Abstract
Primary care providers (PCPs) are considered the first-line defenders in preventive care. Patients seeking service from the same PCP constitute that physician’s panel, which determines the overall supply and demand of the physician. The process of allocating patients to physician panels is called panel design. This study quantifies patient overflow and builds a mathematical model to evaluate the effect of two implementable panel assignments. In specialized panel assignment, patients are assigned based on their medical needs or visit frequency. In equal panel assignment, patients are distributed uniformly to maintain a similar composition across panels. We utilize majorization theory and numerical examples to evaluate the performance of the two designs. The results show that specialized panel assignment outperforms when (1) patient demands and physician capacity are relatively balanced or (2) patients who require frequent visits incur a higher shortage penalty. In a simulation model with actual patient arrival patterns, we also illustrate the robustness of the results and demonstrate the effect of switching panel policy when the patient pool changes over time.
Similar content being viewed by others
Explore related subjects
Discover the latest articles, news and stories from top researchers in related subjects.Avoid common mistakes on your manuscript.
1 Highlights
-
Two physician panel designs are studied to provide a guideline for panel redesign – specialized panel assignment separates patients with high and low visit frequencies, and equal panel assignment maintains the same patient composition across panels.
-
Majorization theory and numerical analysis are used to characterize the benefit of the two panel redesign strategies.
-
Specialized panel assignment incurs less overflow, especially when the patient demand and the physician capacity are balanced.
-
If supply and demand are not balanced, or the consequences of delayed service are severe for patients who require fewer visits, the equal panel assignment may provide a better outcome. However, balancing supply and demand is more critical.
-
The above results remain valid when the assignments diverge from the planned design due to natural patient movement.
2 Introduction
In the United States, accessing medical services with a reasonable wait time has become challenging for patients due to an imbalance in supply and demand. According to a survey by Hawkins [27], the average wait time to visit a family physician is 29 days for large metro areas and 56.3 days for mid-sized metro areas. A similar issue also exists at the Department of Veterans Affairs (VA), where less than 20% of patients are able to secure an appointment within the two-week goal [37].
To improve access to healthcare, the need for patient-doctor contact (PDC) must be accurately accommodated with available appointment slots [29]. In many countries, including the United States, patients are often required to choose (or to be designated with) primary care providers (PCPs) formed by one physician or a medical team. PCPs provide most care required by a patient and play an essential role in preventive care [5]. Patients who choose the same physician comprise a physician panel. To better match supply and demand and improve patients’ outcomes, many large-scale healthcare systems rely on a process called panel design to determine the target patient composition of physicians’ panels.
Panel design, a strategic decision that determines the overall workload of the physician, is an essential long-term task in healthcare management. Because patients often have the privilege of seeking service from their physicians, a physician’s workload highly depends on the panel size and patient visit frequency. Hence, panel design serves as valuable leverage to balance the workload among physicians and prevent physician burnout [10]. A successful panel design strategy also helps reveal the potential performance issues of physicians with comparable patient composition and workload. An appropriately designed panel can better match a patient with a physician based on their medical needs and allows the patients to access their medical service more efficiently, leading to better health outcomes and patient satisfaction [2, 28, 36]. Panel design problem can be applied to multi-physician clinics, a medical group, and some specific departments (e.g., family medicine, internal medicine) in a larger hospital system with multiple physicians. Hereafter, all these systems are referred to a clinic in the paper.
Traditionally, a panel design problem aims to determine the size of each panel (i.e., the number of patients assigned to each physician), which is calculated by a function of a provider’s yearly total appointment slots and the number of visits per patient. Specifically,
However, this simple calculation is often insufficient. Panel composition is also a significant factor. Patients seek medical visits for various reasons and thus require different visiting intervals. According to the CDC National Ambulatory Medical Care Survey data (2018), patients between 25 and 44 years old visit the obstetrics and gynecology (OB/GYN) offices 1.37 times per year on average, whereas pregnant women, depending on their condition, require at least eight visits annually. In other words, even when the numbers of patients in different panels are the same, a physician with more pregnant patients can have a much higher workload than a physician with most patients visiting only for annual check-ups.
The number of visits can also vary due to factors such as age and gender [33]. The workload generated by young and healthy patients can differ from that of senior patients with chronic diseases. For instance, Kroll and Lampert [20] report a higher frequency of visits in Germany for seniors than younger adults based on data from 2007. Consequently, when determining the panel size, it is essential to incorporate factors such as patient health status and potential visit frequency rather than relying solely on the panel size.
From a clinic capacity planner’s perspective, panel composition may also affect the recourse needed. Patients with varying health conditions often require different physician skill sets and experiences. In practice, it is not uncommon to provide care delivery via non-physician providers [6]. For example, in OB/GYN, while a nurse practitioner can perform a routine pap smear, a patient with complications during her pregnancy must be evaluated by experienced physicians. It is estimated that at least 70% of the care required for adults (90% for pediatric patients) can be handled by nurse practitioners and physician assistants [26]. Hence, if patients are assigned to providers based on their needs, a capacity planner may be able to allocate their valuable resources more efficiently.
A poorly designed panel also increases the likelihood of physician mismatch and delay. A 2011 study indicates that VA patient appointments are delayed 2.04 additional days per appointment when the panel size increases by one standard deviation [36]. Rust et al. [34] and Gill [12] report that patients who have difficulty getting appointments with their physicians are more likely to visit the Emergency Room (ER). This creates potential risks for patients, especially those with chronic conditions or complications. These patients often require more dedicated service from their own physicians who are more familiar with their medical history. Gill and Mainous [13] report that patients who visit their PCPs are more likely to receive correct medications and treatment and resolve their medical problems. Conversely, Lane et al. [21] show that older adults with dementia are more likely to receive potentially harmful medications from physicians who are unfamiliar with their patients.
Due to the importance of panel design, we are motivated to investigate potential panel design strategies to improve the match of supply and demand when considering patient visit frequency. Specifically, we study two implementable panel-design strategies – specialized panel assignment and equal panel assignment. In specialized panel assignment, we allocate patients into panels based on their medical needs (e.g., predicted/historical frequency of PDC visits) and assign patients who require similar visit frequencies in the same panel. To maintain a balanced workload among panels, a panel with more low-PDC patients is larger than the one with more high-PDC patients. One potential benefit of specialized panel assignment is that high-PDC patients may receive better long-term care because their PCPs with smaller panels may familiarize them with patients’ medical history better. In equal panel assignment, patients are uniformly assigned into panels. Thus, all panels share nearly identical patient composition and size, with minimal difference.
It is worth noting that the primary goal of the panel design problem is not about redistributing patients to physician panels or finding the “optimal” design. This is because keeping patient-provider care continuity is always a top priority. Besides, a clinic generally cannot achieve any particular assignment entirely because patients always have the right to choose physicians, and their medical needs may change constantly. Hence, the goal of panel design is to provide general guidelines for allocating new patients and reallocating existing patients who decide to change physicians voluntarily. It is a continuously improving process that allows physician panels to adjust over time to achieve a status closer to the target design.
We construct a theoretical model and characterize the proposed panel design strategies. With the help of majorization theory, we demonstrate that a panel with patients who require more frequent visits is less likely to experience a supply shortage when the workloads of the two panels are the same. We also observe that when physician capacity and patient demand are relatively balanced, a clinic that utilizes specialized panel assignment incurs less shortage. However, when capacity and demand are significantly imbalanced, equal panel assignment performs better. Moreover, when considering the cost of delaying service due to overflow, we find that specialized panel assignment often performs better unless the cost of delaying service for low-PDC patients is significantly higher than that for high-PDC patients. The overall patient composition also affects the results. Specialized panel assignment performs better when the arrival frequencies for the two types of patients differ significantly. However, there is one exception. When the patient visit frequency is less heterogeneous, and the cost of denying service for low-PDC patients is higher than that for high-PDC patients, specialized panel assignment can still be more suitable. We summarize the findings in Fig. 1.
The two assignments have also been evaluated and verified through simulation using actual appointment records to understand the implementation in practice. Specifically, we demonstrate that when the cost assumption is not perfectly matched, or the patient composition in the panel is slightly different from the intended design, the insights remain intact. From the healthcare providers’ perspective, this implies that the results are robust, and the outcomes are noticed soon after the target panel design begins to emerge.
The remainder of this paper is organized as follows. Section 2 presents related literature regarding the panel design problem. The model formulation is presented in Section 3. The theoretical analysis is provided in Section 4. Additional numerical results are presented in Section 5. Section 6 elaborates on the implementation in practice with simulation with historical appointment records. Section 7 concludes the paper.
3 Literature review
The importance of having a suitable panel size for a physician has been widely addressed in empirical studies that examine a variety of performance metrics, including clinical quality [2, 9, 36], timely access [1, 11, 23], and physician burnout [15, 18, 24]. For example, Angstman et al. [2] report that a larger panel size negatively affects the diabetic quality results and appointments available to patients. Dahrouge et al. [9] indicate that the likelihood of receiving ambulatory care-sensitive conditions increases with larger panel sizes. Stefos et al. [36] demonstrate the negative impact of increased panel size on vaccination rate and other preventive screenings in the VA system. Further, Margolius et al. [23] report a correlation between panel size and the third next available appointment.
Additional research emphasizes the effect of panel composition on access to the healthcare system. Rossi and Balasubramanian [33] point out the importance of considering factors such as case-mix and practice style in panel size calculation. Altschuler et al. [1] propose a model by delegating 77% of preventive and chronic care services and discovered that it could increase a primary care team’s reasonable panel size. Rajkomar et al. [31] focus on classifying patients into different primary care utilization phenotypes by using granular electronic health record (EHR) data. Such information can be used to predict the workload required in a panel based on individual patient’s demands and complexity.
The application of operations research in healthcare management has also expanded in recent years. We present only studies that address the panel size issue as our paper is more related to research that considers panel composition in panel design optimization problems. Balasubramanian et al. [3], Balasubramanian et al. [4] use stochastic linear programming and simulations to optimize panels in which patient visit frequency differs by gender, age, or other more sophisticated case-mix factors (e.g., chronic conditions). Ozen and Balasubramanian [30] formulate the panel redesign problem of a similar setting with case-mix patients using a nonlinear integer programming problem. They also develop heuristics to improve overflow by transferring patients from the overflow panel to another panel. It is worth mentioning that [3] demonstrate that specialized panel assignment could be a solid strategy to maximize access of service and continuity of care. However, we find that specialized panel assignment may slightly worsen the situation when supply and demand are imbalanced. Another significant difference between our work and that of these studies is that we emphasize the effect of the two practical assignments instead of identifying the optimal panel assignments.
Although less related to our work, other research focuses on the appointment system while considering the panel size issue. Green et al. [17] present a probability model to determine an appropriate panel size that considers overflow. Further, Green and Savin [16] identify proper panel sizes for an open access policy using a queueing model with the delay-dependent no-show. In another related study, Liu and Ziya [22] implement a queueing model to characterize the panel size and the overbooking level decisions. Zacharias and Armony [37] consider a joint problem that determines the panel size and appointment offered together and demonstrate that an open access policy is more appropriate when both appointment delay and clinic delay matter. While such studies may address the panel size optimization issue, they often do not consider patient composition.
4 Model formulation
Suppose that in a clinic system with a central capacity planner, there are n patients and m non-competing physician panels, The capacity for each panel is k. Each patient will be assigned to a panel upon joining the system based on a panel design \(\textbf{a}=(\mathbf {a^{(1)}}, \mathbf {a^{(2)}}, \dots , \mathbf {a^{(m)}})\), where \(\mathbf {a^{(j)}}=(a^{(j)}_{1}, a^{(j)}_{2},a^{(j)}_{3}, \dots , a^{(j)}_{n})\) is a binary vector that indicates if a patient is included in physician-j’s panel. For instance, \(\mathbf {a^{(j)}}=(1,1,1,1,0,0,0,\dots ,0)\) means that only the first four patients are assigned to the panel-j. Patients request the physician visit according to a set of arrival probabilities that is defined by a vector \(\textbf{p} = (p_1, p_2,\dots , p_n)\) where patient-i’s arrival probability is \(p_i\). Without loss of generality, we assume patients are sorted in descending order according to their arrival probabilities. That is, \(1>p_1\ge p_2\ge \dots \ge p_n>0\). We also assume that patients’ arrival probabilities can be estimated from their historical visits (for existing patients) or from factors such as the reason for visits, age, or gender (for new patients). In practice, a patient’s visit frequency might change as their health status changes. However, those changes often can be taken care of because a capacity planner can review the status of each panel to adjust their assignment policy regularly. Thus, our analysis assumes that the changes in visit frequency can be ignored to focus on managerial insights. This is consistent with similar assumptions made in the literature (e.g., Ozen and Balasubramanian [30] and Bavafa et al. [7].)
Our model focuses on long-term panel assignment planning rather than short-term operation decisions. Thus, the model does not directly address the appointment system. Instead, we assume that there is an underlying appointment system and patients can obtain an appointment as long as capacity remains. When the number of patient arrivals is higher than the capacity, patients will not be able to obtain the appointment on time, and a penalty is applied. We assume that the cost (penalty) of being delayed or becoming an overflow is denoted as \(\textbf{c}=(c_1, c_2, \dots , c_n)\). Next, for a given panel-j’s assignment \(\mathbf {a^{(j)}}\), demand for panel-j can be written as
where \(B(\cdot )\) is a random variable that follows the Bernoulli distribution. The expected demand overage (e.g., the number of patients to be delayed or turned away) for physician-j is
where \([Q_j (\mathbf {a^{(j)}})-k]^+\) represents \(\max (\mathbf {a^{(j)}}-k, 0)\). Because patients in the same panel can request the service in any sequences, we assume that all patients in the same panel have an equal chance of being rejected when the capacity is full. Hence, the average demand shortage cost for panel-j can be defined as \(c(\mathbf {a^{(j)}}) = \textbf{c}\cdot \mathbf {a^{(j)}} / \sum _{i=1}^n{a_i^{(j)}}\), where \( \sum _{i=1}^n{a_i^{(j)}}\) is the number of patients in the panel-j. In other words, the expected demand overage cost is \(c(\mathbf {a^{(j)}})\cdot \pi _j(\mathbf {a^{(j)}})\).
The capacity planner’s goal is to determine a panel assignment \(\textbf{a}\) to minimize the overall shortage penalty while balancing panels’ workloads. The mathematical model is presented as follows.
where Constraint (4) ensures that every single patient is allocated to precisely one panel and Constraint (5) ensures that workloads are balanced across panels. Note that Constraint (5) in practice may be relaxed to \(\mathbf {a^{(j)}}\textbf{p} \le \mathbf {a^{(j')}}\textbf{p}+\epsilon \) for all pairs of \((j, j')\) where \(\epsilon \) is a small number. This is because with some patient pools, it may be impossible to create panels with exact equal loads. In Section 5, we will present an example of such scenarios.
Because directly solving the above optimization problem is challenging, we concentrate our analysis on two intuitive and implementable assignments. In specialized panel assignment, we assign patients to panels based on their arrival frequencies. The process is as follows. We begin by filling panel-j with patients one at a time from those with the highest arrival probability until the expected demand load of the panel reaches the designated load for each panel (e.g., \(\mathbf {a^{(j)}}\textbf{p}= \sum _{i=1}^n p_i / m\)). Then, we repeat the process for panel-\((j+1)\) until all panels are filled. Note that because all panels’ demand loads are kept the same, the panels with higher (respectively, lower) PDC patients are smaller (respectively, larger). In equal panel assignment, the patient composition and the size of the panel are identical. Hence, we assign patients to all panels in a round-robin fashion.
An illustration of the two panel assignments is presented in Fig. 2. In this figure, the arrival probability for high-PDC is two times that of the low-PDC arrival probability. Mathematically, \(\mathbf {a^{(1)}}=\{1,1,1,1,0,0,0,0,0,0,0,0\}\) and \(\mathbf {a^{(2)}}=\{0,0,0,0,1,1,1,1,1,1,1,1\}\) for specialized panel assignment and \(\mathbf {a^{(1)}}=\{1,0,1,0,1,0,1,0,1,0,1,0\}\) and \(\mathbf {a^{(2)}}=\{0,1,0,1,0,1,0,1,0,1,0,1\}\) for equal panel assignment. In both cases, we have \(\mathbf {a^{(1)}}\textbf{p}= \mathbf {a^{(2)}}\textbf{p}\) to ensure workloads are equally distributed to the two panels. Note that this example only contains two panels and two patient types (e.g., high-PDC and low-PDC patients) for ease of exposition. However, our model treats each patient independently, meaning we can have up to n different patient arrival frequencies.
5 Analytical results
We utilize certain established results from the theory of majorization to lay out the characteristics of the solutions. To formally define majorization, Definitions 1 and 2 are presented next and more details can be founded in Marshall et al. [25].
Definition 1
Given any two n-component vectors \(\mathbf {v^{[1]}}\in \mathbb {R}^n\) and \(\mathbf {v^{[2]}}\in \mathbb {R}^n\) sorted in descending order, where \(v^{[1]}_1\ge v^{[1]}_2 \ge \dots \ge v^{[1]}_n\) and \(v^{[2]}_1\ge v^{[2]}_2 \ge \dots \ge v^{[2]}_n\). We say that vector \(\textbf{v}^{[1]}\) is weakly majorized (or dominated) by vector \(\textbf{v}^{[2]}\), which is denoted by \(\textbf{v}^{[1]} \prec _w \textbf{v}^{[2]}\) iff \(\sum _{i=1}^l v_i^{[1]} \le \sum _{i=1}^l v_i^{[2]}\) holds for all \(l \le n\).
Definition 1 defines the condition such that one vector (in descending order) is weakly majorized by the other. For instance, suppose that we have three vectors \(\mathbf {v^{[1]}}=[3,2,2]\), \(\mathbf {v^{[2]}}=[4,3,2]\), and \(\mathbf {v^{[3]}}=[4,1,1]\). We can clearly see that \(\mathbf {v^{[1]}}\) is weakly majorized by \(\mathbf {v^{[2]}}\). However, \(\mathbf {v^{[1]}}\) is not weakly majorized by \(\mathbf {v^{[3]}}\) because \(\sum _{i=1}^l v_i^{[1]} \le \sum _{i=1}^l v_i^{[3]}\) does not hold when \(l =3\).
Definition 2
Given any two n-component vectors \(\mathbf {v^{[1]}}\in \mathbb {R}^n\) and \(\mathbf {v^{[2]}}\in \mathbb {R}^n\) where \(\textbf{v}^{[1]} \prec _w \textbf{v}^{[2]}\). If equality \(\sum _{i=1}^n v_i^{[1]} = \sum _{i=1}^n v_i^{[2]}\) holds, we say that vector \(\textbf{v}^{[1]}\) is majorized (or dominated) by vector \(\textbf{v}^{[2]}\), which is denoted by \(\textbf{v}^{[1]}\prec \textbf{v}^{[2]}\).
General speaking, when \(\textbf{v}^{[1]}\prec \textbf{v}^{[2]}\), the components in \(\textbf{v}^{[1]}\) are more diverse than those in \(\textbf{v}^{[2]}\). Next, define \(\textbf{q}^{(j)}=(a^{(j)}_1\cdot p_1, a^{(j)}_2 \cdot p_2, \dots , a^{(j)}_n \cdot p_n)\), which represents the arrival probabilities of all n patients to panel-j for a given patient assignment \(\textbf{a}^{(j)}\). In addition, let \(\textbf{q}^{[j]}\) be \(\textbf{q}^{(j)}\) sorted in descending order. We can then rewrite Equations (2) and (3) as
and
From (6), we can see that the expected demand for assignment \(\textbf{a}^{(j)}\) is \(E[Q_j (\textbf{a}^{(j)})]= \sum _{i=1}^{n}q^{[j]}_i\) from the fact that the patient’s arrival follows Bernoulli distribution. In other words, we say two panels j and \(j'\) have equal load when \(E[Q_j (\textbf{a}^{(j)})]=E[Q_j (\textbf{a}^{(j')})]\), which implies that \( \sum _{i=1}^{n}q^{[j]}_i= \sum _{i=1}^{n}q^{[j']}_i\) . We next present the main result by utilizing majorization theory.
Lemma 1
Suppose that \(\textbf{a}^{(H)}\) is a panel assignment that includes the first r patients with the highest arrival probabilities and \(\textbf{a}^{(L)}\) is an assignment that includes the last l patients with the lowest arrival probabilities. Assume that r and l are chosen such that \(E[Q_j (\textbf{a}^{(L)})]=E[Q_j (\textbf{a}^{(H)})]\). Then, for any arbitrary assignment \(\textbf{a}^{(j)}\) such that \(E[Q_j (\textbf{a}^{(L)})]=E[Q_j (\textbf{a}^{(H)})]=E[Q_j (\textbf{a}^{(j)})]\), \(\textbf{q}^{(L)} \prec \textbf{q}^{(j)} \prec \textbf{q}^{(H)}\) holds.
Proof
Based on the definition, \(\textbf{q}^{(H)}\!=\!\{q^{(H)}_{1},\dots , q^{(H)}_{r}, q^{(H)}_{r+1},\) \( \dots , q^{(H)}_n\}\), where \(q^{(H)}_{i}=p_i\) for \(i\le r\) and \(q^{(H)}_{i}=0\) for \(r+1\le i\le n\). Hence, we observe \(\sum _i^k q^{(H)}_i\ge \sum _i^k q^{(j)}\) for all \(k\le r\) because \(q^{(H)}_i \ge q^{(j)}_i\) for all \(i \le r\). Moreover, because \(\sum _i^k q^{(H)}_i = \sum _i^n q^{(j)}_i\) for all \(r+1\le k \le n\), we further determine that \(\sum _i^k q^{(H)}_i\ge \sum _i^k q_i^{(j)}\) for all \(r+1 \le k \le n\) from the fact that \(q^{(H)}_i = 0\) and \(q^{(j)}_i\ge 0\) for all \(r+1 \le k \le n\). Hence, \(\textbf{q}^{(j)} \prec \textbf{q}^{(H)}\) by Definition 2. Using the same arguments, we can show \(\textbf{q}^{(L)} \prec \textbf{q}^{(j)}\). We omit the details and conclude with the proof. \(\square \)
According to Lemma 1, it is clear that in terms of arrival probability, a panel with lower visit frequency patients is majorized by any panel assignments with an equal load. Similarly, a panel with higher visit frequency patients dominates any other panel assignments with an equal load. This helps us investigate the patient visit variability for different assignments next.
Lemma 2
For any two patient assignments \(\textbf{a}^{(j)}\) and \(\textbf{a}^{(j')}\) such that \(\textbf{q}^{[j']} \prec \textbf{q}^{[j]}\), the convex order \(Q_j (\textbf{a}^{(j)})\le _{cx} Q_j (\textbf{a}^{(j')})\) holds.
Proof
For any integer-convex mapping \(\varphi : \mathbb {N} \rightarrow \mathbb {R}\), where the mapping \(\Phi :[0,1]^n \rightarrow \mathbb {R}\) is defined as
Because \(B(q_i)\) are independent random variables with Bernoulli distributions, \(\Phi _n\) is Schur-convave in \(\textbf{q}\) (see F.1 Proposition on Page 474 in Marshall et al. [25]). From the definition of Schur-concave and the fact that \(\textbf{q}^{[j']} \prec \textbf{q}^{[j]}\), we obtain \(\Phi _n(\textbf{q}^{[j']} ) \le \Phi _n(\textbf{q}^{[j]})\). Next, because \(\Phi _n(\textbf{q}^{[j']} ) \le \Phi _n(\textbf{q}^{[j]})\) for all convex \(\varphi \), we obtain \(\sum _{i=1}^{n}B(q_i^{[j]})\le _{cx} \sum _{i=1}^{n}B(q_i^{[j']})\) based on the definition of convex ordering. Because \(Q_j (\mathbf {a^{(j)}}) = \sum _{i=1}^{n}B(q_i^{[j]}) \) in Equation (6), \(Q_j (\textbf{a}^{(j)})\le _{cx} Q_j (\textbf{a}^{(j')})\) can be obtained and the prove is concluded.
According to a well-known property of convex ordering of random variables shown in literature (e.g., Shaked and Shanthikumar [35]), when \(Q_j (\textbf{a}^{(j)})\le _{cx} Q_j (\textbf{a}^{(j')})\), \(\textrm{Var} (Q_j (\textbf{a}^{(j)})) \le \textrm{Var} (Q_j (\textbf{a}^{(j')}))\) is implied. When Lemmas 1 and 2 are combined, we reach the following conclusion. While all panels share the same patient load, a panel with more high PDC patients incurs a lower demand variability than that of a panel with more low PDC patients. The demand variability from a panel under equal panel assignment is in the middle. This leads to the following main result.
Theorem 1
For any two patient assignments \(\textbf{a}^{(j)}\) and \(\textbf{a}^{(j')}\) with equal patient demand load, if their corresponding \(\textbf{q}^{[j]} \prec \textbf{q}^{[j']}\) holds, then \(\pi _j(\mathbf {a^{(j)}}) \ge \pi _{j'}(\mathbf {a^{(j')}})\).
Proof
The proof is based on the results shown in Bondar [8], Gleser [14], Karlin and Novikof [19] and Rinott [32]. Specifically, suppose that \(X_i\) are independent random variables with Bernoulli distributions with probability \(p_i\) for \(i=1, \dots ,n\). For two vectors \(\textbf{p}=(p_1,\dots p_n)\) and \(\textbf{r}=(\hat{p}_1,\dots \hat{p}_n)\) where \(\textbf{r}\prec \textbf{p}\), the inequality
hold if \(f(\cdot ):\{0,1,\dots ,n\}\rightarrow \mathbb {R}\) is convex. The statement of the proposition follows from the logic based on the fact that the arrival distributions are independent Bernoulli, \(\textbf{q}^{[j]} \prec \textbf{q}^{[j']}\) and \(\pi _j(\cdot )\) is convex. \(\square \)
The result presented in Theorem 1 can be explained as follows. Given that the workloads are the same for any two panels, the panel that is majorized by the other incurs a higher supply shortage. This, along with Lemma 1, shows that a smaller panel formed by high-PDC patients incurs a lower shortage than a larger panel formed by patients requiring fewer visits. A more intuitive explanation can be supported by Lemma 2, in which we indicate that the high-PDC panel can incur a lower arrival variability hence improving the performance.
For a one-panel only clinic, having a smaller panel with patients who visit more frequently helps reduce the overall shortage, assuming we do not need to consider other cost factors. In a two-panel example, a clinic will have one small panel consisting of patients who visit more often and one large panel with patients who visit less frequently with specialized panel assignment. In equal panel assignment, a clinic will have two identical panels in size and patient composition. Based on Theorem 1, it can be shown that the panel with high-PDC patients has the best performance, whereas the panel with low-PDC patients has the worst. Also, a panel from equal panel assignment performs in the middle.
The above results also imply that a high-PDC panel has a stronger ability to handle patients with higher shortage costs. This is beneficial when high-cost patients require more frequent care. However, it is unclear whether specialized panel assignment consisting of the best and the worst performance panels can outperform equal panel assignment with two panels with average performance when we consider the overall combined performance. Therefore, we investigate such scenarios with the help of numerical analysis.
6 Numerical analysis
This section provides numerical examples to compare the combined performance of the two assignments under various scenarios. Specifically, we investigate the effect of shortage penalty, supply capacity, and the homogeneity of patients via separate examples. For ease of presentation, we assume that the system contains only two patient types, and that the arrival probabilities for all patients of the same type are the same. Although this assumption is not required in our model, it helps highlight the difference between the two designs. Moreover, not all patient pools can have patients to be distributed to panels with equal workloads under the two designs. For example, a patient pool that contains six patients with arrival probabilities of [0.2, 0.2, 0.1, 0.1, 0.1, 0.1] can be assigned to two equally loaded panels in both assignments. However, it is impossible to create equally-loaded panels under equal panel assignment for a three-patient pool with arrival probabilities of [0.2, 0.1, 0.1]. Restricting the number of patient types allows us to focus on patient pools that can be assigned to panels with the exact workload in the numerical study. We will remove such a limitation in the experiment presented in Section 6, where patient arrival frequencies are sampled from the real patient data. In other words, each patient is categorized as an individual patient type, as assumed in the model formulation.
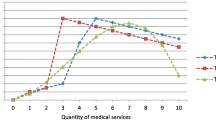
6.1 The effect of the supply capacity
The first scenario investigates the results when the system has different capacity settings. We assume that the total expected patient demand is 80 appointments per period. In both assignments, patients are allocated to the two panels with equal load (e.g., an average of 40 requests per period for each panel). We also vary the appointment slots (or capacity) from 32 to 48 for each panel. In other words, we consider that the system has a supply surplus (respectively, shortage) when the capacity is higher (respectively, lower) than 40. We then compare the supply shortage of the two panel designs and present the results in Fig. 3.
The x-axis represents the capacity provided in each panel. In this example, we assume that the shortage penalties for high-PDC and low-PDC patients are the same. Hence, the y-axis simply represents the relative shortage difference between the two designs. When this cost difference exceeds 0, specialized panel assignment provides a better outcome (e.g., less shortage). In Fig. 3, specialized panel assignment incurs less shortage than equal panel assignment when capacity and demand are relatively balanced (e.g., when the capacity is approximately between 36 and 46). However, when capacity and demand are significantly imbalanced (e.g., capacity is either below 36 or above 46), equal panel assignment performs better than specialized panel assignment. This result is especially notable when a significant capacity surplus exists. When a capacity shortage occurs, the difference between the two designs is insignificant. In addition, the difference between the two designs is more notable when the arrival probabilities of the two patient types are more heterogeneous (e.g., \(p_H=0.6\) and \(p_L=0.04\)).
The results presented in Fig. 3 provide a general guideline for clinics to minimize the expected shortage. We demonstrate with an example next to show how assignment change can affect performance when patient demand increases. We start with two equally assigned panels with the expected demand of 20 per panel and fix the capacity to 40 per panel. Specifically, there are 40 high-PDC patients with \(p_H=0.25\) and 250 low-PDC patients with \(p_L=0.04\) in each panel. In each round, we add eight new high-PDC patients and 50 new low-PDC patients to join the two panels. These parameters are chosen for two reasons: (1) to keep the workload equal for both high and low-PDC patients (e.g., eight new high-PDC patients and 50 new low-PDC generate the same expected arrivals); (2) to ensure that all new patients can be divided equally into two panels (e.g., must be even number of patients). Two new-patient policies are evaluated. In the first policy, the new high-PDC patients are assigned to the first panel, and the low-PDC patients are assigned to the second panel. In the second policy, new patients of both PDC types are assigned equally to the two panels. In other words, the two panels under the first policy will gradually approach specialized panel assignment design while the second policy maintains equal panel assignment. The process is repeated until the expected arrival per panel reaches 70.
The results of the above example are shown in Fig. 4. Note that a negative shortage difference means the first policy that aims to achieve specialized panel assignment has expected lower shortage than the second policy that maintains equal panel assignment. We observe that as more patients are added to the two panels, the second policy is slightly better. However, when the demand continuously increases, the first policy outperforms the second one. Finally, the second policy works better again when we have a moderate capacity shortage and the difference between the two policies disappears when the arrival overwhelms the capacity. Note that because we do not reassign existing patients in this example, the first policy can not fully achieve specialized panel assignment. If we allow all patients to be reshuffled each time when new patients arrive, the region that the first policy outperforms can expand. Overall, the pattern shown in Fig. 4 is consistent with the findings shown in Fig. 3.
When the physician capacity exceeds patient demand, a clinic should distribute patients uniformly across available panels. Once demand increases, new patients should be allocated based on their predicted arrival frequencies. When existing patients decide to switch panels voluntarily, they should also be encouraged to choose from panels that match their historical or predicted arrival probabilities. Once the patient demand outgrows the capacity, increasing the capacity can be more crucial than changing the panel allocation.
6.2 The effect of the physician shortage penalty
This section compares the performance of the two panel assignments under different cost schemes. We establish the shortage cost for low-PDC patients as 1 and vary the shortage cost for high-PDC patients from 0.2 to 2. When the shortage cost for high-PDC patients is higher (respectively, lower) than 1, it implies that patients who require more (respectively, less) frequent visits face more severe consequences when their service access is denied or delayed. All other parameters are kept unchanged from Section 5.1. In addition, we assume that demand and supply are balanced. The results are illustrated in Fig. 5.
We observe that equal panel assignment has a lower shortage cost as compared to specialized panel assignment when the shortage cost for high-PDC patients is much lower than that for the low-PDC patients (e.g., \(c_H\) is less than 0.8 approximately). However, specialized assignment performs better when the shortage cost for high-PDC patients is higher (e.g., \(c_H\) is greater than 0.8). Again, the difference between the two designs is more significant when the arrival probabilities of the two patient types are heterogeneous.
This result can be explained as follows. Recall from Theorem 1, the panel with low-PDC patients suffers a higher expected shortage than the panel with high-PDC patients. Hence, patients who are denied timely access are more likely to be in the low-PDC patient panel for a clinic that utilizes the specialized panel assignment. Consequently, when the shortage penalty for low-PDC patients is higher than that for high-PDC patients, specialized panel assignment is affected more, making it less plausible. However, when the shortage penalty for high-PDC patients is higher, the clinic’s overall performance is less likely to be affected because the shortage cost for a low-performance panel (e.g., low-PDC panel) is far less.
The same observation can be made in the experiment presented in Fig. 6 which investigates the effect of arrival probability on the shortage cost of the two designs. Specifically, we set \(p_L=0.1\) and change \(p_H\) from 0.1 to 0.5. The number of patients for both patient types is adjusted to match the capacity of 40 per panel, and we test three different cost schemes. The results demonstrate that the specialized assignment performs better, especially when the arrival probabilities for the two patient types differ more and a high shortage penalty is associated with high-PDC patients. However, when the shortage cost for the low-PDC patients is higher (e.g., \(c_H=0.5\) and \(c_L=1\)), equal assignment performs better. In this example, supply and capacity are balanced. However, we may obtain a completely different result when a significant supply shortage exists. We will discuss these scenarios next.
We reorganize the results for a two-panel example and represent the effect of shortage penalty, supply capacity, and the homogeneity of patients for a more detailed analysis. In Fig. 7, we compare the two assignments under different panel capacities (e.g., expected demand is 40) and cost ratios (e.g., \(\frac{\textit{high-PDC shortage cost}}{\textit{low-PDC shortage cost}}\)). The four subfigures represent different levels of patient homogeneity in terms of their arrival probabilities. Specifically, Fig. 7a considers cases with the most heterogeneous patients, and Fig. 7d presents the least heterogeneous patients. The darker (respectively, lighter) squares represent a region where equal panel assignment (respectively, specialized panel assignment) is preferred.
When the patients are more heterogeneous, the main determining factor is the balance of capacity and demand. Figure 7a and b show that specialized panel assignment dominates equal assignment when demand and capacity are reasonably matched. However, when the patients are more homogeneous, the shortage cost has a more prominent role. In Fig. 7c and d, specialized panel assignment is better only when the shortage cost for high-PDC patients is higher than other patient types given that demand and capacity generally match or a capacity surplus exists. Conversely, when the capacity is insufficient, specialized panel assignment is better if the shortage cost for high-PDC patients is relatively low. This result was not observed in the previous examples.
To summarize, suppose that the patient arrival probabilities are heterogeneous. The specialized assignment performs well when (i) capacity and demand are balanced, and (ii) the consequence of shortage for high-PDC patients is high. Suppose that the patient arrival probabilities are homogeneous. The specialized panel assignment works well when (1) a capacity surplus and high shortage cost for high-PDC patients exist or (2) a capacity shortage and high shortage cost for low-PDC patients is evident.
6.3 Discussion on panel assignment diversion
This section evaluates the performance of panels when the panel composition diverts from the two target designs. Specifically, we compare all possible panel assignments against the two target assignments in the same two-panel-two-PDC setting. In this numerical example, we start from equal panel assignment. Next, we gradually move high-PDC patients from the second panel to the first and low-PDC patients from the first to the second. We ensure that patients moving in both directions are equally loaded in each adjustment. The adjustments are repeated until specialized panel assignment is fully achieved. This procedure allows us to include all possible assignments while maintaining identical expected arrivals on both panels. The parameters are \(p_H=0.25\) with 160 high-PDC patients and \(p_L=0.04\) with 1000 low-PDC patients (e.g., an average of 40 arrivals per panel). The results are shown in Fig. 8.
In Fig. 8a and b, the left-most column represents equal panel assignment, and the right-most column represents specialized panel assignment. Other columns represent results from all other feasible assignments. Generally, the results from columns toward the left are more similar to equal panel assignment, and those toward the right are closer to specialized panel assignment. The y-axis shows the percentage of shortage increase of each assignment against the optimal assignment.
This result is valuable for the following reasons. As mentioned earlier in the paper, new patients may join the panel, and existing patients may change physicians voluntarily. Hence, it is very likely an optimal panel assignment cannot be fully achieved. However, Fig. 8 demonstrates that when a clinic knows that specialized panel assignment (or equal panel assignment) is better for the system, any panel adjustments that move toward the target design are beneficial.
6.4 Scenario with more than two panels (\(m>2\))
This section extends our analysis to a system with more than two physician panels. Similar to the setup used in Section 5.1, we investigate the results when the system has a supply surplus or shortage. We assume that the total expected patient demand is 120 visits per period. In both designs, patients are distributed among three equally loaded panels. The results presented in Fig. 9 illustrate variations in physician’s capacity and patients’ arrival probability parameters.
Consisting with the results shown in the two-panel example, specialized panel assignment produces less shortage when supply and demand match. However, equal panel assignment performs significantly better when a supply surplus exists, especially when the arrival probabilities of the three patient types are relatively heterogeneous. This result does not change when we increase the number of panels to more than three. However, we might observe the opposite when the capacity is significantly lower than the panel demand. An exception will be discussed next.
In Fig. 10, we change the shortage cost for high-PDC and low-PDC patients while keeping the cost for medium-PDC patients to 1. In other words, Region I represents cases where low-PDC (respectively, high-PDC) patients incur the highest (respectively, lowest) shortage penalty. Conversely, Region IV represents cases where low-PDC (respectively, high-PDC) patients incur the lowest (respectively, highest) shortage penalty. Although less intuitive, Regions II and III represent scenarios in which medium-PDC patients incur the lowest shortage (respectively, highest) cost. In addition, while maintaining the panel demand at 36, we consider three aspects: supply surplus (e.g., \(k=38\) in Fig. 10a), balanced supply (e.g., \(k=36\) in Fig. 10b), and supply shortage (e.g., \(k=32\) in Fig. 10c). The arrival probabilities for the three patient types are \(p_H=0.3\), \(p_M=0.25\), and \(p_L=0.3\).
We found that equal assignment is generally better when the shortage penalty of low-PDC patients is relatively higher than that of high-PDC patients, especially when a capacity surplus exists. However, as Fig. 10c illustrates, the equal assignment can be better when the shortage penalty of low-PDC patients is relatively lower than that of the high-PDC patients. This result is similar to those shown in Fig. 7c and d and may only occur when the arrival probabilities are similar across different patient types.
7 An experiment with real appointment data
In this section, we turn our focus to the practical issues of the two assignments in a realistic environment. In the US, patients can choose to change their physicians within the insurance network without many restrictions. Hence, it is unlikely that the panel assignment matches the design perfectly. There are other considerations. For example, patient shortage costs may not be directly correlated to their visiting frequency. Also, the arrival frequencies of patients can be different. Hence, it may not be possible to assign patients to panels with completely equal loads (as we did in Section 5) when there are only two possible arrival probabilities. Considering these uncertainties, evaluating the robustness of the design in practice is essential because it helps us understand our model when assumptions can not be perfectly met. To do that, we rely on actual patients’ appointment information in a simulation model to evaluate the potential shortage cost under the two assignments. The detailed process is as follows.
7.1 The experiment setup
We utilize patients’ appointment records from a healthcare provider system in the US Midwest region. Specifically, the dataset included 573,642 primary care physician visit records from 237,353 patients in 2007 (see Fig. 11 for distributions). Table 1 provides information about the dataset at the aggregate level. The identities of patients and physicians in the dataset are censored to maintain anonymity. Because we only have patient records in the dataset when visits occurred in 2007, obtaining reliable panel composition information for each physician was not possible given the low physician match rate (e.g., seeing a patient’s primary care physician) in Table 1. For this experiment, we utilize only patients’ arrival frequency (e.g., number of arrivals in a year) and age group(e.g., 1-4, 5-17, 18-64, or 65+) from the data to create a patient pool.
We randomly select patients from this patient pool until the desired expected demand is met. These patients form the patient body to be assigned to panels in our experiment. Note that the number of patients in the patient body varies depending on their arrival frequencies. In other words, the patient pool is larger when more patients who require fewer visits are selected. Next, we assign these patients to panels based on the two designs. For specialized panel assignment, we sort the patients based on their arrival frequencies. Then, we assign patients from the sorted list until the current panel reaches its desired expected demand before moving to the next panel. For equal panel assignment, we assign patients from this sorted list one at a time to different panels following a round-robin mechanism.
Unlike the numerical study in the previous section, the expected workload for each panel in this section can differ because we use real patient data, which often cannot be divided equally. Lastly, we simulate the weekly demand based on patients’ arrival probability and calculate the shortage and the corresponding cost based on denied patients’ age groups. The description of this process is illustrated in Fig. 12.
7.2 Patient composition in the experiment
We discuss patient composition in the experiment to highlight the similarities and differences between our model assumption and the reality in practice. All figures and examples in this section are based on one randomly selected patient pool in which we set the daily expected demand and panel capacity to 20 patients with 18,000 observations (e.g., one observation represents one week). Note that patient composition can differ for each random patient pool, however, it does not affect the findings presented.
Figure 13 presents the patient arrival frequency for the two panels under the two assignments. All patients with higher visit frequencies are assigned to the high-PDC panel under specialized panel assignment. Conversely, patients are uniformly distributed between the two panels under equal panel assignment. However, as discussed previously, obtaining perfectly identical panels and workload in the experiment is unlikely. This can be observed in Fig. 13a, where the distributions for the two panels under equal panel assignment are not identical. Note that Fig. 13a and b are based on the same experiment. To make our point, we hide outliers in Fig. 13b to highlight the differences and similarities in arrival distribution under different designs.
Another difference between our model and the experiment shown in this section is the assumption of the shortage cost. Our model assumes that the shortage penalty matches the arrival probabilities (e.g., a higher shortage cost for high-PDC patients). However, we do not make such an assumption explicitly in this experiment. Instead, we assume that the shortage cost is associated with patients’ age groups. Specifically, a cost index (presented in Table 2) is applied to the experiment. Based on Table 2, the shortage cost for toddlers (e.g., below five years old) is 1.5 times the cost for adults, and the shortage cost for seniors (e.g., above 65 years old) is twice the cost for adults. Note that in such a setup, while a higher visit frequency may not imply a higher shortage cost at the individual level, a panel with more high-PDC patients does have a higher unit shortage cost at the aggregate level because toddlers and seniors in our dataset have higher visiting frequency in general.
Next, we discuss the age groups in our patient pool. Table 3 presents the age distribution for each panel under the two designs; however, the patients are assigned based on their visiting frequencies, not their age groups. We find a significant difference in age distribution between low-PDC and high-PDC panels (\(\chi ^2 (3,N=3685)=120.669\) and \(p\le .001\)). This is intuitive because patient age and visit frequency are often correlated in practice. As expected, there is no statistical difference between the age distributions of the two panels (\(\chi ^2 (3,N=3685)=4.474\) and \(p=.215\)) under equal panel assignment although they are visually different.
The difference in age distribution also affects the unit shortage cost in panels. Figure 14 presents the distribution of the per unit shortage cost for the 18,000 observations in the experiment. Note that the per unit shortage cost is calculated based on patients seeking service that week. Thus, depending on the randomly generated arrivals, the cost differs weekly. However, the unit cost per shortage for the high-PDC panel is the highest, whereas that for the low-PDC panel is the lowest. This is mainly because the high-PDC panel has a higher proportion of toddlers and seniors, and both are associated with higher cost indexes. Moreover, although the composition of the two panels in equal panel assignment is very similar, their cost distributions have a notable difference. The results in Fig. 14 imply that assumptions about cost and visit frequency generally hold, although exceptions exist in the data.
7.3 Experiment results
This section presents the results of the experiment. Figure 15 illustrates how the average shortage for each panel changes over time. Generally, the simulation begins to stabilize at approximately 1,500 observations. To ensure a more reliable conclusion, we run the simulation for at least 15,000 to 20,000 observations for each scenario and present the long-run average.
In the first set of experiments, we compare the two assignments when we vary the daily capacity from 15 to 22 appointments (e.g., from provider shortage to overage). The daily expected demand is set to 20 appointments, and the cost index is set to [1.5,1,1,2]. The results in Table 4 indicate that when supply and demand are better aligned, specialized panel assignment results in a lower shortage cost. However, equal panel assignment performs better when a significant capacity surplus or shortage exists. For example, when the capacity is 21, specialized panel assignment can save 0.76% per week compared to equal panel assignment. This is consistent with the results in Section 5.1 which also demonstrate that specialized panel assignment incurs a lower shortage cost when supply and demand are balanced.
In the following scenario, we evaluate the effect of the age group cost index. We maintain balanced supply and demand (e.g., an average of 20 daily appointments per panel) and vary the cost index for seniors from 3 to 10 (e.g., 3 to 10 times the cost of healthy adults). Based on the results in Table 5, we determine that the benefit of specialized panel assignment is more significant when the cost for seniors is higher. For example, when the cost index for seniors is 10, specialized panel assignment saves 1.67% per week compared to equal panel assignment. This conclusion is consistent with the results presented in Fig. 4 in Section 5, which indicate that specialized panel assignment performs better when the shortage cost for patients with higher PDC is relatively higher.
In the final experiment, we study how results are affected when the panel composition diverges from the intended design. In other words, we want to learn how the conclusion holds when patients can move between panels. Thus, we evaluate two scenarios. In the first scenario, we assume that 5% of the patients from the high-PDC panel will move to the low-PDC panel each time. In the second scenario, we assume a one-time change during which a certain percentage of patients from the high-PDC panel will move to the low-PDC panel. In both cases, randomly selected patients from the low-PDC will also move to the high-PDC panel to ensure that the workloads between the two panels are balanced. In addition, the number of patients moving from the high-PDC panel to the low-PDC panel is generally fewer than the reverse because patients from high-PDC have higher visiting frequencies.
The results for the two scenarios are presented in Figs. 16 and 17, respectively. We determine that the system can tolerate 5% of the patients switching 10-20 times without compromising the benefit of specialized panel assignment. Similarly, we found that specialized panel assignment can generally accept a 10% - 20% diversion from its designed assignment. When the patients in the panels diverge further, the advantage of having specialized panel assignment disappears. This is because the difference in patient composition between the high-PDC and low-PDC panels no longer exists after significant changes. However, our results are robust and can handle deviations due to reasonable patient movement.
8 Conclusion
Both panel size and patient composition play an important role in determining the overall workload of a physician. An adequately designed panel assignment improves patient access to their healthcare provider and helps better allocate valuable and limited medical resources. We constructed a stylized model and utilized majorization theory to evaluate two implementable panel-assignment strategies: specialized panel assignment and equal panel assignment.
We contribute to panel design literature by providing a general guideline for allocating new patients and reallocating existing patients who decide to switch physicians. Our analysis demonstrates that a smaller panel with patients who require more frequent visits is less likely to experience a supply shortage than a larger panel with low-PDC patients. The benefits of specialized panel assignment depend on the patient’s arrival frequencies, cost of delayed service, and the balance between physician capacity and patient demand. We determined that equal panel assignment performs better than specialized panel assignment only when the overall supply and demand are imbalanced. In addition, we discovered that the consequences of denied/delayed access highly influence the results. For example, if the penalty for delaying service for high-PDC patients is high, specialized panel assignment performs better. Alternatively, if the penalty for delaying service for low-PDC patients is high, it is better to utilize equal panel assignment.
We emphasize that the goal of panel design is not to redistribute all patients at once because doing so severely disrupts the existing physician-patient relationship. Our approach identified the characteristics of the two panel designs. By utilizing a simulation model with actual appointment data, we verify that our findings are robust and can allow a reasonable divergence from the intended assignment without compromising the design advantage. This means that forming strategies to encourage patients to switch panels can be beneficial for clinic to achieve a better outcome and potentially minimize pushback from patients. For instance, the healthcare system can strategically open and close specific panels for accepting patients and naturally redistribute them to different panels over time. Various other healthcare systems even offer incentives to patients to move by providing more assistance or offering a better facility to the panels with a supply surplus.
Overall, a panel design problem is more significant for integrated healthcare delivery systems such as Kaiser Permanente and the VA systems. Unlike many private healthcare systems that give physicians more power to manage their own panel rather than focusing on the overall system performance, integrated healthcare delivery systems provide more substantial incentives and control for administration to improve the panel assignment policy. Integrated health delivery systems also make specialized panel assignment more desirable and further reduce operation costs by utilizing non-physician personnel such as nurse practitioners to serve panels of healthier patients without medical complications.
This study has limitations. In the current model, we assume that the penalty cost is linear in overflow. However, depending on the appointment and schedule policy, the penalty cost might potentially be nonlinear in overflow. As mentioned earlier, our model addresses the panel design problem at an aggregate level. We do not consider any specific appointment systems. However, it is evident that appointment strategies-such as open access, same-day appointments, and overbooking-affect the ability to digest patient overflow. Thus, one extension would be to evaluate the panel designs based on different cost functions generated by various appointment strategies. Alternatively, one could consider evaluating the designs from another approach, such as a queueing system, to highlight the effect on visit delays. One might also consider visit frequency and other factors, such as age, gender, and health status, to determine a more sophisticated panel design policy, or consider patient behavior changes due to aging or other factors. Other extensions would be to view the panel design problem from the healthcare provider’s perspective, considering their revenue and operational cost in the decision process.
References
Altschuler J, Margolius D, Bodenheimer T, Grumbach K (2012) Estimating a reasonable patient panel size for primary care physicians with team-based task delegation. Ann Fam Med 10(5):396–400
Angstman KB, Horn JL, Bernard ME, Kresin MM, Klavetter EW, Maxson J, Willis FB, Grover ML, Bryan MJ, Thacher TD (2016) Family medicine panel size with care teams: Impact on quality. J Am Board Fam Med 29(4):444–451
Balasubramanian H, Banerjee R, Denton B, Naessens J, Stahl J (2010) Improving clinical access and continuity through physician panel redesign. J Gen Intern Med 25(10):1109–1115
Balasubramanian H, Muriel A, Ozen A, Wang L, Gao X, Hippchen J (2013) Capacity Allocation and Flexibility in Primary Care. Springer, New York, New York, NY, pp 205–228
Balasubramanian H, Denton BT, Lin QM (2016) Managing physician panels in primary care. In: Handbook of Healthcare Delivery Systems, CRC Press, chap 10
Bavafa H, Savin SV, Terwiesch C (2019) Managing patient panels with non-physician providers. Prod Oper Manag 28:1577–1593
Bavafa H, Savin S, Terwiesch C (2021) Customizing primary care delivery using e-visits. Prod Oper Manag 30(11):4306–4327
Bondar JV (1994) Inequalities: Theory of majorization and its applications: by albert w. marshall and ingram olkin. Linear Algebra and its Applications 199:115–130, special Issue Honoring Ingram Olkin
Dahrouge S, Hogg W, Younger J, Muggah E, Russell G, Glazier RH (2016) Primary care physician panel size and quality of care: A population-based study in ontario, canada. Ann Fam Med 14(1):26–33
Edwards ST, Marino M, Balasubramanian BA, Valenzuela SH, Springer R, Solberg L, Preston A, Cohen D (2017) Burnout among primary care providers and staff in small to medium sized primary care practices: Early findings from evidencenow. J Gen Intern Med 32:83–808
Francis M, Zahnd WE, Varney AJ, Scaife S (2009) Effect of number of clinics and panel size on patient continuity for medical residents. J Grad Med Educ 1(2):310–5
Gill J (2000) The effect of continuity of care on emergency department use. Arch Fam Med 9:333–338
Gill J, Mainous A (1998) The role of provider continuity in preventing hospitalizations. Arch Fam Med 7(4):352–7
Gleser LJ (1975) On the distribution of the number of successes in independent trials. Ann Probab 3(1):182–188
Goldberg D, Soylu T, Kitsantas P, Grady V, Elward K, Nichols L (2021) Burnout among primary care providers and staff: Evaluating the association with practice adaptive reserve and individual behaviors. J Gen Intern Med 36
Green L, Savin SV (2008) Reducing delays for medical appointments: A queueing approach. Oper Res 56:1526–1538
Green LV, Savin S, Murray M (2007) Providing timely access to care: What is the right patient panel size? The Joint Commission Journal on Quality and Patient Safety 33(4):211–218
Helfrich C, Simonetti J, Clinton WL, Wood GB, Taylor LL, Schectman G, Stark R, Rubenstein L, Fihn S, Nelson K (2017) The association of team-specific workload and staffing with odds of burnout among va primary care team members. J Gen Intern Medi 32:760–766
Karlin S, Novikoff A (1963) Generalized convex inequalities. Pac J Math 13(4):1251–1279
Kroll LE, Lampert T (2013) Direct costs of inequalities in health care utilization in germany 1994 to 2009: a top-down projection. BMC Health Serv Res 13(271)
Lane NE, Ling V, Glazier RH, Stukel TA (2021) Primary care physician volume and quality of care for older adults with dementia: a retrospective cohort study. BMC Fam Pract 22(1):51
Liu N, Ziya S (2014) Panel size and overbooking decisions for appointment-based services under patient no-shows. Prod Oper Manag 23:2209–2223
Margolius D, Gunzler D, Hopkins M, Teng K (2018) Panel size, clinician time in clinic, and access to appointments. Ann Fam Med 16(6):546–548
Margolius D, Siff J, Teng K, Einstadter D, Gunzler D, Bolen S (2020) Primary care physician factors associated with inbox message volume. J Am Board Fam Med 33:460–462
Marshall W, Olkin I, Arnold B (2011) Inequalities: Theory of Majorization and Its Applications, 2nd edn. Springer Series in Statistics. Springer
McCleery E, Christensen V, Peterson K, Humphrey L, Helfand M (2011) Evidence brief: The quality of care provided by advanced practice nurses. Tech. rep, VA Evidence Synthesis Program Reports
Hawkins Merritt (2017) 2017 survey of physician appointment wait times. Tech. rep, Merritt Hawkins
Mohr DC, Benzer JK, Young GJ (2013) Provider workload and quality of care in primary care settings: Moderating role of relational climate. Med Care 51(1):108–114
Murray M, Davies M, Boushon B (2007) Panel size: how many patients can one doctor manage? Family Pract Manag 14(4):44–51
Ozen A, Balasubramanian H (2013) The impact of case mix on timely access to appointments in a primary care group practice. Health Care Manag Sci 16:101–118
Rajkomar A, Yim J, Grumbach K, Parekh A (2016) Weighting primary care patient panel size: A novel electronic health record-derived measure using machine learning. JMIR Medical Informatics 4
Rinott Y (1973) Multivariate majorization and rearrangement inequalities with some applications to probability and statistics. Israel J Math 15(1):60–77
Rossi MC, Balasubramanian H (2018) Panel size, office visits, and care coordination events: A new workload estimation methodology based on patient longitudinal event histories. MDM Policy Pract 3(2)
Rust G, Ye J, Baltrus P, Daniels E, Adesunloye B, Fryer GE (2008) Practical Barriers to Timely Primary Care Access: Impact on Adult Use of Emergency Department Services. Arch Intern Med 168(15):1705–1710
Shaked M, Shanthikumar JG (1994) Stochastic Orders and Their Applications. Academic Press
Stefos T, Burgess J, Mayo-Smith M, Frisbee KL, Harvey HB, Lehner L, Lo S, Moran E (2011) The effect of physician panel size on health care outcomes. Health Serv Manag Res 24:105–96
Zacharias C, Armony M (2017) Joint panel sizing and appointment scheduling in outpatient care. Manag Sci 63(11):3978–3997
Acknowledgements
We would like to thank the department editor, associate editor, and the three anonymous reviewers for taking the time and effort during the review process. We sincerely appreciate all valuable comments and suggestions that helped improve our paper.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
A part of this research is supported by Research Awards and Fellowships from the University of Toledo under Grant No. l-26885-01. No other relevant financial or non-financial interests to disclose. Following the policies of the University of Toledo, ethics approval for the data used in this research was not needed. Due to the sensitive nature of the information, the provider of the arrival data used in this study did not consent for their data to be shared publicly. Hence, the data used in the simulation of this study are not available.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Supplementary Information
Below is the link to the electronic supplementary material.
Rights and permissions
Springer Nature or its licensor (e.g. a society or other partner) holds exclusive rights to this article under a publishing agreement with the author(s) or other rightsholder(s); author self-archiving of the accepted manuscript version of this article is solely governed by the terms of such publishing agreement and applicable law.
About this article
Cite this article
Chen, HW. Managing a multi-panel clinic with heterogeneous patients. Health Care Manag Sci 26, 673–691 (2023). https://doi.org/10.1007/s10729-023-09658-z
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s10729-023-09658-z