Abstract
Although major depressive disorder (MDD) is associated with suicidal behaviors, some depressed individuals are not suicidal and others evidence various forms of suicidality. We thus investigated whether aspects of temperament and self-regulation of dysphoria represent risk factors for DSM-IV suicidality (recurrent thoughts of death, recurrent suicidal ideation, suicidal plan, and suicide attempt) in depressed youths. Using a sample of children with MDD (N = 407; ages 7–14 years), recruited from clinical sites across Hungary, we tested the hypotheses that: (a) suicidality is related to higher levels of trait negative emotionality as well as more maladaptive and fewer adaptive regulatory responses to dysphoria and (b) as the severity of suicidal behavior increases, levels of trait negative emotionality and dysfunctional emotion regulation also increase. We also explored if other aspects of temperament relate to suicidality. Children’s DSM-IV diagnoses were based on semi-structured interviews and best-estimate psychiatric consensus. Parents independently provided ratings of their children’s temperament, and children separately completed an inventory of emotion regulation (ER). Using multivariate models, we failed to confirm the hypothesized relations of negative trait emotionality and suicidality, but confirmed that high maladaptive and low adaptive ER response tendencies increase the odds of suicidal behaviors, above and beyond the risk posed by depressive illness severity. Unplanned interaction terms between temperament dimensions (other than negative emotionality) and ER suggested that at some high-extremes of temperament, ER has no impact on suicidality but in their absence, adaptive ER lowers the risk of suicidality. The practical implications of the findings are discussed.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Suicidal behavior in children and adolescents has continued to receive considerable research attention, with particular interest in identifying clinically useful correlates as well as risk and vulnerability factors (for a review, see Bridge et al. 2006). Much of the past body of research has focused on the association of depression and suicidal behavior. Across diverse samples, such as those clinically referred (Haavisto et al. 2003; Kovacs et al. 1993; Myers et al. 1991a; Pfeffer et al. 1986) as well as those in the community (Bridge et al. 2006), findings have consistently shown that depressed children have high rates of suicidal behavior and that suicidal children are likely to have depressive or mood disorders. For example, in clinical settings, between 72 and 85% of children and adolescents with major depression exhibit some form of suicidal behavior (Kovacs et al. 1993; Myers et al. 1991b; Yorbik et al. 2004). It should be noted, however, that suicidal ideation and suicide attempts have been the most often studied forms of suicidality, although according to the DSM (American Psychiatric Association 1994), suicidal behaviors also can manifest as recurrent thoughts of wanting to die or having made suicidal plans.
It is not entirely surprising that depressive disorders and suicidal behaviors tend to go hand-in-hand, given that suicidality has long been considered one of the criterion symptoms of major depressive or dysthymic disorder episodes (American Psychiatric Association 1994; World Health Organization 1994). At the same time, however, partly because most research has focused on suicidal ideation or attempt, it has not yet been established if the four forms of DSM-specified suicidal behaviors (i.e., recurrent thoughts of wanting to die or wishing to be dead, specific thoughts of wanting to kill oneself or suicidal ideation, suicidal plans, and attempted suicide) are distinct categories or represent a continuum of clinical severity. On the one hand, attempted suicide is often associated with a history of suicidal ideation (thinking and/or talking about killing oneself) including plans and threats, suggesting at least some temporal relations between these behaviors (D’Eramo et al. 2004; Kovacs et al. 1993; Lewinsohn et al. 1994; Reinherz et al. 1995). On the other hand, the fact that most youths who think about killing themselves do not attempt suicide (Kovacs et al. 1993; Myers et al. 1991b; Sanchez and Le 2001), suggests that the behaviors are discontinuous.
In addition to considering the role of depressive disorders in suicidal behaviors, researchers also have been examining the potential contribution of personal traits (Bridge et al. 2006). Personal traits have attracted attention because they are generally stable characteristics, and developmentally are likely to antedate the onset of suicidal or related psychopathology (for a review, see Brezo et al. 2006). Traits that have been associated with suicidal behavior in youngsters include impulsivity, impulsive aggression, trait anxiety, and trait anger (Brent et al. 2003; Brezo et al. 2006; Goldston et al. 1996; McKeown et al. 1998; Myers et al. 1991b; Ohring et al. 1996). Notably, in childhood, various traits such as impulsivity have been regarded as aspects of temperament, which has been defined as individual differences in arousability or physiological reactivity and overall self-regulation (for overviews, see Posner and Rothbart 2000; Shiner 1998). Differences in temperament appear very early in life and are believed to remain reasonably stable (for a review, see Rothbart et al. 2000). Although, as Rettew and McKee (2005) noted, investigators differ in how they define and measure temperament, there is agreement that this is a multidimensional construct and that negative emotionality is one of its key dimension. One of the best-known models of childhood personality (Buss and Plomin 1975, 1984) indeed specifies “emotionality” (the tendency to become easily and intensely negatively aroused) as one of four dimensions of temperament. Negative emotionality also has been regarded as a key component of neuroticism (Shiner 1998).
In general, trait negative emotionality in childhood and adolescence has been shown to be associated with depression and related constructs, such as negative self-schema (Austin and Chorpita 2004; Goodyer et al. 1993; Kelvin et al. 1996; Watson et al. 1988). But studies of temperament (including negative emotionality or neuroticism) and suicidal behaviors have involved almost exclusively adults (Bulik et al. 1999; Engström et al. 1996; Lolas et al. 1991; Lynch et al. 2004; Pendse et al. 1999) and older adolescents (Enns et al. 2003; Fergusson et al. 2000), were limited to some forms of suicidal behaviors, and used a variety of temperament scales. Although findings have been somewhat inconsistent, it appears that individuals who exhibit suicidal behavior usually have higher levels of negative affectivity than various comparison groups. However, little is known about whether other potentially maladaptive traits such as dispositional shyness or behavioral inhibition (e.g., Kagan 1994) contribute to the risk of suicidality.
Another trait variable that has been attracting interest for its role in mental health, in general, and in mood disorders, in particular, is the manner in which an individual self-regulates (modulates) negative emotion (for overviews, see Davidson et al. 2002; Gross 1998). Emotion regulation (ER) has been defined as the processes involved in modifying the dynamic and temporal features of the given emotion and thus entails responses that can maintain and enhance, as well as subdue or inhibit it (Thompson 1994). Emotion self-regulatory responses start to unfold in early childhood, evidence stability within individuals, and have been shown to play an important role in adjustment (e.g., Calkins and Dedmon 2000; Calkins et al. 1999; Cole et al. 2004; Grolnick et al. 1996; Thompson 1994). Maladaptive emotion self-regulatory strategies or responses are likely to be ones that exacerbate (e.g., rumination) rather than lessen or ameliorate (e.g. physical exercise) the dysphoric mood. Indeed, dysfunctional or maladaptive emotion-regulation and depressive affect and disorders have been shown to be associated with one another in community (Garber et al. 1995; Larson et al. 1990; Nolen-Hoeksema and Morrow 1993; Silk et al. 2003) and clinic samples of youths (Garber et al. 1991). However, little is known about the relations of emotion self-regulatory responses and risk of suicidal behaviors among depressed youths. Findings from rather small samples of inpatient adolescents suggest that suicide attempters have more problems in controlling their dysphoric emotions than those with current suicidal ideation, although both groups have various self-regulatory difficulties (Zlotnick et al. 1997, 2003).
In summary, there are suggestions in the literature that trait negative emotionality, as an aspect of temperament, is likely to be more pronounced in youngsters with depressive symptoms or disorders than it is in controls, and that suicidal youths may also be characterized by problems in areas of emotion self-regulation. However, temperament and emotion self-regulation have not been assessed in the same sample of clinically depressed youngsters and therefore it is not known to what extent each alone or together contribute to suicidal behaviors. Additionally, none of the studies of temperament and self-regulation in depression has examined the entire range of suicidal behaviors as specified by the DSM (American Psychiatric Association 1994).
In the present study, we therefore addressed this problem area by testing several hypotheses in our sample of carefully diagnosed, psychiatrically referred depressed youngsters. We hypothesized that the presence of any form of suicidal behavior (compared to its absence) will be associated with: (a) higher level of trait negative emotionality, (b) more extensive deployment of maladaptive ER responses to dysphoria, and (c) less extensive use of adaptive ER responses to dysphoria, and that negative emotionality and maladaptive ER will be increasingly likely as suicidal behavior becomes more severe. We also hypothesized that adaptive ER responses to dysphoria would attenuate the impact of negative emotionality on severity of suicidal behavior. Although our hypotheses about temperament focus on negative emotionality, we examine other dimensions of temperament (activity, shyness, and sociability) in the context of exploratory analyses (both main effects and possible interactions with ER), because there is scant information on how they may be related to ER or suicidality.
In testing our hypotheses, we controlled for the effects of several covariates, including sex, because in population samples, girls are generally more likely to exhibit suicidal behaviors than are boys (Bridge et al. 2006), although among clinically referred depressed youngsters, this association is equivocal (Haavisto et al. 2003; Kovacs et al. 1993; Myers et al. 1991a; Ryan et al. 1987). We controlled for chronological age because it is unequivocally related to suicidal behavior in clinical (Kovacs et al. 1993; Myers et al. 1991b; Ryan et al. 1987) and community samples (Bridge et al. 2006). The importance of considering sex and age as covariates is underscored by our study of the clinical correlates of suicidality in the larger sample (Liu et al. 2006). We controlled for socio-economic status (SES), because it has been directly related to suicidal behaviors in some samples of youth (Fergusson and Lynskey 1995, Fergusson et al. 2000; Hawton et al. 1994) although not in others (Hawton et al. 2001). We also controlled for the presence of anxiety disorder because of some indications that this broad diagnostic category may play a role in risk of suicidal behaviors (Fergusson and Lynskey 1995; Gould et al. 1998; Pilowsky et al. 1999; Reinherz et al. 1995). Finally, in a post hoc analysis, we included in our model an index of depression severity in light of prior findings that, both concurrently and prospectively, severity of depression (among depressed and mood disordered youngsters and adults) is associated with risk of suicidal behaviors (Barbe et al. 2005; Liu et al. 2006; Oquendo et al. 2004). In other words, we wanted to examine whether depression severity affected the relations between our independent and dependent variables.Footnote 1
Materials and Method
Participants
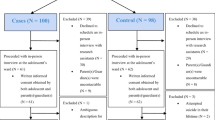
The subjects for the present article are 407 children (189 girls), aged 11.7 years on average (SD = 2.0 years, range of 7.3–14.9 years), who were enrolled and evaluated in a study of genetic and psychosocial risk factors in childhood onset depression by December 31, 2003, had biological mothers as parental informants, and met diagnostic criteria for MDD (detailed below). Ethnic composition was 95.1% Caucasian, 0.3% African, 1.9% multiracial, and 2.7% identifying themselves as Roma or other minorities, representative of the population of Hungary. Years of education of the mothers ranged from 3 to 21 years (M = 11.4 years, SD = 2.8 years). The overall sample has been the focus of various articles addressing facets of subjects’ depressive illness (Kapornai et al. 2007; Kiss et al. 2007), including clinical correlates of suicidality (Liu et al. 2006); sample size have varied across these articles as a function of data base cut-off dates which were used. Further, this study represents part of a larger Program Project of research examining risk factors for and correlates of juvenile-onset depression (e.g., Forbes et al. 2005; Perez-Edgar et al. 2006; Silk et al. 2006).
Enrollment and Assessment Procedures
Children were recruited through 23 child psychiatric facilities (seven of which had both inpatient and outpatient units) across Hungary, serving both urban and rural areas. Based on information available on most sites for the year 2004, we estimate that they provided services to at least 80% of the newly registered child psychiatry cases, giving us access to a significant portion of the referred population nationwide. Children presenting at each research site were scheduled for a research assessment if they met the following criteria: 7.0–14.9 years old, not mentally retarded, no evidence of major systemic medical disorder, had available at least one biologic parent and a 7- to 17.9-year-old sibling (required by the study’s genetic component but not included in this article), and attained a predetermined cut-off score on one of various depressive symptom screens designed for this project. Children meeting these initial criteria were scheduled for a 2-part evaluation, conducted on two separate occasions, about 6 weeks apart, by different clinicians (all with advanced degrees in psychology or psychiatry). Written consent for participation was signed by both parents and the child, in accordance with the legal requirements in Hungary and the IRB of the University of Pittsburgh, Pittsburgh, PA, USA.
The first part of the evaluation entailed administration of the “Mood Disorder Module” of a diagnostic interview (described below), as well as the Intake General Information Sheet (IGIS), a comprehensive demographic and psychosocial history data form. Participants also completed self-rated scales, including the two on which we report in the present article. At each evaluation, parents were interviewed first about their children, and then children were interviewed separately about themselves. To provide a framework and facilitate recall, evaluations started with a semi-structured interview in order to construct a time line (“chronograph”) for the patient from birth to the date of the assessment (identifying key events as markers); this served to identify the chronology of the child’s symptoms and to date disorder onsets and offsets.
The second part of the evaluation involved the full diagnostic interview and the completion of additional self-rated scales, but was administered only if the child had met DSM criteria for mood disorder at the first evaluation. (If DSM criteria were not met, the child was assigned an “at-risk” status and entered a follow-up arm of the study). For our diagnostic interview, we used the Interview Schedule for Children and Adolescents-Diagnostic Version (ISCA-D), which is an extension of the Interview Schedule for Children and Adolescents (ISCA) (Sherrill and Kovacs 2000). The ISCA-D covers the relevant Axis-I DSM-IV as well as some DSM-III disorders and yields symptom ratings and diagnoses for “current” as well as “lifetime” episodes. For any given episode, the ratings reflect the patient’s status at its worst point. The interview was administered by the same interviewer separately to a parent about the child, and then to the child about him/herself.
To increase diagnostic validity, results of the two assessments and associated documentation (e.g., psychiatric records) were subjected to a consensus diagnostic procedure (Maziade et al. 1992). Pairs of senior child psychiatrists, trained as Best Estimate Diagnosticians (BEDs), separately reviewed all material, and then together derived consensus diagnoses. “Caseness,” as well as onset dates of disorders, was based on best-estimate consensus. As described in connection with previous work (Kovacs et al. 1984a, b), operational rules were used to define disorder onset and recovery, and associated dates.
The interviews were administered by child psychiatrists and psychologists who completed 3 months of didactic and practical training in the semi-structured interview technique. They were required to reach an average of 85% symptom-agreement on five consecutive videotaped interviews against “gold standard” ratings provided by the trainers. Routine monitoring and follow-up training sessions served to minimize rater drift. All interviews were audiotaped. Interrater reliability on ISCA-D symptoms was satisfactory (using audiotapes of interviews for n = 46 pairs of raters). For MDD symptoms, kappas ranged from 0.64 to 0.88, with 80% of the coefficients at or above 0.70. For DD symptoms (using DSM-IV criteria), kappas ranged from 0.38 to 0.93, with 80% at or above 0.70. For Generalized Anxiety Disorder symptoms (the most common DSM-IV anxiety diagnosis), kappas ranged from 0.53 to 1.00, with 63% at or above 0.70. Similar inter-rater reliability coefficients were obtained for other disorders as well.
Dependent Variables
Type of Suicidal Behavior
The ISCA-D’s depressive disorders section contains four items on suicidal behavior (as per DSM criteria) in the following order: recurrent thoughts of death (repeatedly thinking about one’s own death and dying; thoughts of wanting to die or wanting to be dead), recurrent suicidal ideation (specific thoughts of wanting to kill oneself), suicidal plan (having formulated a plan and a method to kill oneself), and attempted suicide (an executed behavior, with the goal of killing oneself, which can be of varying degrees of lethality). Each of these items is rated as not present or present. According to a “skip rule,” either of the first two items has to be endorsed in order to proceed to the last two, or else the latter are skipped.
At each assessment, after having recorded the rating for each symptom based on the parent interview and the child interview, the interviewer renders his/her clinician’s overall rating for each symptom. Symptom ratings are recorded for (a) the current or most recent episode of depression, and (b) the first episode of depression (if the current episode is not the first episode). For both current and past ratings, the symptoms are rated for the worst point in that episode. Also in our project, the interviewers had to follow operational rules in reaching their own “overall” rating for each symptom, namely: (a) each overall rating had to be within the ratings given by the parent and child separately for that symptom (e.g., if the parent gave a “3” rating and the child gave a “1” rating to a symptom, the clinician’s overall rating had to be within those bounds), (b) whether the clinician’s final rating is exactly the same as the parent’s, or the child’s, or somewhere in between had to be based on the veracity of the informants on that given symptom (e.g., extent of detailed information; examples of functional impairment they provide; the overall credibility of the information in light of the child’s general context), and (c) having recorded the respondent’s answers, if the clinician did not feel that sufficient information was available to give an overall rating, he/she had to use the “missing information” data code for the overall rating for that given symptom.
Based on the clinicians’ overall ratings, we assigned each subject an overall “suicidal behavior” classification using the current and/or past episode of MDD and assuming a hierarchy of severity. In the present sample, 76.9% were in their first episodes of MDD; thus, for the majority of the sample, the suicidality classification was based on and reflected behavior within the current, first episode. Each subject was assigned to only one group, namely, those with a history of suicidal attempt, or suicidal plan, or suicide ideation, or recurrent thoughts of death, or no evidence of suicidal behavior. If more than one type of item had been endorsed (i.e., both suicidal ideation and suicide attempt), the “more severe” behavior determined the child’s classification.
For the subset of the cases (n = 46) from the larger study who had participated in an inter-rater reliability project, wherein two clinicians independently rated the same interviews, we computed children’s suicidality classification as described above. For these 46 cases, 39 of the children (84.8%) would be categorized into the same suicidality group based on both interviewers’ overall ratings (kappa = 0.79; weighted kappa = 0.89), and no set of interviewers’ ratings resulted in children being more than 1 classification group apart.
Independent Variables
Temperament
Temperament of children was assessed via the parent rated EAS Temperament Questionnaire (Buss and Plomin 1984), completed at the Time 1 assessment, that measures four dimensions: Emotionality (the tendency to experience negative emotions such as irritability, anger), Activity (the preferred level of activity and speed of action), Sociability (the tendency to prefer the presence of others rather than being alone), and Shyness (the tendency to be inhibited and awkward in new social situations).
The EAS has 20 items, five corresponding to each of the four temperament dimensions. Each item is rated on a 5-point scale from “1: not characteristic or typical of your child,” to “5: very characteristic or typical of your child,” and the relevant items are summed to obtain the four temperament scores. In our study, we obtained the following Cronbach’s alphas: emotionality = 0.72; activity = 0.65; sociability = 0.52; and shyness = 0.66, similar to results reported by others (e.g., 0.48–0.79 in Mathiesen and Tambs 1999; and 0.78 on average in Boer and Westenberg 1994). The reported intercorrelations among the four dimensions range from 0.02 to 0.61 and test–retest correlations range from 0.37 to 0.61 (Mathiesen and Tambs 1999). The factor structure of the EAS does not vary substantially with age of the children (Boer and Westenberg 1994; Mathiesen and Tambs 1999). As reported by several investigators, the EAS has construct and predictive validity (Bradley and Lang 1999; Shiner 1998).
Emotion Regulation
The self-rated “Feelings and Me” Child version (FAM-C; Kovacs 2000) questionnaire served as an index of children’s self-regulatory responses to dysphoria and distress. This new instrument, suitable for ages 7–17 years, lists a variety of adaptive and maladaptive responses (representing the behavioral, social–interpersonal, cognitive, and physical/somatic regulatory domains), which can be deployed when feeling sad or upset. Items were derived from multiple sources (including pilot testing with children), were pre-tested with various samples of youngsters, and were each classified by seven clinical psychologists according to whether it represented an adaptive (or functional) versus a maladaptive (or dysfunctional) response, and the primary and secondary response domain being exemplified.
In the questionnaire, the stem “When I feel sad or upset, I: ...” is followed by a series of statements (e.g., “... throw, kick, or hit things”) that respondents rate on a scale ranging from “0 = not true of me” to “2 = many times true of me.” For the present analyses, we used the two major FAM subscale scores: Adaptive ER (32 items) and Maladaptive ER (22 items). In accordance with the logic underlying the scale construction, unpublished work on a large sample (unrelated to the present article) suggested that the adaptive–maladaptive dimension is the primary factor underlying the questionnaire. Adaptive ER mirrors responding to one’s own dysphoric emotion in ways which are likely to attenuate or modulate it (e.g., “I get my mom to give me a hug,” “I try to think of fun things”); Maladaptive ER mirrors responding which is likely to maintain and exacerbate the dysphoria (e.g., “I go away and hide,” “I throw and hit things”).
The FAM-C questionnaire has face validity and acceptable initial psychometric properties, as suggested by the following. In the present sample, Cronbach’s alpha is 0.89 for the Adaptive ER subscale and .87 for the Maladaptive ER subscale. Construct validity is partially supported by the correlation of 0.64 (p < 0.0001) between the Maladaptive ER score and the Children’s Depression Inventory (Kovacs 2003). Concurrent validity is supported by the correlation of 0.71 between the Maladaptive ER subscale and a version of the Depressive Rumination scale (Nolen-Hoeksema and Morrow 1993) modified for children. In the larger depressed clinical sample enrolled in the main study (n = 649) the mean Maladaptive ER score was significantly higher (p < 0.0001) than in an age-and-sex matched school-based sample in Hungary (15.20 versus 8.24, respectively). In two USA based pediatric (normal control and at-risk for depression) samples, also involved in the overall Program Project, the correlation coefficients we obtained were similar to those noted above (in the Hungarian sample) with regard to Maladaptive ER and (a) self-rated depression (rs = 0.46 and 0.52, respectively) and (b) rumination (rs = 0.57, and .49, respectively). As also shown in the USA sample, the instrument has acceptable long-term stability: re-test with n = 42 youngsters (mean initial age = 8.5 years) after a 1-year (± 3 months) interval yielded an intraclass correlation coefficient of 0.44 (p < 0.01) for each of the two subscores.
Covariates
Anxiety Disorders
The presence of any anxiety disorder (regardless of its type and timing) was used as a covariate. Altogether 143 children (35.1%) had anxiety disorders, with all the relevant DSM-IV anxiety diagnoses having been represented.
MDD Severity
Clinicians rated children’s overall severity of their current or most recent episode of MDD on a 5-point scale: 1 = mild, 2 = moderate, 3 = severe without psychotic features, 4 = severe with mood-congruent features and 5 = severe with mood-incongruent features. The observed values for this index ranged from 1 to 4 (M = 2.28, SD = 0.71).
Child’s sex, child’s age, and maternal educational level were also controlled, as noted in the Introduction.
Statistical Analyses
The association of independent variables and covariates with type of suicidal behavior was tested with Kruskal–Wallis tests for continuous variables and chi-square tests for categorical variables. The Kruskal–Wallis test was used because of non-normal distributions for the continuous variables at one or more levels of suicidal behavior.
Using a hierarchical method, polychotomous regression models were developed to investigate the association between temperament and emotion regulation and type of suicidal behavior, adjusting for covariates. First we entered into the model the covariates of interest: age, sex, maternal education, and anxiety. Temperament scales were then entered as independent variables, followed by Maladaptive and Adaptive ER scores, and interaction terms between ER and temperament scale scores. Continuous variables were centered (i.e., a new variable was created by the original variable minus its mean) prior to computing interaction terms. We then repeated the entire procedure with the addition of depression severity as a covariate.1 Although our results with regard to our hypotheses did not substantially change, we report the outcome of the model which included depression severity. We summarize the results as odds ratios (OR) and their 95% confidence intervals (CI). Statistical Analyses Software (SAS) version 8.2 was used to perform all analyses.
Results
In this clinical sample of children with MDD, 67% had a history of suicidal behavior (Table 1). Recurrent thoughts of death, suicidal ideation, and suicidal plan had comparable rates of around 18–20% each, with suicidal attempt being the least common (12%).
There were no statistically significant differences in Emotionality, Sociability, or Shyness across the groups of children with different types of suicidal behaviors. The four groups of subjects significantly differed only on one temperament dimension: those with a history of suicide attempts were rated by their mothers as displaying the lowest levels of trait Activity.
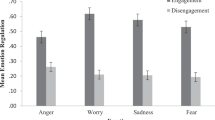
The means for the ER scales were found to be generally in the predicted direction: that is, Maladaptive ER response scores tend to increase and Adaptive ER response scores tend to decrease as the type of suicidal behavior becomes more severe. Additionally, we found that non-suicidal children were younger than suicidal ones, that the oldest children were the most likely to have attempted suicide, and that more girls than boys had suicidal ideation and suicidal attempts (although the sex ratio was reversed with regard to recurrent thoughts of death and suicide plans) (Table 1). Rates of anxiety disorders, which ranged from 13 to 22% across the various categories of suicidality, were not significantly different.
Association among Independent Variables
Three of the four temperament subscales were significantly inter-correlated: Shyness and Sociability r = −0.50 (p < 0.001); Shyness and Activity r = −0.36 (p < 0.001); and Sociability and Activity r = 0.35 (p < 0.001). But Emotionality was not related to the other temperament dimensions (ps > 0.31). We found a very modest correlation between Adaptive and Maladaptive ER scale scores (r = 0.15, p = 0.002) and similarly modest (although statistically significant) associations between Maladaptive ER and Shyness (r = −0.12, p < 0.05), and between Adaptive ER and Shyness (r = −0.15, p < 0.05), Sociability (r = 0.16, p < 0.01), and Activity (r = 0.10, p < 0.05). We also examined whether any of the covariates (age, sex, maternal education level, comorbid anxiety disorder) was related to temperament and ER. We found that age was moderately related both to Adaptive and Maladaptive ER scale scores (r = −0.22, 0.20, respectively, p < 0.0001), and Adaptive ER scale score and maternal education level also were related (r = −0.18, p < 0.0002).
Sex differences were detected on two independent variables. Namely, parents rated sons significantly higher on the Activity subscale of the EAS than daughters (t (401) = −3.55, p = 0.0004), and girls reported higher rates of Maladaptive ER responses than did boys (t (400) = 4.97, pd < 0.0001). Finally, children with comorbid anxiety disorder scored significantly higher on the Emotionality and Shyness scales than children without anxiety (t (402) = −2.62, p = 0.0092; t (398) = −2.55, p = 0.0112, respectively).
Modeling the Various Types of Suicidal Behaviors
In the polychotomous model, mother’s education was not statistically significant; therefore it was not included in any later models. Interaction terms were dropped sequentially from the model based on their p-values, and only those with p < 0.05 were retained in the final model. All EAS and ER scale scores were included in the model as well as sex, age, and anxiety, regardless of their p-values. Subjects at each level of suicidal behavior were individually compared to the non-suicidal group in the same model. A given odds ratio therefore indicates the risk of exhibiting a specific suicidal behavior in comparison to the non-suicidal group for a given independent variable. The overall model (with depression severity included) was significant (−2 Log Likelihood for intercept and covariates = 995.80, p < 0.0001) and is shown in Table 2.
As can be seen (Table 2), subjects with recurrent thoughts of death and non-suicidal subjects were indistinguishable on each of the independent variables. Additionally, the EAS Temperament scales had very inconsistent relationships to the remaining three categories of suicidality: suicide ideators and nonsuicidal subjects were similar on all four EAS scales; increased Emotionality (OR = 1.53, p < 0.05) and Activity (OR = 1.89 p < 0.01) distinguished those with suicidal plans from non-suicidal ones; whereas higher scores on Shyness differentiated attempters and non-suicidal cases (OR = 2.06, p < 0.05).
In contrast, the association between emotion regulatory responses and suicidality was more straightforward. Maladaptive ER was consistently associated with specific suicidal behavior (except with recurrent thoughts of death), with the odds ratios increasing very slightly for suicide attempters (Table 2). Thus, as can be seen in Table 2, higher Maladaptive ER scores differentiated each of the three suicidal groups from the non-suicidal group. Similarly, lower scores on the Adaptive ER subscale characterize ideators (OR = 0.96, p < 0.01), those with suicidal plan (OR = 0.94, p < 0.001), and attempters (OR = 0.93, p < 0.01), compared to non-suicidal youngsters.
We also found statistically significant interactions between Adaptive ER and Shyness (OR = 1.08, p < 0.01), as well as Adaptive ER and Sociability (OR = 1.08, p < 0.01) in the model of suicide attempters (compared to non-suicidal children). As illustrated in Fig. 1, for children high on trait Shyness, the extent of Adaptive ER repertoire (i.e., High versus Low in the figure) does not substantially alter the odds of being a suicide attempter. In contrast, extent of Adaptifsve ER does make a difference for children with lower levels of trait Shyness; for them, adaptive ways of regulating dysphoria are associated with lower odds of being a suicide attempter. The other interaction (see Fig. 2) indicates that, at higher levels of trait Sociability, extent of Adaptive ER does not substantially impact on the odds of being an attempter. However, among children at lower levels of Sociability, having an extensive repertoire of Adaptive ER skills (i.e., High ER in the figure) signals decreased odds of being a suicide attempter.
The results also reveal that severity of the depressive episode is very significantly related to risk of suicidal behavior: this is most dramatic with regard to suicidal plans and suicide attempts. For example, each unit change in depression severity increases the odds of being a suicide attempter about seven-fold (Table 2). Importantly, however, given that the model in Table 2 has accounted for the effect of depression severity, the results indicate that the contribution of ER response tendencies to suicidality is independent of MDD severity.
Discussion
Although the association between depressive disorders and suicidal behaviors is well documented (Haavisto et al. 2003; Kovacs et al. 1993; Myers et al. 1991a; Pfeffer et al. 1986, 1991), the fact remains that many depressed youngsters do not manifest suicidality, and that the rest display various types of suicidal symptoms. In the present study, we were primarily interested in investigating whether trait negative emotionality (as an index of temperament) and aspects of emotion self-regulation contribute to the variability in suicidal behaviors among depressed children and adolescents.
As an index of temperament, negative emotionality is typically evident early in life (Shiner 1998) and by late childhood and thereafter, has been associated with the presence of depression (Goodyer et al. 1993; Kelvin et al. 1996; Watson et al. 1988). Having a predominantly negative affective temperament may plausibly contribute to the risk of suicidality in depression in several ways, including by worsening the extent of dysphoria or anhedonia, exacerbating the overall severity of the disorder, or compromising cognitive appraisal.
The ways in which youngsters respond to (or regulate) their own dysphoric mood also are presumed to have their origins in early childhood, during which time individual differences in emotion self-regulation already are evident (Thompson 1994). By adolescence, difficulties in modulating or “downregulating” dysphoric mood have been associated with depression and suicidal behaviors (Garber et al. 1991; Zlotnick et al. 1997, 2003). The ability to adaptively self-modulate dysphoria (e.g., to decrease its intensity or duration) may alter the risk of suicidal behaviors in depression by impacting on the mood component of the disorder.
Accordingly, we posited that, among depressed youngsters, the presence and severity of suicidal behavior would be associated with higher levels of trait negative emotionality, and more maladaptive (and fewer adaptive) emotion regulatory responses to dysphoria. We also hypothesized that adaptive ER responding would moderate the relations between high negative emotionality and suicidal behaviors. While it has been proposed that, in infancy, temperament dispositions may be closely related to ER skill acquisition (e.g., Calkins 1994), our hypotheses suggest that we regard temperament and ER as separable constructs in the age groups under consideration. Indeed, studies of children have found that emotionality and regulation are only modestly related (e.g., Rydell et al. 2003), underscoring that these dimensions are not homologous. In testing our hypotheses, we controlled for the effects of variables (e.g., age and sex) that have been shown to be associated with suicidal behaviors. Then, we also added an index of depression severity owing to its previously documented relations to suicidality.
Using data from a very large sample of depressed youngsters, we failed to confirm our hypothesis that high level of trait negative emotionality is associated with suicidal behaviors. In fact, our depressed non-suicidal and depressed suicidal children had comparable levels of negative emotionality (see Table 1). And this trait variable only distinguished children with suicide plans from nonsuicidal depressed children, but at a modest level (p < 0.05), thereby rendering the finding tentative. Negative emotionality (quantified by the EAS scale) has been associated with depression in children recruited from the community (Goodyer et al. 1993; Lengua et al. 1998). Our failure to find strong and consistent main effects for negative emotionality may be due to the fact that the corresponding scores were negatively skewed in our sample, with about 8% at the maximum value of 5.00 (whereas the Shyness, Sociability, and Activity scores were more normally distributed). Thus, a ceiling effect could have decreased the likelihood of obtaining the predicted results for Negative Emotionality.
However, we confirmed our hypotheses about the relations of dysphoria-focused emotion self-regulation and suicidality, with some interesting exceptions. First, we found that, with regard to how they reportedly self-regulate distress, nonsuicidal children and those with recurrent thoughts of death cannot be distinguished from one another. Because these two groups of depressed children also were very similar on the four dimensions of temperament, it is possible that recurrent thoughts of death are less closely related to suicidal behavior than hitherto thought. This possibility should be investigated in future research.
Second, we found that depressed children with the remaining three types of suicidal behaviors consistently differ from non-suicidal peers by virtue of higher scores on the Maladaptive and lower scores on the Adaptive ER scales. In other words, a depressed child who is characterized by many maladaptive regulatory responses to dysphoria is likely to be a child with definite suicidal behaviors (ideation, plans, or attempts). Conversely, a more extensive repertoire of adaptive regulatory responses to dysphoria signals a decreased likelihood of specific suicidal behavior. Notably, these two aspects of emotion regulation represent relatively independent dimensions. Thus, from a clinical perspective, these findings could suggest that the risk of specific suicidal behavior in depressed children may be lowered in two ways: by enlarging their repertoire of adaptive ER responses to dysphoria, and by decreasing their repertoire of maladaptive ER responses.
Our results also suggest that youngsters who have attempted suicide have the least favorable distress-specific emotion regulatory profile as mirrored by their considerably higher Maladaptive ER score than those of the other groups of children (see Table 1). Other researchers have specifically commented on the affect regulatory problems of adolescent suicide attempters and have suggested that overt suicidal acts may represent ways to reduce “intolerable emotional states” (Zlotnick et al. 1997). Although addressing primarily the context of borderline personality disorder, Marsha Linehan’s conceptual paradigm also highlights that suicidal behavior can be a direct response to intense negative affect and can serve to downregulate or dissipate it (for overviews, see Harned et al. 2006; McMain et al. 2001). Thus, in the presence of mood disorder, attempted suicide may represent a behaviorally-focused ER response which presumably can interrupt or modulate the dysphoric affect.
Importantly, our findings regarding ER and temperament did not notably change when we added severity of depression to the model. Depression severity, indexed as a sum of clinical symptom ratings, has been found to be related to suicidality in the larger sample of our study (Liu et al. 2006) and in another sample of 7- to 17-year-old depressed youngsters (Barbe et al. 2005). And among adults with mood disorder, self-rated depression severity also predicted subsequent suicidal acts (Oquendo et al. 2004). It is not entirely clear how depression severity accounts for the increased risk of suicidality. Thus, future research on the relations of depression severity and suicidality should address mediators and moderators (including possibly ER). We suspect, however, that “severity indices” may either reflect the overall mood component of the disorder (extent of despondency and anhedonia), or possibly the multiplicity of symptoms that significantly impair daily functioning, either of which may become “too much” to bear. According to our findings, a child’s maladaptive dysphoria-related ER response repertoire poses a risk for suicidal behavior, which is above and beyond the contribution of depression severity. Please note that the ER scale-related odds ratios is Table 2 refer to a change in the odds of the given outcome per unit change on the ER scale. Thus, for example, given a depressed child, whose Maladaptive ER score is eight points higher (∼1 SD) than the score of another child, the higher scorer is about 3.3 times more likely (i.e., 1.168) to be an attempter than a non-suicidal depressed peer. This finding may have relevance to prevention efforts, because ER response styles appear to be moderately stable and may be assessed in children at risk for, but prior to a depressive episode.
Although we did not have hypotheses addressing temperament dimensions other than Emotionality, we detected interaction terms between ER and trait Shyness as well as trait Sociability in the statistical model for suicide attempters. Taken together, these findings may suggest that when some temperament traits become extreme, emotion regulatory competence (or its lack therein) has little impact on the odds of suicide attempt, but in the absence of extreme traits, Adaptive ER skills appear to serve as protective factors and lower the odds of attempted suicide.
Several other findings are also of note. The overall portion of our depressed sample with some type of suicidal behavior is generally comparable to rates for depressed young patients in Finnish and USA samples (Haavisto et al. 2003; Myers et al. 1991b). The sex effect across suicidal behaviors in this Hungarian sample (for which we controlled in our analyses) echoes a large body of research on the preponderance of girls among suicide ideators and attempters (Bridge et al. 2006). In future research, it would be interesting to examine whether sex moderates the relations of ER and suicidality. Finally, although rates of recurrent thoughts of death and suicide plans among clinically referred youngsters have not yet been established, our findings parallel reports from other studies indicating that a suicide attempt is the least frequent expression of suicidal behavior in our targeted age group (Haavisto et al. 2003; Kovacs et al. 1993; Myers et al. 1991b; Pfeffer et al. 1986, 1991).
The results of our study should be evaluated in light of several limitations. First, we used a cross-sectional design and therefore cannot prove that aspects of temperament and maladaptive emotion regulation preceded and were causally related to suicidal behaviors. Although temperament and emotion self-regulatory styles are believed to emerge early in development and remain fairly stable (Calkins 1994; Rothbart et al. 2000; Thompson 1994), longitudinal research is needed to verify their prospective contribution to depressive psychopathology, including suicidal behaviors. Second, our measures of temperament and ER may be viewed as constraining our findings. The EAS temperament scales showed somewhat low reliability and surprisingly low or nonsignificant associations with other measures (e.g., negative emotionality was uncorrelated with ER scales). Additionally, the FAM scale used to quantify emotion regulatory responding is a new instrument. Although its initial psychometric properties are promising, further research is needed to determine its validity and usefulness. Finally, even though our study included a diverse and nationally representative clinical sample of carefully diagnosed depressed children in Hungary, the sample is homogeneous in terms of ethnicity. All in all, while we expect that our findings would generalize to other populations of psychiatrically referred depressed youth, this will have to be explored in future studies.
Notes
We thank the anonymous reviewers for their suggestions in this regard.
References
American Psychiatric Association (1994). Diagnostic and statistical manual of mental disorders (4th ed.). Washington, DC: Author.
Austin, A. A., & Chorpita, B. F. (2004). Temperament, anxiety, and depression: Comparison across five ethnic groups of children. Journal of Clinical Child and Adolescent Psychology, 33, 216–226.
Barbe, R. P., Williamson, D. E., Bridge, J. A., Birmaher, B., Dahl, R. E., Axelson, D. A., et al. (2005). Clinical differences between suicidal and nonsuicidal depressed children and adolescents. Journal of Clinical Psychiatry, 66, 492–498.
Boer, F., & Westenberg, P. M. (1994). The factor structure of the Buss and Plomin EAS temperament survey (Parental Ratings) in Dutch sample of elementary school children. Journal of Personality Assessment, 62, 537–551.
Bradley, M. M., & Lang, P. J. (1999). Fearfulness and affective evaluations of pictures. Motivation and Emotion, 23, 1–13.
Brent, D. A., Oquendo, M., Birmaher, B., Greenhill, L., Kolko, D., Stanley, B., et al. (2003). Peripubertal suicide attempts in offspring of suicide attempters with siblings concordant for suicidal behavior. The American Journal of Psychiatry, 160, 1486–1493.
Brezo, J., Paris, J., & Turecki, G. (2006). Personality traits as correlates of suicidal ideation, suicide attempts, and suicide completions: A systematic review. Acta Psychiatrica Scandinavica, 113, 180–206.
Bridge, J. A., Goldstein, T. R., & Brent, D. A. (2006). Adolescent suicide and suicidal behavior. Journal of Child Psychology and Psychiatry, 47, 372–394.
Bulik, C. M., Sullivan, P. F., & Joyce, P. R. (1999). Temperament, character and suicide attempts in anorexia nervosa, bulimia nervosa and major depression. Acta Psychiatrica Scandinavica, 100, 27–32.
Buss, A. H., & Plomin, R. (1975). A temperament theory of personality development. New York: Wiley.
Buss, A. H., & Plomin, R. (1984). Temperament: Early developing personality traits. Hillsdale, NJ: Lawrence Erlbaum.
Calkins, S. D. (1994). Origins and outcomes of individual differences in emotion regulation. Monographs of the Society for Research in Child Development, 59, 2–3 (Serial No. 240), 53–72.
Calkins, S. D., & Dedmon, S. E. (2000). Physiological and behavioral regulation in two-year-old children with aggressive/destructive behavior problems. Journal of Abnormal Child Psychology, 28, 103–118.
Calkins, S. D., Gill, K. l., Johnson, M. C., & Smith, C. L. (1999). Emotional reactivity and emotional regulation strategies as predictors of social behavior with peers during toddlerhood. Social Development, 8, 310–334.
Cole, P. M., Martin, S. E., & Dennis, T. A. (2004). Emotion regulation as a scientific construct: methodological challenges and directions for child development research. Child Development, 75, 317–333.
D’Eramo, K. S., Prinstein, M. J., Freeman, J., Grapentine, W. L., & Spirito, A. (2004). Psychiatric diagnoses and comorbidity in relation to suicidal behavior among psychiatrically hospitalized adolescents. Child Psychiatry and Human Development, 35, 21–35.
Davidson, R. J., Pizzagalli, D., Nitschke, J. B., & Putnam, K. (2002). Depression: Perspectives from affective neuroscience. Annual Review of Psychology, 53, 545–574.
Engström, G., Nyman, G. E., & Träskman-Bendz, L. (1996). The Marke–Nyman Temperament (MNT) scale in suicide attempters. Acta Psychiatrica Scandinavica, 94, 320–325.
Enns, M. W., Cox, B. J., & Inayatulla, M. (2003). Personality predictors of outcome for adolescents hospitalized for suicidal ideation. Journal of the American Academy of Child and Adolescent Psychiatry, 42, 720–727.
Fergusson, D. M., & Lynskey, M. T. (1995). Childhood circumstances, adolescent adjustment, and suicide attempts in a New Zealand birth cohort. Journal of the American Academy of Child and Adolescent Psychiatry, 34, 612–622.
Fergusson, D. M., Woodward, L. J., & Horwood, L. J. (2000). Risk factors and life processes associated with the onset of suicidal behaviour during adolescence and early adulthood. Psychological Medicine, 30, 23–39.
Forbes, E. E., Miller, A., Cohn, J. F., Fox, N. A., & Kovacs, M. (2005). Affect-modulated startle in adults with childhood-onset depression: Relations to bipolar course and number of lifetime depressive episodes. Psychiatry Research, 134, 11–25.
Garber, J., Braafladt, N., & Weiss, B. (1995). Affect regulation in depressed and nondepressed children and young adolescents. Development and Psychopathology, 7, 93–115.
Garber, J., Braafladt, N., & Zeman, J. (1991). The regulation of sad affect: An information-processing perspective. In J. Garber & K. A. Dodge (Eds.), The development of emotion regulation and dysregulation (pp. 208–240). New York: Cambridge University Press.
Goldston, D. B., Daniel, S., Reboussin, D. M., Kelley, A., Ievers, C., & Brunstetter, R. (1996). First-time suicide attempters, repeat attempters, and previous attempters on an adolescent inpatient psychiatry unit. Journal of the American Academy of Child and Adolescent Psychiatry, 35, 631–639.
Goodyer, I. M., Ashby, L., Altham, P. M., Vize, C., & Cooper, P. J. (1993). Temperament and major depression in 11 to 16 year olds. Journal of Child Psychology and Psychiatry, 34, 1409–1423.
Gould, M. S., King, R., Greenwald, S., Fisher, P., Schwab-Stone, M., Kramer, R., et. al. (1998). Psychopathology associated with suicidal ideation and attempts among children and adolescents. Journal of the American Academy of Child and Adolescent Psychiatry, 37, 915–923.
Grolnick, W. S., Bridges, L. J., & Connell, J. P. (1996). Emotion regulation in two-year-olds: Strategies and emotional expression in four contexts. Child Development, 67, 928–941.
Gross, J. J. (1998). The emerging field of emotion regulation: An integrative review. Review of General Psychology, 3, 271–299.
Haavisto, A., Sourander, A., Ellilä, H., Välimäki, M., Santalahti, P., & Helenius, H. (2003). Suicidal ideation and suicide attempts among child and adolescent psychiatric inpatients in Finland. Journal of Affective Disorders, 76, 211–221.
Harned, M. S., Banawan, S. F., & Lynch, T. R. (2006). Dialectical behavior therapy: An emotion-focused treatment for borderline personality disorder. Journal of Contemporary Psychotherapy, 36, 67–75.
Hawton, K., Fagg, J., Simkin, S., & Mills, J. (1994). The epidemiology of attempted suicide in the Oxford area, England (1989–1992). Crisis: The Journal of Crisis Intervention and Suicide Prevention, 15, 123–135.
Hawton, K., Harriss, L., Simkin, S., Bale, E., & Bond, A. (2001). Social class and suicidal behaviour: The associations between social class and the characteristics of deliberate self-harm patients and the treatment they are offered. Social Psychiatry and Psychiatric Epidemiology, 36, 437–443.
Kagan, J. (1994). On the nature of emotion. In N. A. Fox (Ed.), Emotion regulation: Behavioral and biological considerations. Monographs of the Society for Research in Child Development, vol. 2–3, Serial no. 240 (pp. 7–24).
Kapornai, K., Gentzler, A. L., Tepper, P. G., Kiss, E., Mayer, L., Tamás, Zs., et al. (2007). Early developmental characteristics and features of major depressive disorder among child psychiatric patients in Hungary. Journal of Affective Disorders, in press.
Kelvin, R. G., Goodyer, I. M., & Altham, P. M. E. (1996). Temperament and psychopathology amongst siblings of probands with depressive and anxiety disorders. Journal of Child Psychology and Psychiatry, 37, 543–550.
Kiss, E., Gentzler, A. L., Kapornai, K., Tamás, Zs., Kovacs, M., & Vetró, A., et al. (2007). Factors influencing mother–child reports of depressive symptoms and agreement among clinically referred depressed youngsters in Hungary. Journal of Affective Disorders, in press.
Kovacs, M. (2000). The “Feelings and Me” emotion regulatory strategy utilization questionnaires. Pittsburgh, PA: University of Pittsburgh School of Medicine.
Kovacs, M. (2003). Children’s depression inventory: Technical manual update. Toronto, Multi-health Systems.
Kovacs, M., Feinberg, T. L., Crouse-Novak, M. A., Paulauskas, S. L., & Finkelstein, R. (1984a). Depressive disorders in childhood. I. A longitudial prospective study of characteristics and recovery. Archives of General Psychiatry, 41, 229–237.
Kovacs, M., Feinberg, T. L., Crouse-Novak, M. A., Paulauskas, S. L., Pollock, M., & Finkelstein, R. (1984b). Depressive disorders in childhood. II. A longitudinal study of the risk for a subsequent major depression. Archives of General Psychiatry, 41, 653–659.
Kovacs, M., Goldston, D., & Gatsonis, C. (1993). Suicidal behaviors and childhood-onset depressive disorders: A longitudinal investigation. Journal of the American Academy of Child and Adolescent Psychiatry, 32, 8–20.
Larson, R. W., Raffaelli, M., Richards, M. H., Ham, M., & Jewell, L. (1990). Ecology of depression in late childhood and early adolescence: A profile of daily states and activities. Journal of Abnormal Psychology, 99, 92–102.
Lengua, L. J., West, S. G., & Sandler, I. N. (1998). Temperament as a predictor of symptomatology in children: Addressing contamination of measures. Child Development, 69, 164–181.
Lewinsohn, P. M., Rohde, P., & Seeley, J. R. (1994). Psychosocial risk factors for future adolescent suicide attempts. Journal of Consulting and Clinical Psychology, 62, 297–305.
Liu, X., Gentzler, A. L., Tepper, P., Kiss, E., Kothencné, V., Tamás, Z., et al. (2006). Clinical features of depressed children and adolescents with various forms of suicidality. Journal of Clinical Psychiatry, 67, 1442–1450.
Lolas, F., Gomez, A., & Suarez, L. (1991). EPQ-R and suicide attempt: The relevance of psychoticism. Personality and Individual Differences, 12, 899–902.
Lynch, T. R., Cheavens, J. S., Morse, J. Q., & Rosenthal, M. Z. (2004). A model predicting suicidal ideation and hopelessness in depressed older adults: The impact of emotion inhibition and affect intensity. Aging & Mental Health, 8, 486–497.
Mathiesen, K. S., & Tambs, K. (1999). The EAS Temperament Questionnaire—Factor structure, age trends, reliability, and stability in a Norwegian sample. Journal of Child Psychology and Psychiatry, 40, 431–439.
Maziade, M., Roy, M. A., Fournier, J. P., Cliché, D., Mérette, C., Caron, C., et al. (1992). Reliability of best-estimate diagnosis in genetic linkage studies of major psychoses: Results from the Quebec pedigree studies. The American Journal of Psychiatry, 149, 1674–1686.
McKeown, R. E., Garrison, C. Z., Cuffe, S. P., Waller, J. L., Jackson, K. L., & Addy, C. L. (1998). Incidence and predictors of suicidal behaviors in a longitudinal sample of young adolescents. Journal of the American Academy of Child and Adolescent Psychiatry, 37, 612–619.
McMain, S., Korman, L. M., & Dimeff, L. (2001). Dialectical behavior therapy and the treatment of emotion dysregulation. Psychotherapy in Practice, 57, 183–196.
Myers, K., McCauley, E., Calderon, R., Mitchell, J., Burke, P., & Schloredt, K. (1991a). Risks for suicidality in major depressive disorder. Journal of the American Academy of Child and Adolescent Psychiatry, 30, 86–94.
Myers, K., McCauley, E., Calderon, R., & Treder, R. (1991b). The 3-year longitudinal course of suicidality and predictive factors for subsequent suicidality in youths with major depressive disorder. Journal of the American Academy of Child and Adolescent Psychiatry, 30, 804–810.
Nolen-Hoeksema, S., & Morrow, J. (1993). Effects of rumination and distraction on naturally occuring depressed mood. Cognition and Emotion, 7, 561–570.
Ohring, R., Apter, A., Ratzoni, G., Weizman, R., Tyano, S., & Plutchik, R. (1996). State and trait anxiety in adolescent suicide attempters. Journal of the American Academy of Child and Adolescent Psychiatry, 35, 154–157.
Oquendo, M. A., Galfalvy, H., Russo, S., Ellis, S. P., Grunebaum, M. F., Burke, A., et al. (2004). Prospective study of clinical predictors of suicidal acts after a major depressive episode in patients with major depressive disorder or bipolar disorder. American Journal of Psychiatry, 161, 1433–1441.
Pendse, B., Westrin, Å., & Engström, G. (1999). Temperament traits in seasonal affective disorder, suicide attempters with non-seasonal major depression and healthy controls. Journal of Affective Disorders, 54, 55–65.
Perez-Edgar, K., Fox, N. A., Cohn, J. F., & Kovacs, M. (2006). Behavioral and electrophysiological markers of selective attention in children of parents with a history of depression. Biological Psychiatry, 60, 1131–1138.
Pfeffer, C. R., Klerman, G. L., Hurt, S. W., Lesser, M., Peskin, J. R., & Siefker, C. A. (1991). Suicidal children grow up: Demographic and clinical risk factors for adolescent suicide attempts. Journal of the American Academy of Child and Adolescent Psychiatry, 30, 609–616.
Pfeffer, C. R., Plutchik, R., Mizruchi, M. S., & Lipkins, R. (1986). Suicidal behavior in child psychiatric inpatients and outpatients and in nonpatients. The American Journal of Psychiatry, 143, 733–738.
Pilowsky, D. J., Wu, L. T., & Anthony, J. C. (1999). Panic attacks and suicide attempts in mid-adolescence. The American Journal of Psychiatry, 156, 1545–1549.
Posner, M. I., & Rothbart, M. K. (2000). Developing mechanisms of self-regulation. Development and Psychopathology, 12, 427–441.
Reinherz, H. Z., Giaconia, R. M., Silverman, A. B., Friedman, A., Pakiz, B., Frost, A. K., et al. (1995). Early psychosocial risks for adolescent suicidal ideation and attempts. Journal of the American Academy of Child and Adolescent Psychiatry, 34, 599–611.
Rettew, D. C., & McKee, L. (2005). Temperament and its role in developmental psychopathology. Harvard Review of Psychiatry, 13, 14–27.
Rothbart, M. K., Ahadi, S. A., & Evans, D. E. (2000). Temperament and personality: Origins and outcomes. Journal of Personality and Social Psychology, 78, 122–135.
Ryan, N. D., Puig-Antich, J., Ambrosini, P., Rabinovich, H., Robinson, D., Nelson, B., et al. (1987). The clinical picture of major depression in children and adolescents. Archives of General Psychiatry, 44, 854–861.
Rydell, A., Berlin, L., & Bohlin, G. (2003). Emotionality, emotion regulation, and adaptation among 5- to 8-year-old children. Emotion, 3, 30–47.
Sanchez, L. E., & Le, L. T. (2001). Suicide in mood disorders. Depression and Anxiety, 14, 177–182.
Sherrill, J. T., & Kovacs, M. (2000). Interview schedule for children and adolescents (ISCA). Journal of the American Academy of Child and Adolescent Psychiatry, 39, 67–75.
Shiner, R. L. (1998). How shall we speak of children’s personalities in middle childhood? A preliminary taxonomy. Psychological Bulletin, 124, 308–332.
Silk, J. S., Shaw, D. S., Skuban, E. M., Oland, A. A., & Kovacs, M. (2006). Emotion regulation strategies in offspring of childhood-onset depressed mothers. Journal of Child Psychology and Psychaitry, 47, 69–78.
Silk, J. S., Steinberg, L., & Morris, A. S. (2003). Adolescents’ emotion regulation in daily life: Links to depressive symptoms and problem behavior. Child Development, 74, 1869–1880.
Thompson, R. A. (1994). Emotion regulation: A theme in search of definition. In N. A. Fox (Ed.), Emotion regulation: Behavioral and biological considerations. Monographs of the Society for Research in Child Development, vol. 2–3, Serial no. 240 (pp. 25–52).
Watson, D., Clark, L. A., & Carey, G. (1988). Positive and negative affectivity and their relation to anxiety and depressive disorders. Journal of Abnormal Psychology, 97, 346–353.
World Health Organization. (1994). International statistical classification of diseases and related health problems (10th revision). Geneva: Author.
Yorbik, O., Birmaher, B., Axelson, D., Williamson, D. E., & Ryan, N. D. (2004). Clinical characteristics of depressive symptoms in children and adolescents with major depressive disorder. Journal of Clinical Psychiatry, 65, 1654–1659.
Zlotnick, C., Donaldson, D., Spirito, A., & Pearlstein, T. (1997). Affect regulation and suicide attempts in adolescent inpatients. Jounal of the American Academy of Child and Adolescent Psychiatry, 36, 793–798.
Zlotnick, C., Wolfsdorf, B. A., Johnson, B., & Spirito, A. (2003). Impaired self-regulation and suicidal behavior among adolescent and young adult psychiatric inpatients. Archives of Suicide Research, 7, 149–157.
Acknowledgements
Members of the International Consortium for Childhood-Onset Mood Disorders include: Ildikó Baji M.D., István Benák, Emília Kaczvinszky M.D., Krisztina Kapornai M.D., Viola Kothencné Osváth M.S., László Mayer M.D., Szeged University Medical Faculty, Department of Child and Adolescent Psychiatry, Szeged. Márta Besnyő M.D., Julia Gádoros M.D., Ph.D., Vadaskert Hospital, Budapest. Judit Székely M.D. Semmelweis University I. Pediatric Department, Budapest. Edit Dombovári M.D., Heim Pál Hospital for Sick Children Outpatient Unit of Child Psychiatry, Budapest. Special thanks are due to the following participating physicians across various research sites in Hungary: Zsuzsa Bánk M.D., Katalin Bense M.D., Katalin Benkő M.D., Ferenc Dicső M.D., Emőke Endreffy Ph.D., Edina Farkas M.D., Gyöngyi Farkas M.D., Zsuzsanna Fekete M.D., Márta Fohn M.D., Magdolna Gácser M.D., Eszter Gyenge M.D., Éva Gyulai M.D., Mária Gyurcsó M.D., Rózsa Hasuly M.D., Ágnes Horváth M.D., Enikő Juhász M.D., Mária Károlyfalvi M.D., Dénes Kövendy M.D., Mária Mojzes M.D., Ilona Mógor M.D., Róza Oláh M.D., Mária Palaczky M.D., Mária Révhelyi M.D., Ilona Riegler M.D., Zsuzsanna Sörföző, M.D., Péter Steiner M.D., Zsuzsa Takács M.D. and Mariann Vados M.D, and to Charles J. George, MS, for his statistical comments on an earlier version of this manuscript.
This work was supported by Program Project Grant #MH056193 from the National Institute of Mental Health, HHS, Washington, D.C.
Disclosure
The Children’s Depression Inventory and the Feelings and Me Scales are published by MultiHealth Systems, Inc., from which Dr. Kovacs receives royalties.
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Tamás, Z., Kovacs, M., Gentzler, A.L. et al. The Relations of Temperament and Emotion Self-regulation with Suicidal Behaviors in a Clinical Sample of Depressed Children in Hungary. J Abnorm Child Psychol 35, 640–652 (2007). https://doi.org/10.1007/s10802-007-9119-2
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s10802-007-9119-2