Abstract
Introduction
Higher preoperative myopic astigmatism is associated with a higher probability of retreatment due to patient dissatisfaction as a result of residual cylindrical error. Nonetheless, retreatment is safe and the final clinical results are comparable to those of patients with lower preoperative astigmatism who were satisfied with the primary treatment. Our purpose is to compare the efficacy and safety of femtosecond LASIK (FS-LASIK) for the refractive correction of patients with low (< 1.5 Diopters (D) versus high (≥ 1.5 D) myopic astigmatism.
Methods
Retrospective observational study of 841 eyes of 825 eligible patients treated with FSLASIK for the correction of simple or compound myopic astigmatism. Outcome measures included residual error, best corrected and uncorrected distance visual acuity (BCVA and UCVA), efficacy and safety 3 months after the primary procedure or the retreatment.
Results
Of 841 eyes in total, 432 (51.37%) had < 1.5 D (Group 1) and 409 (48.63%) had ≥ 1.5 D (Group 2) preoperative myopic astigmatism. The efficacy index of primary treatment was 0.94 ± 0.18 in Group 1 and 0.89 ± 0.22 in Group 2 (P = 0.001). Of 138 eyes (16.41%) that were retreated due to dis-satisfaction related to residual refractive error, 28 belonged to Group 1 (6.5%) and 110 (26.9%) to Group 2 (P < 0.001). Following retreatment, small but statistically significant differences in the residual mean postoperative cylinder (−0.08 ± 0.24 vs −0.27 ± 0.46 D, P = 0.001) and UCVA (1.11 vs 0.96, P = 0.0001) were detected for Groups 1 and 2, respectively. However, there were no statistically significant differences in the safety and efficacy indices.
Conclusion
Following FS-LASIK, eyes with myopic astigmatism ≥ 1.5 D have approximately four times more chances of undergoing retreatment due to dis-satisfaction caused by residual refractive error compared to eyes with myopic astigmatism < 1.5 D. However, the clinical results after retreatment are highly satisfactory and comparable in both groups.
Similar content being viewed by others
Explore related subjects
Discover the latest articles, news and stories from top researchers in related subjects.Avoid common mistakes on your manuscript.
Introduction
Femtosecond LASIK (FS-LASIK) is a variation of LASIK, in which a Femtosecond laser is used to cut a thin corneal flap with an intended thickness of 90–110 μm [1]. The technique has gained widespread popularity as it combines a number of attractive characteristics. Compared to a mechanical microkeratome, the femtosecond LASIK is more precise (i.e., small difference of intended vs achieved) and more accurate (i.e., reduced variability) in terms of flap thickness [2,3,4]. Residual stromal thickness is an important determinant of postoperative LASIK safety. By creating a predictably thin flap, FS-LASIK can ensure a thicker remaining stromal bed so that the risk of post-LASIK ectasia is decreased. As a consequence, a better margin of safety is possible especially when the correction of higher refractive errors is attempted [5]. The fact that FS-LASIK allows for greater residual stromal thickness may be of particular clinical relevance in eyes with high preoperative cylindrical error. It is accepted that in these cases the physician should carefully evaluate the corneal topography, because the presence of an asymmetric bowtie, inferior steepening or skewed radial axis patterns are well-known risk factors for ectasia [6].
In addition to benefits related to the lower risk of postoperative LASIK-induced ectasia, a qualitative advantage of the homogenously thin femtosecond-created corneal flap is the induction of fewer higher order aberrations compared to a microkeratome-created flap [7]. Besides, in contrast to corneal biomechanical changes observed with a mechanical microkeratome, the alterations induced with a femtosecond laser are more predictable and exhibit a stronger correlation with ablation depth [8]. Clinically, the superior qualitative characteristics of femtosecond-created flaps may translate into higher predictability and better refractive outcomes [9]. In fact, previous work has shown that patients who underwent FS-LASIK had better refractive results than those who underwent LASIK with a microkeratome-created flap for the correction of mild to moderate hyperopia [10]. Given the fact that the role of FS-LASIK in astigmatism correction has not been analyzed in depth yet, was decided to compare the predictability of this technique in the correction of low versus high myopic astigmatism.
Methods
This was a single-center, retrospective chart review study that included eyes of consecutive eligible patients who underwent FS-LASIK for the correction of simple or compound myopic astigmatism at the Vissum Ophthalmic Institute, Madrid, Spain between the years 2007 and 2011. Institutional review board approval was obtained by a regional ethics committee. The exclusion criteria were as follows: history of glaucoma or retinal detachment, corneal disease, previous corneal or intraocular surgery, macular degeneration or retinopathy, any neuro-ophthalmic disease, previous complicated ophthalmic surgery or postoperative macular oedema, and history or signs of ocular inflammation. Eyes that were intentionally undertreated or needed retreatment for reasons other than residual refractive error such as epithelial ingrowth, flap striae, or diffuse lamellar keratitis were excluded.
The same experienced surgeon (MAT) performed all FS-LASIK procedures using the IntraLase 60-kHz femtosecond laser (IntraLase Corp, Irvine, CA, USA) with an intended flap thickness of 100 μm. The ablation was performed with an Esiris excimer laser (Schwind, Kleinostheim, Germany) in all cases. The follow-up visits were at 1 day, 1 week, and then 1, 3 and 6 months postoperatively. All patients received the same postoperative medication regimen of topical fluorometholone 1 mg/ml and ciprofloxacin 3 mg/ml, each instilled four times daily for 7 days.
At the baseline preoperative visit, an optometrist and the surgeon performed a complete ophthalmic examination that included manifest refraction, distance uncorrected visual acuity (UCVA), distance best corrected visual acuity (BCVA), automated refraction and keratometry (Topcon KR-800 autorefractometer, Tokyo, Japan), slit-lamp biomicroscopy, Goldmann applanation tonometry, corneal topography (CSO, Compagnia Strumenti Oftalmici, Florence, Italy), corneal pachymetry (DGH 5100 contact pachymeter, DGH Technology Inc, Exton, PA) and binocular indirect ophthalmoscopy through a dilated pupil. The same examiners performed a complete ophthalmic evaluation at the 3-month postoperative visit. Visual acuity was determined with Snellen decimal optotypes and converted to LogMAR notation for the statistical analysis, however, for clarity of presentation, all visual acuity data is shown in decimal notation. The cumulative average visual acuity values were calculated using the LogMAR notation. Refractive astigmatism was expressed as a negative value.
Refractive measurements were taken objectively using the autorefractometer. Subjective refractions were performed using the phoropter at a nominal vertex distance of 13.75 mm with the corneal vertex located at the large mark on the calibration scale [11].
The criterion for retreatment was residual correctable refractive error causing the patient to be dissatisfied with the uncorrected vision at 3 months postoperatively, after the stability of the postoperative refraction had been confirmed. Exclusion criteria for retreatment were thin pachymetry, suboptimal posterior corneal elevation according to the surgeon’s best clinical judgment and other visual alterations that did not improve with optical correction. No retreatments were performed prior to 3 months postoperatively and nearly all retreatments were performed between 3 and 6 months postoperatively.
All the data were checked for normality using the Kolmogorov–Smirnoff test. The relationship between the postoperative BCVA, with the spherical error, and the astigmatism were assessed using linear regression analysis and Pearson’s correlation coefficient. The chi-square test was used for the comparison of the proportion of patients who underwent retreatment. For other comparisons, the unpaired two-tailed Student’s t test was used. P values < 0.05 were considered statistically significant.
Data analysis was performed using the StatView SE + Graphics software (Abacus Concepts Inc., Berkeley, CA) for Macintosh (Apple Computer Inc, Cupertino, CA).
Results
In total, 841 eyes of 825 patients were analyzed. The sample was divided in two groups based on magnitude of preoperative myopic astigmatism: 432 eyes (51.37%) had < 1.5 D (Group 1) and 409 eyes (48.63%) had ≥ 1.5 D (Group 2). The mean patient age in Groups 1 and 2 were 32.24 ± 6.20 years (range: 19–66) and 34.18 ± 7.51 years (range: 19–57), respectively (P < 0.0001). Preoperative and 3 months postoperative refractive characteristics, keratometry and visual acuity results are shown in Table 1.
Significant differences between the two groups were detected for all assessed parameters at the three months postoperative visit (P < 0.05). Three months after primary surgery, the efficacy index was 0.94 ± 0.18 (range: 0.05–1.31) for Group 1 versus 0.89 ± 0.22 (range: 0.11–1.75) for Group 2 (P < 0.001).
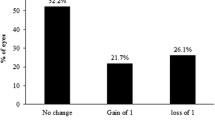
In total, 138 eyes (16.41%) were retreated. Of these, 28 were from patients of Group 1 (6.5%) and 110 (26.9%) were from patients of Group 2 (P < 0.001). The main visual parameters in the retreated versus non-retreated eyes are shown in Table 2. The initial flap could be lifted easily in all retreated eyes. The characteristics of spherical and cylindrical errors, UCVA and BCVA before the retreatment in both study groups are shown in Table 3. The value of the residual cylinder was higher in the high preoperative astigmatism group.
Table 4 depicts the ultimate mean characteristics of all eyes after treatment (i.e., final results 3 months after primary treatment in non-retreated eyes and 3 months after retreatment in retreated eyes).
There was a statistically significant but clinically not significant difference in the residual mean postoperative cylinder between Groups 1 and 2 (−0.08 ± 0.24 vs −0.27 ± 0.46 D respectively, P = 0.001). No significant difference was found in the mean spherical error (P = 0.1, Table 3). Following retreatment, the efficacy index improved to 0.97 ± 0.15 for Group 1 and 0.97 ± 0.17 for Group 2 (P = 0.92). The safety index was not statistically different 3 months after retreatment (1.00 ± 0.12 in Group 1 vs 1.02 ± 0.15 in Group 2, P = 0.06).
Table 5 shows the definitive results for eyes that underwent primary intervention only and eyes that underwent retreatment. In Group 1, compared to retreated eyes, non-retreated eyes had statistically lower astigmatism and significantly better UCVA and BCVA (P < 0.001 for all comparisons). In Group 2, the difference in residual cylinder between retreated and non-retreated eyes was of marginal statistical significance (P = 0.04) but there were no differences in UCVA, efficacy or safety. BCVA however was better in non-retreated eyes in a statistically significant way (P = 0.01).
Discussion
Our results show that patients with preoperative myopic astigmatism < 1.5 D or ≥ 1.5 D can safely be treated with FS-LASIK. Nonetheless, 3 months after the primary surgery, eyes with preoperative myopic astigmatism ≥ 1.5 D have significantly worse corrected- and uncorrected visual acuity and worse refractive characteristics compared to eyes with lower myopic astigmatism.
The proportion of eyes that required a retreatment due to postoperative refraction-related dis-satisfaction was four times higher in the group of patients with higher preoperative myopic astigmatism (26.9% vs 6.5%, P < 0.001). Although we believe that the significant proportion of patients with high preoperative myopic astigmatism who underwent retreatment is explained by the residual refractive error following the primary procedure, we should also acknowledge that the pain-free, fast visual rehabilitation following FS-LASIK might have lowered the patients’ threshold for a vision-enhancing retreatment [12].
Following retreatment, UCVA and BCVA improved both for Group 1 and 2 (Table 4). Compared to Group 2, participants of Group 1 had statistically better UCVA and BCVA after retreatment (P = 0.0001 for both comparisons). These differences however were clinically unimportant. The residual cylinder was statistically greater in Group 2 even after the retreatment, but this difference was also clinically unimportant.
Interestingly, despite the improvement of UCVA and BCVA that retreatment afforded to patients dissatisfied after the primary procedure, the final cylindrical error, UCVA and/or BCVA in these retreated eyes were statistically worse than those of eyes that did not need a retreatment (Table 5). This peculiar pattern was observed not only in eyes with higher (≥ 1.5 D), but also with lower preoperative astigmatism (< 1.5 D). Although these differences were statistically significant, they are of no clinical relevance. The explanation for these findings is unclear, but it might be reasonable to assume that ablation algorithms for retreatments are slightly less accurate than those for primary treatments.
It is generally agreed that the surgical correction of moderate to high astigmatism is less predictable than the correction of spherical errors [13,14,15]. The suboptimal results with high astigmatism may be due to the imprecise alignment of the elliptic ablation axis, the under-compensated cyclotorsion and the unaccounted coupling effect that toric ablation can have on spherical error [16]. Similarly to our study, other reports have identified preoperative astigmatism as a risk factor for retreatment [17,18,19]. For example, Hersh et al. [17] found retreatment rates of 29.2% due to residual astigmatism in patients with greater values of astigmatism. Of note, their figure (29.2%) is very similar to ours (26.9%). In parallel with these findings, Pokroy and co-workers reported that the retreatment rate in patients with myopic astigmatism between 1.5 and 2.5 D or patients with myopic astigmatism > 2.5D was significantly higher compared to the retreatment rate of patients with myopic astigmatism < 1.5D [18].
A number of studies have compared the efficacy of different surgical techniques in correcting myopic astigmatism [20,21,22,23,24,25]. A consistent finding of these reports is that visual and refractive outcomes are better in eyes with lower, rather than higher cylindrical error. Nonetheless, to the best of our knowledge, the comparative efficacy of FS-LASIK in treating higher or lower myopic astigmatism had yet to be further investigated.
Overall, 16.41% of the included eyes in our study were retreated. A direct comparison of these results with data reported for microkeratome-assisted LASIK is not possible for several reasons: while our only inclusion criterion for the patients analyzed was dis-satisfaction due to stable residual refractive error, other studies have included in their analyses patients who additionally may have required retreatment due to regression or suboptimal UCVA due to under-correction [26, 27]. Furthermore, factors such as study design or treatment-related differences (e.g., multiple surgeons and laser platforms, dissimilar cut-off values for astigmatism) and population characteristics (e.g., preoperative refraction, length of follow-up, socioeconomic circumstances affecting patient decisions) may have all affected the results of different studies [28, 29].
From a clinical viewpoint, our study underlies the necessity for clinicians to inform patients with significant myopic astigmatism who are considering FS-LASIK for their refractive correction about the possibility of residual cylindrical error. The likelihood of a retreatment becoming necessary due to residual refractive error should also be clearly communicated to patients. On the other hand, highly satisfactory clinical results can be expected following a retreatment in patients unsatisfied after a primary FS-LASIK due to residual refractive error.
Certain limitations of our study need to be acknowledged. In the current investigation, all cases were operated by a single experienced surgeon using the same femtosecond and excimer lasers. Consequently, our data may not be applicable to interventions using different refractive platforms. On the other hand, the advantage of using data from an adequate sample of patients operated by a single surgeon with the same devices is that some well-known weaknesses of multicenter studies (e.g., different laser platforms, surgeons’ experience and technique etc.) are avoided. Astigmatic vector analysis is the ideal instrument for the study of surgically induced astigmatism. However, we did not opt for a vector analysis in this study because our primary aim was not to examine the precise effect of FS-LASIK on the magnitude and axis of cylindrical error, but rather to compare the clinical precision and usefulness of correcting lower or higher myopic astigmatism with this particular technique. Finally, the exact reason for the patients’ dis-satisfaction, such as halos or other dysphotopic phenomena were not specifically recorded. Therefore, we cannot comment on the specific nature or intensity of symptoms that led patients to request a retreatment.
Conclusion
Our study shows that higher preoperative myopic astigmatism is associated with a higher probability of retreatment due to patient dis-satisfaction as a result of residual cylindrical error. Nonetheless, retreatment is safe and the final clinical results are comparable to those of patients with lower preoperative astigmatism who were satisfied with the primary treatment.
References
Farjo AA, Sugar A, Schallhorn SC, Majmudar PA, Tanzer DJ, Trattler WB, Cason JB, Donaldson KE, Kymionis GD (2013) Femtosecond lasers for LASIK flap creation: a report by the American academy of ophthalmology. Ophthalmology 120:5–20
Dawood YF, Al Hassany U, Issa AF (2017) Temporal and spatial flap variability in laser in-situ keratomileusis by optical coherence tomography. J Ophthalmic Vis Res 12(4):368–373
Aristeidou A, Taniguchi EV, Tsatsos M, Muller R, McAlinden C, Pineda R, Paschalis EI (2015) The evolution of corneal and refractive surgery with the femtosecond laser. Eye Vis (Lond) 14(2):12
Santhiago MR, Kara-Junior N, Waring GO (2014) Microkeratome versus femtosecond flaps: accuracy and complications. Curr Opin Ophthalmol 25:270–274
Wong RC, Yu M, Chan TC, Chong KK, Jhanji V (2015) Longitudinal comparison of outcomes after sub-bowman keratomileusis and laser in situ keratomileusis: randomized, double-masked study. Am J Ophthalmol 159:835–845
Chan C, Saad A, Randleman JB, Harissi-Dagher M, Chua D, Qazi M, Saragoussi JJ, Shetty R, Ancel JM, Ang R, Reinstein DZ, Gatinel D (2018) Analysis of cases and accuracy of 3 risk scoring systems in predicting ectasia after laser in situ keratomileusis. J Cataract Refract Surg 44(8):979–992
Yvon C, Archer TJ, Gobbe M, Reinstein DZ (2015) Comparison of higher-order aberration induction between manual microkeratome and femtosecond laser flap creation. J Refract Surg 31:130–135
Sun Q, Deng ZZ, Zhou YH, Zhang J, Peng XY (2016) Effect of femtosecond and microkeratome flaps creation on the cornea biomechanics during laser in situ keratomileusis: one year follow-up. Int J Ophthalmol 9(10):1409–1414
Hashmani S, Hashmani N, Rajani H, Ramesh P, Soomro JA, Hussain Shah SR, Kumar J, Mahmood Shah SM (2017) Comparison of visual acuity, refractive outcomes, and satisfaction between LASIK performed with a microkeratome and a femto laser. Clin Ophthalmol 23(11):1009–1014
Gil-Cazorla R, Teus MA, de Benito-Llopis L, Mikropoulos DG (2011) Femtosecond laser vs mechanical microkeratome for hyperopic laser in situ keratomileusis. Am J Ophthalmol 152:16–21
Holladay JT, Moran JR, Kerizian M (2001) Analysis of aggregate surgically induced refractive changes, prediction error, and intraocular astigmatism. J Cataract Refract Surg 27:61–79
Gros-Otero J, Garcia-Gonzalez M, Teus MA, Iglesias-Iglesias M, Gimenez-Vallejo C (2016) Femtosecond laser-assisted sub-bowman keratomileusis versus laser-assisted subepithelial keratomileusis to correct myopic astigmatism. J Optom 13:1888–4296
Yan P, Du Z, Zhang Y (2017) Polar value analysis of low to moderate astigmatism with wavefront-guided sub-bowman keratomileusis. J Ophthalmol 20:564–615
Ivarsen A, Naeser KM, Hjortdal J (2013) Laser in situ keratomileusis for high astigmatism in myopic and hyperopic eyes. J Cataract Refract Surg 39:74–80
Katz T, Wagenfeld L, Galambos P et al (2013) LASIK versus photorefractive keratectomy for high myopic (> 3 diopter) astigmatism. J Refract Surg 29:824–831
Davis EA, Listrom RL (2001) Astigmatism management: ablation patterns. Curr Opin Ophthalmol 12:300–303
Hersh PS, Fry KL, Bishop DS (2003) Incidence and associations of retreatment after LASIK. Ophthalmology 110:748–754
Pokroy R, Mimouni M, Sela T, Munzer G, Kaiserman I (2016) Myopic laser in situ keratomileusis retreatment: incidence and associations. J Cataract Refract Surg 42(10):1408–1414
Schallhorn SC, Venter JA (2009) One-month outcomes of wavefront-guided LASIK for low to moderate myopia with the VISX STAR S4 laser in 32,569 eyes. J Refract Surg 25:634–641
Jun I, Kang DSY, Arba-Mosquera S, Choi JY, Lee HK, Kim EK, Seo KY, Kim TI (2018) Comparison between wavefront-optimized and corneal wavefront-guided transepithelial photorefractive keratectomy in moderate to high astigmatism. BMC Ophthalmol 18(1):154
de Ortueta D, von Rüden D, Verma S, Magnago T, Arba-Mosquera S (2018) Transepithelial photorefractive keratectomy in moderate to high astigmatism with a non-wavefront-guided aberration-neutral ablation profile. J Refract Surg 34(7):466–474
Xi L, Zhang C, He Y (2018) Clinical outcomes of transepithelial photorefractive keratectomy to treat low to moderate myopic astigmatism. BMC Ophthalmol 18(1):115
Qin B, Li M, Chen X, Sekundo W, Zhou X (2018) Early visual outcomes and optical quality after femtosecond laser small-incision lenticule extraction for myopia and myopic astigmatism correction of over −10 dioptres. Acta Ophthalmol 96(3):341–346
Ghoreishi M, Naderi Beni A, Naderi Beni Z, Zandi A, Kianersi F (2017) Comparing aspheric ablation profile with standard corneal ablation for correction of myopia and myopic astigmatism, a contralateral eye study. Lasers Med Sci 32(9):2129–2138
Patel S, Bohac M, Biscevic A, Koncarevic M, Anticic M, Gabric N (2017) A Critical evaluation of refractive outcomes following LASIK for moderate to high astigmatism using two excimer laser platforms. J Refract Surg 33(2):104–109
Reinstein DZ, Carp GI, Archer TJ, Lewis TA, Gobbe M, Moore J, Moore T (2016) Long-term visual and refractive outcomes after LASIK for high myopia and astigmatism from −8.00 to −14.25 D. J Refract Surg 32(5):290–7
Patel NP, Clinch TE, Weis JR, Ahn C, Lundergan MK, Heidenreich K (2000) Comparison of visual results in initial and re-treatment laser in situ keratomileusis procedures for myopia and astigmatism. Am J Ophthalmol 130:1–11
Sugar A, Rapuano CJ, Culberston WW, Huang D, Varley GA, Agapitos PJ, de Luis VP, Koch DD (2002) Laser in situ keratomileusis for myopia and astigmatism: safety and efficacy: a report by the American academy of ophthalmology. Ophthalmology 109:175–187
Katz T, Frings A, Linke SJ, Richard G, Druchkiv V, Steinberg J (2014) Laser in situ keratomileusis for astigmatism ≤ 0.75 Diopter combined with low myopia: a retrospective data analysis. BMC Ophthalmol 14:1
Funding
No private or public support was received for this study.
Author information
Authors and Affiliations
Contributions
All named authors meet the International Committee of Medical Journal Editors (ICMJE) criteria for authorship for this article, take responsibility for the integrity of the work as a whole, and have given their approval for this version to be published.
Corresponding author
Ethics declarations
Conflict of interest
None of the authors has any financial or proprietary interest in any aspect of this study.
Data availability
The datasets during and/or analyzed during the current study are available from the corresponding author on reasonable request.
Consent to participate
The authors received the approval of an institutional review board, the COMITÉ ÉTICO DE INVESTIGACIÓN CLÍNICA REGIONAL DE LA COMUNIDAD DE MADRID (code 216/03, version 2.0 Mayo 2016), and the study conformed to the Helsinki Declaration. All participants accepted the possibility of their data being used to participate in this study by signing the informed consent of their intervention.
Consent to publish
All participants accepted the possibility that their data be published with the signing of the informed consent of their intervention. The tables are original and have been produced by the authors for this particular publication.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
About this article
Cite this article
Cañones-Zafra, R., Katsanos, A., Garcia-Gonzalez, M. et al. Femtosecond LASIK for the correction of low and high myopic astigmatism. Int Ophthalmol 42, 73–80 (2022). https://doi.org/10.1007/s10792-021-02001-x
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s10792-021-02001-x