Abstract
Effortful control, the ability to regulate complex and goal-directed behavior, may protect individuals from developing mental health symptoms. This study tested the potential for child effortful control and executive functioning to buffer the effects of familial liability for attention deficit hyperactivity disorder (ADHD) problems across a one-year timeframe. Data from the prospectively-collected Adolescent Brain Cognitive Development (ABCD)® study were used to examine whether caregiver-rated child effortful control and executive functioning moderated the association between familial ADHD risk and later ADHD symptoms in a sample of children (N = 6,133; ages 9–10 years at baseline). Two independent variables were considered to compare the predictive powers of specific (family ADHD) and broad (family psychopathology) risk factors. Two additional moderating variables (surgency, negative affect) were tested to examine specificity of effortful control and executive functioning as moderators. All variables of interest were measured on a continuum and via caregiver report. At high levels of effortful control and executive functioning, there was no association between familial liability for ADHD or broad psychopathology and later child ADHD problems. The moderator effects were specific to effortful control and executive functioning domains. Etiological models of heritable psychiatric disorders, such as ADHD, should consider the risk and protective contributions of individual traits, such as effortful control and executive functioning. Clinical prevention and intervention efforts may target self-regulation skills in children to buffer against familial liability for ADHD problems.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Effortful control describes an individual’s temperamental predisposition to inhibit a dominant response and perform a less salient behavior (Eisenberg, 2017). Together with two other temperamental dimensions—negative affect and surgency—effortful control facilitates adaptive self-regulation (Diamond, 2013; Rothbart & Bates, 2006). Negative affect refers to the tendency to experience negative emotions, such as frustration or fear; surgency is interpreted as high levels of activity, pleasure-seeking, and impulsivity (Rothbart, 2007). Ontogenetically, effortful control is a precursor to closely related constructs, such as cognitive control and executive functioning (Nigg, 2017). At the neurobiological level, the frontal-cingulate-parietal-insular network appears to support these “top-down” regulatory processes (McTeague et al., 2016). Developmental psychology and psychiatry have a long-standing interest in effortful control (and related constructs) and are increasingly conceptualizing regulatory behaviors as protective factors against atypical development. The frontoparietal control system has been likened to the “immune system of the mind” in that it regulates mental health symptoms (Cole et al., 2014). More specifically, intact executive functioning skills are believed to protect at-risk populations from developing aberrant brain systems and subsequent diagnoses of neurodevelopmental disorders (Johnson, 2012).
Attention deficit/hyperactivity disorder (ADHD) is one of the most prevalent neurodevelopmental disorders, affecting roughly 5–7% of the school-aged population (American Psychological Association, 2013). ADHD is a highly heterogenous disorder with a complex and multifactorial etiology (Nigg et al., 2020); executive functioning deficits have been described as one of several central factors in the behavioral expression of inattention, hyperactivity, and impulsivity. For Barkley’s self-regulation model of ADHD suggests that impaired executive functioning and behavioral self-regulation underlie core symptoms of ADHD (Barkley, 1997, 2015). Disruptions in attention regulation, for example, may manifest as difficulties sustaining attention on cognitively-demanding or less-preferred tasks. Similarly, difficulties with behavioral self-regulation may be reflected in increased activity levels (e.g., fidgeting with hands; acting as if driven by a motor). Given that no single executive functioning skill (e.g., working memory, inhibitory control) has been consistently linked to ADHD symptoms (Arnett et al., 2022; Pennington, 2006), investigations of executive functioning correlates of ADHD must incorporate a range of cognitive-behavioral constructs.
Longitudinal research suggests that greater effortful control in toddlerhood is associated with fewer parent- and teacher-reported ADHD symptoms during school age (Joseph et al., 2021). From a developmental psychopathology perspective, pathways toward psychopathology are best understood through the joint consideration of multiple interacting risk and protective factors across time (Cicchetti, 1984). The present study considers the potential interaction of two variables that have featured prominently in etiological models of ADHD: effortful control and familial ADHD risk. We test the idea that parent-reported effortful control (and the closely related construct executive functioning) operates as the mind’s “immune system” and buffers against familial liability for ADHD.
Behavioral genetics models have highlighted the heritability of ADHD. The relative risk of ADHD among children born of parents with ADHD ranges from 6.2 to 11.7, with 20–40% of offspring meeting criteria for an ADHD diagnosis (Solberg et al., 2021). An estimated 30–40% of individual differences in adult ADHD symptoms can be accounted for by genetic factors (Boomsma et al., 2010; van den Berg et al., 2006). Interestingly, while childhood ADHD typically presents with a combination of inattentive and hyperactive/impulsive symptoms, the adult ADHD phenotype is largely characterized by inattentive behaviors, suggesting these are “core” features of ADHD across development (Martel et al., 2012, 2016). In this study, we use self-reported, behaviorally-measured caregiver ADHD symptoms as an index of familial liability for ADHD problems in children.
Environmental stress has been suggested to disrupt the development of neural systems associated with executive functioning, thereby leading to heightened risk for psychopathology (McLaughlin, 2016). We therefore include socioeconomic status as a control variable in all models to account for the potential influence of such environmental factors. Given that hierarchical models of psychopathology are receiving increasing attention and empirical support (Caspi et al., 2014), we additionally consider the predictive role of broad familial psychopathology factor (referred to as “p risk” hereafter).
This study aimed to examine the potential for child effortful control and executive functioning to buffer the effects of familial liability for ADHD problems across a one-year timeframe. Informed by prior research, we predicted that two measures of self-regulation (i.e., effortful control, executive functioning), would moderate the association between familial ADHD liability and child ADHD symptoms (Hypothesis 1a, b). We also predicted that the model for ADHD risk would better fit the data compared to the model for p risk (Hypothesis 2). Lastly, we expected the moderation effects identified in Hypothesis 1 to be specific to effortful control and executive functioning. By contrast, we did not expect significant moderation by two temperament constructs that are also related to self-regulation, surgency and negative affect (Hypothesis 3). While many children with ADHD struggle in social and emotional domains, these symptoms are not core diagnostic features.
Methods
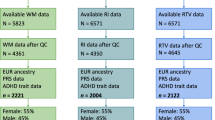
Study Design. Our hypotheses were tested using data from the Adolescent Brain Cognitive Development (ABCD)® study, a longitudinal and multi-site study conducted in the United States (Garavan et al., 2018). At baseline, a large cohort (N = 11,875) of 9- and 10-year-old children was recruited at 21 sites across the United States (2016–2018). Participating children and families have been completing comprehensive yearly laboratory assessments. Detailed information on study design and recruitment have been described elsewhere (Garavan et al., 2018). Results presented in this paper are based on data collected at year 2 (referred to as “T1” hereafter) and year 3 (referred to as “T2” hereafter; data version 4.0, released September 2021).
Participants. The final sample for this study consisted of children who completed measures at T1 and T2 (n = 6,133). At T1 the mean age for children was 11.98 years (SD = 7.8 months). Fifty-three percent of the sample were assigned male sex at birth. Regarding socioeconomic status (SES), self-reported total combined family income for the last few months at T1 included: 2% less than $5,000 (Group 1); 2.5% $5,000–11,999 (Group 2); 1.7% $12,000–15,999 (Group 3); 3.4% $16,000–24,999 (Group 4); 4.8% $25,000–34,999 (Group 5); 6.9% $35,000–49,999 (Group 6); 13.3% $50,000–74,999 (Group 7); 14.7% $75,000–99,999 (Group 8); 35% $100,000-199,999 (Group 9); 15% $200,000 or more (Group 10); 470 participants did not provide information on SES and are not included in these percentages). Study design and recruitment efforts (Garavan et al., 2018) resulted in a study sample that is generally viewed to be representative of the general US population (for a review, please see Compton et al., 2019).
Measures. Demographic variables. Demographic information was collected at T1. The child’s age (in months), sex assigned at birth, and race were reported by the primary caregiver. Total combined family income for the past 12 months was used as a proxy for socioeconomic status. This latter variable was measured on a 10-point ordinal scale ranging from “less than $5,000” to “$200,000 and greater.” Demographic information was used to describe the sample and as covariates in main analyses.
Familial liability. Family liability for ADHD and p risk were calculated using caregiver questionnaires at T1. The participating caregiver completed the self-report Achenbach Adult Self Report Questionnaire (ASR) to assess their own adaptive functioning and problem behaviors (Achenbach & Rescorla, 2003). The participating caregiver also completed the Adult Behavior Checklist (ABCL) about the other parent (when applicable, n = 5325), which provided dimensional measures of adaptive functioning and psychopathology (Achenbach & Rescorla, 2003). Family ADHD risk was calculated as the mean of ABCL inattention and ASR inattention scales. P risk was calculated as the mean of ABCL total and ASR total T scores. Higher scores indicated greater levels of parental symptomatology.
Effortful control. The caregiver completed the Early Adolescent Temperament Questionnaire (EATQ-R; Capaldi & Rothbart, 1992) at T1 to assess child effortful control. Respondents are asked to rate their child’s behavior using a 5-point Likert scale, ranging from almost always untrue of your child to almost always true of your child. The effortful control factor consists of three subscales: attention, inhibitory control, and activation control. Sample items include “finds it easy to really concentrate on a problem” (attention), “is usually able to stick with his/her plans and goals” (inhibitory control), and “usually finishes her/his homework before it is due” (activation control). Higher scores reflected greater effortful control. Two additional EATQ-R factors were considered in the present study: surgency and negative affect. Surgency includes frustration, fear (reverse scored), and shyness (reverse scored); negative affect includes frustration, depressive mood, and aggression subscales. Cronbach alpha values for the present study were 0.88 for effortful control, 0.79 for surgency, and 0.87 for negative affect.
Executive functioning. The short form of the Barkley Deficits in Executive Functioning Scale – Children and Adolescents (BDEFS-CA; Barkley, 2012) was used to evaluate executive functioning dimensions of daily life (e.g., time management, organization, self-regulation). At T2, caregivers rated their child’s behavior on a 4-point Likert scale, ranging from never or rarely to very often. Sample items include “doesn’t seem to process information quickly or accurately” and “has a poor sense of time.” In order to be consistent with the other moderating variable of interest (effortful control), the BDEFS-CA was reverse coded such that higher values reflected stronger executive functioning skills. For this sample, the Cronbach alpha for the BDEFS-CA was 0.93.
Child ADHD problems. Caregivers completed the Child Behavior Checklist (CBCL; age 6–18; Achenbach & Edelbrock, 1991) at T2, a normed and validated broad-band measure of problem behaviors and adaptive functioning. Parents indicated the degree to which certain behaviors applied to their child using a 3-point scale (0 = not true; 1 = somewhat or sometimes true; 2 = very true or often true). The DSM-ADHD subscale was used as a continuous measure of child ADHD problems. Higher T scores were indicative of greater ADHD symptoms. Strong psychometric properties have been suggested for the CBCL and prior research suggests that CBCL subscales can accurately differentiate children with and without ADHD (Achenbach & Edelbrock, 1991; Chen et al., 1994).
Data Analysis. Statistical analyses were executed in R Studio with child ADHD symptoms as the outcome variable. Descriptive statistics were computed to characterize the sample and evaluate normality of study variables. Bivariate correlations were initially computed for the main study variables. To test Hypothesis 1 (i.e., the moderating effects of effortful control and executive functioning on ADHD risk), linear regression models were run with socioeconomic status, ADHD risk, effortful control or executive functioning, and the interaction between ADHD risk and effortful control or executive functioning as predictors for child ADHD problems. To compare the predictive validity of ADHD risk versus p risk (Hypothesis 2), we ran a second set of linear regressions in which p risk was modeled as the predictor rather than ADHD risk. Finally, to test specificity of effortful control and executive functioning as moderators (Hypothesis 3), we examined whether surgency and negative affect moderated the association between familial ADHD liability and child ADHD symptoms.
Results
Descriptive Statistics. Basic descriptive statistics and bivariate correlations are presented in Table 1. Main study variables were normally distributed (i.e., <|3| skew, <|5| kurtosis). Age was not significantly correlated with any of the main study variables and was therefore not included in subsequent analyses. Correlations for the main study variables mostly fell in the expected directions (Table 1). The two familial risk factors, ADHD risk and p risk, had a strong positive correlation, r(5,299) = 0.78, p < 0.001. Effortful control and executive functioning (i.e., reverse-coded BDEFS-CA scores) also had a strong positive correlation r(5,976) = 0.65, p < 0.001. Child ADHD symptoms were negatively correlated with effortful control, r(6,061)=-0.56, p < 0.001. Unexpectedly, child ADHD symptoms and surgency were also negatively correlated, though the effect size was small, r(6,061)=-0.05, p < 0.001.
There was a significant effect of socioeconomic status on child ADHD symptoms, F(9, 5653) = 3.20, p < 0.001). Tukey’s HSD test for multiple comparisons suggested that the mean severity of ADHD symptoms was significantly higher in group 7 as compared to groups 9 (p < 0.05, 95% C.I.=[-1.53, -0.09]) and10 (p < 0.01, 95% C.I.=[-1.91, -0.23]). SES was therefore included as a covariate in all subsequent models.
Hypothesis 1
Effortful control and executive functioning will moderate the association between ADHD risk and child ADHD symptoms.
Results from a linear regression model with sex, SES, and the interaction between familial ADHD risk and effortful control supported our a priori prediction (Hypothesis 1a). As reported in Table 2 (see Model 1), the interaction between familial ADHD risk and effortful control was statistically significant, B=-0.18, p < 0.001. Similar results emerged when executive functioning was modeled as the moderator (Hypothesis 1b; see Model 2 in Table 2).
To better understand the interaction term in Model 1, we plotted simple slopes for low, medium, and high values of effortful control, defined as -1, 0, and + 1 standard deviations relative to the mean, respectively (Fig. 1a) and tested for their significance. Starting with average levels of effortful control, familial ADHD risk positively and significantly predicted child ADHD symptoms, b = 0.10, p < 0.001. The magnitude of this association was stronger for children with low effortful control, b = 0.21, p < 0.001. In contrast, for high levels of effortful control, familial ADHD risk did not predict child ADHD symptoms (b=-0.01, p = 0.58). Similar trends were found for executive functioning (Model 2). As is shown in Fig. 1b, at average levels of executive functioning, the association between ADHD risk and child ADHD symptoms was positive and significantly different from zero (b = 0.05, p < 0.01). At low levels of executive functioning, the magnitude of this association was stronger and also statistically different from zero (b = 0.13, p < 0.001). By contrast, at high levels of executive functioning, the slope was negative and not statistically different from zero (b=-0.03, p = 0.14). Altogether, this indicates that familial risk for ADHD is negated at high levels of effortful control and/or executive functioning.
The region of significance for effortful control and executive functioning was established using the Johnson-Neyman technique. As depicted in Fig. 2a and b, effortful control scores above 3.82 and executive functioning scores above 3.53 protect against ADHD risk.
Hypothesis 2
Familial ADHD risk will better predict child ADHD symptoms compared to familial p risk.
Contrary to Hypothesis 2, model estimates for ADHD risk and p risk were comparable (see Models 1 & 3 in Table 2). Specifically, estimates for interaction terms (-0.18 and − 0.13 for ADHD risk and p risk, respectively) as well as overall model fit (R square = 0.34 for both models) were similar.
Hypothesis 3
Surgency and negative affect will not moderate the association between familial ADHD risk and child ADHD symptoms (specificity of model).
To evaluate the specificity of effortful control and executive functioning as moderators of familial liability for ADHD symptoms (Hypothesis 3), we ran two additional linear regression models with surgency and negative affect as alternative moderators. Although we had predicted that the moderating effect would be unique to effortful control, the interaction between ADHD risk and surgency was statistically significant, B=-0.05, p < 0.05. To better understand the interaction term for surgency, we plotted simple slopes for low, medium, and high values of surgency (see Fig. 1c). Unlike with effortful control, the effect of surgency on the association between ADHD risk and child ADHD symptoms was positive at low (b = 0.28, p < 0.001), medium (b = 0.31, p < 0.001), and high (b = 0.33, p < 0.001) levels of surgency. This indicates that while low levels of surgency attenuated the effect of ADHD risk on ADHD outcomes, it did not fully neutralize the association. Moreover, comparison of R square values for the surgency and effortful control models suggested a better model fit for effortful control (surgency R2 = 0.08, versus effortful control R2 = 0.35). Negative affect did not significantly moderate the association between ADHD risk and child ADHD symptoms, B=-0.04, p = 0.10.
Discussion
Effortful control and closely-related constructs, such as cognitive control and executive functioning, play an ubiquitous (“transdiagnostic”) role across mental health disorders (Johnson, 2012; Zelazo, 2020). On the “flip side of the coin,” within at-risk populations, individuals with strong executive function skills are “better able to compensate for atypicalities in other brain systems early in life,” thereby protecting them from developing high levels of psychopathology (Johnson, 2012). We used data from the ABCD study® to test the potential buffering effect of effortful control and executive functioning against familial liability for ADHD problems in a large and representative sample of children.
As predicted, not only were low effortful control and executive functioning prospectively associated with higher child ADHD problems, but variation in these domains moderated the effect size of familial liability for ADHD. More specifically, plotting and probing of simple slopes revealed that the association between familial ADHD risk and child self-regulation abilities was the strongest at low levels of self-regulation. Whereas the association between mean levels of effortful control/executive functioning and child ADHD problems was still positive and significant, this was not the case for greater regulatory capacity. Stated differently, individuals with well-developed self-regulation skills appeared to be protected against the impacts of parental ADHD symptoms. Interestingly (and contrary to our predictions), models for ADHD specific family risk and broad psychopathology risk had comparable estimates. These findings are consistent with prior studies linking polygenic risk for ADHD with general psychopathology in children (Brikell et al., 2020; Waszczuk et al., 2021), and provide additional support for the validity and utility of a broad p factor in developmental psychology and psychiatry research (Caspi et al., 2014).
These findings integrate well within the existing body of research. In their recent analysis of ABCD study data, Cordova and colleagues (2022) found that children in the top decile of polygenic load had a 63% increased chance of having ADHD compared to the bottom half of the polygenic load. Our results align with those reported by Cordova in that they highlight the considerable contribution made by familial factors in the emergence of ADHD symptoms. Our results help account for some of the unexplained variability by highlighting the additional role of self-regulation skills in accounting for ADHD problems. The utility of considering multiple interacting risk and protective factors across time has been suggested by Cicchetti’s developmental psychopathology framework (Cicchetti, 1984). It is, of course, important to acknowledge that our sample included children with and without a clinical diagnosis of ADHD;our dependent variable was measured on a continuum to capture the full range of possible symptoms. Of note, the CBCL considers 6 of the possible 18 symptoms; neither age of onset nor functional impairment were considered.
Our results also align with those recently described by Romer and Pizzagalli (2021). These authors likewise used ABCD study data to examine whether executive dysfunction is a cause or consequence of general psychopathology. Using residualized-change models with data from baseline and 2-year follow-up, Romer and Pizzagalli found that executive functioning prospectively predicted p factor scores, accounting for baseline psychopathology, sex, age, race/ethnicity, parent education, and family income. We found that individual differences in self-regulation skills prospectively predicted child ADHD problems. Taken together, our results as well as those reported by Romer and Pizzagalli corroborate Barkley’s inhibition model of ADHD, which posits a central role of behavioral inhibition and attention system in the emergence of ADHD symptoms (Barkley, 1997).
Regarding specificity of the effortful control model, we found partial support for our prediction. Whereas negative affect did not moderate the association between familial ADHD risk and ADHD problems, surgency emerged as a significant moderator. However, further investigation revealed that surgency constitutes only a risk, rather than a protective, factor. Our results align with those reported by Martel who used latent class profile analysis to divide young children with ADHD into subgroups based on temperamental profile (Martel, 2016). Martel reports that children with ADHD and high surgency not only showed deficits in core executive functioning skills (such working memory), but were also at elevated risk for comorbid psychiatric symptoms when compared to children in two other temperamental subgroups (Martel, 2016).
Our findings add to a growing literature suggesting that effortful control may be a developmental precursor to ADHD symptoms (Nigg et al., 2004). The diagnosis of ADHD is made on the basis of behavioral symptoms, many of which are developmentally appropriate in early childhood, thus impeding accurate diagnosis prior to school age (Americal Psychiatric Association, 2013). In contrast, effortful control can be measured early in development and appears to lay the foundation for more advanced self-regulation skills, including executive functioning (Diamond, 2013). Thus, effortful control may be a key component to precision medicine care for children at-risk for ADHD and represents a promising target for prevention and early intervention efforts. A growing body of literature supports the notion that executive functioning skills can be strengthened through targeted training (Diamond, 2013; Zelazo, 2020). Child self-regulation skills could also be improved through Parent Management Training (PMT; Helander et al., 2022). Consistent with Belsky’s model of differential susceptibility (Belsky, 1997), we could hypothesize from our results that treatments that strengthen effortful control and executive functioning early in life may have the potential to reduce, or eventually protect against, the development of ADHD symptoms. However, longitudinal studies starting in early childhood are needed to test this hypothesis.
Results should be interpreted in the context of this study’s limitations and strengths. Focusing first on limitations, it is important to acknowledge the conceptual similarities among effortful control, executive functioning, and ADHD symptoms, and the possibility that these constructs are overlapping in nature (please see Tiego et al., 2020 as an example of treating effortful control and executive functioning as a single self-regulation construct). Second, results are based on a community sample with low levels of ADHD symptoms in children. Additionally, data reported here were obtained through caregiver report, which may be biased, especially in the presence of parental psychopathology (Kroes et al., 2003). Although all study questionnaires were selected due to their strong psychometric properties (and were confirmed to have strong Cronbach alpha values in this sample), there is the potential for reporter bias and common method variance, which could have affected study results. It is also important to note that our measure of executive functioning was based on caregiver reports of the child’s everyday behaviors. Prior research has clearly demonstrated that these types of measures are not well correlated with laboratory-based measures of executive functioning (Toplak et al., 2013). It remains unclear to what extent our results extend to cognitive functions measured in the laboratory. Future research could include additional measurement of child self-regulation, such as the Lab TAB (Gagne et al., 2011) and the Delis-Kaplan Executive Function System (D-KEFS; Delis et al., 2001). Regarding the predictor variable—familial liability for ADHD—we relied on caregiver reported inattentive symptoms. Admittedly, adult inattention symptoms could result from a myriad of causes, including anxiety, insomnia, and trauma (American Psychiatric Association, 2013), suggesting that results should be interpreted with at least some caution.
Further, and in line with the developmental psychopathology framework (Cicchetti, 1984), etiological models for disorders of childhood need to consider the dynamic interplay between various risk and protective factors. ADHD is a highly heterogenous clinical diagnosis with a multifactorial etiology (Joel T. Nigg, Margaret H. Sibley, Anita Thapar, & Sarah L. Karalunas, 2020). Our models focused on familial liability and self-regulation (while accounting for sex and socioeconomic status); other potential contributory variables, such as cognitive ability, early life adversity, or parenting behaviors, were not considered in this investigation. In fact, Joseph and colleagues recently highlighted the importance of temperament and parenting as early predictors for ADHD (Joseph et al., 2021). Relatedly, our models did not elucidate the mechanism(s) by which genetic versus environmental familial risks interplay with self-regulation to contribute to ADHD symptoms and we were unable to account for baseline ADHD problems.
Strengths of this study include the large and representative sample, which allowed us to probe for small effects and draw conclusions about the general population of children in the US. Further, we measured individual traits and symptoms on a continuum (rather than using dichotomous diagnostic criteria), which aligns with the Research Domain Criteria (RDoC) framework (Mittal & Wakschlag, 2017). Additionally, although there are limitations to reliance on caregiver questionnaires, these measures are low cost and easy to administer, therefore increasing the potential feasibility of applying this knowledge to clinical settings.
Future work should address these shortcomings by considering additional variables as well as underlying mechanisms. Cole and colleagues (Cole et al., 2014), for example, called for research that expands what is known about the control system, including associated brain correlates. Our research group recently used electroencephalography (EEG) methods to examine cortical activity related to self-regulation. We found that cognitive control mediated the association between cortical activity and neurodevelopmental symptoms in a sample of 7–11 year-old children (Peisch & Arnett, 2022). Integrating neurobiological measures into moderation models represents a promising next step in this line of work. Future studies should also examine whether the buffering role of effortful control is unique to ADHD or whether (and to what degree) it applies to other clinical disorders (such as autism spectrum disorder and obsessive-compulsive disorder). Relatedly, analyses should be replicated in clinical samples—that is, in a sample of children with a clinical diagnosis of ADHD. Lastly, genetic liability for ADHD could be calculated through the use of polygenic risk scores—a promising new approach that reliably quantified genetic risk for ADHD (Ronald et al., 2021).
In conclusion, our results expand what is known about the interplay of familial liability for ADHD and child self-regulation across time in a large and representative sample of children. We add to the growing body of literature suggesting that two aspects of self-regulation—effortful control and executive functioning—may play a protective role for individuals at-risk for ADHD.
Data Availability
Data used in the preparation of this article were obtained from the ABCD Study (www.abcdstudy.org), held in the National Institute of Mental Health Data Archive (NDA). The ABCD data used in this report came from NDA DOI https://doi.org/10.15154/1524795. ABCD consortium investigators designed and implemented the study and/or provided data but did not participate in the analysis or writing of this report.
References
Achenbach, T. M., & Edelbrock, C. (1991). Child behavior checklist. Burlington (Vt), 7, 371–392.
Achenbach, T. M., & Rescorla, L. A. (2003). Manual for the ASEBA Adult Forms & Profiles. University of Vermont, Research Center for Children, Youth, & Families.
American Psychiatric Association. (2013). Diagnostic and statistical manual of mental disorders (DSM-5®). American Psychiatric Pub.
Arnett, A., McGrath, L., Flaherty, B., Pennington, B., & Willcutt, E. (2022). Heritability and clinical characteristics of neuropsychological Profiles in Youth with and without elevated ADHD symptoms. Journal of Attention Disorders.
Barkley, R. A. (1997). Behavioral inhibition, sustained attention, and executive functions: Constructing a unifying theory of ADHD. Psychological Bulletin, 121(1), 65.
Barkley, R. A. (2012). Barkley deficits in executive functioning scale–children and adolescents (BDEFS-CA). Guilford Publications.
Barkley, R. A. (2015). Executive functioning and self-regulation viewed as an extended phenotype. Implications of the theory for ADHD and its treatment.
Belsky, J. (1997). Variation in susceptibility to environmental influence: An evolutionary argument. Psychological Inquiry, 8(3), 182–186. https://doi.org/10.1207/s15327965pli0803_3
Boomsma, D. I., Saviouk, V., Hottenga, J. J., Distel, M. A., De Moor, M. H., Vink, J. M., & de Geus, E. J. (2010). Genetic epidemiology of attention deficit hyperactivity disorder (ADHD index) in adults. PLoS One, 5(5), e10621.
Brikell, I., Larsson, H., Lu, Y., Pettersson, E., Chen, Q., Kuja-Halkola, R., & Martin, J. (2020). The contribution of common genetic risk variants for ADHD to a general factor of childhood psychopathology. Molecular Psychiatry, 25(8), 1809–1821.
Capaldi, D. M., & Rothbart, M. K. (1992). Development and validation of an early adolescent temperament measure. The Journal of Early Adolescence, 12(2), 153–173. https://doi.org/10.1177/0272431692012002002
Caspi, A., Houts, R. M., Belsky, D. W., Goldman-Mellor, S. J., Harrington, H., Israel, S., & Poulton, R. (2014). The p factor: One general psychopathology factor in the structure of psychiatric disorders? Clinical Psychological Science, 2(2), 119–137.
Chen, W. J., Faraone, S. V., Biederman, J., & Tsuang, M. T. (1994). Diagnostic accuracy of the child behavior checklist scales for attention-deficit hyperactivity disorder: A receiver-operating characteristic analysis. Journal of Consulting and Clinical Psychology, 62(5), 1017.
Cicchetti, D. (1984). The emergence of developmental psychopathology. Child Development, 55(1), 1–7.
Cole, M. W., Repovš, G., & Anticevic, A. (2014). The frontoparietal control system: A central role in mental health. The Neuroscientist, 20(6), 652–664.
Compton, W. M., Dowling, G. J., & Garavan, H. (2019). Ensuring the best use of data: The adolescent brain Cognitive Development Study. JAMA Pediatr, 173(9), 809–810. https://doi.org/10.1001/jamapediatrics.2019.2081
Cordova, M. M., Antovich, D. M., Ryabinin, P., Neighbor, C., Mooney, M. A., Dieckmann, N. F., & Nigg, J. T. (2022). Attention-Deficit/Hyperactivity disorder: Restricted phenotypes prevalence, Comorbidity, and polygenic risk sensitivity in ABCD Baseline Cohort. Journal of the American Academy of Child & Adolescent Psychiatry. https://doi.org/10.1016/j.jaac.2022.03.030
Delis, D. C., Kaplan, E., & Kramer, J. H. (2001). Delis-Kaplan executive function system (D-KEFS). APA PsycTests.
Diamond, A. (2013). Executive functions. Annual Review of Psychology, 64, 135–168.
Eisenberg, N. (2017). Commentary: What’s in a word (or words)–on the relations among self-regulation, self‐control, executive functioning, effortful control, cognitive control, impulsivity, risk‐taking, and inhibition for developmental psychopathology–reflections on Nigg (2017). Journal of Child Psychology and Psychiatry, 58(4), 384–386.
Gagne, J. R., Van Hulle, C. A., Aksan, N., Essex, M. J., & Goldsmith, H. H. (2011). Deriving childhood temperament measures from emotion-eliciting behavioral episodes: Scale construction and initial validation. Psychological Assessment, 23(2), 337–353. https://doi.org/10.1037/a0021746
Garavan, H., Bartsch, H., Conway, K., Decastro, A., Goldstein, R., Heeringa, S., & Zahs, D. (2018). Recruiting the ABCD sample: Design considerations and procedures. Developmental Cognitive Neuroscience, 32, 16–22.
Helander, M., Enebrink, P., Hellner, C., & Ahlen, J. (2022). Parent management training combined with group-CBT compared to parent management training only for oppositional defiant disorder symptoms: 2-year follow-up of a randomized controlled trial. Child Psychiatry & Human Development, 1–15.
Johnson, M. H. (2012). Executive function and developmental disorders: The flip side of the coin. Trends in Cognitive Sciences, 16(9), 454–457.
Joseph, H. M., McKone, K. M., Molina, B. S., & Shaw, D. S. (2021). Maternal parenting and toddler temperament: Predictors of Early School Age Attention-Deficit/Hyperactivity disorder-related behaviors. Research on Child and Adolescent Psychopathology, 49(6), 763–773.
Kroes, G., Veerman, J. W., & De Bruyn, E. E. (2003). Bias in parental reports? Maternal psychopathology and the reporting of problem behavior in clinic-referred children. European Journal of Psychological Assessment, 19(3), 195.
Martel, M. M. (2016). Dispositional trait types of ADHD in young children. Journal of Attention Disorders, 20(1), 43–52.
Martel, M. M., von Eye, A., & Nigg, J. (2012). Developmental differences in structure of attention-deficit/hyperactivity disorder (ADHD) between childhood and adulthood. International Journal of Behavioral Development, 36(4), 279–292. https://doi.org/10.1177/0165025412444077
Martel, M. M., Levinson, C., Langer, J., & Nigg, J. (2016). A network analysis of developmental change in ADHD symptom structure from preschool to adulthood. Clinical Psychological Science, 4(6), 988–1001.
McLaughlin, K. A. (2016). Future directions in childhood adversity and youth psychopathology. Journal of Clinical Child & Adolescent Psychology, 45(3), 361–382.
McTeague, L. M., Goodkind, M. S., & Etkin, A. (2016). Transdiagnostic impairment of cognitive control in mental illness. Journal of Psychiatric Research, 83, 37–46. https://doi.org/10.1016/j.jpsychires.2016.08.001
Mittal, V. A., & Wakschlag, L. S. (2017). Research domain criteria (RDoC) grows up: Strengthening neurodevelopment investigation within the RDoC framework. Journal of Affective Disorders, 216, 30–35. https://doi.org/10.1016/j.jad.2016.12.011
Nigg, J. (2017). Annual Research Review: On the relations among self-regulation, self‐control, executive functioning, effortful control, cognitive control, impulsivity, risk‐taking, and inhibition for developmental psychopathology. Journal of Child Psychology and Psychiatry, 58(4), 361–383.
Nigg, J. T., Goldsmith, H. H., & Sachek, J. (2004). Temperament and attention deficit hyperactivity disorder: The development of a multiple pathway model. Journal of Clinical Child and Adolescent Psychology : The Official Journal for the Society of Clinical Child and Adolescent Psychology, American Psychological Association, Division 53, 33(1), 42–53. https://doi.org/10.1207/s15374424jccp3301_5
Nigg, J. T., Sibley, M. H., Thapar, A., & Karalunas, S. L. (2020). Development of ADHD: Etiology, heterogeneity, and early life course. Annual Review of Developmental Psychology, 2(1), 559–583. https://doi.org/10.1146/annurev-devpsych-060320-093413
Nigg, J. T., Sibley, M. H., Thapar, A., & Karalunas, S. L. (2020a). Development of ADHD: Etiology, heterogeneity, and early life course. Annual Review of Developmental Psychology, 2, 559–583.
Peisch, V., & Arnett, A. (2022). Neural activation, cognitive control, and neurodevelopmental symptoms: Evaluating two competing etiological models. Development and Psychopathology.
Pennington, B. F. (2006). From single to multiple deficit models of developmental disorders. Cognition, 101(2), 385–413. https://doi.org/10.1016/j.cognition.2006.04.008
Romer, A. L., & Pizzagalli, D. A. (2021). Is executive dysfunction a risk marker or consequence of psychopathology? A test of executive function as a prospective predictor and outcome of general psychopathology in the adolescent brain cognitive development study®. Developmental Cognitive Neuroscience, 51, 100994. https://doi.org/10.1016/j.dcn.2021.100994
Ronald, A., de Bode, N., & Polderman, T. J. C. (2021). Systematic review: How the Attention-Deficit/Hyperactivity disorder polygenic risk score adds to our understanding of ADHD and Associated Traits. Journal of the American Academy of Child and Adolescent Psychiatry, 60(10), 1234–1277. https://doi.org/10.1016/j.jaac.2021.01.019
Rothbart, M. K. (2007). Temperament, development, and personality. Current Directions in Psychological Science, 16(4), 207–212.
Rothbart, M. K., & Bates, J. E. (Eds.). (2006). Temperament (3 vol.). Wiley. Social Emotional and Personality Development.
Solberg, B. S., Hegvik, T. A., Halmøy, A., Skjærven, R., Engeland, A., Haavik, J., & Klungsøyr, K. (2021). Sex differences in parent–offspring recurrence of attention-deficit/hyperactivity disorder. Journal of Child Psychology and Psychiatry, 62(8), 1010–1018.
Tiego, J., Bellgrove, M. A., Whittle, S., Pantelis, C., & Testa, R. (2020). Common mechanisms of executive attention underlie executive function and effortful control in children. Developmental Science, 23(3), e12918.
Toplak, M. E., West, R. F., & Stanovich, K. E. (2013). Practitioner review: Do performance-based measures and ratings of executive function assess the same construct? Journal of Child Psychology and Psychiatry, 54(2), 131–143.
van den Berg, S. M., Willemsen, G., de Geus, E. J., & Boomsma, D. I. (2006). Genetic etiology of stability of attention problems in young adulthood. American Journal of Medical Genetics Part B: Neuropsychiatric Genetics, 141(1), 55–60.
Waszczuk, M. A., Miao, J., Docherty, A. R., Shabalin, A. A., Jonas, K. G., Michelini, G., & Kotov, R. (2021). General v. specific vulnerabilities: Polygenic risk scores and higher-order psychopathology dimensions in the Adolescent Brain Cognitive Development (ABCD) Study. Psychological medicine, 1–10.
Zelazo, P. D. (2020). Executive function and psychopathology: A neurodevelopmental perspective. Annual Review of Clinical Psychology, 16, 431–454.
Funding
The authors have no funding to disclose related to this work.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Disclosures
None to disclose.
Informed Consent and Ethics Approval
As is detailed on the Adolescent Brain Cognitive DevelopmentSM (ABCD) Study website (http://abcdstudy.org), the ABCD study met.
Permission to Reproduce Material from Other Sources
None to disclose.
Additional information
Publisher’s Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Springer Nature or its licensor (e.g. a society or other partner) holds exclusive rights to this article under a publishing agreement with the author(s) or other rightsholder(s); author self-archiving of the accepted manuscript version of this article is solely governed by the terms of such publishing agreement and applicable law.
About this article
Cite this article
Peisch, V., Li, V. & Arnett, A.B. Effortful Control Protects Against Familial Liability for ADHD: Longitudinal Results from the ABCD Study in the United States. Res Child Adolesc Psychopathol 52, 595–604 (2024). https://doi.org/10.1007/s10802-023-01131-3
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s10802-023-01131-3