Abstract
Purpose
Smaller pupil size under binocular conditions could justify partially the improvement of visual performance when compared to monocular conditions. The purpose of this study was to assess the binocular summation for increasing levels of spherical and cylindrical defocus when the pupil size factor is ruled out as a confounding factor.
Methods
Fifteen young subjects were recruited in this crossover study. Light disturbance index (LDI) was evaluated with the light disturbance analyzer and low (LCDVA) and high (HCDVA) contrast visual acuity with the ETDRS test. Two positive spherical and cylindrical defocus levels (+ 1.5 and + 3.0 D) were used to induce a controlled degradation of the retinal image for two pupil sizes (3 and 5 mm).
Results
Our results showed poorer visual performance in monocular than the binocular condition. An increasing deterioration was observed with the level of spherical defocus. Positive binocular summation for visual acuity was found in all the parameters studied and was stronger under larger pupil size and for higher levels of spherical defocus. It was observed a positive binocular summation for the LDI under all the conditions studied. Strong and significant correlations were found between LDI and LCDVA and between LDI and HCDVA for all the conditions. Higher correlations were obtained between disturbance index and visual acuity for spherical defocus compared to cylindrical.
Conclusion
Binocular summation was observed under different conditions of spherical and cylindrical optical degradation of the image quality when the pupil size was fully controlled. This suggests that a neural factor is involved.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Normal binocular vision depends on a considerable number of optical and neural parameters [1]. One of these important parameters is the pupil size. Human visual performance depends strongly on pupil size, particularly in highly aberrated eyes [2,3,4,5], but also in healthy eyes [6,7,8]. Several physiological factors affect pupil size [9]: namely age [10], environmental lighting or visual complexity task among others [11, 12]. Pupil size also changes between monocular and binocular vision conditions being generally lower under binocular vision for the same age and environmental light. In healthy people, binocular sensitivity has been found to be higher compared to monocular sensitivity, due to binocular summation [13,14,15]. Nevertheless, an opposite effect (decrease) in the binocular summation was disclosed after corneal refractive surgery procedures such as LASIK [16, 17]. Binocular summation refers to the superiority of binocular vision performance over monocular vision performance [14, 15, 18, 19]. If this factor is above 1, there is a positive effect and, therefore, an enhancement on binocular condition compared to the best monocular condition [9, 14]. Moreover, this factor positively affects several metrics of visual performance, including improvements in visual acuity, contrast sensitivity [4, 11, 18, 20,21,22] and reduction of light disturbance [23]. Light disturbance is a photic phenomenon which includes some specific visual disturbances generally described as glare disability, starburst and halos. Regarding these visual disturbances, glare disability causes a reduction of visual performance due to a glare source. Starburst and halos can alter and degrade the object shape or size. Also, halos can occur with or without starbursts (radial or regular scattering of light from a point source) [24]. In fact, light disturbance is an important aspect to take into account in multifocal contact lenses [23] and intraocular implantation of multifocal intraocular lenses [25, 26]. Sabesan et al. [4] observed that binocular summation increases as contrast decreases under the conditions of high stimulus energies and low noise. Plainis et al. [20] investigated the effect of binocular summation in eyes undergoing deterioration of retinal-image quality with defocus and showed that binocular vision ameliorates the effect of retinal blur on spatial visual performance. Escandon-Garcia et al. [25] observed a 30% improvement in light disturbance under binocular compared to monocular conditions after multifocal IOL implantation. However, they did not control for potential changes of pupil size between binocular and monocular conditions. Therefore, it is unclear whether this improvement reflects a neural summation factor or simply an optical effect due to the improvement in optical quality by pupil reduction under binocular vision conditions.
With this in mind, the present study has been designed to assess the impact of pupil size on high and low contrast visual acuity and light disturbance in young healthy eyes undergoing different spherical and cylindrical defocus levels. Moreover, this study has investigated the binocular summation under different pupil size conditions, fixed for monocular and binocular conditions in order to eliminate the potential effect of pupil constriction. The study has also evaluated the potential correlations between visual acuity (psychophysical parameter) and light disturbance index (a psychophysical parameter which quantifies the light disturbance). This information will be used as reference for designing future studies involving these two metrics of visual performance. For example, it can be used in subjects with ocular disease, or in those undergoing optical or surgical visual correction. Also, it might be helpful for comparing with objective parameters.
Methods
Subjects
The inclusion criteria to participate on this crossover study were: only emmetropic or myopic subjects with a spherical refraction less than |− 3.0 D| and an astigmatism less than |− 1.0 D|, monocular and binocular visual acuity ≤ 0.00 (logMAR notation) with binocular visual acuity better than monocular ones, no ocular pathology or surgery and no pharmacological treatment which could affect their vision or pupil response. Additionally, all the subjects had to have a pupil diameter larger than five millimeters under the illumination conditions for the visual acuity optotype (illuminance of 170.27 ± 3.86 lx) and LDA (light disturbance analyzer) device (see Light Disturbance section for device description) allowing to standardize an artificial pupil size of 5 mm and 3 mm using artificial diaphragms (5 mm and 3 mm). A full eye examination for each participant was conducted including objective and subjective refraction using the endpoint criterion of maximum plus for the best visual acuity. A subjective refraction examination was checked (best monocular VA for each eye and corresponding best binocular balance). The pupil diameter was measured with the NeurOptics pupilometer (NeurOptics VIP TM- 200, California) which has been proved to have very good repeatability and high safety [27]. Pupil size was measured while the subject was looking at the light disturbance analyzer central light to ensure we measured the smaller pupil as a reference under this and the remaining test conditions (i.e., visual acuity measurement). Two positive spherical defocus levels (+ 1.5 and + 3.0 D) and two positive cylindrical defocus levels (+ 1.5 and + 3.0 D at 90°) were used to induce a controlled degradation of the retinal image. The order of defocus was random for the two pupil size conditions (5 and 3 mm) using artificial diaphragms at 12 mm from the corneal vertex on a trial frame. To obtain all the data, two sessions of one hour were required. In the first session, all the low (LCDVA) and high (HCDVA) contrast distance visual acuity measurements (parameters used to measure and assess visual acuity at different contrasts. See more description in the high and low contrast distance visual acuity section) were determined for the baseline and all the defocus levels (spherical and cylindrical) with the two pupil size conditions (5 and 3 mm). In the second session, all the LDI (light disturbance index, parameter used to measure and quantify the halo size. See more description in the light disturbance section) values were obtained for the two pupil size conditions and the different levels of defocus (spherical and cylindrical). Patients wore the best spectacle correction on trial frame for the evaluation distance. Following the Declaration of Helsinki, all patients were informed and carry out about the purpose of the study and all methods. All the subjects had the opportunity to clarify their doubts and sign an informed consent form before being enrolled in the study. So, the informed consent was obtained for all the participants. The study protocol was reviewed and approved by the Ethics Subcommittee for Life and Health Sciences of the University of Minho.
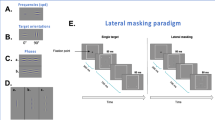
High and low contrast distance visual acuity
The best visual acuity with the ETDRS logMAR charts at a distance of 4 m under low contrast (LCDVA, 10%) and high contrast (HCDVA, 100%) conditions was measured. The measurements were obtained under a photopic illumination room condition: the luminance was 86.23 ± 1.75 cd/m2 and the illuminance was 170.27 ± 3.86 lx, measured with the Minolta LS-110 Luminance meter and the Minolta T10A Illuminance meter, respectively. The different defocus levels and pupil diameters were presented in a random order to avoid any learning effect to influence the results.
Light disturbance
In order to quantify light disturbance, the halometer called light disturbance analyzer (LDA, CEORLab, University of Minho, Braga, Portugal) was used. This device analyses the size and shape of the halo surrounding a bright light under dim illumination conditions. In practical terms, the test consisted of identifying a peripheral stimulus (small white LED ref. HSMW-CL25 from Avago Technologies, San Jose, California) around a central LED stimulus (white LED ref. HLMP-CW47-RU000 from Agilent Technologies, Inc., Berkshire, United Kingdom) under low-illumination conditions. The central LED is responsible for creating the glare condition while the surrounding LEDs are used as threshold discriminators at different positions and angular distances of the visual field [28]. So, the peripheral LEDs are only used to indicate the limits of the size of the halo caused by the central LED stimulus. This methodology is similar to other visual tests to quantify night-vision disturbances which use luminous stimuli around a central high-luminance stimulus to determine the halo size [29, 30]. The peripheral LEDs of the LDA are distributed in twenty-four semi-meridians with an angular separation of 15°. According to Linhares et al. [28] during the test, the central LED had a maximum luminance of 2800 cd/m2, and 6 cd/m2 for the surrounding LEDs, and therefore, the central high-luminance LED is responsible of the halo perception and, maintaining constant the luminance of the stimuli, the detection of the surrounding LEDs would allow to determine the shape and size of the halo or visual disturbance. The peripheral stimuli were presented randomly around the central LED from the inner to the outer part of the field at random times from 250 to 750 ms. The subject was placed at a distance of two meters from the center of the central LED stimulus under low-illumination surrounding conditions (illuminance of 0.91 ± 0.02 lx) and had to continuously maintain the fixation on the central LED stimulus. The subject has to press the mouse control button each time the peripheral stimulus is seen and the system presents the next semi-meridian. Three evaluations are performed in each semi-meridian before the instrument calculates the mean limit of the light distortion. If the standard deviation (SD) of the three evaluations in each semi-meridian is superior to 20%, the device automatically repeats the measurements in those semi-meridians until reach a SD inferior to 20%. At the end of the test, a map of the size of the light disturbance (halo) is obtained [31]. One main parameter evaluates the degree of these dysphotopsias: the light disturbance index (LDI). The LDI is calculated as the ratio of the area of the points missed by the subject and the total area explored: the higher the LDI, the higher the light disturbance induced by the central source of light and the lower the ability to discriminate surrounding small stimuli. This parameter is commonly used as a percentage in clinical studies using the same device [5, 23, 25, 26, 31], but it can be also expressed as the angular size of the halo radius from the observer position (in degrees or arc min). A LDI value of 100% corresponds to detect no one of the peripheral stimuli showed to the observer (a halo radius of 137.4 arc min from the observer position). In this work, the LDI is expressed as the radius of the halo from the observer position (in arc min).
Binocular summation
The binocular summation characterizes the binocular visual performance [4, 32, 33]. For the low and high contrast visual acuity, the binocular summation ratio \({\mathrm{BS}}_{\mathrm{VA}}\) was calculated using Eq. (1), dividing the binocular visual acuity \({, \mathrm{VA}}_{\mathrm{bin}},\) by the best monocular one, \({\mathrm{VA}}_{\mathrm{best}\_\mathrm{mon}}\) (the higher of the two monocular values). For this calculation, decimal visual acuities were used, which were previously obtained from the logMAR VA values.
Regarding the light disturbance parameter LDI (light disturbance index), the discrimination capacity increases when the LDI decreases. Therefore, the LDI binocular summation\(, {\mathrm{BS}}_{\mathrm{LDI}}\), was calculated using Eq. (2), dividing the lowest monocular value,\({\mathrm{LDI}}_{\mathrm{best}\_\mathrm{mon}},\) by the binocular LDI value\({\mathrm{LDI}}_{\mathrm{bin}}\). This calculation is in accordance with other authors who used an index comparable to the LDI [9].
A binocular summation ratio superior to 1 indicates a positive binocular summation showing that the vision is better binocularly compared to monocular conditions.
Statistical procedures
The statistical analysis was performed using SPSS 23.0 (SPSS Inc., Chicago, IL) for Windows. The normality was checked using the Shapiro–Wilk test (n = 15). In case of normal distribution, a t-test for two-sided alternatives was performed to compare each visual variable separately (LCDVA and HCDVA): right eye vs left eye, monocular vs binocular and pupil size 5 mm versus pupil size 3 mm. Similarly, Wilcoxon signed rank test (two-sided hypothesis tests) was used in the case of no normal distribution (LDI). Repeated measures ANOVA with Bonferroni correction were used for LCDVA and HCDVA parameters and the multiple comparisons between baseline, defocus and pupil sizes. Alike, in case of non-parametric nature of the data, Friedman test with post-hoc correction was used for LDI and the multiple comparisons between baseline, defocus and pupil sizes. Degree of freedom shortened in DF. Therefore, in case of normality, Pearson correlation (Pearson R) was performed to find the relationship between defocus and visual acuity. Spearman correlation (Spearman R) was made to find the relationship between light disturbance parameters and visual acuity (LCDVA and HCDVA). Differences were considered statistically significant when the p value was lower than 0.05.
Results
Subjects
A total of 15 young subjects (11 females, 4 males) were recruited in this crossover study. The mean age was 28.5 ± 7.7 years. Table 1 shows mean refractive error of the participants as well as their mean pupil size under natural conditions but also under the LDA measurement conditions.
High and low contrast distance visual acuity
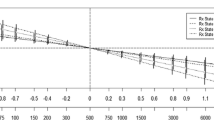
Figure 1 shows the mean values of the low contrast distance visual acuity (LCDVA), monocularly and binocularly, under the different defocus conditions studied and for the two pupil diameters (3 and 5 mm). No significant differences between right and left eye in all measuring conditions (spherical and cylindrical defocus, and pupil sizes) were found (t(14) = − 1.431, p = 0.174) Nevertheless, all the LCDVA monocular parameters were found to be significantly higher than the binocular ones in all measuring conditions (t(14) = 2.654, p = 0.019), which indicates a poorer visual performance in logMAR scale. The pupil size of 5 mm showed a statistically significant deterioration compared to the pupil size 3 mm in all measuring conditions (t(14) = 2.529, p = 0.024). With spherical defocus and pupil size of 5 mm condition, a statistically significant deterioration in LCDVA was found proportionally with the amount of defocus. Monocularly, for each amount of + 1.5 D, a deterioration of 0.53 logMAR in LCDVA (Pearson R = 0.999, p ˂ 0.001) was disclosed (\({F}_{\mathrm{1,14}}\)= 100.870, p < 0.001). Similarly, in the binocular condition (pupil size of 5 mm), a statistically significant deterioration (\({F}_{\mathrm{1,14}}\)= 104.334, p < 0.001) was showed with increasing the spherical defocus (Pearson R = 0.999, p < 0.001). A deterioration of 0.41 logMAR on average between baseline and spherical defocus of + 1.5 D and a mean value deterioration of 0.47 logMAR between spherical defocus of + 1.5 and + 3.0 D were found. Likewise, with the pupil size of 3 mm, monocularly and binocularly, a statistical significant deterioration (\({F}_{\mathrm{1,14}}\)= 106,258, p < 0.001) was found proportionally with the amount of defocus (Pearson R = 0.999, p < 0.001).
Average and standard deviation values of logMAR distance visual acuity for low contrast (LCDVA) under spherical (+ 1.5 and + 3.0 D) and cylindrical defocus (+ 1.5 D at 90° and + 3.0 D at 90°) for 3 and 5 mm (mm) pupil size condition (n = 15). Baseline data (no defocus) are included. Error bars represent standard deviation
Similarly, results showed a statistically significant deterioration of LCDVA inducing cylindrical defocus compared with baseline measurements. Monocularly, for the pupil size of 5 mm, a degradation was shown for cylindrical defocus condition, with a minimum mean difference of 0.32 logMAR between baseline and + 1.5 D (\({F}_{\mathrm{1,14}}\)= 151.874, p < 0.001) and of 0.33 logMAR between + 1.5 D and + 3.0 D of cylindrical defocus (\({F}_{\mathrm{1,14}}\)= 122.263 p < 0.001). Similar results were obtained binocularly: an average LCDVA deterioration for cylindrical defocus condition with a mean difference of 0.31 logMAR between baseline and + 1.5 D (\({F}_{\mathrm{1,14}}\)= 157.118, p < 0.001) and a mean difference of 0.28 logMAR between + 1.5 D and + 3.0 D of cylindrical defocus (\({F}_{\mathrm{1,14}}\)= 115.126, p < 0.001). As a result, a strong correlation was demonstrated between cylindrical defocus and LCDVA (Pearson R = 0.999, p ˂ 0.001) for the 5 mm pupil.
For the pupil size of 3 mm, significant deteriorations of LCDVA were also found for cylindrical defocus condition under monocular viewing for both comparisons: a mean difference of 0.29 logMAR between baseline and + 1.5 D (\({F}_{\mathrm{1,14}}\)= 163.348 p < 0.001) and a mean difference of 0.30 logMAR between + 1.5 D and + 3.0 D of cylindrical defocus (\({F}_{\mathrm{1,14}}\)= 128.986, p < 0.001). Binocularly, average LCDVA deteriorations were also obtained, with a mean difference of 0.29 logMAR between baseline and + 1.5 D (\({F}_{\mathrm{1,14}}\)= 128.986, p < 0.001) and a mean difference of 0.25 logMAR between + 1.5 and + 3.0 D of cylindrical defocus (\({F}_{\mathrm{1,14}}\)= 115.126, p < 0.001). As a result, a strong correlation was demonstrated between cylindrical defocus and LCDVA (Pearson R = 0.999, p < 0.001) for the smallest pupil.
Figure 2 shows mean values for the high contrast distance visual acuity (HCDVA) under the different conditions tested (spherical and cylindrical defocus and the two pupil sizes of 3 and 5 mm). No statistically significant differences were found between left and right eye in all the conditions (t(14) = − 1.076, p = 0.300). A strong correlation between defocus (spherical and cylindrical) and HCDVA (Pearson R = 0.999) was demonstrated. All the binocular mean values were statistically better than the monocular ones (t(14) = 3.351, p = 0.005). Comparing pupil size between 5 and 3 mm, the HCDVA mean values were significantly better for the 3 mm pupil (t(14) = 2.377, p = 0.032 for baseline; t(14) = 3.489, p = 0.004 for spherical conditions and t(14) = 2.504, p = 0.025 for cylindrical defocus) in all the conditions (spherical and cylindrical defocus, monocularly and binocularly) except binocularly for the baseline where differences were no significant (− 0.20 ± 0.07 logMAR for the 5 mm and − 0.21 ± 0.07 logMAR for the 3 mm pupil, t(14) = 1.522, p = 0.150).
Average and standard deviation values of logMAR distance visual acuity for high contrast (HCDVA) under spherical (+ 1.5 D and + 3.0 D) and cylindrical defocus (+ 1.5 D at 90° and + 3.0 D at 90°) for 3 and 5 mm (mm) pupil size condition (n = 15). Baseline data (no defocus) are included. Error bars represent standard deviation
Table 2 shows the mean values of the binocular summation for the visual acuities studied (LCDVA and HCDVA). In all conditions, a positive binocular summation was obtained: the mean binocular summation was higher than 1, highlighting the superiority of binocular visual system compared with the monocular one. Therefore, the binocular visual acuity was better than the best monocular one. As a result, for the LCDVA, it was observed that the binocular summation increased significantly under larger pupil size in all the conditions (t(14) = 2.538, p = 0.024 for baseline; t(14) = 5.641, p = 0.001 for spherical and t(14) = 3.388, p = 0.004 for cylindrical) and, furthermore, higher level of spherical defocus was achieved.
For the HCDVA, the binocular summation increased significantly with pupil size for the + 1.5 D spherical defocus (t(14) = 2.473, p = 0.027) and for the + 3.0 D cylindrical defocus (t(14) = 2.282, p = 0.039). In the other conditions, binocular summation showed a tendency to improve with larger pupil but with no significant differences (t(14) = 1.470, p = 0.164 for baseline; t(14) = 0.612, p = 0.550 for + 3.0D spherical defocus; and t(14) = 0.930, p = 0.368 for + 1.5D cylindrical defocus).
Light disturbance
Figure 3 shows the mean values of the LDI (radius, in minutes of arc) under spherical and cylindrical defocus and the two pupil sizes studied (5 and 3 mm). There were no significant differences between right eye and left eye for all the conditions measured (with a minimum of Z value = − 1.59, DF = 14, p = 0.11 for + 3.0 cylindrical). The binocular LDI values asserted a statistically significant difference compared to the same condition monocularly (with of a minimum Z value = 2.31, DF = 14, p = 0.02 for baseline) except for the comparison of the LDI monocular baseline with the binocular LDI baseline under the 3 mm pupil condition, with no significant difference (Z value = 1.385, DF = 14, p = 0.17) and neither did the binocular LDI with a spherical defocus of + 1.5 D comparing left eye with binocular condition (Z value = 1.61, DF = 14, p = 0.11). As a result, the binocular LDI values were lower than the monocular ones for the pupil sizes analyzed, with a significant difference in the most of conditions. Therefore, under monocular conditions, the light disturbance was stronger.
Comparing pupil size between 5 and 3 mm, LDI mean values were significantly better for the 3 mm pupil for spherical defocus of + 3.0D (monocularly, Z value = − 2.04, DF = 14, p = 0.04; Binocularly, Z value = − 2.84, DF = 14, p = 0.005) and both cylindrical defocus binocularly (Z value = − 2.53, DF = 14, p = 0.01).
For both pupil size conditions, the monocular and binocular LDI values increased significantly with spherical and cylindrical defocus (Z value = 3.11, DF = 14, p = 0.002). In fact, the LDI proportionally worsened with defocus, showing a stronger effect of the light disturbance on halo perception. With the amount of defocus, the LDI was more deteriorated monocularly than binocularly with statistically significant differences.
Table 3 shows a positive binocular summation effect of the LDI for all the experimental conditions. So, the best values were obtained binocularly compared to monocularly (best monocular value of the two eyes). We found no statistically significant differences between 5 mm pupil size and 3 mm pupil size conditions (t(14) = 0.429, p = 0.675). Only for the + 3.0D spherical defocus, the binocular summation disclosed a statistically significant difference (t(14) = − 2.516, p = 0.025) between 5 mm pupil size and 3 mm pupil size. Finally, no statistically significant differences between the different defocus conditions and pupil size conditions (with of a minimum Z value = − 1.48, DF = 14, p = 0.14 between + 1.5 cylindrical and + 3.0D cylindrical for pupil diameter of 3 mm) were reported.
Correlations
Table 4 shows high statistically significant correlations (p < 0.001) between LDI and LCDVA, but also between LDI and HCDVA for all the conditions (defocus and pupil size). Higher coefficient correlations were reported monocularly respect to binocularly in all the conditions. The highest correlations (Spearman R > 0.86) were obtained with spherical defocus respect to cylindrical defocus between LDI (a psychophysical parameter) and LCDVA (a visual subjective parameter), but also between LDI and HCDVA (Spearman R > 0.85). The pupil size conditions did not show significant differences (p > 0.05) comparing their results with the same amount of defocus.
Discussion
The main purpose of the study was to investigate the potential role of the pupil size and defocus on binocular summation for high and low contrast visual acuity and light disturbance metrics. A group of healthy and young subjects was chosen because the factor of age is an important factor which could influence the results of binocular summation [10, 32]. The present study shows that binocular summation in healthy and non-surgical patients is consistent under controlled pupil size conditions. In fact, this study has corroborated that might involve essentially a neural factor and not an optical factor because it is not just the result from the expected pupil size reduction under binocular conditions and the quality of the optics forming the retinal image but it could be the ability of the visual cortex to resolve the details of that [1, 20, 34, 35].
The control of the pupil size in this study allowed eliminating one important source of interindividual variability. The factor of the pupil size was controlled for two different visual functions: the visual acuity by means of the LCDVA and the HCDVA and the light disturbance by means of the LDI (psychophysical parameters). That’s why the effect of binocular summation was investigated in low and high contrast distance visual acuity and during the light disturbance phenomena under positive spherical and cylindrical defocus.
Firstly, the binocular performance under photopic conditions was analyzed by measuring the low and high contrast visual acuity. The results indicated a strong enhancement of the binocular summation with increased defocus [36]. The best binocular visual acuity values were found statistically better in all the levels of defocus for the 3 mm pupil size compared to the 5 mm pupil size except for the binocular baseline condition. This result could be explained for the high threshold achieved in baseline binocular viewing. Nevertheless, the binocular summation was found to be stronger for the 5 mm pupil size in photopic conditions. Moreover, a better binocular summation was achieved in low and high contrast visual acuity with higher spherical defocus compared with baseline and other conditions of cylindrical defocus. As reported by Plainis et al. [20], a higher binocular summation was found in a group of young subjects (i.e., same age mean value) with higher spherical defocus and lower binocular summation for natural condition but not at the same distance for visual acuity (i.e., 1 m compared with 4 m in the present research). Also, they have demonstrated that binocular vision improved with the effects of retinal blur on spatial visual performance, but the study was limited since no control of the pupil size was set. These results suggested that the binocular summation for visual acuity task was stronger when the amount of positive defocus increased. Similarly, in the present study, stronger binocular advantages were found for a high level of defocus (+ 3.0D), but also for a lower level of defocus (+ 1.5D). In the same manner, for higher spherical defocus where the retinal blur is the most relevant, the present results corroborated that the binocular summation increased for low and high contrast visual acuity [1, 34, 37, 38] (for + 3.0D spherical, LCDVA: 1.99 ± 0.59 and HCDVA: 1.47 ± 0.39). Banton and Levy [39] found that the binocular superiority for low contrast stimuli has also been shown in Vernier acuity. They suggested that in higher contrasts the binocular advantage diminishes due to saturation. Others studies also confirmed higher binocular summation in contrast using masking experiments (studying neural correlates of consciousness and spatiotemporal limits of visual discrimination) [40, 41]. Correspondingly, the increased binocular summation observed with retinal blur may be due to the activation of a larger population of neurons at close-to-threshold detection meaning that less contrast was required under binocular than under monocular stimulation to obtain the same proportion of cells that contribute to contrast detection [20, 42]. In another study, Castro et al. [9] showed significant differences in contrast sensitivity and visual discrimination between monocular and binocular conditions inducing anisocoria and positive defocus. Due to the interocular differences, they found a deterioration of the binocular summation for the contrast sensitivity function (CSF) after inducing different levels of anisocoria compared with natural conditions. Similar results were found for the visual discrimination index, a parameter which is similar to the LDI, since quantifies the perception of halos [9]. The present study shows that controlling the pupil size, and avoiding any anisocoria, higher positive defocus is associated to superior binocular summation effects on visual acuity (LCDVA and HCDVA). In other words, binocular summation mechanism provides stronger feedback as the monocular image quality of each eye deteriorates further.
Secondly, the light disturbance phenomenon was measured, by means of the LDI, for different defocus and control pupil size conditions. Under such luminance condition, a better binocular performance was corroborated compared to monocular condition as well as an improvement of the binocular summation when the retinal image was further deteriorated. The binocular summations in the LDI were lower compared with the visual acuity. Recently, Amorim et al. [43] found higher light disturbance values in monocular compared to binocular conditions with positive and negative defocus of + 1.0D and cycloplegia in young health subject. However, they did not control the pupil size changes between monocular and binocular conditions. Ferreira-Neves [31] et al. showed that changing the pupil size from 3 to 6 mm did not have a significant impact on light disturbance in healthy subjects under pharmacologically induced mydriasis with 1% phenylephrine. They showed that the role of the pupil size as a main contributor to light disturbances is not so evident. Moreover, Villa et al. [44] found a moderate but not significant positive correlation between the pupil size and the magnitude of the light disturbances in eyes undergoing myopic laser-assisted in situ keratomileusis (LASIK) surgery. The present study did not find statistically significant gain in the binocular summation for the LDI depending on the pupil size except for the highest spherical defocus (better with the pupil size of 3 mm). Other works have shown this trend monocularly and binocularly but using a different device [9]. They found a moderate increase in visual disturbance as pupil size increases, comparing artificial pupils of 2, 3 and 4 mm, but with no significant differences. Such differences were justified by a deterioration of the retinal-image quality with pupil size. However, the visual disturbances were significantly greater with natural pupils (mean diameter of 6.5 mm) compared to the artificial ones, showing a stronger effect when large differences in pupil sizes were compared.
Comparing with the results obtained by Escandon-Garcia et al. [25] in pseudophakic subjects (a mean HCDVA of − 0.16 ± 0.27 logMAR; and a mean LDI of 34.6 ± 16.0%, equivalent to a mean halo radius of about 47.6 arc min), the present results show lower values for light disturbance and high contrast distance visual acuity, which is probably due to the fact that the pupil size was controlled.
Macedo-de-Araujo et al. [5] investigated the effect of positive and negative spherical aberration on the light disturbance. They corroborated that light disturbance is sensitive to changes in image quality caused by modifications in spherical aberrations and that accommodation and pupillary constriction are capable of compensating the degradation of the optical quality induced. However, that study did not control the pupil size and did not measure under monocular and binocular conditions so the combined effect of induced spherical aberration and pupil size as well as binocular summation was not investigated.
Finally, the present results have shown strong correlations (Spearman R > 0.85) between visual acuity and LDI (psychophysical parameters). Hence, the binocularly and monocularly (worst eye) best correlations were obtained with spherical positive defocus (inducing myopia) independently of the pupil size conditions. More specifically, the best correlations were obtained for a 5 mm pupil size.
The influence of the accommodation was controlled for young and healthy subjects inducing myopia by defocus. Furthermore, in baseline condition, neither of the subjects recruited had hyperopia. During all our visual measurements, no statistically significant differences were observed between the two eyes of all the subjects and all the conditions measured. In fact, it is known that the interocular differences influence the binocular summation for different visual functions, such as contrast sensitivity or visual discrimination capacity under low-illumination conditions [4, 9].
Limitations of this study include that actual pupil size was not measured during visual acuity and light disturbance evaluation. However, after measuring the pupil with an infrared pupilometer in dim surrounding conditions with the only illumination given mainly by the central LED in the LDA device without trial frame, it is expected that the actual pupil size “behind” the artificial pupil diaphragm would be always larger and not smaller than the reference measurement. The illuminance reaching the eye under light disturbance measurements is lower (0.91 ± 0.02 lx) than for the remaining test conditions to measure visual acuity (170.27 ± 3.86 lx). Even for LDA examination, when the eye is behind the artificial diaphragm to control the aperture during the experiments, the illuminance will be lower and the pupil size expectedly larger. Thought we could not measure the true pupil size during the experiments (behind the artificial diaphragm), it seems reasonable to assume that actual pupil size during experiments is larger than that measured as control with the infrared pupilometer during LDA exposure. Consequently, we should also assume that the artificial pupil at 12 mm is in fact the limiting aperture (3 and 5 mm pupil). During the measurements of the LDI under defocusing conditions, the subjects see a defocused image of the central and peripheral LEDs. This situation corresponds to a similar situation when the subject is in real life trying to discriminate sources of light around a central light source that generates the glare effect. In addition, the LDA device uses a patient response type of testing which could be affected by subjective cognitive capacity. However, to limit it, the peripheral stimuli were presented randomly around the central LED and at random times. Another limitation could be the small number of participants in this study. Indeed, a higher number could allow a greater precision in our findings. However, this exploratory study demonstrated to be statistically powerful to test the hypothesis raised in the purpose of the study. Future studies with larger and more representative samples shall be conducted.
In summary, the present results confirm that under the conditions of this study, a positive binocular summation is observed with increasing levels of defocus (spherical and cylindrical) even when pupil size is kept constant. This confirms that beyond the eventual optical improvement due to stronger binocular pupil constriction, neural factors are involved in improving the binocular visual performance under challenging conditions of image quality degradation. This might be relevant for surgical or non-surgical visual correction techniques where residual refractive errors or deliberately uncorrected refractive errors are present. It is observed higher binocular summation with higher defocus and lower contrast induced in visual function. This confirms that under the effect of the defocus in combination with the two controlled pupil sizes, the binocular summation prevails and increases due to its neural factor (exceeding the optical effect) and not only to an optical one. Further investigation will be required to confirm the part of the neural factor of the binocular summation in the same conditions investigated. It is also confirmed a strong correlation monocularly and binocularly between LDI and visual acuity (especially with spherical defocus induced). This raises an interesting point that suggests light disturbance might be a candidate to psychophysical indicator of the visual potential involving a detection task rather than a recognition task as in the case of visual acuity where other factors such as literacy might influence the measures.
Data availability
The datasets generated during the current study are available from the corresponding author on reasonable request.
References
Campbell FW, Green DG (1965) Optical and retinal factors affecting visual resolution. J Physiol-Lond 181:576. https://doi.org/10.1113/jphysiol.1965.sp007784
Xu RF, Kollbaum P, Thibos L, Lopez-Gil N, Bradley A (2018) Reducing starbursts in highly aberrated eyes with pupil miosis. Ophthalmic Physiol Opt 38:26–36. https://doi.org/10.1111/opo.12420
Bonaque-Gonzalez S, Rios-Rodriguez S, Lopez-Gil N (2016) Improving vision by pupil masking. Biomed Opt Express 7:2538–2550. https://doi.org/10.1364/boe.7.002538
Sabesan R, Zheleznyak L, Yoon G (2012) Binocular visual performance and summation after correcting higher order aberrations. Biomed Opt Express. https://doi.org/10.1364/boe.3.003176
Macedo-de-Araujo R, Ferreira-Neves H, Rico-del-Viejo L, Peixoto-de-Matos SC, Gonzalez-Meljome JM (2016) Light distortion and spherical aberration for the accommodating and nonaccommodating eye. J Biomed Opt. https://doi.org/10.1117/1.jbo.21.7.075003
Thibos LN, Bradley A, Hong X (2002) A statistical model of the aberration structure of normal, well-corrected eyes. Ophthalmic Physiol Opt 22:427–433. https://doi.org/10.1046/j.1475-1313.2002.00059.x
Mello GR, Rocha KM, Santhiago MR, Smadja D, Krueger RR (2012) Applications of wavefront technology. J Cataract Refract Surg 38:1671–1683. https://doi.org/10.1016/j.jcrs.2012.07.004
Plainis S, Ntzilepis G, Atchison DA, Charman WN (2013) Through-focus performance with multifocal contact lenses: effect of binocularity, pupil diameter and inherent ocular aberrations. Ophthalmic Physiol Opt 33:42–50. https://doi.org/10.1111/opo.12004
Castro JJ, Soler M, Ortiz C, Jimenez JR, Anera RG (2016) Binocular summation and visual function with induced anisocoria and monovision. Biomed Opt Express 7:4250–4262. https://doi.org/10.1364/boe.7.004250
Ross JE, Clarke DD, Bron AJ (1985) Effect of age on contrast sensitivity function: uniocular and binocular findings. Br J Ophthalmol 69:51–56. https://doi.org/10.1136/bjo.69.1.51
Frisen L, Lindblom B (1988) Binocular summation in humans: evidence for a hierarchic model. J Physiol-Lond 402:773–782. https://doi.org/10.1113/jphysiol.1988.sp017233
Medina JM, Jimenez JR, del Barco LJ (2003) The effect of pupil size on binocular summation at suprathreshold conditions. Curr Eye Res 26:327–334. https://doi.org/10.1076/ceyr.26.5.327.15434
Eysteinsson T, Barris MC, Denny N, Frumkes TE (1993) Tonic interocular suppression, binocular summation, and the visual-evoked potential. Invest Ophthalmol Vis Sci 34:2443–2448
Heravian JS, Jenkins TCA, Douthwaite WA (1990) Binocular summation in visually evoked-responses and visual-acuity. Ophthalmic Physiol Opt 10:257–261. https://doi.org/10.1016/0275-5408(90)90008-m
Tyler CW, Apkarian PA (1985) Effects of contrast, orientation and binocularity in the pattern evoked-potential. Vis Res 25:755–766. https://doi.org/10.1016/0042-6989(85)90183-x
Ramon Jimenez J, Villa C, Gonzalez Anera R, Gutierrez R, Jimenez del Barco L (2006) Binocular visual performance after LASIK. J Refract Surg 22:679–688
Villa C, Jimenez JR, Anera RG, Gutierrez R, Hita E (2009) Visual performance after LASIK for a Q-optimized and a standard ablation algorithm. Appl Opt 48:5741–5747. https://doi.org/10.1364/ao.48.005741
Blake R, Sloane M, Fox R (1981) Further developments in binocular summation. Percept Psychophys 30:266–276. https://doi.org/10.3758/bf03214282
Campbell FW, Green DG (1965) Monocular versus binocular visual acuity. Nature 208:191–192. https://doi.org/10.1038/208191a0
Plainis S, Petratou D, Giannakopoulou T, Atchison DA, Tsilimbaris MK (2011) Binocular summation improves performance to defocus-induced blur. Invest Ophthalmol Vis Sci 52:2784–2789. https://doi.org/10.1167/iovs.10-6545
Weeber HA, Featherstone KA, Piers PA (2010) Population-based visual acuity in the presence of defocus well predicted by classical theory. J Biomed Opt. https://doi.org/10.1117/1.3475956
Schwarz C, Manzanera S, Artal P (2014) Binocular visual performance with aberration correction as a function of light level. J Vis. https://doi.org/10.1167/14.14.6
Fernandes P, Amorim-de-Sousa A, Queiros A, Escandon-Garcia S, McAlinden C, Gonzalez-Meijome JM (2018) Light disturbance with multifocal contact lens and monovision for presbyopia. Contact Lens Anterior Eye : J Br Contact Lens Assoc. https://doi.org/10.1016/j.clae.2018.03.006
Fan-Paul NI, Li J, Miller JS, Florakis GJ (2002) Night vision disturbances after corneal refractive surgery. Surv Ophthalmol 47:533–546. https://doi.org/10.1016/s0039-6257(02)00350-8
Escandon-Garcia S, Ribeiro FJ, McAlinden C, Queiros A, Gonzalez-Meijome JM (2018) Through-focus vision performance and light disturbances of 3 new intraocular lenses for presbyopia correction. J Ophthalmol. https://doi.org/10.1155/2018/6165493
Brito P, Salgado-Borges J, Neves H, Gonzalez-Meijome J, Monteiro M (2015) Light-distortion analysis as a possible indicator of visual quality after refractive lens exchange with diffractive multifocal intraocular lenses. J Cataract Refract Surg 41:613–622. https://doi.org/10.1016/j.jcrs.2014.07.033
Schallenberg M, Bangre V, Steuhl K-P, Kremmer S, Selbach JM (2010) Comparison of the colvard, procyon, and neuroptics pupillometers for measuring pupil diameter under low ambient illumination. J Refract Surg 26:134–144. https://doi.org/10.3928/1081597x-20100121-09
Linhares JMM, Neves H, Lopes-Ferreira D, Faria-Ribeiro M, Peixoto-de-Matos SC, Gonzalez-Meijome JM (2013) Radiometric characterization of a novel LED array system for visual assessment. J Mod Opt 60:1136–1144. https://doi.org/10.1080/09500340.2013.842614
Castro JJ, Ortiz C, Pozo AM, Anera RG, Soler M (2014) A visual test based on a freeware software for quantifying and displaying night-vision disturbances: study in subjects after alcohol consumption. Theor Biol Med Model. https://doi.org/10.1186/1742-4682-11-s1-s1
Castro JJ, Pozo AM, Rubino M, Anera RG, Jimenez del Barco L (2014) Retinal-image quality and night-vision performance after alcohol consumption. J Ophthalmol. https://doi.org/10.1155/2014/704823
Ferreira-Neves H, Macedo-de-Araujo R, Rico-del-Viejo L, da-Silva AC, Queiros A, Gonzalez-Meljome JM (2015) Validation of a method to measure light distortion surrounding a source of glare. J Biomed Opt. https://doi.org/10.1117/1.jbo.20.7.075002
Pardhan S (1996) A comparison of binocular summation in young and older patients. Curr Eye Res 15:315–319. https://doi.org/10.3109/02713689609007626
Castro JJ, Jimenez JR, Hita E, Ortiz C (2009) Influence of interocular differences in the Strehl ratio on binocular summation. Ophthalmic Physiol Opt 29:370–374. https://doi.org/10.1111/j.1475-1313.2009.00643.x
Legge GE (1984) Binocular contrast summation.1. detection and discrimination. Vis Res 24:373–383. https://doi.org/10.1016/0042-6989(84)90063-4
Legge GE, Mullen KT, Woo GC, Campbell FW (1987) Tolerance to visual defocus. J Opt Soc Am A-Opt Image Sci Vis 4:851–863. https://doi.org/10.1364/josaa.4.000851
Atchison DA, Woods RL, Bradley A (1998) Predicting the effects of optical defocus on human contrast sensitivity. J Opt Soc Am A-Opt Image Sci Vis 15:2536–2544. https://doi.org/10.1364/josaa.15.002536
Home R (1978) Binocular summation: study of contrast sensitivity, visual-acuity and recognition. Vis Res 18:579–585. https://doi.org/10.1016/0042-6989(78)90206-7
Gagnon RWC, Kline DW (2003) Senescent effects on binocular summation for contrast sensitivity and spatial interval acuity. Curr Eye Res 27:315–321. https://doi.org/10.1076/ceyr.27.5.315.17225
Banton T, Levi DM (1991) Binocular summation in vernier acuity. J Opt Soc Am A-Opt Image Sci Vis 8:673–680. https://doi.org/10.1364/josaa.8.000673
Meese TS, Georgeson MA, Baker DH (2006) Binocular contrast vision at and above threshold. J Vis 6:1224–1243. https://doi.org/10.1167/6.11.7
Baker DH, Meese TS, Georgeson MA (2007) Binocular interaction: contrast matching and contrast discrimination are predicted by the same model. Spat Vis 20:397–413. https://doi.org/10.1163/156856807781503622
Anzai A, Bearse MA, Freeman RD, Cai DQ (1995) Contrast coding by cells in the cats striate cortex - monocular vs binocular detection. Vis Neurosci 12:77–93. https://doi.org/10.1017/s0952523800007331
Amorim-de-Sousa A, Macedo-de-Araujo R, Fernandes P, Queiros A, Gonzalez-Meijome JM (2019) Impact of defocus and high-order aberrations on light disturbance measurements. J Ophthalmol. https://doi.org/10.1155/2019/2874036
Villa C, Gutierrez R, Jimenez JR, Gonzalez-Meijome JM (2007) Night vision disturbances after successful LASIK surgery. Br J Ophthalmol 91:1031–1037. https://doi.org/10.1136/bjo.2006.110874
Funding
This study has been funded by projects PTDC/SAU-BEB/098391/2008, PTDC/FIS-OPT/0677/2014 and UID/FIS/04650/2019 funded by the Portuguese Fundação para a Ciência e Tecnologia (FCT).
Author information
Authors and Affiliations
Contributions
FM contributed on the design of the study, the acquisition, the analysis and the interpretation of data, drafted the article and approved the final version to be published. AFPM contributed on the acquisition of data, revised and approved the final version to be published. AAS carried out the acquisition of data, revised and approved the final version to be published. JJCT designed the figures, analyzed and interpreted the data and revised and approved the final version to be published. JMGM contributed on the conception and the design of the study, revised the article, approved the final version to be published and was responsible of the funding for this study.
Corresponding author
Ethics declarations
Conflict of interest
The authors declare that they have no conflicts of interest. Also, the authors have no relevant financial or non-financial interests to disclose. José Manuel González Méijome has a proprietary interest in the LDA device. Other authors declare that they do not have any proprietary or financial interest in any of the materials mentioned in this article.
Ethical approval and informed consent
Following the Declaration of Helsinki (World Medical Declaration of Helsinki, 2001), all patients were informed and carry out about the purpose of the study and all methods. All the subjects had the opportunity to clarify their doubts and sign an informed consent form before being enrolled in the study. So, the informed consent was obtained for all the participants. The study protocol was reviewed and approved by the Ethics Subcommittee for Life and Health Sciences of the University of Minho.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Springer Nature or its licensor (e.g. a society or other partner) holds exclusive rights to this article under a publishing agreement with the author(s) or other rightsholder(s); author self-archiving of the accepted manuscript version of this article is solely governed by the terms of such publishing agreement and applicable law.
About this article
Cite this article
Martino, F., Pereira-da-Mota, A.F., Amorim-de-Sousa, A. et al. Pupil size effect on binocular summation for visual acuity and light disturbance. Int Ophthalmol 43, 2183–2195 (2023). https://doi.org/10.1007/s10792-022-02614-w
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s10792-022-02614-w