Abstract
To evaluate surgically induced astigmatism (SIA) and axis deviation after coaxial microincision superotemporal clear corneal phacoemulsification incision in eyes with differently located steep axis. This prospective, comparative study included four groups of 45 eyes with age-related cataracts; each group underwent 2.2-mm superotemporal clear corneal incision (CCI) cataract surgery. The four groups of patients were divided by location of the steep axis. Groups were matched according to symmetry of the steep axis for both right and left eyes as follows—0°–45° of steep axis for right eyes, and 136°–180° for left eyes (group 1); 46°–90° for right eyes and 91°–135° for left eyes (group 2); 91°–135° for right eyes and 46°–90° for left eyes (group 3); and 136°–180° for right eyes and 0°–45° for left eyes (group 4). Outcome measures included changes in mean total astigmatism, SIA, and axis deviation. Astigmatism was measured by manual keratometry readings before surgery and week 1, week 4, week 8, and week 12 postoperatively. SIA was calculated by the vector analysis (Holladay–Cravy–Koch method). The magnitude of mean total astigmatism was lowest in group 3 and highest in group 1 at week 12. SIA was 0.39 diopters (D), 0.22 D, 0.17 D, and 0.28 D in group 1, group 2, group 3, and group 4, respectively. The change in astigmatic axis deviation was highest in group 3 (23.6 ± 16.6) (P < 0.05). Axis deviation and SIA were stable after week 4. Planning of CCI on or near the steep axis can help decrease corneal astigmatism.
Similar content being viewed by others
Explore related subjects
Discover the latest articles, news and stories from top researchers in related subjects.Avoid common mistakes on your manuscript.
Introduction
Surgically induced astigmatism (SIA) can be modulated by several methods at the time of cataract surgery. Phacoemulsification incision located on the steep corneal axis corrects small amounts of astigmatism. Peripheral corneal relaxing incisions, and toric intraocular lenses (IOLs) are used for more astigmatism. In recent years, several studies have investigated induced astigmatism after various types of small-incision cataract wounds (scleral, clear corneal, posterior limbal tunnel), and at various locations including superior, superonasal, superotemporal, and temporal [1]. It is generally accepted that small clear corneal cataract incisions are associated with less SIA [2, 3]. Recently, size of incision has been reduced from 3.2 to 1.4 mm [4]. Rapid restoration of visual acuity by reducing SIA and correcting residual astigmatism produces the best satisfactory surgical results [5]. Different located incisions have resulted in different levels of astigmatism [5–7]. Careful planning of the location of the corneal incision before cataract surgery is therefore important to avoid high induced astigmatism. Astigmatism outcomes can vary widely when the incision is made in the same location regardless of preoperative steep axis. In this prospective study, we evaluated SIA after phacoemulsification with a 2.2-mm superotemporal clear corneal incision (CCI) in eyes with differently located steep axis.
Materials and methods
This prospective study of 180 eyes of 135 patients comprised four groups of 45 eyes. Each group underwent clear corneal cataract surgery and implantation of a foldable acrylic IOL through a 2.2-mm superotemporal corneal tunnel incision between November 2011 and September 2012. The patients were divided into four groups by location of the steep axis. We matched the groups according to symmetry of the steep axis for both right and left eyes and evaluated 0°–45° of steep axis for right eyes, and 136°–180° for left eyes as group 1; 46°–90° for right eyes and 91°–135° for left eyes as group 2; 91°–135° for right eyes and 46°–90° for left eyes as group 3; and 136°–180° for right eyes and 0°–45° for left eyes as group 4 (Fig. 1). Preoperative corneal astigmatism between 0.50 diopters (D) and 2.0 D was included in the study. The study included 81 males and 49 females with a mean age of 74.4 years (range 56–78 years). Patients with clear cornea and without any inflammatory conditions or history of previous ocular surgery affecting anterior segment were included in this study. Patients with corneal scar, severe dry eye, pterygium, inflammatory disease of eye, history of previous ocular surgery, systemic connective tissue disease were excluded. Written informed consent was obtained from each patient.
Full ophthalmic examination was performed on all eyes preoperatively and at week 1, week 4, week 8, and week 12 postoperatively. Sex, age, manifest refraction and keratometry measurements were evaluated. Manifest refraction measurement was performed with a Canon RK-F1 autorefractometer. Astigmatism was measured by manual keratometry readings. Axis deviation was calculated as the difference between postoperative and preoperative values. If the changes were <0.05 D for SIA, and 5° for axis deviation in three consecutive visits, the first visit was considered as stabilization time. The CCI was performed at the superotemporal location in all groups. All cataract surgeries were performed by a single surgeon.
All operations were performed using phacoemulsification through a two-step, 0.3-mm groove clear corneal tunnel incision under topical anesthesia. The CCI was made using a 2.2-mm disposable blade and approximately 0.2 mm anterior to the edge of the limbal vessels. The CCI was performed approximately on 110°–120° of the corneal axis for right eyes and on 60°–70° for left eyes. After CCI, capsulorhexis, phacoemulsification and cortex removal stages, an acrylic IOL was inserted. A Monarch III injector and D cartridge (Alcon) system was used for IOL implantation. The ophthalmic viscoelastic material was removed by bimanual irrigation and aspiration system. All surgeries were sutureless and uncomplicated.
Main outcome measurement was SIA consisting of astigmatic amplitude and axis from cross cylinder form by rectangular coordinate method using the Holladay–Cravy–Koch formula. One-way analysis of variance test (ANOVA) was used for comparing the mean values of groups and Tukey’s post hoc test was used to determine which groups differed from each other.
Results
Table 1 shows the change in the mean total astigmatism before surgery and at week 1, 4, 8, and 12 postoperatively. The magnitude of astigmatism was lowest in group 3 and highest in group 1 at all successive examinations. The change in mean total astigmatism was significant between group 1 and 3 at week 12 (P = 0.023).
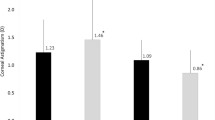
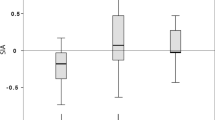
Table 2 shows the mean pre- and postoperative corneal astigmatism and SIA calculated by using vector analysis. Preoperative mean keratometry reading values were not statistically significant between groups (centroid 0.88, 0.78, 0.81, and 0.89 D in groups 1–4, respectively, P > 0.05 for all). The axis of mean preoperative corneal astigmatism was 20°, 79°, 103°, and 161° for right eyes and 10°, 80°, 111°, 165° for left eyes in groups 1–4, respectively (Fig. 1). The comparison of SIA between group 1 and group 3 and between group 3 and group 4 were significant at week 12 (P = 0.018, P = 0.026, respectively). The SIA was lowest in group 3 and highest in group 1 at all successive examinations. The SIA was stabilized after week 4 (Fig. 2).
Table 3 shows the change in mean axis of astigmatism after cataract surgery. The change in axis deviation was highest in group 3. There was a significant difference between group 1 and group 3, between group 2 and group 3, and between group 3 and group 4 at week 12 (P = 0.006, P = 0.025, P = 0.019, respectively). Stabilization of axis deviation occurred after week 4.
Discussion
Identifying surgical methods to provide satisfactory results by reducing SIA and correcting residual astigmatism remains a challenge for surgeons. Correcting astigmatism at the time of cataract surgery can be accomplished either by incisional techniques, such as use of a cataract incision for flattening or astigmatic keratotomy, or by implanting a toric IOL [8, 9]. Corneal astigmatism after phacoemulsification surgery depends on the location, configuration and size of cataract incision, presence or absence of wound suture, optical center of the cornea, and surgical approach [1, 10, 11]. Superior, superotemporal, temporal and steep axis location incisions are commonly used by several surgeons [7]. Despite the superonasal incision not being popular due to more unstable wound healing and higher induced astigmatic results, it is still chosen by some right-handed surgeons [1, 11, 12]. Many studies have demonstrated that temporal location incisions induce less astigmatism than other types of incisions [1, 7, 13, 14]. In a study, magnitude of astigmatism was significantly smaller in oblique incisions than in superior incisions [15]. Rho and Joo compared SIA outcomes in groups with preoperative temporal, superotemporal, and superior 3-mm one-step steep meridian CCIs. 2 months postoperatively, SIA was 0.28 D, 0.40 D, and 0.462 D, respectively [16]. It was generally accepted that smaller incision size is one of the determining factors for less SIA [17, 18]. Luo et al. [19] compared temporal location at three CCI sizes (1.8, 2.2, 3.0 mm). In their study, the mean SIA in the 1.8 and 2.2 mm groups was significantly less than that in 3.0 mm group after one month, without a significant difference between the 1.8 and 2.2 mm groups. Hayashi et al. [20] showed that SIA at 2 months postoperatively was 0.74 D after coaxial 2.65-mm small-incision cataract surgery and 0.56 D after 2.0-mm coaxial microincision cataract surgery (MICS). Wilczynski et al. [21] compared SIA one month after coaxial phacoemulsification through a 1.8-mm microincision with that for bimanual phacoemulsification through a 1.7-mm microincision. The results showed mean SIA of 0.42 ± 0.29 D for the coaxial MICS group and 0.50 ± 0.24 D for the bimanual group; the difference was not statistically significant. These studies revealed that incision size 2.5 mm will have less SIA. In our study, SIA was 0.39 D, 0.22 D, 0.17 D, and 0.28 D in groups 1–4, respectively at week 12. We detected an increase in SIA over the distance from the steep axis to the incision. SIA was significantly lower in group 3 than the other groups. Hovever, we believe that further studies are needed to show the importance of distance between incision location and steep axis. Masket and Tennen reported that astigmatic stabilization of 3.0-mm temporal clear corneal cataract incisions occured at 2 weeks after surgery [22]. Barequet et al. [23] reported that induced astigmatism was evident at week 6 and persisted to 12 months postoperatively. In our study, SIA was stable after week 4 postoperatively. In additon, a longer follow-up period could be more beneficial to show stability or plateau.
The aim of all surgical procedures is reduced astigmatism and better visual function, but incisional astigmatism is usually inevitable. Astigmatism outcomes can cover a wide range if the incision is made in the same location regardless of preoperative values. It is not clear why astigmatism outcomes depend on incision location. The effect of CCI on astigmatism can be explained by the architecture of the corneal curvature. The high frequency of SIA associated with nasal incision [1, 13] suggests it might be due to the proximity to the optical center, approach angle to the cornea, or wound distortion and stretch of the cornea during surgery. Similarly, it is well known that the horizontal meridian is approximately 1 mm wider than vertical length. A superotemporal incision is closer to the corneal apex than a temporal incision which could explain the greater effect of incision location on the central corneal curvature [24–26]. The magnitude of preoperative astigmatism may affect postoperative astigmatism and axis shift. A study reported that preoperative astigmatism >1.2 D caused greater postoperative astigmatism, although modulating through different incision locations [15]. Tejedor and Murube recommended at least 1.5–D of corneal astigmatism in superior incisions with the steep axis between 70 and 110°, in order to avoid a 90° shift [27]. In our study, the preoperative astigmatic values were <1.5 D. The axis shift was greatest in group 3, but it was not more than 90°. It is generally accepted that reducing astigmatism without significantly changing the axis is well tolerated and satisfactory for patients. An axis shift >90° is not well tolerated [24].
In conclusion, taking the preoperative corneal axis into consideration can provide more predictable astigmatic results for surgeons. The careful planning of corneal incision location on or near the steep axis can help decrease SIA. Therefore, surgeons may consider varying the location of corneal incisions depending on the location of the steep axis.
References
Kohnen S, Neuber R, Kohnen T (2002) Effect of temporal and nasal unsutured limbal tunnel incisions on induced astigmatism after phacoemulsification. J Cataract Refract Surg 28:821–825
Alió JL, Rodriguez-Prats JL, Galal A, Ramzy M (2005) Outcomes of microincision cataract surgery versus coaxial phacoemulsification. Ophthalmology 112:1997–2003
Alió JL, Agdeppa MC, Rodriguez-Prats JL, Amparo F, Piñero DP (2010) Factors influencing corneal biomechanical changes after microincision cataract surgery and standard coaxial phacoemulsification. J Cataract Refract Surg 36:890–897
Liu Y, Jiang Y, Wu M, Liu Y, Zhang T (2008) Bimanual microincision phacoemulsification in treating hard cataracts using different power modes. Clin Experiment Ophthalmol 36:426–430
Rainer G, Menapace R, Vass C, Annen D, Findl O, Schmetterer K (1999) Corneal shape changes after temporal and superolateral 3.0 mm clear corneal incisions. J Cataract Refract Surg 25:1121–1126
Lyhne N, Krogsager J, Corydon L, Kjeldgaard M (2000) One year follow-up of astigmatism after 4.0 mm temporal clear corneal incisions and superior scleral incisions. J Cataract Refract Surg 26:83–87
Simşek S, Yaşar T, Demirok A, Cinal A, Yılmaz OF (1998) Effect of superior and temporal clear corneal incisions on astigmatism after sutureless phacoemulsification. J Cataract Refract Surg 24:515–518
Sun XY, Vicary D, Montgomery P, Griffiths M (2000) Toric intraocular lenses for correcting astigmatism in 130 eyes. Ophthalmology 107:1776–1781
Poll JT, Wang L, Koch DD, Weikert MP (2011) Correction of astigmatism during cataract surgery: toric intraocular lens compared to peripheral corneal relaxing incisions. J Refract Surg 27:165–171
Koch KM, Kohnen T (1999) Refractive cataract surgery. Curr Opin Ophthalmol 10:10–15
Ermiş SS, Inan UU, Oztürk F (2004) Surgically induced astigmatism after superotemporal and superonasal clear corneal incisions in phacoemulsification. J Cataract Refract Surg 30:1316–1319
Altan-Yaycioglu R, Akova YA, Akca S, Gur S, Oktem C (2007) Effect on astigmatism of the location of clear corneal incision in phacoemulsification of cataract. J Refract Surg 23:515–518
Anders N, Pham DT, Antoni HJ, Wollensak J (1997) Postoperative astigmatism and relative strength of tunnel incisions: a prospective clinical trial. J Cataract Refract Surg 23:332–336
Borasio E, Mehta JS, Maurino V (2006) Surgically induced astigmatism after phacoemulsification in eyes with mild to moderate corneal astigmatism: temporal versus on-axis clear corneal incisions. J Cataract Refract Surg 32:565–572
Matsumoto Y, Hara T, Chiba K, Chikuda M (2001) Optimal incision sites to obtain an astigmatism-free cornea after cataract surgery with a 3.2 mm sutureless incision. J Cataract Refract Surg 27:1615–1619
Rho CR, Joo CK (2012) Effects of steep meridian incision on corneal astigmatism in phacoemulsification cataract surgery. J Cataract Refract Surg 38:666–671
Can I, Takmaz T, Yildiz Y, Bayhan HA, Soyugelen G, Bostanci B (2010) Coaxial, microcoaxial, and biaxial microincision cataract surgery: prospective comparative study. J Cataract Refract Surg 36:740–746
Masket S, Wang L, Belani S (2009) Induced astigmatism with 2.2- and 3.0-mm coaxial phacoemulsification incisions. J Refract Surg 25:21–24
Luo L, Lin H, He M, Congdon N, Yang Y, Liu Y (2012) Clinical evaluation of three incision size-dependent phacoemulsification systems. Am J Ophthalmol 153:831–839
Hayashi K, Yoshida M, Hayashi H (2009) Postoperative corneal shape changes: microincision versus small-incision coaxial cataract surgery. J Cataract Refract Surg 35:233–239
Wilczynski M, Supady E, Piotr L, Synder A, Palenga-Pydyn D, Omulecki W (2009) Comparison of surgically induced astigmatism after coaxial phacoemulsification through 1.8 mm microincision and bimanual phacoemulsification through 1.7 mm microincision. J Cataract Refract Surg 35:1563–1569
Masket S, Tennen DG (1996) Astigmatic stabilization of 3.0 mm temporal clear corneal cataract incisions. J Cataract Refract Surg 22:1451–1455
Barequet IS, Yu E, Vitale S, Cassard S, Azar DT, Stark WJ (2004) Astigmatism outcomes of horizontal temporal versus nasal clear corneal incision cataract surgery. J Cataract Refract Surg 30:418–423
Raviv T, Epstein RJ (2000) Astigmatism management. Int Ophthalmol Clin 40:183–198
Merriam JC, Zheng L, Merriam JE, Zaider M, Lindström B (2003) The effect of incisions for cataract on corneal curvature. Ophthalmology 110:1807–1813
Cravy TV (1991) Routine use of a lateral approach to cataract extraction to achieve rapid and sustained stabilization of postoperative astigmatism. J Cataract Refract Surg 17:415–423
Tejedor J, Murube J (2005) Choosing the location of corneal incision based on preexisting astigmatism in phacoemulsification. Am J Ophthalmol 139:767–776
Financial disclosure
No author has a financial or proprietary interest in any material or method mentioned.
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Özyol, E., Özyol, P. Analyses of surgically induced astigmatism and axis deviation in microcoaxial phacoemulsification. Int Ophthalmol 34, 591–596 (2014). https://doi.org/10.1007/s10792-013-9858-8
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s10792-013-9858-8