Abstract
De novo mutations in the adenomatous polyposis coli (APC) gene are estimated to constitute approximately 25% of familial adenomatous polyposis (FAP) cases. A small percentage of these arise in the mosaic form, affecting only a subset of cells in the affected individual. A family is described here whereby an unaffected mother with no detectible mutation in APC, transmitted the identical APC c.4729G>T (p.Glu1577X) mutation to two children. A third child, with the same APC allelic haplotype received a normal APC allele, suggesting that the mutation originated in the gonadal tissues of the mother. These results underscore the utility of mutation-specific genetic testing for the parents and siblings of a proband of an adult-onset disease, even if the proband appears to have a de novo mutation. Parents who test negative for the mutation should be counseled about the possibility of having another affected child due to gonadal mosaicism.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
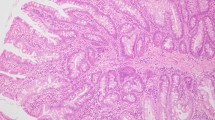
Familial adenomatous polyposis (FAP [MIM 175100]) is an autosomal dominant colorectal cancer predisposition syndrome characterized by hundreds to thousands of colonic polyps and an average age of onset of 16 years. Colon cancer often occurs by the 30s or 40s [1]. Affected individuals also have an increased risk for extra-colonic malignancies including gastric [2], duodenal [3], thyroid [4, 5] and pancreatic cancer [6]. FAP is usually caused by a germline mutation of the adenomatous polyposis coli (APC) gene. However, approximately 25–30% of individuals clinically and genetically diagnosed with FAP have no family history of the condition and appear to represent de novo mutations [7]. In this report, a family with two siblings representing seemingly sporadic cases of FAP, without apparent parental transmission, is investigated for parental mosaicism.
Parental mosaicism was previously reported in a family with FAP in which the mother had a known APC mutation and also had another, second mutation in her germ cells [8]. In addition to this case involving FAP, parental mosaicism has been reported in several other inherited conditions such as Cornelia de Lange [9], myoclonic epilepsy [10, 11], osteogenesis imperfecta [12–16], and even in recurrent miscarriages [17]. The incidence of gonadal mosaicism varies by the condition involved; it is unknown in FAP.
Methods
This study was approved by the Institutional Review Board of the University of Utah. Informed consent was obtained from all research participants.
Research subjects
The family under investigation originally presented to the Family Cancer Assessment Clinic at the University of Utah’s Huntsman Cancer Institute for genetic counseling and testing. The proband reported that he and his sister had a clinical diagnosis of FAP, while both parents were unaffected. After appropriate counseling regarding the possibility of non-paternity and the rarity of gonadal mosaicism, the family elected to enroll in research to evaluate the possibility of parental mosaicism. Phenotype information (including colonoscopy reports, presence or absence of osteomas, dental anomalies and skin findings) was collected on the parents and adult children. Cancer history in extended family was reported by the proband’s parents.
Genetic testing
DNA for research was extracted from lymphoblast and buccal cells using Puregene® DNA Purification Kit, Gentra Systems (Minneapolis, Minnesota) according to manufacturer’s protocols. PCR amplification of genomic DNA of amplicon APC 15-6 (spanning nucleotides c.4304 to c.4904 according to established nomenclature guidelines [18]), was performed using human-specific primers, APC 15-6 Forward, (5′GAAGTAAAACACCTCCACCACC3′) and APC 15-6 Reverse, (5′CCCGGTGTAAAACTAACATGC3′). Standard PCR conditions were followed, using 2.5 mM MgCl2 and an annealing temperature of 60°C. Sequence reactions were performed in both directions on PCR products using APC 15-6 Forward and APC 15-6 Reverse primers. Reaction products were run on Applied Biosystems 3730 capillary sequencer.
Genotyping
A panel of 25 heterozygous short tandem repeat (STR) markers on four chromosomes were used to confirm maternity and paternity, these included D19S210, D19S216, D19S220, D19S221, D19S414, D19S420, D19S884, D19S902, D20S100, D20S107, D20S112, D20S115, D20S117, D20S119, D20S171, D20S186, D20S196, D20S889, D21S1252, D21S266, D22S274, D22S280, D22S420, D22S423, and D22S539. Linkage equilibrium was assumed between alleles on the same chromosomes. At each locus, non-maternity and non-paternity probabilities for each offspring were calculated as the chances that unknown individuals could have been the parents; the product of the prevalences of each STR allele detected for which published allele frequencies were available at http://www.ncbi.nlm.nih.gov/projects/SNP/. For each child, the likelihood of parentage was calculated to be (1-likehood of non-parentage) and was >99.999%. Four STR markers flanking the APC locus (D5S346, D5S2501, D5S2027, and D5S421) were used to determine inheritance patterns of the APC locus. Genetic marker PCR products were resolved on Applied Biosystems 3130xl Genetic Analyzer with a 36-cm capillary using POP-7 polymer.
Allele specific cloning
The APC 15-6 PCR product from lymphoblast DNA was cloned into pCR®2.1-Topo® vector and transformed into chemically competent E. coli strain TOP10 using the TOPO® TA Cloning Kit (Invitrogen Life Technologies, Carlsbad, California). PCR amplification of the cloned APC 15-6 amplicon was performed on isolated colonies and the products were digested with MboII restriction enzyme to distinguish the clones which contained the APC c.4729G>T mutation. The products were then sequenced to determine which rs41115 single nucleotide polymorphism (SNP) was in cis with the APC c.4729G>T mutation.
Results
To verify the clinical status of the family under investigation, colonoscopy and genetic data were collected on several family members. The phenotypic and genotypic information collected on the immediate family members is detailed in Fig. 1. The father (II-6) had two adenomatous polyps at age 66 and the mother (II-7) did not have any polyps at the age of 64. Individuals III-1, III-2, and III-4 reported no polyps. Individual III-3 was diagnosed with greater than 100 polyps at the age of 28, and subsequently underwent a colectomy at the age of 33. Individual III-5 was initially referred for evaluation based on her jaw osteomas at age 14; by age 25, she had greater than 100 cumulative polyps. No gastrointestinal polyps or cancers were reported in any of the extended family members. The mother (II-7) reported that her father and two brothers were diagnosed with prostate cancer at the ages of 79, 53, and 55 respectively. As prostate cancer is not typically associated with FAP, it is likely that this familial clustering of prostate cancer is independent of the APC mutation in this family.
Family Pedigree: Pedigree shows FAP clinical diagnosis, prostate cancers and lack of evidence for clinical suspicion of FAP in previous generations. Age at time of family evaluation, APC genetic test results, and APC locus haplotype data are included in the following order (top-to-bottom): D5S2501, D5S2027, D5S346, and D5S421
Genetic testing was conducted on each of the family members. A mutation, APC c.4729G>T (p.Glu1577X), was found in the proband (III-3) by sequencing of the APC gene from peripheral blood at Myriad Genetic Laboratories (Salt Lake City). Subsequently, full APC sequencing and MYH testing for the two common mutations was also performed on III-5. She also had a solitary APC c.4729G>T mutation identified; no mutations in MYH were detected. Clinical genetic testing for the familial mutation was performed on blood samples from one unaffected sibling, III-4, and both parents; no mutation was detected. Under a research protocol, mutation-specific testing was completed on blood from the parents, II-6 and II-7, the unaffected siblings, III-1, III-2 and III-4, and the affected siblings III-3 and III-5. In order to determine if the mutation is present in another tissue, mutation specific testing was repeated on buccal samples from each of the parents. Once again, the mutation was not identified. A summary of the genetic and clinical information is provided in Fig. 1.
Identity testing was used to confirm the genetic contributions of both the mother and father to each of their children. This was conducted by using 25 markers on 4 chromosomes. Based on known frequencies of these alleles in the general population, non-paternity can be ruled out with >99.999% certainty (Fig. 2). Since maternal and paternal inheritance was not an issue, the haplotype analysis of the APC locus was done to determine if the mutant allele originated from mother or father. Both affected children (III-3 and III-5) and an unaffected sibling (III-1) inherit the identical APC alleles from mother and father (Fig. 1). Thus, there was evidence of gonadal mosaicism since one unaffected sibling also inherited the same alleles, although the parental origin was ambiguous. To further address the question of parental origin, a SNP (rs41115,) was identified 250 base-pairs upstream of the mutation site, for which the father (II-6) was homozygous AA and the mother (II-7) was homozygous GG. Sequence analysis confirmed that each of the five children was heterozygous, AG. DNA cloning and sequencing of individual alleles demonstrated that the c.4729G>T mutation was co-inherited with the rs41115 G allele at position 4479 in every clone sequenced, indicating that the origin of the mosaicism was maternal (Fig. 3).
Sequence analysis of genomic DNA and PCR-amplified mutation-specific clones at rs41115 SNP variant position APC c.4479G>A. (a) Sequence from paternal and maternal genomic DNA alleles demonstrating AA and GG homozygosity respectively at rs41115 SNP position 4479 are shown along with the two heterozygous (GA) affected children. (b) Sequence from representative PCR-amplified clones containing the APC c.4729G>T mutation in cis with the maternal rs41115 G SNP at position c.4479 from both affected individuals III-3 and III-5
Discussion
We describe a family where an APC allele is transmitted to three offspring through an unaffected mother; two individuals inherit an APC mutation responsible for FAP whereas the third individual inherits a normal allele of APC. Although this case is not the first instance of gonadal mosaicism reported in a family with FAP [19], it reiterates the possibility that seemingly new mutations may be a result of a parent with gonadal mosaicism. This case has important implications for genetic counseling of families with apparently de novo cases of FAP. Parents who test negative for the mutation should be counseled about the small possibility of having another affected child due to gonadal mosaicism. Likewise, all siblings of the affected individual should be offered genetic testing for the mutation or undergo colonoscopic evaluation (if genetic testing is not pursued), even if neither of the parents is affected.
Recent studies have described the presence of somatic mosaicism in between 11 and 20% of apparently de novo mutations [20, 21]. In the cases described, the phenotype was consistently milder than expected due to the mosaicism, whereas affected offspring of these cases would be expected to have fully penetrant disease. We do not believe this phenomenon explains the current case as the sequence traces of the mother failed to reveal any appreciable sign of the mutation in the peripheral blood (mesoderm) or buccal cells (ectoderm) and she had no polyps upon colonoscopy at age 64 (endoderm). Therefore, neither the mutation nor the phenotype is present in tissues representing the three germinal layers of early fetal development. Most importantly, one child without the mutation inherits the identical allele as the two affected children, suggesting that this mutation arose in one of the estimated 6 primordial germ cell progenitors or their descendants.
In general, when a de novo mutation is detected in a proband and not in either parent or any siblings, which is estimated to account for up to 25% of cases, the clinical interpretation is that the mutation arose in the proband, or the egg or sperm that contributed to the proband [22]. However, our results and recent reports on the prevalence of somatic mosaicism show that it is important to rule out that the mutation may have arisen one generation earlier, as mosaicism in the germline of one of the parents. Interestingly, recent studies have suggested that APC point mutations such as the one described here, are more likely to arise on the paternal allele [23]; however, as the proband’s maternal grandparents are both deceased, it was not feasible to pursue this line of inquiry.
Abbreviations
- Familial adenomatous polyposis:
-
FAP
- Adenomatous polyposis coli:
-
APC
References
Petersen GM, Slack J, Nakamura Y (1991) Screening guidelines and premorbid diagnosis of familial adenomatous polyposis using linkage. Gastroenterology 100(6):1658–1664 Jun
Burt RW (2003) Gastric fundic gland polyps. Gastroenterology 125(5):1462–1469 Nov
Kadmon M, Tandara A, Herfarth C (2001) Duodenal adenomatosis in familial adenomatous polyposis coli. A review of the literature and results from the Heidelberg Polyposis Register. Int J Colorectal Dis 16(2):63–75 Apr
Cetta F, Curia MC, Montalto G et al (2001) Thyroid carcinoma usually occurs in patients with familial adenomatous polyposis in the absence of biallelic inactivation of the adenomatous polyposis coli gene. J Clin Endocrinol Metab 86(1):427–432 Jan
Cetta F, Montalto G, Gori M, Curia MC, Cama A, Olschwang S (2000) Germline mutations of the APC gene in patients with familial adenomatous polyposis-associated thyroid carcinoma: results from a European cooperative study. Journal of Clin Endocrinol Metabolism 85(1):286–292 Jan
Wallace MH, Phillips RK (1998) Upper gastrointestinal disease in patients with familial adenomatous polyposis. Br J Surg 85(6):742–750 Jun
Rustin RB, Jagelman DG, McGannon E, Fazio VW, Lavery IC, Weakley FL (1990) Spontaneous mutation in familial adenomatous polyposis. Dis Colon Rectum 33(1):52–55 Jan
Davidson S, Leshanski L, Rennert G, Eidelman S, Amikam D (2002) Maternal mosaicism for a second mutational event—a novel deletion—in a familial adenomatous polyposis family harboring a new germ-line mutation in the alternatively spliced-exon 9 region of APC. Hum Mutat 19(1):83–84 Jan
Niu DM, Huang JY, Li HY et al (2006) Paternal gonadal mosaicism of NIPBL mutation in a father of siblings with Cornelia de Lange syndrome. Prenat Diagn 26(11):1054–1057 Nov
Depienne C, Arzimanoglou A, Trouillard O et al (2006) Parental mosaicism can cause recurrent transmission of SCN1A mutations associated with severe myoclonic epilepsy of infancy. Hum Mutat 27(4):389 Apr
Gennaro E, Santorelli FM, Bertini E et al (2006) Somatic and germline mosaicisms in severe myoclonic epilepsy of infancy. Biochem Biophys Res Commun 341(2):489–493 Mar 10
Byers PH, Tsipouras P, Bonadio JF, Starman BJ, Schwartz RC (1988) Perinatal lethal osteogenesis imperfecta (OI type II): a biochemically heterogeneous disorder usually due to new mutations in the genes for type I collagen. Am J Hum Genet 42(2):237–248 Feb
Cohen-Solal L, Bonaventure J, Maroteaux P (1991) Dominant mutations in familial lethal and severe osteogenesis imperfecta. Hum Genet 87(3):297–301 Jul
Grange DK, Balfour IC, Chen SC, Wood EG (1998) Familial syndrome of progressive arterial occlusive disease consistent with fibromuscular dysplasia, hypertension, congenital cardiac defects, bone fragility, brachysyndactyly, and learning disabilities. Am J Med Genet 75(5):469–480 Feb 17
Lund AM, Nicholls AC, Schwartz M, Skovby F (1997) Parental mosaicism and autosomal dominant mutations causing structural abnormalities of collagen I are frequent in families with osteogenesis imperfecta type III/IV. Acta Paediatr 86(7):711–718 Jul
Raghunath M, Mackay K, Dalgleish R, Steinmann B (1995) Genetic counselling on brittle grounds: recurring osteogenesis imperfecta due to parental mosaicism for a dominant mutation. Eur J Pediatr 154(2):123–129 Feb
Somprasit C, Aguinaga M, Cisneros PL et al (2004) Paternal gonadal mosaicism detected in a couple with recurrent abortions undergoing PGD: FISH analysis of sperm nuclei proves valuable. Reprod Biomed Online 9(2):225–230 Aug
den Dunnen JT, Antonarakis SE (2000) Mutation nomenclature extensions and suggestions to describe complex mutations: a discussion. Hum Mutat 15(1):7–12
Farrington SM, Dunlop MG (1999) Mosaicism and sporadic familial adenomatous polyposis. Am J Hum Genet 64(2):653–658 Feb
Aretz S, Stienen D, Friedrichs N et al (2007) Somatic APC mosaicism: a frequent cause of familial adenomatous polyposis (FAP). Hum Mutat 28(10):985–992
Hes FJ, Nielsen M, Bik EC, et al (2007) Somatic APC Mosaicism: An Underestimated Cause Of Polyposis Coli. Gut (in press)
Bisgaard ML, Fenger K, Bulow S, Niebuhr E, Mohr J (1994) Familial adenomatous polyposis (FAP): frequency, penetrance, and mutation rate. Hum Mutat 3(2):121–125
Aretz S, Uhlhaas S, Caspari R et al (2004) Frequency and parental origin of de novo APC mutations in familial adenomatous polyposis. Eur J Hum Genet 12(1):52–58 Jan
Acknowledgements
We greatly appreciate the diagnostic skills and far-reaching intuition of Dr. Mark Peterson D.D.S, who first recognized osteomas and cysts in the family and referred them for further medical attention. We also acknowledge Jared Cox for family history data evaluation and pedigree construction. This research is supported by NCI grants P01-CA073992 (RWB) and R01-CA040641(RWB).
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Schwab, A.L., Tuohy, T.M.F., Condie, M. et al. Gonadal mosaicism and familial adenomatous polyposis. Familial Cancer 7, 173–177 (2008). https://doi.org/10.1007/s10689-007-9169-1
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s10689-007-9169-1