Abstract
High scores of lymphocyte-to-high-density lipoprotein cholesterol ratio (lymphocyte-to-HDL-c) may be a new indicator of inflammation and metabolic syndrome. Here, we investigated the associations of the lymphocyte-to-HDL-c with traditional and non-traditional cardiometabolic risk markers in subjects at high cardiovascular risk. This study is a cross-sectional analysis with subjects assisted in a Secondary Health Care (n = 581, age = 63.06 ± 13.86 years; 52.3% women). Lymphocyte-to-HDL-c ratio were assessed by routine laboratory tests. Anthropometric and/or biochemical variables were used to calculate traditional (body mass index – BMI, and waist-to-height ratio – WHtR) and non-traditional (lipid accumulation product index—LAP, visceral adiposity index—VAI, deep-abdominal-adipose-tissue index—DAAT, atherogenic index of plasma—AIP, and waist-hypertriglyceridemic phenotype—HTGW) cardiometabolic risk markers. Furthermore, anthropometric measurement waist circumference (WC), blood pressure, metabolic syndrome (MS), and biochemical markers (lipid and glycemic profile) were considered traditional markers of cardiometabolic risk. Pearson's chi-square test, Poisson regression with robust variance, or multinomial logistic regression were performed (α = 0.05). Individuals with a high lymphocyte-HDL-c ratio (> 0.84, 3rd tertile) were associated with the HTGW phenotype, high VAI, high LAP, hypertriglyceridemia, high AIP, high very low-density lipoprotein-cholesterol (VLDL-c), pre-diabetes, and 3 and 4 MS components compared with individuals in the first tertile, independent of confounders. Our findings supported the lymphocyte-to-HDL-c ratio as a potential biomarker during the screening of subjects at high cardiovascular risk.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Background
Obesity is a chronic disease characterized by low-grade inflammation [1, 2] and is reaching alarming proportions worldwide [3], directly contributing to metabolic dysregulation and the development of cardiovascular risk factors, as well as being an independent risk for cardiovascular events and mortality [4].
According to the World Health Organization [5], obesity is characterized by an abnormal or excessive accumulation of fat that poses a risk to health. This accumulation occurs when there is an imbalance between calorie intake and energy expenditure, resulting in excess energy being stored in adipocytes. The hyperplasia and hypertrophy of adipose tissue result in oxygen depletion and the establishment of cellular distress, which in turn leads to the recruitment of macrophages [6], comprising up to 40% of the cells in obese adipose tissue when compared with under 10% in lean individuals [7]. Both adipocytes and macrophages produces pro-inflammatory cytokines with potential to alter hematologic parameters, particularly regarding white blood cells [8, 9].
The Body Mass Index (BMI) is a commonly used diagnostic tool in the current obesity classification system. BMI is a useful measure in epidemiological studies due to its simplicity and low cost. However, its ability to accurately assess an individual's body composition and associated cardiovascular risk has been questioned [10, 11]. This finding supports the need to establish other indices that consider abdominal adiposity and body fat distribution when assessing obesity-related cardiometabolic risk. Waist circumference (WC) [12] and waist-to-height ratio (WHtR) [13] are traditional indicators of central obesity and are well established in the identification of cardiovascular risk [4].
Alternatively, some non-traditional cardiometabolic risk markers are easy-to-use indicators of visceral adiposity which could combine anthropometric and lipid metabolism indicators, contributing to early diagnosis and treatment of individuals at cardiometabolic risk [14], such as deep-abdominal-adipose-tissue index (DAAT) [15], visceral adiposity index (VAI) [16], lipid accumulation product index (LAP) [17], atherogenic index of plasma (AIP) [18], and waist-hypertriglyceridemic phenotype (HTGW phenotype) [19].
In addition to the traditional inflammatory markers, the neutrophil–lymphocyte ratio, platelet-lymphocyte ratio, and monocyte-lymphocyte ratio have been associated with inflammation in inflammatory diseases such as diabetic cardiomyopathy [20] and Crohn's disease [21]. Furthermore, obesity has been associated with relative and sometimes absolute lymphocytosis, and the connection between lymphocytosis and cardiometabolic risk markers has aroused the interest of the scientific community [22, 23]. In this context, the lymphocyte-to-high-density lipoprotein cholesterol (lymphocyte-to-HDL-c) ratio has emerged as a novel inflammatory and metabolic syndrome biomarker that has the advantage of being cost-effective and easily measurable [24,25,26,27]. Because obesity can lead to a pro-inflammatory state and dyslipidemia and both disruptions could increase cardiovascular risk, we suspected that the lymphocyte-to-HDL-c has the potential to be a cardiometabolic risk marker with great applicability. However, to the best of our knowledge, all available studies enrolled West Asian populations [24,25,26,27] and the relationship between lymphocyte account and the risk of cardiovascular events remains controversial [28]. Evidence shows that Asians are at a higher risk of cardiometabolic disease at a lower BMI than other races [29] and this increases the need for studies assessing such relationships in distinct populations. Therefore, we aimed to evaluate the associations of lymphocyte-to-HDL-c with traditional and non-traditional cardiometabolic risk markers in a Brazilian population at high cardiovascular risk.
Methods
Study Design and Population
The STrengthening the Reporting of OBservational Studies in Epidemiology (STROBE) guideline was used to report the data presented in this article (https://www.strobe-statement.org/) [30]. This is a cross-sectional study enrolling baseline data from adults and older adults (aged 18 years or older) referred for the treatment of non-communicable chronic diseases from 2015 to 2020 in a Secondary Healthcare unit situated at Zona da Mata, Minas Gerais, Brazil. The referral criteria adopted by the service, according to the assistance sector, were as follows [31]:
-
1.
Cardiology: hypertensive individuals with high and very high cardiovascular risk determined by the Framingham Score [32]; suspected secondary arterial hypertension; resistant arterial hypertension;
-
2.
Endocrinology: individuals with type 2 diabetes mellitus (T2DM) in the following cases i) use of insulin with poor metabolic control (considered glycated hemoglobin (HbA1C) > 9%); ii) use of full-dose oral antidiabetics that have poor metabolic control; iii) impossibility to perform insulin treatment at the Primary Healthcare;
-
3.
Nephrology: individuals with systemic arterial hypertension and/or T2DM and i) chronic kidney disease (CKD) in stages 3B, 4 or 5 (non-dialysis); ii) estimated annual glomerular filtration loss ≥ 5mL/min/year; iii) proteinuria >1g/day or proteinuria <1g/day + hematuria; iv) abrupt increase in serum creatinine (≥ 30%); v) 25% decrease in estimated glomerular filtration when starting any medication that blocks the renin-angiotensin-aldosterone axis.
All active records were assessed, and the exclusion criteria were the absence of data on lymphocyte and/or HDL-c from baseline. Of 1,179 records, 581 had complete data on lymphocyte-to-HDL-c and thus were included in this study (Fig. 1).
The study was conducted by consulting the institution's records and did not directly involve any patient. The managers signed the Term of Institutional Consent and the survey followed the precepts of Resolutions 466/12 [33] and 580/18 [34], the last one regarding the ethical specificities of surveys with strategic interest to the Brazilian Unified Healthcare System. The study protocol was approved by the Ethics Committee of the Federal University of Viçosa (opinion: 5.164.152, CAAE: 50015621.4.0000.5153).
Data Collection
Sociodemographic, lifestyle, and clinical data were extracted from records of active patients. Marital status was classified as “married” and “unmarried/not married” (single or widowed or other). Health self-perception was assessed by the question: “How do you classify your health status?” and classified as positive (“excellent, very good or good”) or negative (“regular or poor”) [35]. Sleep self-perception was assessed by the questions adapted from Zucconi and Ferri [36]: “Are you dissatisfied with your sleep?”, “Are you sleepy or fatigued during daily activities?”, “Does the partner or other observers complain of unusual sleep behavior (i.e., snoring, pauses in breathing or leg movements, and/or daytime drowsiness or fatigue)?”. Sleep condition was classified according to the presence of fatigue/irregular/dissatisfied sleep sensations.
Blood pressure (mmHg), body weight (kg), height (m), and WC (cm) were routinely measured by trained nurses. Blood pressure is measured in the antecubital region using a digital pressure gauge (Omron®, model HEM 7122) following standard clinical protocols. Body weight was obtained using an electronic scale with a capacity of 300 kg and a division of 100 g with individuals wearing light clothes. The height was measured using a wall-mounted vertical stadiometer with a maximum length of 220 cm and a precision of 1 mm with an acrylic display, with users barefoot, upright, with their heels against the wall. WC was measured at the umbilical level using an inelastic measuring tape.
Blood samples and analyses were performed by accredited laboratories through venipuncture following standard protocols. Individuals were instructed to proceed with blood collection after 12 h of overnight fasting. Data from the following biochemical parameters were assessed: differential blood cell counts (red blood cells, platelets, total white blood cells, lymphocytes, monocytes, neutrophils, basophils, and eosinophils) (unit/mm3), glucose (mg/dL), HbA1C (%), triglycerides (TG) (mg/dL), total cholesterol (TC) (mg/dL) and the fractions high-density lipoprotein-cholesterol (HDL-c) (mg/dL), low-density lipoprotein-cholesterol (LDL-c) (mg/dL), and very low-density lipoprotein-cholesterol (VLDL-c) (mg/dL).
Traditional and Non-Traditional Cardiometabolic Risk Markers
Anthropometric and/or biochemical variables were used to calculate traditional (BMI and WHtR) and non-traditional (LAP, VAI, DAAT, AIP, and HTGW) cardiometabolic risk markers (Chart 1). Furthermore, anthropometric measurement (WC), blood pressure, metabolic syndrome (MS), and biochemical markers (lipid and glycemic profile) were considered traditional markers of cardiometabolic risk in the present study.
Obesity was defined by a BMI ≥ 30.00 kg/m2 [37]. Abdominal obesity is defined by the presence of WC ≥ 80 or 88 cm for women and ≥ 94 or 102 cm for men [12]. WtHR was classified according to the cut-off point (< and ≥ 0.5) [13]. The presence of MS [38], altered lipid profile (high triglycerides ≥ 150 mg/dl; high LDL-c ≥ 160 mg/dl) [39] or glucose status (pre-T2DM: fasting glucose between 100 to 125 mg/dL and/or HbA1C between 5.7 to 6.4%; or T2DM: fasting glucose > 125 mg/dL and/or HbA1C > 6.4%) [40] was determined. For MS, the component HDL-c was excluded because the marker is used in the lymphocyte-to-HDL, which was the focus of the paper. Furthermore, due to the absence of well-established cut-off values, the markers DAAT [15], VAI [16], LAP [17], and AIP [18] were classified according to median values. Those using antihypertensive medications and/or with systolic and diastolic blood pressure ≥ 140 mmHg and ≥ 90 mmHg, respectively, were considered to have hypertension [41].
Statistical Analysis
Statistical analysis was performed using the SPSS version 21.0 and STATA version 13.0. The level of significance in two-tailed tests was set at 5%. Categorical variables were assessed according to lymphocyte-to-HDL-c tertiles through linear trend chi-square and presented as absolute and relative frequencies. Poisson regression with robust variance was performed when the outcome prevalence was ≥ 10%. This analysis evaluated the association between lymphocyte-to-HDL-c tertiles (independent variable) and cardiometabolic risk markers (binary dependent variables). The absence of the outcome was considered the category of reference. Multinomial logistic regression was used to evaluate the association between lymphocyte-to-HDL-c tertiles (independent variable) according to fasting glucose categories (normal, pre-diabetes, and diabetes). Normal fasting glucose was considered the reference category. Adjustment variables were selected based on statistical criteria (p-value ≤ 0.2) in the relation between lymphocyte-to-HDL-c tertiles with sociodemographic, clinical, and lifestyle variables. Figure 2 represents the theoretical model to summarize the relationships between study variables.
Theoretical model to summarize the relationships between study variables. Abbreviations: CKD, chronic kidney disease; HDL-c, high-density lipoprotein cholesterol; DM, diabetes mellitus; MS, metabolic syndrome. By https://www.dagitty.net/ [42]
Assuming a prevalence of HTGW phenotype in the exposed (third Lymphocyte/HDL-c ratio tertile) and non-exposed (first Lymphocyte/HDL-c ratio tertile) groups (42.5% and 26.4%, respectively), bilateral alpha, the analysis had approximately 90% power to detect a difference of this magnitude or larger (prevalence ratio = 1.6%; difference in prevalence = 16.1%), according to the OpenEpi online software [43] (https://www.openepi.com/Menu/OE_Menu.htm).
Results
Of the 581 participants included in the study, the majority were more like older adults (63.9%), married (58.1%), and female (52.3%). Furthermore, 87.4% had a family history of chronic diseases, 70.1% used multiple medications, 86.2% had hypertension, and 52.7% had three or four MS components.
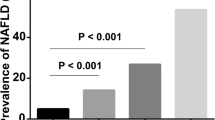
Lymphocyte-to-HDL-c had a mean of 0.79 (sd 0.32) in our sample. The prevalence of older adults, married subjects, the practice of physical activity, diabetes history, and use of diabetes drugs increased, while smoking and chronic kidney disease history decreased, across lymphocyte-to-HDL-c tertiles (Table 1). Moreover, values of LAP, VAI, triglycerides, VLDL, and AIP increased according to the increase in lymphocyte-to-HDL-c tertiles. The prevalence of subjects with HTGW phenotype, diabetes, and three or four MS components also increased across the tertiles (Table 2).
In regression analysis, the lymphocyte-to-HDL-c ratio was positively associated with traditional and non-traditional markers of cardiometabolic risk. Those participants included in the third tertile of lymphocyte-to-HDL-c had a higher prevalence of HTGW phenotype, pre-diabetes, diabetes, hypertriglyceridemia, and 3 and 4 MS components compared to those in the first tertile. Also, the higher prevalence of subjects with high VAI, LAP, VLDL, and AIP was associated with the 3th tertile of lymphocyte-to-HDL-c > 0.84. All results remain significant after adjustment for age, marital status, practice of physical activity, smoking history, history of diabetes, and chronic kidney disease (Table 3).
Discussion
In this cross-sectional study, we investigated the association between lymphocyte-to-HDL-c with traditional and non-traditional cardiometabolic risk markers in subjects at high cardiovascular risk assisted in a Secondary Healthcare service. The main findings of this study were as follows: i) Sociodemographic and clinical variables were distinctly associated with the presence of higher lymphocyte-to-HDL-c ratio; ii) Increased lymphocyte-to-HDL-c ratio is consistently associated with traditional cardiometabolic risk markers, such as higher number of MS components, pre-diabetes, diabetes, and hypertriglyceridemia; iii) Lymphocyte-to-HDL-c ratio is also positively associated with several non-traditional cardiometabolic risk markers such as LAP, VAI, AIP, and HTGW phenotype; iv) The value of 0.84 for high lymphocyte-to-HDL-c ratio presents significant associations after adjustment for potential confounders. To the best of our knowledge, this study is the first to focus on the relationship between lymphocyte-to-HDL-c as a novel and indirect cardiometabolic risk marker in Brazilians.
Obesity is characterized by a low-intensity chronic inflammatory process caused by excessive and inappropriate activation of the immune system, affecting the proportion of circulating cells, which results in exacerbation of the metabolic abnormalities of obesity [22]. Previous studies have demonstrated that total peripheral lymphocyte counts assessed isolated are positively associated with adiposity, visceral adipose tissue, and the presence of metabolic disruptions [22, 23]. Therefore, changes in circulating lymphocytes could represent a key factor in the study of obesity and its associated co-morbidities, since these changes could reflect adipose inflammation in obesity [44] and low-grade systemic inflammation is considered the link between obesity and cardiometabolic disorders [45]. On the other hand, important findings from the Framingham [46], Tromsø Heart [47], and Prospective Cardiovascular Munster (PROCAM) [48] studies revealed an inverse and consistent relationship between serum concentrations of HDL-c and the risk of cardiovascular disease. Thus, the incorporation of HDL-c in the lymphocyte-to-HDL-c seems to be a more powerful indicator of cardiometabolic risk. Furthermore, our results were consistent with some of the previous studies reporting increased lymphocyte-to-HDL-c in subjects with MS [24,25,26,27]. MS is a combination of metabolic factors related to obesity, involving central obesity, hypertension, dyslipidemia, impaired glucose tolerance, and insulin resistance.
The literature has also supported mechanisms for the positive association of lymphocyte-to-HDL-c and traditional and non-traditional cardiometabolic risk markers and further indicated the bidirectional nature of such relationships [22, 25, 49,50,51,52]. Adipose tissue is a primary source of inflammatory mediators which could alter hematologic indicators, particularly the white blood cell, culminating in peripheral blood lymphocytosis [8, 9]. However, the contribution of adipose tissue over systemic inflammation appears to be site dependent. Central obesity, characterized by fat deposition in visceral adipose tissue, can increase the pro-inflammatory status than peripheral obesity, marked by subcutaneous adipose tissue [53]. In fact, increased visceral adipose tissue can injure adipocyte metabolic homeostasis and promote abnormal pro-inflammatory signaling, activating resident immune cells to release increased amounts of pro-inflammatory mediators with peripheral action [54]. In the present study, markers of central obesity (VAI, LAP, and HTGW phenotypes), and not general adiposity makers (obesity by BMI). This outcome could reflect the influence of central obesity in cardiometabolic risk accessed by peripheral lymphocytosis.
Increase in total lymphocyte appears to play also a prominent role during the early stages of obesity, even when their comorbidities are not present [22, 23], since the increase in lymphocyte-to-HDL-c is present in individuals with high visceral adipose tissue irrespective of the presence of MS [22]. However, visceral fat accumulation is a well-established predictor of enhanced risks for diabetes, metabolic syndrome, and cardiovascular diseases [55, 56] while increased total lymphocyte count in peripheral blood would be responsible for amplifying the inflammatory response in patients with central obesity [22], leading to metabolic disruptions such as insulin resistance and increasing cardiovascular risk. Therefore, in the present study, the prominent role of visceral adipose tissue in systemic inflammation and consequently in lymphocytosis could explain the positive and consistent associations between lymphocyte-to-HDL-c with markers of central obesity and metabolic disruptions. On the other hand, metabolic disruptions could also change lymphocyte-to-HDL-c. Insulin could stimulate white blood cell proliferation and down-regulate HDL-c [50,51,52], even so, disruptions in glucose metabolism may affect the lymphocyte-to-HDL-c. These findings reinforce the interest in the use of lymphocyte-to-HDL-c as a novel cardiometabolic biomarker.
Furthermore, our results showed an increase in lymphocyte-to-HDL-c as the cardiovascular risk indicators increased, showing positive associations. However, previous study indicates that this relationship could be shifted in patients with established coronary disease [28]. The authors of the controversial study [28] discussed that the results were unexpected, since atherosclerotic plaque is characterized by the migration of monocytes/macrophages and lymphocytes from the peripheral space into subendothelial layers of arteries, and a parallel increase in absolute or proportionate lymphocyte counts could be postulated to maintain equilibrium with plaque fractions. Thereby, immune system cells interact in a complex network and more studies are needed to better investigate the dynamics of lymphocyte counts in individuals with different degrees of cardiovascular risk.
In the present study, we investigated the role of the novel but easily measurable, low-cost blood biomarker, which employs the use of two biochemical tests that have been widely investigated in clinical practice, the lymphocyte-to-HDL-c ratio, in accessing cardiometabolic risk in a sample of Brazilians at the high cardiovascular risk. However, that recent scientific literature indicates other biomarkers that may be sensitive in the diagnosis of cardiometabolic risk among this population. For example, the anti-aging gene Sirtuin 1, a nicotinamide adenine dinucleotide (NAD +) dependent histone deacetylase, is a regulator of mitochondrial biogenesis, cell metabolism, stress response and transcription [57, 58]. This leads to a potent anti-inflammatory, insulin sensitizing, and anti-atherosclerosis effect [58]. Consequently, Sirtuin 1 is critical to the maintenance of cardiovascular function and hepatic lipid metabolism and its expression has been associated with the risk for diabetes, MS, and cardiovascular disease. Thus, it represents a promising biomarker for cardiovascular disease that may be used for early diagnosis and more sensitive assessment of cardiovascular risk in distinct populations [59, 60]. Furthermore, diet and dietary specific compounds can modulate Sirtuin 1 activity, by activation (calorie restriction, zinc, magnesium, resveratrol) [58, 61] or inhibition (alcohol, bacterial lipopolysaccharides) [61]. Thus, Sitruin 1 could also reflect early changes in cardiovascular risks from the diet therapy. New studies that comparatively evaluate the use of the lymphocyte-to-HDL-c in relation to epigenetic markers may be useful in the search for cardiometabolic risk markers that have a good cost–benefit ratio in specific populations.
Limitations
The present study has some limitations. First, collected data represents outpatient follow-up routine and there was an absence of other inflammatory biomarkers and cytokines to attest the results. Secondly, despite the relatively large sample enrolled, this is a retrospective single-center cross-sectional study and inference is limited. Thirdly, as the study involved subjects at high cardiovascular risk assisted in a Secondary Healthcare service, ROC curves were not appropriate and tertile cut-off points cannot be used in other ethnic groups.
Conclusion
In conclusion, lymphocyte-to-HDL-c ratio is positively associated with traditional (MS components, pre-diabetes, diabetes, and hypertriglyceridemia) and non-traditional (LAP, VAI, AIP, and HTGW phenotype) cardiometabolic risk markers among individuals assisted at the Secondary Health Care, supporting its use as a simple and adjuvant biomarker during the screening of subjects with high cardiovascular risk. A prospective population-based cohort study is now needed for definitive considerations.
Data Availability
The datasets analyzed during the current study are not publicly available as they are still used in other studies. However, they are available from the corresponding author upon reasonable request.
Change history
29 July 2024
A Correction to this paper has been published: https://doi.org/10.1007/s10753-024-02111-5
References
Hermsdorff, H.H., M.Á. Zulet, B. Puchau, and J.A. Martínez. 2011. Central adiposity rather than total adiposity measurements are specifically involved in the inflammatory status from healthy young adults. Inflammation. https://doi.org/10.1007/s10753-010-9219-y.
Hermsdorff, H.H., A.C. Volp, B. Puchau, K.B. Barbosa, M.A. Zulet, and J. Bressan. 2012. Contribution of gender and body fat distribution to inflammatory marker concentrations in apparently healthy young adults. Inflammation Research. https://doi.org/10.1007/s00011-011-0429-z.
Tiwari, A., P. Balasundaram. 2023. Public health considerations regarding obesity. In StatPearls [Internet]. Treasure Island (FL): StatPearls Publishing. PMID:34283488. https://www.ncbi.nlm.nih.gov/books/NBK572122/. Accessed 27 July 2023.
Powell-Wiley, T.M., P. Poirier, L.E. Burke, J.P. Després, P. Gordon-Larsen, and C.J. Lavie. 2021. Obesity and cardiovascular disease: A scientific statement from the american heart association. Circulation. https://doi.org/10.1161/CIR.0000000000000973.
World Health Organization. 2023. Obesity Overview. https://www.who.int/health-topics/obesity#tab=tab_1. Accessed 27 July 2023.
Grosso, G., D. Laudisio, E. Frias-Toral, L. Barrea, G. Muscogiuri, S. Savastano, and A. Colao. 2022. Anti-inflammatory nutrients and obesity-associated metabolic-inflammation: State of the art and future direction. Nutrients. https://doi.org/10.3390/nu14061137.
Weisberg, S.P., D. McCann, M. Desai, M. Rosenbaum, R.L. Leibel, and A.W. Ferrante. 2003. Obesity is associated with macrophage accumulation in adipose tissue. The Journal of Clinical Investigation. https://doi.org/10.1172/jci19246.
Gregor, M.F., and G.S. Hotamisligil. 2011. Inflammatory mechanisms in obesity. Annual Review of Immunology. https://doi.org/10.1146/annurev-immunol-031210-101322.
Fantuzzi, G. 2005. Adipose tissue, adipokines, and inflammation. The Journal of Allergy and Clinical Immunology. https://doi.org/10.1016/j.jaci.2005.02.023.
Gómez-Ambrosi, J., C. Silva, J.C. Galofré, J. Escalada, S. Santos, and D. Millán. 2012. Body mass index classification misses subjects with increased cardiometabolic risk factors related to elevated adiposity. International Journal of Obesity. https://doi.org/10.1038/ijo.2011.100.
Nazare, J.A., J. Smith, A.L. Borel, P. Aschner, P. Barter, and L. Van Gaal. 2015. Usefulness of measuring both body mass index and waist circumference for the estimation of visceral adiposity and related cardiometabolic risk profile (from the INSPIRE ME IAA study). The American Journal of Cardiology. https://doi.org/10.1016/j.amjcard.2014.10.039.
Tsai, A.G., and T.A. Wadden. 2013. In the clinic: Obesity. Annals of Internal Medicine. https://doi.org/10.7326/0003-4819-159-5-201309030-01003.
Gibson, S., and M. Ashwell. 2020. A simple cut-off for waist-to-height ratio (0·5) can act as an indicator for cardiometabolic risk: Recent data from adults in the Health Survey for England. British Journal of Nutrition. https://doi.org/10.1017/S0007114519003301.
Golabi, S., S. Ajloo, F. Maghsoudi, M. Adelipour, and M. Naghashpour. 2021. Associations between traditional and non-traditional anthropometric indices and cardiometabolic risk factors among inpatients with type 2 diabetes mellitus: A cross-sectional study. Journal of International Medical Research. https://doi.org/10.1177/03000605211049960.
Brundavani, V., S.R. Murthy, and A.V. Kurpad. 2006. Estimation of deep-abdominal-adipose-tissue (DAAT) accumulation from simple anthropometric measurements in Indian men and women. European Journal of Clinical Nutrition. https://doi.org/10.1038/sj.ejcn.1602366.
Amato, M.C., C. Giordano, M. Galia, A. Criscimanna, S. Vitabile, and M. Midiri. 2010. Visceral adiposity index: A reliable indicator of visceral fat function associated with cardiometabolic risk. Diabetes Care. https://doi.org/10.2337/dc09-1825.
Kahn, H.S. 2005. The “lipid accumulation product” performs better than the body mass index for recognizing cardiovascular risk: A population-based comparison. BMC Cardiovascular Disorders. https://doi.org/10.1186/1471-2261-5-26.
Cai, G., G. Shi, S. Xue, and W. Lu. 2017. The atherogenic index of plasma is a strong and independent predictor for coronary artery disease in the Chinese Han population. Medicine (Baltimore). https://doi.org/10.1097/MD.0000000000008058.
Lemieux, I., A. Pascot, C. Couillard, B. Lamarche, A. Tchernof, and N. Alméras. 2000. Hypertriglyceridemic waist. Circulation. https://doi.org/10.1161/01.CIR.102.2.179.
Saad, H., H.A. Soliman, B. Mahmoud, A.A. Moneim, and M.Y. Zaky. 2023. The pathogenic role of oxidative stress, cytokine expression, and impaired hematological indices in diabetic cardiovascular diseases. Inflammation. https://doi.org/10.1007/s10753-022-01718-w.
Soufli, I., A. Hablal, S. Bessaad, M. Amri, M. Labsi, and R.S. Boussa. 2023. Nitric oxide, neutrophil/lymphocyte, and platelet/lymphocyte ratios as promising inflammatory biomarkers in complicated crohn’s disease: Outcomes of corticosteroids and anti-tnf-α therapies. Inflammation. https://doi.org/10.1007/s10753-023-01796-4.
Rodríguez, C.P., M.C. González, C.A. Aguilar-Salinas, and O. Nájera-Medina. 2018. Peripheral lymphocytes, obesity, and metabolic syndrome in young adults: An immunometabolism study. Metabolic Syndrome and Related Disorders. https://doi.org/10.1089/met.2018.0005.
Ryder, E., M. Diez-Ewald, J. Mosquera, E. Fernández, A. Pedreañez, and R. Vargas. 2014. Association of obesity with leukocyte count in obese individuals without metabolic syndrome. Diabetes & Metabolic Syndrome. https://doi.org/10.1016/j.dsx.2014.09.002.
Chen, T., H. Chen, H. Xiao, H. Tang, Z. Xiang, X. Wang, et al. 2020. Comparison of the value of neutrophil to high-density lipoprotein cholesterol ratio and lymphocyte to high-density lipoprotein cholesterol ratio for predicting metabolic syndrome among a population in the Southern Coast of China. Diabetes, Metabolic Syndrome and Obesity. https://doi.org/10.2147/dmso.s238990.
Chen, H., C. Xiong, X. Shao, J. Ning, P. Gao, and H. Xiao. 2019. Lymphocyte to high-density lipoprotein ratio as a new indicator of inflammation and metabolic syndrome. Diabetes, Metabolic Syndrome and Obesity. https://doi.org/10.2147/dmso.s219363.
Yu, S., X. Guo, G. Li, H. Yang, L. Zheng, and Y. Sun. 2021. Lymphocyte to high-density lipoprotein ratio but not platelet to lymphocyte ratio effectively predicts metabolic syndrome among subjects from rural china. Frontiers in Cardiovascular Medicine. https://doi.org/10.3389/fcvm.2021.583320.
Kohsari, M., M. Moradinazar, Z. Rahimi, F. Najafi, Y. Pasdar, and E. Shakiba. 2022. New inflammatory biomarkers (lymphocyte and monocyte percentage to high-density lipoprotein cholesterol ratio and lymphocyte to monocyte percentage ratio) and their association with some cardiometabolic diseases: Results from a large Kurdish cohort study in Iran. Wiener Klinische Wochenschrift. https://doi.org/10.1007/s00508-022-02029-8.
Horne, B.D., J.L. Anderson, J.M. John, A. Weaver, T.L. Bair, and K.R. Jensen. 2005. Which white blood cell subtypes predict increased cardiovascular risk? Journal of the American College of Cardiology. https://doi.org/10.1016/j.jacc.2005.02.054.
Min, L.Y., R.B. Islam, N. Gandrakota, and M.K. Shah. 2022. The social determinants of health associated with cardiometabolic diseases among Asian American subgroups: A systematic review. BMC Health Services Research. https://doi.org/10.1186/s12913-022-07646-7.
von Elm, E., Altman, D. G., Egger, M., Pocock, S. J., Gøtzsche, P. C., Vandenbroucke, J. P., and STROBE Initiative. 2008. The Strengthening the Reporting of Observational Studies in Epidemiology (STROBE) statement: guidelines for reporting observational studies. Journal of Clinical Epidemiology. https://doi.org/10.1016/j.jclinepi.2007.11.008
Minas Gerais. Secretaria de Estado de Saúde. 2015. Protocolo Clínico dos Centros Hiperdia Minas. https://www.saude.mg.gov.br/images/documentos/Protocolo-Clinico-dos-Centros-Hiperdia-Minas_03-2015-1.pdf. Accessed 27 July 2023.
D’Agostino, R.B., R.S. Vasan, M.J. Pencina, P.A. Wolf, M. Cobain, and J.M. Massaro. 2008. General cardiovascular risk profile for use in primary care: The Framingham Heart Study. Circulation. https://doi.org/10.1161/circulationaha.107.699579.
Brasília, DF. 2012. Resolução nº 466, de 12 de dezembro de 2012. Dispõe sobre diretrizes e normas regulamentadoras de pesquisas envolvendo seres humanos. Diário Oficial [da] República Federativa do Brasil. https://conselho.saude.gov.br/resolucoes/2012/Reso466.pdf. Accessed 28 July 2023.
Brasília, DF. 2018. Resolução nº 580, de 22 de março de 2018. Dispõe sobre as especificidades éticas das pesquisas de interesse estratégico para o SUS. Diário Oficial [da] República Federativa do Brasil. https://conselho.saude.gov.br/resolucoes/2018/Reso580.pdf. Accessed 28 July 2023.
Iser, B.P., R.M. Claro, E.C. de Moura, D.C. Malta, and O.L. Neto. 2011. Risk and protection factors for chronic non communicable diseases by telephone survey - VIGITEL - 2009. Revista Brasileira de Epidemiologia. https://doi.org/10.1590/S1415-790X2011000500010.
Zucconi, M.A., and R.A. Ferri. 2014. Assessment of sleep disorders and diagnostic procedures. European Sleep Research Society 23 (95): 110.
Clinical Guidelines on the Identification. 1998. Evaluation, and Treatment of Overweight and Obesity in Adults-The Evidence Report National Institutes of Health. Obesity Research 6 (Suppl 2): 51S-209S. https://doi.org/10.1002/j.1550-8528.1998.tb00690.x.
Grundy, S.M., I.J. Neeland, A.T. Turer, and G.L. Vega. 2014. Ethnic and gender susceptibility to metabolic risk. Metabolic Syndrome and Related Disorders. https://doi.org/10.1089/met.2013.0113.
Faludi, A.A., Saraiva JF. de Oliveira, A.P. Chacra, H.T. Bianco, and Neto. 2017. Atualização da Diretriz Brasileira de Dislipidemias e Prevenção da Aterosclerose – 2017. Arquivos Brasileiros de Cardiologia. https://doi.org/10.5935/abc.20170121.
Cobas, R., Rodacki, M., Giacaglia, L., Calliari, L., Noronha, R., Valerio, C., Custódio, J., Santos, R., Zajdenverg, L., Gabbay, G., Bertoluci, M. 2023. Diagnóstico do diabetes e rastreamento do diabetes tipo 2. Diretriz Oficial da Sociedade Brasileira de Diabetes. ISBN: 978-85-5722-906-8. https://doi.org/10.29327/557753.2022-2. Accessed 28 July 2023.
Barroso, W.K., C.I. Rodrigues, L.A. Bortolotto, M.A. Mota-Gomes, A.A. Brandão, and A.A.D.M. Feitosa. 2021. Brazilian guidelines of hypertension - 2020. Arquivos Brasileiros de Cardiologia. https://doi.org/10.36660/abc.20201238.
Textor, J., B. van der Zander, M.S. Gilthorpe, M. Liśkiewicz, and G.T. Ellison. 2016. Robust causal inference using directed acyclic graphs: The R package ‘dagitty.’ International Journal of Epidemiology. https://doi.org/10.1093/ije/dyw341.
Sullivan, K.M., A. Dean, and M.M. Soe. 2009. OpenEpi: A web-based epidemiologic and statistical calculator for public health. Public Health Reports. https://doi.org/10.1177/003335490912400320.
Donninelli, G., M. Cornò, M. Pierdominici, B. Scazzocchio, R. Varì, and B. Varano. 2017. Distinct blood and visceral adipose tissue regulatory t cell and innate lymphocyte profiles characterize obesity and colorectal cancer. Frontiers in Immunology. https://doi.org/10.3389/fimmu.2017.00643.
Kim, J.A., and K.M. Choi. 2020. Newly discovered adipokines: Pathophysiological link between obesity and cardiometabolic disorders. Frontiers in Physiology. https://doi.org/10.3389/fphys.2020.568800.
Castelli, W.P., J.T. Doyle, T. Gordon, C.G. Hames, M.C. Hjortland, and S.B. Hulley. 1977. HDL cholesterol and other lipids in coronary heart disease. The cooperative lipoprotein phenotyping study. Circulation. https://doi.org/10.1161/01.cir.55.5.767.
Mora, S., R.J. Glynn, and P.M. Ridker. 2013. High-density lipoprotein cholesterol, size, particle number, and residual vascular risk after potent statin therapy. Circulation. https://doi.org/10.1161/circulationaha.113.002671.
Assmann, G., H. Schulte, A. Von Eckardstein, and Y. Huang. 1996. High-density lipoprotein cholesterol as a predictor of coronary heart disease risk. The PROCAM experience and pathophysiological implications for reverse cholesterol transport. Atherosclerosis. https://doi.org/10.1016/0021-9150(96)05852-2.
Hagita, S., M. Osaka, K. Shimokado, and M. Yoshida. 2011. Adipose inflammation initiates recruitment of leukocytes to mouse femoral artery: Role of adipo-vascular axis in chronic inflammation. PLoS ONE. https://doi.org/10.1371/journal.pone.0019871.
Pasini, E., V. Flati, S. Paiardi, D. Rizzoni, E. Porteri, and R. Aquilani. 2010. Intracellular molecular effects of insulin resistance in patients with metabolic syndrome. Cardiovascular Diabetology. https://doi.org/10.1186/1475-2840-9-46.
Bersch, N., J.E. Groopman, and D.W. Golde. 1982. Natural and biosynthetic insulin stimulates the growth of human erythroid progenitors in vitro. The Journal of Clinical Endocrinology & Metabolism. https://doi.org/10.1210/jcem-55-6-1209.
Li, N., J. Fu, D.P. Koonen, J.A. Kuivenhoven, H. Snieder, and M.H. Hofker. 2014. Are hypertriglyceridemia and low HDL causal factors in the development of insulin resistance? Atherosclerosis. https://doi.org/10.1016/j.atherosclerosis.2013.12.013.
Boutens, L., and R. Stienstra. 2016. Adipose tissue macrophages: Going off track during obesity. Diabetologia. https://doi.org/10.1007/s00125-016-3904-9.
Kolb, H. 2022. Obese visceral fat tissue inflammation: From protective to detrimental? BMC Medicine. https://doi.org/10.1186/s12916-022-02672-y.
Hajer, G.R., T.W. Van Haeften, and F.L. Visseren. 2008. Adipose tissue dysfunction in obesity, diabetes, and vascular diseases. European Heart Journal. https://doi.org/10.1093/eurheartj/ehn387.
Bijari, M., S. Jangjoo, N. Emami, S. Raji, M. Mottaghi, and R. Moallem. 2021. The accuracy of visceral adiposity index for the screening of metabolic syndrome: A systematic review and meta-analysis. International Journal of Endocrinology. https://doi.org/10.1155/2021/6684627.
Caldas, A.P., D.M. Rocha, J. Bressan, and H.H. Hermsdorff. 2021. Dietary fatty acids as nutritional modulators of sirtuins: A systematic review. Nutrition Reviews. https://doi.org/10.1093/nutrit/nuaa007.
Fraiz, G.M., A.R. da Conceição, D.L. de Souza Vilela, D.M. Rocha, J. Bressan, and H.H. Hermsdorff. 2021. Can resveratrol modulate sirtuins in obesity and related diseases? A systematic review of randomized controlled trials. European Journal of Nutrition. https://doi.org/10.1007/s00394-021-02623-y.
Martins, I.J. 2016. Anti-Aging Genes Improve Appetite Regulation and Reverse Cell Senescence and Apoptosis in Global Populations. Advances in Aging Research. https://doi.org/10.4236/aar.2016.51002.
Martins, I.J. 2017. Single gene inactivation with implications to diabetes and multiple organ dysfunction syndrome. Journal of Clinical Epigenetics 3 (3): 24.
Martins, I.J. 2018. Biotherapy and the immune system in ageing science. Acta Scientific Nutritional Health 2 (4): 29–31.
Funding
This paper is related to the project “Elaboration of guidelines and tools to obesity management in the Unified Health System: from Prevention to treatment”, supported by the Agreement Letter between the Arthur Bernardes Foundation, Pan-American Health Organization, and Federal University of Viçosa (Funarbe/ OPAS/ UFV, process number SCON2021-00201). The CAPES Foundation has also supported this study (Code 001). FG Cândido (process number 151832/2022–6) is a National Council for Scientific and Technological Development postdoctoral fellowship. HHM Hermsdorff is a National Council for Scientific and Technological Development fellowship in Research Productivity – 1D-level (process number 308772/2017–2). The funders had no involvement in the paper.
Author information
Authors and Affiliations
Contributions
F.G.C. study design, data collection, analysis and interpretation of data, drafting and editing of manuscript. A.Silva. study design, data collection, analysis and interpretation of data, drafting and editing of the manuscript. G.A.Z. and N.M.C.O. data collection and drafting and editing of the manuscript. H.H.M.H. study design, financial management, supervision, data interpretation, and drafting of the manuscript. All authors approved the version submitted for publication.
Corresponding author
Ethics declarations
Ethics Approval
The study protocol was approved by the Ethics Committee of the Federal University of Viçosa (opinion: 5.164.152, CAAE: 50015621.4.0000.5153). The study was based on institutional records and did not directly involve patients. The managers signed the institutional consent form, and the study complied with the provisions of Resolutions 466/12 [26] and 580/18 [27], the latter regarding the ethical peculiarities of studies of strategic interest to the Brazilian Unified Health System.
Consent for Publication
All authors consent for publication.
Competing Interests
The authors declare no competing interests.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
The original online version of this article was revised: The author found a mistake in the affiliations. It was requested to change the affiliation of one author only but the rest of the author’s affiliations were changed as well, leaving the wrong affiliations.
Rights and permissions
Springer Nature or its licensor (e.g. a society or other partner) holds exclusive rights to this article under a publishing agreement with the author(s) or other rightsholder(s); author self-archiving of the accepted manuscript version of this article is solely governed by the terms of such publishing agreement and applicable law.
About this article
Cite this article
Cândido, F.G., da Silva, A., Zanirate, G.A. et al. Lymphocyte to High-density Lipoprotein Cholesterol Ratio is Positively Associated with Pre-diabetes, Metabolic Syndrome, and Non-traditional Cardiometabolic Risk Markers: A Cross-sectional Study at Secondary Health Care. Inflammation (2024). https://doi.org/10.1007/s10753-024-02063-w
Received:
Revised:
Accepted:
Published:
DOI: https://doi.org/10.1007/s10753-024-02063-w