Abstract
A high proportion of ovarian cancers from women who carry germline mutations in mismatch repair (MMR) genes demonstrate microsatellite instability (MSI). The utility of pre-screening ovarian cancer specimens for MSI to identify potential patients for germline screening for MMR mutations is uncertain. 656 women with malignant ovarian cancer underwent both MSI testing and germline mutation testing for large rearrangements in three MMR genes, MLH1, MSH2 and MSH6. Germline DNA sequencing data for the same genes was available. Among the 656 women, only four (0.6%) carried a clearly pathogenic MMR mutation. All four cancers from patients with mutations had loss of two or more microsatellite markers (MSI-high). Eighty-four of 652 (13.0%) women without a mutation had MSI-high ovarian cancers. Using MSI-high as a prescreening criterion, the sensitivity of MSI testing to identify germline MMR gene mutations was 100% and the positive predictive value was 4.5%. Germline mutations in MLH1, MSH2 and MSH6 are rare among unselected cases of ovarian cancer. Patients with germline mutations often will have MSI-positive cancers and pre-screening of ovarian cancer specimens may be an efficient way of identifying patients with Lynch syndrome.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
As many as one quarter of cases of ovarian cancer may be inherited. BRCA1 and BRCA2 mutations account for more than one-half of these [1]. A small proportion of ovarian cancers are found in women from families with Lynch syndrome, an autosomal dominant syndrome of cancer predisposition arising from germline mutations in the mismatch repair (MMR) genes. We have estimated that about 1% of ovarian cancer are attributable to MMR mutations [2]. Women with Lynch syndrome are at high risk for cancers of the ovary, colon and endometrium. The lifetime risk of ovarian cancer among carriers of MMR gene mutations is estimated to be approximately 12% [3] and preventive oophorectomy is an option for these women.
One of the hallmarks of impaired MMR gene function is the presence of microsatellite instability (MSI) in tumor cells [4]. Microsatellites are short, polymorphic sequences of DNA between one and five base pairs that are repeated 15–30 times and occur across the genome [5]. Inactivation of the MMR system leads to the accumulation of mutations, particularly in these highly repeated sequences (microsatellites), leading to MSI [6]. In 1997, the National Cancer Institute (NCI) developed criteria to classify MSI in colorectal cancer [7]. Five specific markers for microsatellite analysis in colorectal cancer were recommended: two mononucleotide repeats (Bat25 and Bat26) and three dinucleotide repeats (D2S123, D5S346 and D17S250). Tumors are classified as having high levels of MSI (MSI-H) if two or more of the five markers exhibit variations in microsatellite sequence length and low level MSI (MSI-L) if one marker has variations.
Evaluation of MSI in a tumour specimen has been proposed to be a sensitive and cost-effective strategy to identify colon cancer patients for whom germline MMR gene testing is indicated [8–10], but the paradigm has not been applied to ovarian cancer. Further, the costs of DNA sequencing are much lower now than they were a decade ago and it is not clear if there are savings to made by using MSI as a prescreening test prior to panel based DNA sequencing. The objectives of the current study were: (1) to estimate the frequency of point mutations and chromosomal rearrangements in three MMR genes which been implicaitons in MLH1, MSH2, and MSH6 among unselected patients with ovarian cancer, and (2) to assess the utility of MSI analysis as a prescreening test for women with ovarian cancer prior to screening germline DNA for mutations in the MMR genes.
Materials and methods
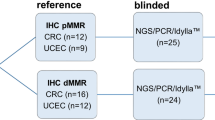
Participants
Data for this study were drawn from three population-based studies of epithelial ovarian cancer: the Familial Ovarian Tumor Study (FOTS) in Toronto [11], the Tampa Bay Ovarian Cancer Study (TBOCS) at the Moffitt Cancer Center [12], and the North Carolina Ovarian Cancer Study (NCOCS) at Duke University [13]. Details about study design, populations, and data collection methods have been published previously. The study protocol was approved by the institutional review board at each center, and written informed consent was obtained from all participants.
Eligibility criteria for study enrollment included diagnosis of incident, pathologically confirmed primary epithelial ovarian cancer, either borderline or invasive, at age 20 years or above in whom an ovarian tumor sample was collected. Participants completed a questionnaire posted to them by mail to collect demographic, clinical, and family history information. Medical and pathology records were collected and reviewed to determine tumor histopathology. Specimen collection included blood for DNA extraction and analysis.
Gene mutation screening
A multiplex ligation-dependent probe amplification (MLPA) test was used for detecting large rearrangements in these genes. MLPA assay P003 (MRC-Holland Inc., Amsterdam, Netherland) was used for the screening of MLH1 and MSH2 genes and MLPA assay P248 was used for confirming the mutations identified in P003 assay. For screening the MSH6 gene for large rearrangements, the MLPA assay P072 was used. For confirming the identified MSH6 exon1 deletion identified by MLPA in some patients, a TaqMan CNV Assay (Assay ID: Hs01984403-cn, Life Technologies Inc, Grand Island, NY, U.S.A) was employed. The RNase P gene was used as a control for the TaqMan CNV assay. The germline DNA sequencing data on the three MMR genes including MLH1, MSH2 and MSH6 were obtained from our other study published previously [2].
Haplotype analysis
Genome-wide genotype data for the eight patients carrying the MSH6 exon1 deletion as well as of four non-carrier patients were obtained using the Illumina HumanCoreExome microarray chip. The chromosome 2 haplotypes were estimated by Beagle software version 3.3.2 [14] using the microarray genotype data.
MSI analyses
Tumor DNA extracted from deparaffinized cells was analyzed by polymerase chain reaction (PCR), using the five standardized microsatellite markers developed by the National Cancer Institute (NCI) for colorectal cancer [7] with germline DNA as the normal control. The standardized markers consisted of two mononucleotide repeats (Bat25 and Bat26) and three dinucleotide repeats (D2S123, D5S346 and D17S250) [7]. Tumors were classified according to shifts in allelic bands as follows: (1) Microsatellite Instability-high (MSI-H) if two or more of the five biomarkers were discrepant between tumour and germline DNA; (2) Microsatellite Instability-low (MSI-L) if one of the 5 biomarkers was discrepant between tumour and germline DNA; and (3) Microsatellite stable (MSS) in all other instances.
Statistical analyses
Participant characteristics were summarized using descriptive statistics, including means and standard deviations for continuous variables and frequencies and proportions for categorical variables. After dividing participants into three groups based on MSI status (MSI-H, MSI-L, and MSS), descriptive statistics were calculated to allow demographic and clinical comparisons across groups. The frequency of germline mutations was determined by dividing the number of participants with identifiable mutations by the total number of participants. MSI-H and mutation status were cross-classified in order to calculate sensitivity, specificity, and positive predictive value (PPV).
Results
Among the 656 ovarian cancer patients in the study, the mean age at diagnosis was 57.1 years (range 20 to 79 years). Demographic and clinical details of the participants are summarized in Table 1.
Germline genetic testing of the coding regions of MLH1, MSH2, and MSH6 identified four clearly pathogenic mutations (0.6%), including one in MLH1, one in MSH2, and 2 in MSH6 (summarized in Table 2). All four of the women with a mutation had MSI-high tumors (Table 2). Of the 644 women without a mutation, 84 had an MSI high tumour (13%). The sensitivity of using MSI-high as a prescreening test was 100%, but this was based on only four cases. The specificity was 87.0% and the positive predictive value was 4.5%.
Discussion
Our study suggests that a germline mutation in one of three MMR genes is present in approximately 0.6% of ovarian cancer patients. Prior reports have been based on smaller samples [15, 16], have not included testing for large rearrangements [15, 16], or have restricted testing to early-onset cases [15]. Recently, a single-institution report of 360 unselected ovarian cancer cases tested for 12 genes through next-generation sequencing. MSH6 mutations were detected in two individuals [1]. Our findings are consistent with a clinic-based study of 67 MLH1, MSH2 and MSH6 mutation carriers that included ten women with ovarian cancer, six of which occurred in MSH6 carriers [17]. None of our families with an MSH6 mutation met clinical diagnostic criteria for Lynch syndrome [18].
Furthermore, our findings suggest there may be utility to using MSI screening to identify those women for whom germline testing for Lynch syndrome mutations should be performed. All women with a Lynch mutation had an MSI-high tumour. If this finding were confirmed in other data sets, it might be justified to offer pre-screening of tumours with MSI. However, the cost of genetic sequencing has declined greatly since this study was initiated and at present MSI is equally expensive as testing for a panel of cancer susceptiblity genes. Also the costs of retrieval of the tumour specimen and processing DNA for MSI analysis is restrictive. Several genes can now be tested simultaneously and at a relatively low cost. For example, mutations in 12 ovarian cancer predisposition genes were evaluated through next-generation sequencing in a study of 360 women with primary ovarian, peritoneal, or fallopian tube carcinoma [1]. Results indicated germline loss of function mutations in 24%, including 18% in BRCA1 and BRCA2, and 6% in the other inherited cancer predisposition genes (including two in MSH6.) These findings, together with the current study, suggest that it may be reasonable to consider germline genetic testing for a wide panel of genes for all unselected cases of ovarian cancer, regardless of family history of cancer. It is important that panel testing should be able to detect large rearrangements, since many of the current next-generation sequencing platforms currently on offer do not detect this kind of mutation.
The issue of screening for ovarian cancer among women with mutations in the MMR genes is matter of clinical importance. Studies have estimated the risk of ovarian cancer among carriers of the mutations to between 8%, or five times higher than expected [19, 20]. At this level of risk, many unaffected carrier women may conclude that preventive bilateral salpingo-ophoreotmy is warranted [19]. At present there is little clinical evidence to support annual screening with CA125 and/or ultrasound [21].
The strengths of the current study include the large sample size, the population-based design, and the comprehensive mutation analysis. Some limitations should be noted. We did not test for PMS2 [19] and EPCAM [20] mutations; testing for these genes whose mutations may predispose to Lynch syndrome has more recently become available but mutation frequencies are very low.
In summary, we estimate that approximately 0.6% of unselected ovarian cancer patients have mutations in the MMR genes. This estimate is much lower than the previous estimate of Walsh et al. [1], but it is not clear if the patients in that study were unselected for family history. The majority of the ovarian cancers from Lynch syndrome patients are MSI-high but we do not not support tumor screening through MSI analysis in ovarian cancer patients to identify those in whom to offer germline MMR gene testing because of cost considerations and because the frequency of these mutations in unselected cases is below one percent. Based on the total frequency of mutations in women with ovarian cancer we currently recommend direct sequencing in all cases of ovarian cancer for BRCA1 and BRCA2 [12, 21] and given the small additional costs, it may be appropriate to add MSH2, MLH1, and PMS2 to the genetic test panel as well.
References
Walsh T, Casadei S, Lee MK et al (2011) Mutations in 12 genes for inherited ovarian, fallopian tube, and peritoneal carcinoma identified by massively parallel sequencing. Proc Natl Acad Sci USA 108:18032–18037
Pal T, Akbari MR, Sun P et al (2012) Frequency of mutations in mismatch repair genes in a population-based study of women with ovarian cancer. Br J Cancer 107:1783–1790
Bonadona V, Bonaïti B, Olschwang S et al (2011) Cancer risks associated with germline mutations in MLH1, MSH2, and MSH6 genes in Lynch syndrome. JAMA 305:2304–2310
Peltomaki, Lothe RA P, Aaltonen LA et al (1993) Microsatellite instability is associated with tumors that characterize the hereditary non-polyposis colorectal carcinoma syndrome. Cancer Res 53:5853–5855
Thibodeau SN, Bren G, Schaid D (1993) Microsatellite instability in cancer of the proximal colon. Science 260:816–819
Parsons R, Li GM, Longley MJ et al (1993) Hypermutability and mismatch repair deficiency in RER + tumor cells. Cell 75:1227–1236
Boland CR, Thibodeau SN, Hamilton SR et al (1998) A national cancer institute workshop on microsatellite instability for cancer detection and familial predisposition: development of international criteria for the determination of microsatellite instability in colorectal cancer. Cancer Res 58:5248–5257
Mvundura M, Grosse SD, Hampel H, Palomaki GE (2010) The cost-effectiveness of genetic testing strategies for Lynch syndrome among newly diagnosed patients with colorectal cancer. Genet Med 12:93–104
Palomaki GE, McClain MR, Melillo S, Hampel HL, Thibodeau SN (2009) EGAPP supplementary evidence review: DNA testing strategies aimed at reducing morbidity and mortality from Lynch syndrome. Genet Med 11:42–65
Evaluation of Genomic Applications in Practice and Prevention (EGAPP) Working Group (2009) Recommendations from the EGAPP Working Group: genetic testing strategies in newly diagnosed individuals with colorectal cancer aimed at reducing morbidity and mortality from Lynch syndrome in relatives. Genet Med 11(1):35–41
Risch HA, McLaughlin JR, Cole DE et al (2001) Prevalence and penetrance of germline BRCA1 and BRCA2 mutations in a population series of 649 women with ovarian cancer. Am J Hum Genet 68:700–710
Pal T, Permuth-Wey J, Betts JA et al (2005) BRCA1 and BRCA2 mutations account for a large proportion of ovarian carcinoma cases. Cancer 104:2807–2816
Wenham RM, Schildkraut JM, McLean K et al (2003) Polymorphisms in BRCA1 and BRCA2 and risk of epithelial ovarian cancer. Clin Cancer Res 9:4396–4403
Browning SR, Browning BL (2007) Rapid and accurate haplotype phasing and missing data inference for whole genome association studies using localized haplotype clustering. Am J Hum Genet 81:1084–1097
Stratton JF, Thompson D, Bobrow L et al (1999) The genetic epidemiology of early-onset epithelial ovarian cancer: a population-based study. Am J Hum Genet 65:1725–1732
Rubin SC, Blackwood MA, Bandera C et al (1998) BRCA1, BRCA2 and hereditary nonpolyposis colorectal cancer gene mutations in an unselected ovarian cancer population: Relationship to family history and implications for genetic testing. Am J Obstet Gynecol 178:670–677
Ramsoekh D, Wagner A, van Leerdam ME et al (2009) Cancer risk in MLH1, MSH2 and MSH6 mutation carriers; different risk profiles may influence clinical management. Hered Cancer Clin Pract 7:17
Vasen HF, Watson P, Mecklin JP, Lynch HT (1999) New clinical criteria for hereditary nonpolyposis colorectal cancer (HNPCC, Lynch syndrome) proposed by the International collaborative group on HNPCC. Gastroenterology 116:1453–1456
Lindor NM, Peterson GM, Hadley DW et al (2006) Recommendations for the care of individuals with an inherited predisposition to Lynch syndrome: a systematic review. JAMA 12:1507–1517
Bonadona V, Bonaiti B, Olschwang S et al (2011) Cancer risks associated with germline mutations in MLH1, MSH2, and MSH6 genes in Lynch syndrome. JAMA 305:2304–2310
Narod SA, Sopik V, Giannakeas V (2016) Should we screen for ovarian cancer? A commentary on the UK collaborative trial of ovarian cancer screening (UKCTOCS) randomized trial. Gynecol Oncol 141(2):191–194
de Jong AE, van Puijenbroek M, Hendriks Y et al (2004) Microsatellite instability, immunohistochemistry, and additional PMS2 staining in suspected hereditary nonpolyposis colorectal cancer. Clin Cancer Res 10:972–980
Kovacs ME, Papp J, Szentirmay Z, Otto S, Olah E (2009) Deletions removing the last exon of TACSTD1 constitute a distinct class of mutations predisposing to Lynch syndrome. Hum Mutat 30:197–203
Zhang S, Royer R, Li S, McLaughlin JR, Rosen B, Risch HA, Fan I, Bradley L, Shaw PA, Narod SA (2011) Frequencies of BRCA1 and BRCA2 mutations among 1,342 unselected patients with invasive ovarian cancer. Gynecol Oncol 121:353–357
Acknowledgements
Financial Support: Supported by grants R01 CA111914 (TP), K07 CA108987 (TP), R01 CA063682 (HAR), R01 CA063678 (SN) and R01 CA080978 (SN) from the National Cancer Institute.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of interest
The author’s declare no conflict of interest.
Additional information
Mohammad R. Akbari and Shiyu Zhang are Joint first authors.
Rights and permissions
About this article
Cite this article
Akbari, M.R., Zhang, S., Cragun, D. et al. Correlation between germline mutations in MMR genes and microsatellite instability in ovarian cancer specimens. Familial Cancer 16, 351–355 (2017). https://doi.org/10.1007/s10689-017-9973-1
Published:
Issue Date:
DOI: https://doi.org/10.1007/s10689-017-9973-1