Abstract
Ferulic acid (FA), a hydroxycinnamic acid, is an organic compound found in several plant species. Previous studies have shown that FA contains anti-inflammatory and anti-arthritic properties. This study aimed to investigate the anti-arthritic activity and possible mechanism(s) of action of FA in complete Freund’s adjuvant (CFA)-induced arthritis. The progression of rheumatoid arthritis (RA) involves the activation of the Janus kinase-signal transducer and activator of transcription (JAK/STAT) pathway by proinflammatory cytokines. Molecular docking of FA showed promising Janus kinase 2 (JAK2) inhibition with a docking score of − 6.7, which is comparable with that of ruxolitinib, a standard inhibitor. However, in vitro JAK2 inhibition assay showed a half maximal inhibitory concentration (IC50) of 6.67 ± 0.88 µg/ml. Both doses of FA (25 and 50 mg/kg) significantly attenuated primary (volume of paw edema) and secondary lesions. CFA-induced arthritic rats showed a significant decrease in body weight, A/G ratio, and Hb but showed a greater arthritic index, ESR levels, and percentage of lymphocytes. These alterations were significantly reduced in rats treated with FA and prednisolone. FA also reversed changes to biochemical parameters and inflammatory markers, such as C-reactive protein (CRP) and rhematoid factor (RF). Additionally, we found CFA-induced arthritis triggered the secretion of TNF- α, increased JAK2 levels, and reduced TGF-β levels in tissue homogenates. However, in rats treated with FA, such alterations significantly improved. Thus, our results reveal that FA contains anti-arthritic activity, which is possibly mediated by the inhibition of the JAK/STAT pathway.
Graphic abstract

Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Rheumatoid arthritis (RA) is a chronic systemic inflammatory syndrome that mainly damages the articular cartilage and ankylosis of the joints by producing a nonsuppurative proliferative and inflammatory synovitis (McInnes and Schett 2011). Even though the etiological factors of RA remain unidentified, autoimmunity plays a crucial part in its evolution and duration. RA is associated with articular cartilage damage, reduced movement, progressive disability, systemic complications, high socioeconomic costs, and early death (McInnes and Schett 2011). In inflamed RA joints, the production of proinflammatory cytokines, tumour necrosis factor alpha (TNF- α) and interleukin-1ß (IL-1ß), metalloproteinase, and free radicals by polymorphonucleate cells are responsible for cartilage and bone injury (McInnes and Schett 2011). Treatment of RA includes immunosuppressants, steroid and nonsteroidal anti-inflammatory drugs, and new biological drugs (Boyce 2006). Biological drugs that target proinflammatory cytokines have transformed treatment and management of rheumatoid arthritis (RA), among other autoimmune diseases (Boyce 2006).
The evolution of RA involves the activation of several signal transduction pathways, such as the Janus kinase (JAK)-signal transducer and activator of transcription (JAK/STAT) pathway by IL-6 and IFN-γ and the mitogen-activated protein kinase (MAPK) pathway by IL-1ß, IL-6, and IFN-γ (Ohori 2008; Heim 1999; Malemud 2009). TNF-α has also been reported to activate the MAPK pathway. Wajant et al. (2003) showed that recombinant human (rh)-TNF-α produced the phosphorylation of the STAT3 protein without altering its content. The activation of the JAK/STAT pathway plays a crucial role in the treatment of RA, which was confirmed with the FDA approval of tofacitinib, a JAK3-selective small molecule inhibitor (SMI). Undeniably, including tofacitinib as a treatment for RA has enabled the development of new drugs that target the JAK/STAT pathway (Kaur et al. 2014; Malemud 2018).
Ferulic acid (FA), a hydroxycinnamic acid, is an organic compound present in several plant species, with particularly high concentrations in grains, such as rice and corn (Zhang et al. 2010). Oral administration of ferulic acid has a low degree of toxicity. An acute LD50 of 3200 mg/kg was calculated in mice (Wang and Ou-Yang 2005), whereas LD50 values for male and female rats were calculated as 2445 mg/kg and 2113 mg/kg, respectively (Tada et al. 1999; Ou and Kwok 2004). This low toxicity has been confirmed by numerous experimental studies (Mancuso and Santangelo 2014) FA has been reported to have antioxidant and anti-inflammatory properties (Zhang et al. 2018) and to be effective in treating ulcerative colitis (Thyagaraju 2008), epilepsy (Hassanzadeh et al. 2017), arthritis (Cunha et al. 2015), liver disease (Panneerselvam et al. 2013), and Alzheimer’s disease (Sultana et al. 2005; Zeni et al. 2017) Other studies have reported that substances derived from ferulic acid exhibit free radical scavenger activity as they increase the expression of antioxidant proteins via the activation of nuclear factor kappa B (NF-kB) and Cyclo-oxygenase-2 (COX-2) and the inhibition of Nitric oxide synthases (iNOS) (Islam et al. 2009; Bolling et al. 2011; Sultana 2012).
This study sought to investigate whether orally administrated FA affects complete Freund's adjuvant (CFA)-induced arthritis in rats. We also aimed to evaluate whether the effect, if present, is mediated by the inhibition of the JAK/STAT pathway.
Materials and methods
Materials used
FA was purchased from Sigma Aldrich, USA. The JAK2 ELISA kit (MBS2019409), the rat transforming growth factor beta (TGF-β) ELISA Kit (MBS260302), and the rat rheumatoid factor (RF) ELISA Kit (1906410B) were purchased from MyBioSource, California, USA. The rat TNF-α ELISA Kit (ELR- TNF-α) and the rat C-reactive protein (CRP) ELISA Kit (ELR-CRP) were purchased from RayBio, Georgia, USA.
In silico study
Predicting biological activity
The web resource PASS Online was used to predict the biological activity of small organic molecules with an average accuracy above 95% (https://www.way2drug.com/passonline). To predict the pharmacological activity of the ferulic acid, we uploaded its structures using the file format “.mol” in PASS online and registered the corresponding Pa (probability to be active) and Pi (probability to be inactive) values, based on Lagunin et al. (2011) and Poroikov et al. (2003).
Ligand
The chemical structure of the 4-hydroxy-3-methoxycinnamic acid was accessed from Pubchem (https://pubchem.ncbi.nlm.nih.gov/).
Target
The three-dimensional structure of the target Janus-kinase enzyme was retrieved from the Protein Data Bank (PDB) using the PDB ID: 2B7A (https://www.rcsb.org/pdb). We used Chimera software to identify different residues, structure clarifications, and molecular properties.
Molecular docking
Mcule.com (1-Click Dockings) was used for molecular docking of the target and the ligand. The target protein was uploaded using a PDB format, downloaded from PDB. Only one ligand can be uploaded for docking at a time, thus the MOL2 file of only one ligand was uploaded at a given time. The docked score was compared with standard inhibitor ruxolitinib.
JAK2 assays
The JAK2 assay was performed using a commercial ELISA kit. Briefly, the test compound (1 mg/ml) was dissolved in dimethyl sulfoxide and successively diluted with a kinase assay buffer to achieve the following concentrations: 0.001, 0.01, 0.1, 1, and 10 µg/ml. We then prepared a master mixture as follows: 6 µl 5 × kinase assay buffer 1 + 1 µl of ATP (500 µM) + 1 µl 50X Poly (Glu: Tyr, 4:1) + 17 µl distilled water. The kinase assay buffer, ATP, and Poly (Glu:Tyr, 4:1) were thawed before being used in the mixture. We added 25 µl of the mixture to every well. We then thawed the JAK2 enzyme on ice. Upon first thawing, the tube having the enzyme was briefly whirled to recover the full content of the tube. The enzyme was then diluted to ~ 2.5 ng/µl with a 1 × kinase assay buffer. The remaining undiluted enzyme was stored at -80 °C. The reaction was initiated by adding 20 µl of the diluted JAK2 enzyme to the wells. The wells were then incubated at 30 °C for 45 min. After which, we added 50 µl of a Kinase-Glo Max reagent, previously thawed at room temperature, to each well. We covered the plates with aluminium foil and incubated them at room temperature for 15 min. Luminescence was measured using BMG Fluostar microplate reader.
In vivo methods
Animals
Male and female Wistar rats, weighing between 210 and 250 g, were kept at 25 ± 1 °C with a 12 h light/12 h dark cycle and received standard chow and water ad libitum. The animals were treated according to their respective treatment group (see below) with a vehicle solution (0.1%CMC in 0.9%NaCl solution), FA or prednisolone. Animals were not given food for 12 h prior to treatment. At the end of the study, the animals were euthanized with a thiopental sodium (100 mg/kg) overdose. The experimental protocol IAEC/05/2018 was approved by the Institutional Animal Ethical Committee (IAEC), on 18 August 2018.
Complete Freund’s adjuvant-induced arthritic model
Rats were divided into five groups (n = 6 rats/group): group A: vehicle control—rats were given saline orally—10 ml/kg; group B: model control; group C: standard treatment—rats were given prednisolone orally—5 mg/kg; group D: ferulic acid (FA)—rats were given a dosage of 25 mg/kg of FA; group E: ferulic acid (FA)—rats were given a dosage of 50 mg/kg of FA; group F: ferulic acid (FA)—rats were given a dosage of 100 mg/kg of FA. Arthritis was induced in all rats, except for those in the vehicle control group (group A), by injecting them with 0.1 ml of Freund's complete adjuvant (Sigma, Germany). The injection was given in the left hind paw (subplantar region) on day 0. This adjuvant is composed of dead Mycobacterium tuberculosis suspended in heavy paraffin oil to achieve a final concentration of 0.5 mg/ml. Treatments (FA—25 mg/kg, 50 mg/kg and 100 mg/kg—or prednisolone) were administered orally once a day according to Vogel and Vogel (2002). The anti-arthritic effect of FA and prednisolone was evaluated by determining paw volume of the injected paw with a Plethysmometer on day 3, 5, 9, 13, and 21 of our study.
The percentage inhibition of paw edema in treated groups was calculated using the formula:
where Vt is the edema volume in the drug-treated group and Vc is the edema volume in the model control group.
Body weight changes were recorded daily; primary and secondary lesions were also measured daily. The edema formed in the injected paw peaked 3–5 days after the injection and was measured on day 5. The percent inhibition of the edema, calculated using the formula described above, was considered as a primary lesion. While immunological mediated alterations, such as inflammation of non-injected sites (hindleg, forepaw, ears, nose, and tail) and body weight changes, were considered secondary lesions. Secondary lesions were assessed with an arthritic index, defined as the sum of scores according to Vogel and Vogel (2002; Table 1). Radiographic images were taken on day 21. For such, two animals were anesthetized with an intra-muscular injection containing ketamine (50 mg/kg) and xylazine (5 mg/kg). On day 22, blood samples were collected from each animal through the retro-orbital plexus; for such, the animals were anesthetized with ether. The blood samples collected were put in an EDTA test tube and a simple test tube. The blood of the simple test tube was kept for 30 min to coagulate, allowing the serum to be isolated and removed. The serum was then centrifuged at 4000 rpm, after which total WBC count, differential WBC count, ESR, C-reactive protein (CRP), RF, TNF α, and TGF- β were examined. After blood collection, animals were euthanized with a high dose of thiopental and the paws were excised to estimate JAK2 levels in the paw tissues.
Statistical analysis
Values are expressed as mean ± SE. Data distribution was verified using the Shapiro–Wilk test. One-way ANOVA followed by Tukey’s post-hoc tests were used to compare paw edema, haematological parameters, and biochemical parameters among groups. Kruskal–Wallis followed by Dunn’s multiple comparison test was used to compare arthritic score (nonparametric variables) among groups. Significant differences were considered when p < 0.05. All analyses were carried out in the SPSS software.
Results
Pharmacological activity and molecular docking
We predicted the biological activity of ferulic acid (FA) and ruxolitinib using the PASS Online software. The results received were filtered to identify targets with higher Pa (probability to be active) values and lower Pi (probability to be inactive) values (Table 2). Additionally, the website “Mcule.com” was used for molecular docking of the JAK2 protein (PDB ID: 2B7A), the target protein, and the ligand. Ferulic acid showed a docking score of − 6.7 (Table 2), which is comparable with the standard JAK2 inhibitor, ruxolitinib, that has a docking score of − 7.8 (Fig. 1).
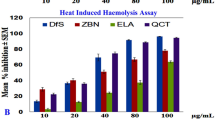
In vitro JAK2 assay
We evaluated how FA inhibits the JAK2 enzyme in vitro by measuring luminescence using the BMG Fluostar microplate reader. A commercial ELISA kit was treated with different concentrations (0.1, 0.01, 0.001, 1 and 10 µg/ml) of FA. FA showed a half maximal inhibitory concentration (IC50) of 6.67 ± 0.88 µg/ml (Table 3).
CFA-induced arthritic model
On day 3, we observed a substantial decrease of primary lesions (volume of paw edema) in rats treated with 25 mg/kg of FA, 50 mg/kg of FA, and prednisolone (Table 4). On day 21, rats treated with 25 mg/kg and 50 mg/kg of FA showed a decrease in the edema volume of 46.25% and 60%, respectively in comparison to model control rats, while rats treated with 100 mg/kg of FA showed a decrease of 62.5% and rats treated with prednisolone showed a decrease of 65% (Table 4).
Percentage change in body weight
No change in body weight was observed during the acute stage of arthritis, however, as the disease evolved, significant changes were observed. Rats treated with FA exhibited a progressive increase in body weight (Fig. 2), while rats from the model control group showed significant weight loss (− 5.71%) in comparison to rats from the vehicle control group. Treatment with 25 mg/kg, 50 mg/kg and 100 mg/kg of FA significantly improved body weight by 5.59%, 3.96%, and 3.69%, respectively, when compared to rats from the model control group.
Effect of Ferulic acid and Prednisolone on percentage body weight during CFA induced arthritis in the rat. The data represent the mean ± standard error of the mean (n = 6). Values are statistically significant at *P < 0.05 compared with the vehicle model group, #P < 0.05 compared with the model control group (one way ANOVA followed by Tukey’s test)
C-reactive protein (CRP) and Rheumatoid Factor (RF)
The CRP and RF are indicators of systemic inflammation and antibody production against the injected adjuvant. We observed elevated levels of CRP (13.14 ± 0.92) and RF (51.12 ± 0.28 IU/ml) in rats of the model control group. Rats treated with FA and prednisolone showed reduced levels of CRP and RF (Table 5).
Albumin–globulin ratio (A/G ratio)
Rats from the model control group showed a significant decrease in the A/G ratio in comparison to the vehicle control group (p < 0.05; Table 5). Such change was reversed by treating rats with either FA or prednisolone.
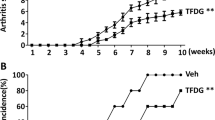
Arthritic score
Incidence of arthritis was observed in all rats that were given Freund’s adjuvant, indicating that all rats showed an arthritic scored > 1 when no anti-rheumatic treatment was administered. All experimental treatments used in this study showed a reduction in the arthritic score, which was eventually restored to scores indicating no arthritis (Table 5).
Haematological parameters
We observed a significant decrease in RBC and haemoglobin levels and an increase in WBC and ESR levels of arthritic rats in comparison to rats from the normal control group (Table 6). However, treatments (FA and prednisolone) were efficient and restored the haematological parameters.
Radiographic images
Radiographs of the arthritic paws were taken at the end of the experiment with a digital X-ray machine. We observed that the damage to the joints of CFA-induced arthritic rats treated with 25, 50 and 100 mg/kg of FA and 5 mg/kg of prednisolone was reduced. Rats treated with 25, 50 and 100 mg/kg of FA, as well as rats treated with prednisolone, showed little bone erosion at the end of the experiment (Fig. 3).
TNF α and TGF β levels in serum
The sandwich ELISA method was used to measure TNF α and TGF β levels. TNF α levels of rats from the model control group were significantly greater in comparison to the vehicle control group (p < 0.05; Fig. 4). However, rats treated with 25, 50 and 100 mg/kg of FA showed significantly lower levels of TNF α. Conversely, TGF β levels of rats from the model control group were significantly lower in comparison to the vehicle control group (p < 0.05; Fig. 5), while rats treated with 25 and 50 mg/kg of FA showed significantly greater TGF β levels. Rats given prednisolone significantly reversed the levels of TNF α and TGF β in comparison with the model control. Thus, both FA and prednisolone showed better effects in rats with CFA-induced arthritis.
JAK2 levels in tissue homogenates
At the end of experiment (day 22), rat’s paws were excised to estimate JAK2 levels in tissue homogenates using the sandwich ELISA method. JAK2 levels of rats from the model control group were significantly greater compared to rats from the vehicle control group (p < 0.05; Fig. 6). However, JAK2 levels found in tissue homogenates of rats treated with 25 and 50 mg/kg of FA were significantly lower to model control group.
Effects of ferulic acid on estimate JAK2 levels in tissue (paw) homogenates. The data represent the mean ± standard error of the mean (n = 6). Values are statistically significant at *P < 0.05 compared with the vehicle control group, #P < 0.05 compared with the model control group (one way ANOVA followed by Tukey’s test)
Discussion
Rheumatoid arthritis (RA) is a chronic and progressive autoimmune disorder that damages multiple joints and leads to deformity, disability, and early death in most patients. The pathogenesis of RA involves a multifaceted development mediated by a symbiotic network of cytokines, proteolytic enzymes, and prostanoids. In Asian countries, traditional medicine is the prevalent and most effective treatment to manage RA. Thus, studies exploring what the herbal drugs are consisted of may ultimately provide additional therapeutic agents for the treatment of RA. In this study, we evaluated the pharmacological activity of an organic compound found in popcorn and bamboo shoots, ferulic acid (FA), using the PASS Online software. Fa showed pharmacological activity for the JAK2 protein and had a docking score of − 6.7 (Table 2). In vitro assay is considered a tool for the broad selection of binding and to access the major targets for cross-target liability profiling. In this study, we screened FA to determine its potential to inhibit JAK2. JAK2 protein was treated with different concentrations (0.1, 0.01, 0.001, 1 and 10 µg/ml) of FA; the percentage of inhibition was calculated and plotted according to the respective concentrations. IC50 value for FA was found to be 6.67 ± 0.88 µg /ml.
Pearson (1956) developed a CFA-induced arthritic model, which has been used in several rat breeds by administering heat-killed Mycobacterium tuberculosis (Durai et al. 2004). The administration of CFA induces measurable polyarthritis (Patel and Shah 2013). Notably, the joint morphology observed in the rat model shares the synovial hyperplasia and cartilage degradation seen in humans with RA (Andersen et al. 2004; Kim et al. 2016). In this study, we detected a significant reduction of the edema in CFA-induced rats treated with FA, indicating FA has anti-inflammatory properties and the ability to attenuate immune system responses (Vogel and Vogel 2002). Additionally, most autoimmune disorders lead to reduced body weights, probably due to the release of inflammatory cytokines, loss of appetite, increased energy expenditure, and enhanced protein catabolism (Argiles and Lopez-Soriano 2002; Rall and Roubenoff 2004; Shelton et al. 2005). However, body weight of rats treated with 25 and 50 mg/kg of FA increased when compared to those in the model control group.
Our results suggest that an anaemic condition evolves in rats with CFA-induced arthritis (model control), which could be due to an atypical storage of iron in the reticuloendothelial system and the failure of bone marrow to respond to anaemia (Mowat 1971). The substantial rise in white blood cells in CFA-induced arthritic rats, due to the activation of the immune system, and the corresponding reduction of white blood cells in FA treated rats indicate the immunomodulation effect of FA. The increased levels of ESR found in rats from the model control group was not observed in rats treated with FA and prednisolone, suggesting that both FA and prednisolone are important in treating arthritis. Moreover, the increase in WBC and RF levels may be a consequence of immune system response to invading pathogenic microorganisms (Patel and Pundarikakshudu 2016).
The release of degradative enzymes substantially alters the connective tissue, inducing an immune response in CFA-induced arthritic rats (Vetal et al. 2013). Furthermore, C-reactive protein (CRP), which has been recognized as a biomarker for chronic RA (Gomes et al. 2010), was greater in rats from the model control group in comparison to FA treated groups, indicating that FA attenuated CFA-induced alterations in CRP levels and could potentially recover its stability. The presence of RF, a diagnostic marker, is associated with an increased risk of developing RA in patients with mild arthritic symptoms (Jones et al. 1990; Nell et al. 2005). As expected, we observed significantly greater RF levels in rats from the model control group in comparison to the vehicle control, as RF levels in CFA induced arthritic rats are usually high (Nielen et al. 2006). However, RF levels were reduced in rats treated with prednisolone and FA (25 and 50 mg/kg). Thus, the ability of FA to protect cartilage and synovial membrane damage might additionally prevent systemic inflammation as it hinders injured synovial tissue from releasing cytokines.
Arthritic rats exhibited soft tissue swelling around the joints during the acute phase of the disease. Bones of rats from the model control group were unprotected as they were directly exposed to proteolytic enzymes that degrade cartilage (Bansod et al. 2011). Joint X-rays of rats from the FA and prednisolone treated groups showed reduced soft tissue inflammation and bone erosion, suggesting that FA can effectively treat the disease.
TGF-β, an immunosuppressive cytokine, inhibits the proliferation and production of cytokines and the cytotoxic activity of NK and T cells mediated by IL-12 (Chantry et al. 1989; Fox et al. 1992; Bright and Sriram 1998). Kuruvilla et al. (1991) reported that the systemic administration of TGF-β led to the prevention of Th1 cell-mediated autoimmune diseases. Additionally, Bright and Sriram (1998) demonstrated TGF-β had an inhibitory effect on IL-12-induced tyrosine phosphorylation and activation of JAK2 and tyrosine kinase 2 (TYK2) and STAT3 and STAT4 proteins in T cells. In the present study, rats from the model control group showed decreased levels of TGF-β, causing the overexpression of IL-12, which might be responsible for induced arthritis (Scott 1993). Nonetheless, FA treatment was effective in restoring levels of TGF-β and JAK2.
Cytokines play a critical role in the pathogenesis of RA and preventing the production and activation of cytokines inhibition can provide therapeutic benefits. The role of cytokines (TNF-α and ILs), macrophage colony stimulating factor, interferon, and platelet-derived growth factors have been reported in the pathogenesis of RA (McInnes and Schett 2011). In this study, we found that TNF-α levels were higher in CFA-induced arthritic rats, but such levels decreased when rats were treated with FA (25 and 50 mg/kg). Further, JAK2 levels in paw tissue homogenates were also reduced in FA treated groups. These results suggest that FA inhibits TNF induced alterations, such as tyrosine phosphorylation and activation of intracellular JAK2 (Guo et al. 1998). Thus, our results indicate that FA is an effective anti-arthritic agent.
Conclusion
Our results provide compelling evidence that FA exhibits anti-arthritic activity in CFA-induced arthritis by modulating cytokines, such as TNF-α and TGF-β, which leads to the inhibition of intracellular levels of Janus tyrosine kinases (JAK2). Consequently, FA can be considered an additional or alternative treatment for arthritis.
References
Andersen ML, Santos EHR, Seabra MDLV, da Silva AAB, Tufik S (2004) Evaluation of acute and chronic treatments with Harpagophytum procumbens on Freund's adjuvant-induced arthritis in rats. J Ethnopharm 91(2–3):325–330
Argiles JM, Lopez-Soriano FJ (2002) Catabolic proinflammatory cytokines. Curr Opin Clin Nutr Metab Care 1:245–251
Bansod S, Kagathara VG, Pujari RR, Patel VB, Ardeshna H (2011) Therapeutic effect of a poly-herbal preparation on adjuvant induced arthritis in wistar rats. Int J Pharm Pharm Sci 3(2):186–192
Bolling BW, Ji LL, Lee C, Parkin KL (2011) Dietary supplementation of ferulic acid and ferulic acid ethyl ester induces quinone reductase and glutathione-S-transferase in rats. Food Chem 124:1–6
Boyce EG (2006) Rheumatoid arthritis. In: Herfindal ET, Gourley DR (eds) Textbook of therapeutics: drugs and disease management, 8th edn. Williams & Wilkins, Baltimore
Bright JJ, Sriram S (1998) TGF-β INHIBITS IL-12-induced activation of Jak-STAT pathway in T lymphocytes. J Immunol 161(4):1772–1777
Chantry D, Turner M, Abney E, Feldmann M (1989) Modulation of cytokine production by TGF-β1. J Immunol 142:4295
Cunha FV, Gomes Bde S, Neto Bde S, Ferreira AR, de Sousa DP, de Carvalho e Martins MC, Oliveira FA (2015) Ferulic acid ethyl ester diminished Complete Freund's ADJUVANT-induced incapacitation through antioxidant and anti-inflammatory activity. Naunyn-Schmiedeberg's Arch Pharmacol 389(1):117–130
Durai M, Kim HR, Moudgil KD (2004) The regulatory C-terminal determinants within mycobacterial heat shock protein 65 are cryptic and cross-reactive with the dominant self homologs: implications for the pathogenesis of autoimmune arthritis. J Immunol 173(1):181–188
Fox FE, Capocasale RJ, Ford HC, Lamb RJ, Moore JS, Nowell PC (1992) Transforming growth factor-β inhibits human T cell proliferation through multiple targets. Lymphokine Cytokine Res 11:299–305
Gomes A, Bhattacharya S, Chakraborty M, Bhattacharjee P, Mishra R, Gomes A (2010) Anti-arthritic activity of Indian monocellate cobra (Naja kaouthia) venom on adjuvant induced arthritis. Toxicon 55:670–673
Guo D, Dunbar JD, Yang CH, Pfeffer LM, Donner DB (1998) Induction of Jak/STAT signaling by activation of the type 1 TNF receptor. J Immunol 160(6):2742–2750
Hassanzadeh P, Arbabi E, Atyabi F, Dinarvand R (2017) Ferulic acid exhibits antiepileptogenic effect and prevents oxidative stress and cognitive impairment in the kindling model of epilepsy. Life Sci 179:9–14
Heim MH (1999) The JAK-STAT pathway: signaling from the receptor to nucleus. J Recept Signal Trans Res 19:75–120
Islam S, Yoshida H, Matsuki N, Ono K, Nagasaka R, Ushio H, Guo Y, Hiramatsu T, Hosoya T, Murata T, Hori M, Ozaki H (2009) Antioxidant, free radical–scavenging, and NF-κB–inhibitory activities of phytosteryl ferulates: structure–activity studies. J Pharmacol Sci 111:328–337
Jones MG, Shipley ME, Hearn JP, Hay FC (1990) Specificity of rheumatoid factors in relation to the disease state in rheumatoid arthritis. Ann Rheum Dis 49:757–762
Kaur S, Kaira S, Kaushal S (2014) Systematic review of tofacitinib: a new drug for the management of rheumatoid arthritis. Clin Ther 36:1074–1086
Kim W, Park S, Choi C, Kim YR, Park I, Seo C, Youn D, Shin W, Lee Y, Choi D, Kim M, Lee H, Kim S (2016) Evaluation of anti-inflammatory potential of the new Ganghwaljetongyeum on adjuvant-induced inflammatory arthritis in rats. Evid Based Complement Altern Med 2016:1–10
Kuruvilla AP, Shah R, Hochwald GM, Liggitt HD, Palladino MA, Thorbecke GJ (1991) Protective effect of TGF β1 in experimental autoimmune diseases in mice. Proc Natl Acad Sci 88:2918–2921
Lagunin A, Zakharov A, Filimonov D, Poroikov V (2011) QSAR modelling of rat acute toxicity on the basis of PASS prediction. Mol Inform 30:241–250
Malemud CJ (2009) Recent advances in neutralizing the IL-6 pathway in arthritis. Open Access Rheumatol 1:133–150
Malemud CJ (2018) The role of the JAK/STAT signal pathway in rheumatoid arthritis. Ther Adv Musculoskel Dis 10(5–6):117–127
Mancuso C, Santangelo R (2014) Ferulic acid: Pharmacological and toxicological aspects. Food Chem Toxicol 65:185–195
McInnes IB, Schett J (2011) The pathogenesis of rheumatoid arthritis. N Engl J Med 365:2205–2219
Mowat AG (1971) Hematologic abnormalities in Rheumatoid arthritis. Sem Arthr Rheum 1(3):195–219
Nell VP, Machold KP, Stamm TA, Eberl G, Heinzl H, Uffmann M, Smolen JS, Steiner G (2005) Autoantibody profiling as early diagnostic and prognostic tool for rheumatoid arthritis. Ann Rheum Dis 64(12):1731–1736
Nielen MM, van Schaardenburg D, Reesink HW, Twisk JWR, van de Stadt RJ, van der Horst-Bruinsma IE, de Koning MH, Habibuw MR, Dijkmans BA (2006) Simultaneous development of acute phase response and autoantibodies in preclinical rheumatoid arthritis. Ann Rheum Dis 65:535–537
Ohori M (2008) Erk inhibitors as a potential new therapy for rheumatoid arthritis. Drug News Perspect 21:245–250
Ou S, Kwok KC (2004) Ferulic acid: pharmaceutical functions, preparation and applications in food. J Sci Food Agric 84:1261–1269
Panneerselvam L, Subbiah K, Arumugam A, Senapathy JG (2013) Ferulic acid modulates fluoride-induced oxidative hepatotoxicity in male Wistar rats. Biol Trace Elem Res 151:85–91
Patel MG, Pundarikakshudu K (2016) Anti-arthritic activity of a classical Ayurvedic formulation Vatari Guggulu in rats. J Tradit Complement Med 6(4):389–394
Patel SS, Shah PV (2013) Evaluation of anti-inflammatory potential of the multidrug herbomineral formulation in male Wistar rats against rheumatoid arthritis. J Ayurveda Integr Med 4(2):86–93
Pearson CM (1956) Development of arthritis, periarthritis and periostitis in rats given adjuvants. Exp Biol Med 91(1):95–101
Poroikov VV, Filimonov DA, Ihlenfeldt WD, Gloriozova TA, Lagunin AA, Borodina YV, Stepanchikova AV, Nicklaus MC (2003) PASS biological activity spectrum predictions in the enhanced open NCI database browser. J Chem Inf Comput Sci 43:228–236
Rall LC, Roubenoff R (2004) Rheumatoid cachexia: metabolic abnormalities, mechanisms and interventions. Rheumatology 10:1219–1223
Scott P (1993) IL-12: initiation cytokine for cell-mediated immunity. Science 260:496–497
Shelton DL, Zeller J, Ho WH, Pons J, Rosenthal A (2005) Nerve growth factor mediates hyperalgesia and cachexia in auto-immune arthritis. Pain 116:8–16
Sultana R (2012) Ferulic acid ethyl ester as a potential therapy in neurodegenerative disorders. Biochim Biophys Acta 1822:748–752
Sultana R, Ravagna A, Mohmmad-Abdul H, Calabrese V, Butterfield DA (2005) Ferulic acid ethyl ester protects neurons against amyloid beta-peptide(1–42)-induced oxidative stress and neurotoxicity: Relationship to antioxidant activity. J Eurochem 92:749–758
Tada Y, Tayama K, Aoki N (1999) Acute oral toxicity of ferulic acid, natural food additive, in rats. Ann Rep Tokyo Metr Lab PH 50:311–313
Thyagaraju BM (2008) Ferulic acid supplements abrogate oxidative impairments in liver and testis in the streptozotocin-diabetic rat. Zool Sci 25:854–860
Vetal S, Bodhankar SL, Mohan V, Thakurdesai PA (2013) Anti-inflammatory and anti-arthritic activity of type-A procyanidine polyphenols from bark of Cinnamomum zeylanicum in rats. Food Sci Hum Wellness 2:59–67
Vogel HG, Vogel WH (eds) (2002) Drug discovery and evaluation pharmacological assays, 2nd edn. Springer, Berlin
Wajant H, Pfizernmaier K, Scheurich P (2003) Tumor necrosis factor signaling. Cell Death Differ 10:45–65
Wang BH, Ou-Yang JP (2005) Pharmacological actions of sodium ferulate in cardiovascular system. Cardiovasc Drug Rev 23:161–172
Zeni ALB, Camargo A, Dalmagro AP (2017) Ferulic acid reverses depression-like behavior and oxidative stress induced by chronic corticosterone treatment in mice. Steroids 125:131–136
Zhang L, Al-Suwayeh SA, Hsiehc P, Fang J (2010) A comparison of skin delivery of ferulic acid and its derivatives: evaluation of their efficacy and safety. Int J Pharm 399:44–51
Zhang S, Wang P, Zhao P, Wang D, Zhang Y, Wang J, Chen L, Guo W, Gao H, Jiao Y (2018) Pretreatment of ferulic acid attenuates inflammation and oxidative stress in a rat model of lipopolysaccharide-induced acute respiratory distress syndrome. Int J Immunopathol Pharmacol 31:1–9
Author information
Authors and Affiliations
Corresponding author
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
About this article
Cite this article
Zhu, L., Zhang, Z., Xia, N. et al. Anti-arthritic activity of ferulic acid in complete Freund’s adjuvant (CFA)-induced arthritis in rats: JAK2 inhibition. Inflammopharmacol 28, 463–473 (2020). https://doi.org/10.1007/s10787-019-00642-0
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s10787-019-00642-0