistic regression model for the absence or presence of autism. This model was significant (χ2 = 55.56, df = 5, P < .001, −2 log likelihood = 687.05) accounting for about 11% of the variance (R 2). The highest odds ratio was for ID level, with participants with severe ID being almost twice more likely to be autistic than participants with mild or moderate ID. The lowest odds ratio was for patients with personality disorders who were less than half as likely to be autistic as someone with any other psychiatric diagnosis. Male patients, and those who took medication, were also 1.6 times more likely to be autistic, as compared to female patients, and those without receiving medication. Finally, participants who were under 35 were more likely to be diagnosed as autistic than the older patients.
Analysis of PAS-ADD Sample
In an effort to validate the diagnoses of autism spectrum disorder the means of PAS-ADD Checklist on the following autism-related items were compared: item 6 (Repeated actions, such as checking over and over that a door has been locked, or having to do thinks in a particular order) and item 28 (Odd gestures and mannerisms). On item 6 the means (and SEs) were .46 (SE = 1.11) and 0.16 (SE = .04) which was a significant difference (t = 2.99, P < .01). On item 28 the means (and SEs) were .25 (SE = .06) and .13 (SE = .02) which was also a significant difference (t = 2.14, P < .01). Thus, the groups did differ in terms of autism-related symptoms.
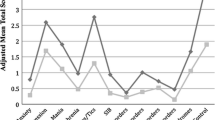
The groups were then compared in terms of scores on non-autistic psychopathology on the PAS-ADD Checklist. There were no differences on the three subscales scores (all Ps > .05). The numerical differences in the mean PAS-ADD scores between autistic (Affective/Neurotic = 4.62, Possible Organic = 1.90, Psychotic Disorders = 1.02) and non-autistic participants (Affective/Neurotic = 4.29, Possible Organic = 1.60, Psychotic Disorders = .87) were not statistically significant, all ts < 1. This result suggests an agreement between psychiatric diagnoses, made by the two clinicians, and psychopathology, as assessed by the PAS-ADD, which was completed by key informants.
Discussion
This study compared psychopathology as measured by psychiatric diagnosis and by the PAS-ADD Checklist in a large group of adults with ID and autism and people with ID alone. Both groups did indeed differ in the presence of autistic symptoms as measured by the PAS-ADD Checklist. However, both multivariate analysis of psychiatric disorders and univariate analyses of the PAS-ADD Checklist data revealed few differences between the groups. The multivariate analysis of psychiatric diagnosis demonstrated that, although the groups differed in that those with autism were younger, more likely to be male, more likely to be diagnosed with severe ID, more likely to take psychotropic medication, the only psychiatric diagnosis that distinguished between the groups was that people with autism spectrum disorders were less likely to be diagnosed with personality disorders. Thus, in contrast to some other research (Bradley et al., 2004; Morgan et al., 2003) we found little evidence of increased rates of psychopathology. We also replicated early findings that there was no increased risk of psychoses (Mouridsen et al., 1999; Volkmar & Cohen, 1991) in people with autism and ID. The male-to-female ratio was found to be elevated in the autistic group in accord with most previous studies showing a male predominance in autism (for a review see Baron-Cohen, 2003).
The failure to find differences in psychopathology between these two groups requires some comment. This study took place in a naturalistic clinical environment, and the sample size was quite large, if not larger than most previous studies, including also standardised methods of data collection using the PAS-ADD checklist. Thus, simple lack of power is a possible explanation, but not a likely one. One methodological explanation is that in this study we used multivariate analyses that controlled for possible confounds between the groups. Hence, it is possible that in some previous studies the observed differences between people with autism and people with ID only were due to other uncontrolled variables. Another methodological explanation for the absence of differences might be that the measures used in this study were insensitive to differences between the groups. The PAS-ADD did indeed detect differences between the groups in autism symptoms. However, it may be the case that the PAS-ADD scales are too short and hence insensitive to detect more subtle differences between the groups.
Morgan et al. (2003) collected their data retrospectively, by reviewing case notes over a period of time. We collected data at one point in time as part of delivering clinical service. Hence, the figures reported by Morgan et al. may be closer to period prevalences of psychopathology, and hence may have been more sensitive measures of psychopathology. Our data were collected at one point in time, and hence may be closer to point prevalence measures and hence be less sensitive measures of differences between the groups. Another possibility is that because nearly 70% of people with autism spectrum disorders were taking psychotropic medication that any psychopathology was well controlled. Alternatively, there may be measures of other aspects of psychopathology, such as social behaviour and language functioning, and challenging behaviours, that might detect differences between people with and without autism.
Psychotropic medication was found to be more frequent in the autistic group, a result that concurs with past evidence (Posey & McDougle, 2000), despite the fact that psychiatric disorders were less frequent in this group. It is possible that the elevated medication levels in people with ID and autism may reflect an effort to reduce autism-related behaviours, such as stereotypy and aggression. This result may also reflect pressures to prescribe medication in cases of greater complexity, despite the absence of overt clinical psychopathology.
Unlike Morgan et al. we found no increased rates of depression in people with autism spectrum disorders. The sample employed the Morgan et al. consisted predominantly (57%) of patients with severe disability, although the present sample consisted mainly (85%) of patients with mild and moderate disability. It could be suggested, for example, that increased levels of depression might be limited to people with severe ID. However, analysis of the present data showed that no case with severe ID and autism received a diagnosis of depression (0.0%), although some depression rates were observed in moderate (4.1%) and mild ID (11.1%). In people with ID but no autism spectrum disorder a similar pattern was observed in terms of the depression rates as a function of the ID level. The proportion of people with depression was severe (0.0%) moderate (5.8%) and mild ID (11.1%). Hence, these differences between Morgan et al. and the present study are unlikely to account for the reported differences. People with autism were more likely to have severe ID than their non-autistic counterparts. This may reflect an over-diagnosis of autism in low functioning individuals due to assessment difficulties. Another possibility would be that the developmental co-existence of autism with ID is likely to have a gradually detrimental effect on cognitive functioning, increasing the likelihood of severe ID. Consequently, further research is needed to elucidate the relationship between autism and levels of ID.
Our sample contained mostly adolescents and young adults, but did contain approximately 20% of adults aged over 35 years. Our multiple regression model identified age as the variable that best predicted autism (See also Table 1). Other research has reported trends to diagnosing autism spectrum disorders in children and adolescents more frequently than in adults (Fombonee, 1999; Sturmey & James, 2001.) There is evidence that certain autism-related behaviours are more likely to improve in older patients, as compared to younger patients (Seltzer et al., 2003). Age differences may partly reflect a particular neuro-developmental pattern in autism. Brain development in autism follows an abnormal pattern, with accelerated growth in early life (resulting in brain enlargement) and subsequent decrease in brain volume in later life, as a part of a maturation/normalisation process (Aylward, Minshew, Field, Sparks, & Singh, 2002). Consequently, such a neuro-developmental process could account for the fact that autism was found to be more frequent in younger (<35) than in older patients. The cumulative effects of education and environmental opportunity to learn alternative non-pathological behaviours over the lifespan may also be an important variable influencing the course of development in adults with autism.
The rates of epilepsy were roughly equivalent between the autistic and non-autistic group, despite the well-known association between autism and seizure disorders (e.g., Gillberg, 1991; Giovanardi-Rossi, Posar, & Parmeggiani, 2000; Volkmar & Nelson, 1990). There seems to be a bimodal age distribution of seizures in autism, as one peak occurs in infancy and the other in adolescence (Volkmar & Nelson, 1990). Therefore, the present results probably reflect the age range of the sample, as the majority was older than 25 years. In addition, considering that the majority of the present sample consisted of cases with mild and moderate ID, it is possible that the association between epilepsy and autism may exist mainly for cases with severe ID.
Given that in many cases previous diagnoses were available from past medical records, it could be argued that such information would bias the assessing clinicians towards confirming previous diagnoses. Such a possible bias would be particularly likely for older cases, due to a likelihood of historic misinterpretation of autistic symptoms as evidence of ‘‘schizophrenia spectrum’’ or ‘‘personality disorder.’’ However, the experience of two of the co-authors (NB & GH), who were also assessing clinicians for the present sample, was somehow different. All the cases were refereed from Primary Care, Social Services, and Mainstream Mental Health Services to a Specialist Service. The assessing clinicians, specialists in ID and autism, sometimes reconsidered an old diagnosis of ‘‘schizophrenia spectrum’’ or ‘‘personality disorder’’ to have been in fact a misdiagnosis of autism.
One potential limitation of the study is that both psychiatric diagnosis and autism was assessed by clinical interviews. The diagnosis of autism during concurrent clinical assessment, despite being more reliable than retrospective assessment, may have overshadowed other psychiatric diagnoses. Taking into account communication problems in autism (Howlin, 1997), coupled with the present finding that personality disorder was found less likely in the autistic group, the possibility of such an under-diagnosis might constitute a challenge for future investigations to overcome. Furthermore, the present study investigated only one subgroup of the autistic spectrum (low functioning group), and therefore the findings might not apply to those with normal intelligence. High self-awareness of autism-related social problems and limitations may be an important contributing factor to mental health in people with autism and normal intelligence.
In summary, the present results seem to cast doubts on the suggestion that people with ID and autism may have an increased risk for psychiatric disorders. However, although people with autism may not fulfill the conventional ICD-10 criteria, they still may suffer from psychiatric symptoms and maladaptive behaviours. Firm conclusions on the relationship between low-functioning autism and psychiatric co-morbidity may be premature in light of the diagnostic difficulties, inherent methodological problems, and possible overlap between autistic behaviours and those relating to other disorders. In this respect, diagnostic tools designed to address the specific needs of people with autism could contribute substantially. In terms of mental health policy planning, a stronger evidence base is needed prior to committing resources for clinical services.
References
American Psychiatric Association. (1994). Diagnostic and statistical manual of mental disorders, 4th edn. Washington: author.
Aylward, E. H., Minshew, N. J., Field, K., Sparks, B. F., & Singh, N. (2002). Effects of age on brain volume and head circumference in autism. Neurology, 59, 175–183.
Baron-Cohen, S. (2003). The essential difference: The truth about the male and female brain. New York: Basic Books.
Bolton, P. F., Pickles, A., Murphy, M., & Rutter, M. (1998). Autism, affective and other psychiatric disorders: Patterns of familial aggregation. Psychological Medicine, 28, 385–395.
Bouras, N., Cowley, A., Holt, G., Newton, J. T., & Sturmey, P. (2003). Referral trends of people with intellectual disabilities and psychiatric disorders. Journal of Intellectual Disability Research, 47, 439–446.
Bradley, E. A., Summers, J. A., Wood, H. L., & Bryson, S. E. (2004). Comparing rates of psychiatric and behaviour disorders in adolescents with young adults with severe intellectual disability with and without autism. Journal of Autism & Developmental Disorders, 34, 151–161.
Clarke, D. J., LittleJohns, C. S., Corbett, J. A., & Joseph, S. (1989). Pervasive developmental disorders and psychoses in adult life. British Journal of Psychiatry, 155, 692–699.
Deb, S., Mathews, T., Holt, G., & Bouras, N. (2001). Practice guidelines for the assessment and diagnosis of mental health problems in adults with intellectual disability. UK: Pavillion.
Deb, S., Thomas, M., & Bright, C. (2001). Mental disorder in adults with intellectual disability, 1: Prevalence of functional psychiatric illness among a community-based population aged between 16 and 64 years. Journal of Intellectual Disability Research, 45, 495–505.
Eisenberg, L., & Kanner, L. (1958). Early infantile autism, 1943–1955. In: C. F. Reed, I. E. Alexander, & S. S. Tomkins (Eds.), Psychopathology: A source book (pp. 3–14). Cambridge, MA: Harvard University Press.
Fombonne, E. (1999). The epidemiology of autism: A review. Psychological Medicine, 29, 769–786.
Fombonne, E., Mazaubrun, C., Cans, C., & Grandjean, H. (1997). Autism and associated medical disorders in a French epidemiological survey. Journal of the American Academy of Child & Adolescent Psychiatry, 36, 1561–1569.
Ghaziuddin, M., Ghaziuddin, N., & Greden, J. (2002). Depression in persons with autism: Implications for research and clinical care. Journal of Autism & Developmental Disorders, 32, 299–306.
Giovanardi-Rossi, P., Posar, A., & Parmeggiani, A. (2000). Epilepsy in adolescents and young adults with autistic disorder. Brain Development, 22, 102–106.
Gillberg, C. (1991). The treatment of epilepsy in autism. Journal of Autism and Developmental Disorders, 21, 61–77.
Gillberg, C. (1999). Autism and its spectrum disorders. In: N Bouras (Ed.), Psychiatric and behavioural disorders in developmental disabilities and mental retardation (pp. 73–95). New York: Cambridge University Press.
Gillberg, C., & Billstedt, E. (2000). Autism and Asperger syndrome: Co-existence with other clinical disorders. Acta Psychiatrica Scandinavica, 102, 321–330.
Howlin, P. (2000). Outcome in adult life for more able individuals with autism or Asperger syndrome. Autism, 4, 63–83.
Howlin, P. (1997). Autism: Preparation for adulthood. London: Routledge.
Lainhart, J. E. (1999). Psychiatric disorders, executive function and the broader autism phenotype in parents of autistic probands. Molecular Psychiatry, 4, 303.
Morgan, C. N., Roy, M., & Chance, P. (2003). Psychiatric comorbidity and medication use in autism: A community survey. Psychiatric Bulletin, 27, 378–381.
Moss, S., Prosser, H., Costello, H., Simpson, N., & Patel, P. (1998). Reliability and validity of the PAS-ADD Checklist for detecting psychiatric disorders in adults with intellectual disability. Journal of Intellectual Disability Research, 42, 173–183.
Mouridsen, S. E., Rich, B., & Isager, T. (1999). Psychiatric morbidity in disintegrative psychosis and infantile autism: A long-term follow-up study. Psychopathology, 32, 177–183.
Petty, L. K., Ornitz, E. M., Michelman, J. D., & Zimmerman, E. G., (1984). Autistic children who become schizophrenic. Archives of General Psychiatry, 41, 129–135.
Piven, J., & Palmer, P. (1999). Psychiatric disorders and the broad autism phenotype: Evidence from a family study of multiple incidence autism families. American Journal of Psychiatry, 156, 557–563.
Posey, D. J., & McDougle, C. J. (2000). The pharmacotherapy of target symptoms associated with autistic disorder and other pervasive developmental disorders. Harvard Review of Psychiatry, 8, 45–63.
Seltzer, M. M., Krauss, M. W., Shattuck, P. T., Orsmond, G., Swe, A., & Lord, C. (2003). The symptoms of autism spectrum disorders in adolescence and adulthood. Journal of Autism and Developmental Disorders, 33, 565–581.
Sturmey, P., & James, V. (2001). Letter to the Editor. The administrative prevalence of autism in the Texas school system. Journal of the American Academy of Child and Adolescent Psychiatry, 40, 621–622.
Volkmar, F. R., & Cohen, D. J. (1991). Comorbid association of autism and schizophrenia. American Journal of Psychiatry, 148, 1705–1707.
Volkmar, F. R., & Nelson, D. S. (1990). Seizure disorders in autism. Journal of American Academy of Child and Adolescent Psychiatry, 29, 127–129.
World Health Organization (1992). The ICD-10 classification of mental and behavioural disorders – clinical descriptions and diagnostic guidelines. Geneva: author.
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Tsakanikos, E., Costello, H., Holt, G. et al. Psychopathology in Adults with Autism and Intellectual Disability. J Autism Dev Disord 36, 1123–1129 (2006). https://doi.org/10.1007/s10803-006-0149-3
Published:
Issue Date:
DOI: https://doi.org/10.1007/s10803-006-0149-3