Abstract
Low vitamin C and reduced alpha-carotene intake are associated with increased asthma risk in children. In addition, mean serum vitamin A concentrations are significantly lower in asthmatic children than in controls. All-trans retinoic acid (ATRA) is a derivative of vitamin A. Macrophage-derived chemokine (MDC) is a T helper cell-type 2 (Th2)-related chemokine involved in the recruitment of Th2 cells toward inflammatory sites. On the other hand, Th1-related chemokine, interferon-inducible protein 10 (IP-10)/CXCL10 is also important in allergic inflammation. Both Th1- and Th2-related chemokines play an important role in allergic asthma. To survey whether ATRA and ascorbic acid effect Th1- and Th2-related chemokine expression in monocytes. To test this, THP-1 cells were pre-treated with ATRA or ascorbic acid and stimulated by lipopolysaccharide (LPS) or poly I:C. Supernatants were measured for Th2-related (MDC) and Th1-related (IP-10) chemokine concentrations by ELISA. The effects of ATRA on mitogen-activated protein kinase (MAPK) and NFkb were evaluated with Western blotting. After stimulation, ATRA significantly down-regulated MDC and IP-10 in a dose-dependent manner. Similarly, ascorbic acid reduced the LPS-induced changes in MDC but only with a high dose. However, asorbic acid had no effect on IP-10 changes either induced by LPS or poly I:C. RT-PCR showed ATRA inhibited IP-10 expression through decreasing the level of transcription. Furthermore, ATRA suppressed the expression of LPS-stimulated c-Raf, MKK1/2 and ERK expression of THP-1 cells. In conclusion, ATRA suppressed Th2- and Th1-related chemokines expression in THP-1 cells, at least in part via the c-Raf-MKK1/2-ERK/MAPK pathway.
Similar content being viewed by others

Avoid common mistakes on your manuscript.
Introduction
Asthma is a chronic inflammatory disorder of the airway [1]. Infiltrating eosinophils, macrophages, Th2 cells, and monocytes comprise the largest proportion of cell-types within the airways of patients with allergic asthma. In addition, these cell-types are associated with airway hyper-reactivity [2]. T helper cell-type 2 (Th2) immunoregulatory cytokines play a central role in the pathogenesis of allergic asthma [2]. In addition, low vitamin C and alpha-carotene intake are associated with increased asthma risk in children [3]. Moreover, vitamin A deficiency remains a persistent problem in the developing world where environmental air pollution is increasing. Vitamin A is an essential micronutrient and plays important roles in the immunity and maintenance of normal epithelial cell differentiation [4]. Asthmatic children possess significantly lower mean serum vitamin A concentrations compared to age-matched controls. Thus, vitamin A hypovitaminosis in asthmatic children may not only be involved in the acute phase response, but may also contribute to the various degrees of chronic epithelial damage in asthmatic airways [4]. Furthermore, there is a correlation between vitamin A deficiency and the mechanism of asthmatic response [4]. In addition, retinoic acid can suppress IL-4-induced eotaxin production in airway epithelial cells [5]. Macrophage-derived chemokine (MDC) is a Th2-related chemokine which can recruit CC chemokine receptor 4-bearing Th2 cells during allergen-challenged inflammation [6]. The Th1-related chemokine, interferon-inducible protein 10 (IP-10) /CXCL10 is also involved in the human allergic pulmonary reaction [7]. Finally, plasma IP-10 and MDC levels are increased in asthmatic children [8, 9]. Our previous data showed that LPS could induce Th1-related chemokine (IP-10) and Th2-related chemokine (MDC) production in human monocytes [10]. However, there are still no data examining the influence of all-trans retinoic acid (ATRA), a derivative of vitamin A, on Th1- and Th2-related chemokine expression in monocytes. Therefore, we investigated whether ATRA could suppress the LPS-induced Th2-related chemokine (MDC) and Th1-related chemokine (IP-10) expression in monocytes. In addition, we explored the detailed mechanisms underlying the effects of ATRA on LPS-induced chemokine expression in monocytes.
Methods
Cell Preparation
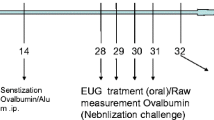
The human monocytic cell line, THP-1 (American Type Culture Collection, Rockville, MD), was cultured in RPMI 1640 medium (Sigma Chemical Co., St. Louis, MO) supplemented with 10% fetal bovine serum, 100 U/mL of penicillin, and 100 μg/mL of streptomycin at 37°C and 5% CO2 in a humidified incubator. Cells were centrifuged and resuspended in fresh media in 24-well plates at a concentration of 106/mL for 24 h before experimental use. The cells were pre-treated with ATRA, ascorbic acid (Sigma Chemical Co., St. Louis, MO) or vehicle alone 2 h before LPS (0.2 μg/ml) (Escherichia coli derived; Sigma Chemical Co., St. Louis, MO) stimulation. Cell supernatants were collected at different time points after LPS or polyinosinic:polycytidylic acids [poly(I:C)] stimulation.
ELISA Assay
The MDC and IP-10 concentrations of cell supernatants were determined using a commercially available ELISA-based assay system (R&D System, Minneapolis, MN). Assays were performed using the protocols recommended by the manufacturer.
RNA Extraction and Real-time PCR
THP-1 cells were pre-treated with ATRA or ascorbic acid (0.1, 1, and 10 μM) 2 h before LPS (0.2 μg/ml) stimulation. The total RNA of cells was extracted using RNeasy Mini Kits (Qiagen, Helden, Germany) according to the manufacturer’s instructions. 3 μg RNA from each sample was subsequently reverse-transcribed to single-stranded cDNA in a 20 μl reaction mixture using a SuperScriptTM First-Strand Synthesis System with a RT-PCR kit (Invitrogen, USA). Measurements were performed by an ABI PRISM 9700 HT sequence detection system (Applied Biosystems, Foster City, CA) using a predeveloped Taqman probe/primer combination for IP-10. Taqman PCR was performed in a 10 μl volume using AmpliTaq Gold polymerase and a universal master mix (Applied Biosystems). Threshold cycle numbers were transformed using the ΔΔCt (threshold cycle) and relative value method as described by the manufacturer. These values were expressed relative to β-actin, which was used as a housekeeping gene by multiplexing single reactions.
Western Blotting
After 2 h with or without ATRA (0.1, 1, and 10 μM) treatments, the cells were stimulated with LPS (0.2 μg/ml) for 1 h and then lysed with equal volumes of ice-cold 150-μl lysis buffer. After centrifugation at 13,000 × g for 15 min, equal amounts of cell lysates were analyzed by Western blot with anti-MAPK (p38, ERK, and JNK) and anti-phosphor-p65 and anti-phospho-MAPK (pp38, p-ERK and p-JNK) antibodies (Santa Cruz Biotechnology, Santa Cruz, CA). Anti-p-c-Raf, anti-c-Raf, anti-p-MKK1/2 and anti-MKK1/2 antibodies were also used for evaluating c-Raf- MKK1/2 pathway (Santa Cruz Biotechnology, Santa Cruz, CA). Immunoreactive bands were visualized using a horseradish peroxidase-conjugated secondary antibody and the enhanced chemiluminescence (ECL) system (Amersham Pharmacia Biotech).
Statistical Analyses
All data are presented as mean ± SD. One-way analysis of variance was used for all statistical comparisons, and the Student-Newman–Keuls test was conducted for multiple comparisons. A P value of <0.05 was considered indicative of significant differences. SigmaStat software (Jandel Scientific, Erkrath, Germany) was used for all statistical analyses.
Results
ATRA Significantly Down Regulated LPS-Induced MDC Expression of THP-1
ATRA (0.1–10 μM) significantly down-regulated LPS-induced MDC production of THP-1 cells after LPS stimulation for 6, 12 and 24 h (Fig. 1a). Only a high dose (10 μM) of ascorbic acid could suppress the production of LPS-induced MDC (Fig. 1b).
The THP-1 cells were pre-treated with ATRA or ascorbic acid 2 h before LPS stimulation. Cell supernatants were collected for measurement of MDC concentration after LPS stimulation for 6, 12 and 24 h. ATRA could significantly suppress LPS-induced MDC production of THP-1 cells after LPS stimulation for 6, 12 and 24 h (a). Only higher dose of ascorbic acid reduced LPS-induced MDC expression for 24 h (b).
ATRA Suppressed LPS or Poly I: C-induced IP-10 Expression of THP-1 Cells
ATRA (0.1–10 μM) significantly down-regulated LPS-induced IP-10 expression for 6, 12, and 24 h (Fig. 2a). ATRA cold also suppress Poly I:C-induced IP-10 expression (Fig. 2b). However, IP-10 increases from LPS and Poly I:C induction could not be reduced by treatment with ascorbic acid (Fig. 2c,d). Furthermore, ATRA significantly reduced the amount of IP-10 mRNA when THP-1 cells were stimulated with LPS (Fig. 3). These findings demonstrate that ATRA could regulate IP-10 expression, at least at the transcriptional level.
The THP-1 cells were pre-treated (6, 12 or 24 h) with ATRA or ascorbic acid 2 h before LPS stimulation and then the IP-10 concentration was measured by ELISA. ATRA (1–10 μM) significantly down-regulated LPS-induced IP-10 expression for 6, 12 and 24 h (a). ATRA could also reduce Poly I:C-induced IP-10 expression for 24 h (b). However, IP-10 induction from LPS and Poly I:C treatments could not be reduced by treatment with ascorbic acid (c and d).
THP-1 cells were pre-treated with ATRA 2 h before LPS stimulation for 6 h. The total RNA of cells was extracted and the expression profiles were measured with real-time PCR. Each condition was expressed relative to β-actin. The result showed that ATRA reduced IP-10 mRNA amounts when THP-1 cells were stimulated with LPS.
Vitamin A Significantly Down-Regulated LPS-Induced pERK Expression of THP-1 Cells
NFkB-related proteins, p65 and pp65 in THP-1 cells were slightly reduced when pre-treated with 10 μM ATRA and stimulated with LPS (Fig. 4a). Mitogen-activated protein kinases (MAPKs) are import for cytokines expression of monocyte lineage [10, 11]. We next examined whether the suppressive effect of ATRA on Th1- and Th2-related chemokines is via inhibition of MAPK. Pre-treatment with ATRA (0.1–10 μM) for 2 h dramatically suppressed LPS-induced pERK expression in THP-1 cells (P < 0.05) (Fig. 4b). Other MAPKs which were also induced by LPS, such as pp38 was slightly decreased, but pJNK was not regulated by ATRA (Fig. 4c). C-Raf and MKK1/2 are the upstream signaling of ERK [12]. Therefore, we next evaluated the upstream pathway of ATRA. The results showed ATRA could also decrease p-c-Raf and p-MKK1/2 expression, suggesting ATRA suppressed MDC and IP-10 expression, at least, in part through c-Raf-MKK 1/2-ERK pathway (Fig. 4d).
THP-1 cells were pre-treated with ATRA 2 h before LPS stimulation for 30 min. Cell lysates were used for Western blotting. NFkB-related proteins, p65 and pp65 were slightly reduced when THP-1 cells were treated with 10 μM ATRA and then challenged with LPS (a). Pre-treatment with ATRA (0.1–10 μM) for 2 h dramatically suppressed LPS-induced pERK/MAPK expression in THP-1 cells in a dose-dependent manner (b). ATRA could decrease LPS-induced pp38 slightly, but not pJNK expression in THP-1 cells (c). C-Raf and MKK1/2 are the upstream signaling of ERK [12]. ATRA could also decrease p-c-Raf and p-MKK1/2 expression, suggesting ATRA suppressed MDC and IP-10 expression, at least, in part through c-Raf-MKK 1/2-ERK pathway (d).
Discussion
In recent decades, both the prevalence of autoimmune (Th1-related) and allergic (Th2-related) diseases have increased, yet the causes of these diseases remain unclear [13]. Asthma is one of the most common chronic airway diseases and accounts for substantial morbidity and health costs. House dust mite avoidance during early childhood did not prevent the onset of allergies [14]. Vitamin supplementation is essential for a properly functioning immune system. Stimulation of human PBMCs and purified T cells with all-trans retinoic acid and 9-cis-retinoid acid increased the mRNA and protein levels of Th2 cytokines and decreased levels of Th1 cytokines upon activation with anti-CD3 and/or anti-CD28 mAbs [15]. Therefore, the impact of retinoic acids on pulmonary allergic reactions remains elusive. The relationship between the supplementation of vitamins and the risk of allergic diseases has been controversial [16]. However, vitamin A is clearly involved in several mechanisms of asthma. Diminished auto-inhibitory muscarinic receptor-2 function contributes to the increased airway responsiveness to pulmonary C-fiber stimulation in vitamin A deficient rats [17]. Retinoic acid also decreases the chemotactic ability of HMC-1 cells and may regulate the inflammatory effects of mast cells, which are one of the most import cell-types involved in asthma [18]. Our result also suggested that ATRA regulated both Th1- and Th2-related inflammatory responses which are important in asthmatic reactions.
Exposure to airborne endotoxins (such as LPS) in infancy may protect against asthma by promoting tolerance to allergens later in life. However, LPS adversely affects patients with asthma in later life [19]. LPS can induce the Th1-related chemokine (IP-10) and the Th2-related chemokine (MDC) production in human monocytes [10]. In addition, the Th1- and Th2-related chemokines play an important role in human allergic asthma [8, 9, 20]. Several anti-allergic or anti-asthmatic medications, such as mast cell stabilizers and leukotriene receptor antagonists, have some effects on chemokine expression or chemokine-induced chemotaxis [10, 21]. In the present study, the suppressive effects of retinoic acid on LPS-induced Th1- and Th2-related chemokine expression suggested that the chemotactic abilities of Th1 and Th2 cells could be suppressed. Thus, vitamin A may be beneficial for asthma and autoimmune diseases via inhibition of Th2- and Th1-related chemokines.
Rhinovirus-induced asthma is the most frequent trigger for asthma exacerbations. Serum IP-10 is often increased during these infections and is a novel biomarker of rhinovirus-induced asthma exacerbations [22]. Increased serum IP-10 levels were strongly associated with severe airflow obstruction and predictive of virus-induced asthma [23]. Polyinosinic:polycytidylic acids [poly(I:C)] is a synthetic mimetic of dsRNA and functions through an endosomal receptor, such as Toll-like receptor 3, or cytosolic receptors and can activate innate immunity [22]. MDCs play a role not only in asthma but also in allergic rhinitis [8, 24]. MDCs were increased in the exhaled breath condensate and plasma in children with asthma [25]. The clear suppression of LPS- and poly I:C-induced IP-10 and MDC production in monocytes by ATRA suggested that ATRA may be good for the treatment of Th1-related inflammation of rhinovirus-induced asthma, as well as allergic rhinitis. In our previous study, MAPK played an important role for Th1- and Th2-related chemokine expression in monocytes [10]. The dose-dependent suppression of LPS-induced ERK/MAPK expression by ATRA suggested the effect of ATRA on chemokine production in monocytes may at least, in part, through inhibition of the ERK/MAPK pathway.
References
Barnes, P. J., K. F. Chung, and C. P. Page. 1998. Inflammatory mediators of asthma: an update. Pharmacol. Rev. 50:515–596.
Crimi, E., D. Gaffi, E. Frittoli, B. Borgonovo, and S. E. Burastero. 1997. Depletion of circulating allergen specific TH2 T lymphocytes after allergen exposure in asthma. J. Allergy Clin. Immunol. 99:788–797. doi:10.1016/S0091-6749(97)80013-9.
Harik-Khan, R. I., D. C. Muller, and R. A. Wise. 2004. Serum vitamin levels and the risk of asthma in children. Am. J. Epidemiol. 159:351–357. doi:10.1093/aje/kwh053.
Mizuno, Y., T. Furusho, A. Yoshida, H. Nakamura, T. Matsuura, and Y. Eto. 2006. Serum vitamin A concentrations in asthmatic children in Japan. Pediatr. Int. 48:261–264. doi:10.1111/j.1442-200X.2006.02200.x.
Takamura, K., Y. Nasuhara, M. Kobayashi, T. Betsuyaku, Y. Tanino, I. Kinoshita, E. Yamaguchi, S. Matsukura, R. P. Schleimer, and M. Nishimura. 2004. Retinoic acid inhibits interleukin-4-induced eotaxin production in a human bronchial epithelial cell line. Am. J. Physiol. Lung Cell Mol. Physiol. 286:L777–L785. doi:10.1152/ajplung.00289.2003.
Pilette, C., J. N. Francis, S. J. Till, and S. R. Durham. 2004. CCR4 ligands are up-regulated in the airways of atopic asthmatics after segmental allergen challenge. Eur. Respir. J. 23:876–884. doi:10.1183/09031936.04.00102504.
Liu, L., N. N. Jarjour, W. W. Buss, and E. A. Kelly. 2004. Enhanced generation of helper T type 1 and 2 chemokines in allergen-induced asthma. Am. J. Respir. Crit. Care Med. 169:1118–1124. doi:10.1164/rccm.200312-1659OC.
Hung, C. H., C. Y. Li, Y. S. Lai, P. C. Hsu, Y. M. Hua, and K. D. Yang. 2005. Discrepant clinical responses and blood chemokine profiles between two non-steroidal anti-inflammatory medications for children with mild persistent asthma. Pediatr. Allergy Immunol. 16:306–309.
Lai, S. T., C. H. Hung, Y. M. Hua, S. H. Hsu, Y. J. Jong, and J. L. Suen. 2008. T-helper 1-related chemokines in the exacerbation of childhood asthma. Pediatr. Int. 50:99–102. doi:10.1111/j.1442-200X.2007.02533.x.
Hung, C. H., J. L. Suen, Y. M. Hua, W. Chiang, H. C. Chang, C. N. Chen, and Y. J. Jong. 2007. Suppressive effects of ketotifen on Th1- and Th2-related chemokines of monocytes. Pediatr. Allergy Immunol. 18:378–384. doi:10.1111/j.1399-3038.2007.00535.x.
Tudhope, S. J., T. K. Finney-Hayward, A. G. Nicholson, R. J. Mayer, M. S. Barnette, P. J. Barnes, and L. E. Donnelly. 2008. Different mitogen-activated protein kinase-dependent cytokine responses in cells of the monocyte lineage. J. Pharmacol. Exp. Ther. 324:306–312. doi:10.1124/jpet.107.127670.
Jones, N. C., Y. V. Fedorov, R. S. Rosenthal, and B. B. Olwin. 2001. ERK1/2 is required for myoblast proliferation but is dispensable for muscle gene expression and cell fusion. J. Cell Physiol. 186:104–115. doi:10.1002/1097-4652(200101)186:1<104::AID-JCP1015>3.0.CO;2-0.
Seiss, S. T. 2002. Eat dirt-the hygiene hypothesis and allergic diseases. N. Engl. J. Med. 347:930–931. doi:10.1056/NEJMe020092.
Marks, G. B., S. Mihrshahi, A. S. Kemp, E. R. Tovey, K. Webb, C. Almqvist, R. D. Ampon, D. Crisafulli, E. G. Belousova, C. M. Mellis, J. K. Peat, and S. R. Leeder. 2006. Prevention of asthma during the first 5 years of life: a randomized controlled trial. J. Allergy Clin. Immunol. 118:53–61. doi:10.1016/j.jaci.2006.04.004.
Dawson, H. D., G. Collins, R. Pyle, M. Key, A. Weeraratna, V. Deep-Dixit, C. N. Nadal, and D. D. Taub. 2006. Direct and indirect effects of retinoic acid on human Th2 cytokine and chemokine expression by human T lymphocytes. BMC Immunol. 7:27. doi:10.1186/1471-2172-7-27.
Kull, I., A. Bergström, E. Melén, G. Lilja, M. van Hage, G. Pershagen, and M. Wickman. 2006. Early-life supplementation of vitamins A and D, in water-soluble form or in peanut oil, and allergic diseases during childhood. J. Allergy Clin. Immunol. 118:1299–1304. doi:10.1016/j.jaci.2006.08.022.
McGowan, S. E. 2007. Vitamin A deficiency increases airway resistance following C-fiber stimulation. Respir. Physiol. Neurobiol. 157:281–289. doi:10.1016/j.resp.2007.01.011.
Ko, J., C. Y. Yun, J. S. Lee, D. H. Kim, J. E. Yuk, and I. S. Kim. 2006. Differential regulation of CC chemokine receptors by 9-cis retinoic acid in the human mast cell line, HMC-1. Life Sci. 79:1293–1300. doi:10.1016/j.lfs.2006.03.046.
Reed, C. E., and D. K. Milton. 2001. Endotoxin-stimulated innate immunity: a contributing factor for asthma. J. Allergy Clin. Immunol. 108:157–166. doi:10.1067/mai.2001.116862.
Bochner, B. S., S. A. Hudson, H. Q. Xiao, and M. C. Liu. 2003. Release of both CCR4-active and CXCR3-active chemokines during human allergic pulmonary late-phase reactions. J. Allergy Clin. Immunol. 112:930–934. doi:10.1016/j.jaci.2003.08.012.
Hung, C. H., C. Y. Li, Y. M. Hua, K. D. Yang, and Y. J. Jong. 2006. Effects of leukotriene receptor antagonists on monocyte chemotaxis, p38 and cytoplasmic calcium. Pediatr Allergy Immunol. 17:250–258. doi:10.1111/j.1399-3038.2006.00385.x.
Wark, P. A., F. Bucchieri, S. L. Johnston, P. G. Gibson, L. Hamilton, J. Mimica, G. Zummo, S. T. Holgate, J. Attia, A. Thakkinstian, and D. E. Davies. 2007. IFN-gamma-induced protein 10 is a novel biomarker of rhinovirus-induced asthma exacerbations. J. Allergy Clin. Immunol. 120:586–593. doi:10.1016/j.jaci.2007.04.046.
Sugiyama, T., K. Hoshino, M. Saito, T. Yano, I. Sasaki, C. Yamazaki, S. Akira, and T. Kaisho. 2008. Immunoadjuvant effects of polyadenylic:polyuridylic acids through TLR3 and TLR7. Int. Immunol. 20:1–9. doi:10.1093/intimm/dxm112.
Yanai, M., K. Sato, N. Aoki, Y. Takiyama, K. Oikawa, H. Kobayashi, S. Kimura, Y. Harabuchi, and M. Tateno. 2007. The role of CCL22/macrophage-derived chemokine in allergic rhinitis. Clin Immunol. 125:291–298. doi:10.1016/j.clim.2007.08.002.
Leung, T. F., G. W. Wong, F. W. Ko, C. W. Lam, and T. F. Fok. 2004. Increased macrophage-derived chemokine in exhaled breath condensate and plasma from children with asthma. Clin. Exp. Allergy. 34:786–791. doi:10.1111/j.1365-2222.2004.1951.x.
Author information
Authors and Affiliations
Corresponding author
Additional information
Supported by a grant from the Chi-Mei Medical Center and Kaohsiung Medical University Research Foundation (CM-KMU_ X096009)
Rights and permissions
About this article
Cite this article
Tsai, YC., Chang, HW., Chang, TT. et al. Effects of All-Trans Retinoic Acid on Th1- and Th2-Related Chemokines Production in Monocytes. Inflammation 31, 428–433 (2008). https://doi.org/10.1007/s10753-008-9095-x
Published:
Issue Date:
DOI: https://doi.org/10.1007/s10753-008-9095-x