Abstract
In this paper, we analyzed the association among trends in COVID-19 cases, climate, air quality, and mobility changes during the first and second waves of the pandemic in five major metropolitan counties in the United States: Maricopa in Arizona, Cook in Illinois, Los Angeles in California, Suffolk in Massachusetts, and New York County in New York. These areas represent a range of climate conditions, geographies, economies, and state-mandated social distancing restrictions. In the first wave of the pandemic, cases were correlated with humidity in Maricopa, and temperature in Maricopa and Los Angeles. In Suffolk and New York, cases were correlated with mobility changes in recreation, grocery, parks, and transit stations. Neither cases nor death counts were strongly correlated with air quality. Periodic fluctuations in mobility were observed for residential areas during weekends, resulting in stronger correlation coefficients when only weekday datasets were included in the analysis. We also analyzed case-mobility correlations when mobility days were lagged, and found that the strongest correlation in the first wave occurred between 12 and 14 lag days (optimal at 13 days). There was stronger but greater variability in correlation coefficients across metropolitan areas in the first pandemic wave than in the second wave, notably in recreation areas and parks. In the second wave, there was less variability in correlations over lagged time and geographic locations. Overall, we did not find conclusive evidence to support associations between lower cases and climate in all areas. Furthermore, the differences in cases-mobility correlation trends during the two pandemic waves are indicative of the effects of travel restrictions in the early phase of the pandemic and gradual return to travel routines in the later phase. This study highlights the utility of mobility data in understanding the dynamics of disease transmission. It also emphasizes the criticality of timeline and local context in interpreting transmission trends. Mobility data can capture community response to local travel restrictions at different phases of their implementation and provide insights on how these responses evolve over time alongside disease trends.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
1 Introduction
The COVID-19 pandemic has caused tremendous health and socio-economic burdens since the disease was first reported in December 2019 and subsequently declared a global pandemic by the World Health Organization (Sohrabi et al. 2020). As of October 6, 2021, 237 million cases and 4.84 million deaths have been attributed to COVID-19 worldwide (Worldometer 2021). When the outbreak began, countries implemented different strategies to slow the spread of the disease. Historically, disease outbreaks are contained through a combination of pharmaceutical and non-pharmaceutical interventions (NPIs). Where vaccines are available, combining patient containment with population vaccination is highly effective for dense urban areas (Eubank et al. 2004). But for the novel SARS-CoV-2, the virus that causes COVID-19, vaccines were not initially available. Thus, initial mitigation efforts mostly focused on NPIs that are broadly categorized into containment, suppression, or mitigation. Containment is the measure associated with isolating individual infections and can only be implemented prior to community spread. Suppression encompasses measures that aim to reduce the effective reproduction number Rt at time t to values lower than 1 (e.g., school and business closures, lockdowns, and travel bans). Finally, mitigation is the set of measures most closely associated with the “flatten the curve” concept, which includes the 3Ws (wear your mask, watch your distance, and wash your hand). Generally speaking, suppression measures are stricter than mitigation but both aim to reduce infection rates and ease the burden on healthcare systems (Santos and Pagsuyoin 2021). Notably in the United States, when the federal government declared the COVID-19 pandemic a national emergency, states implemented control strategies to varying degrees of severity and included measures such as business closures, travel bans, stay-at-home orders, remote work, and mask mandates.
The impacts of austere measures such as lockdowns and travel bans during outbreaks are complex and have been the subject of much interest. By using scenario simulations, Poletto et al. (2014) concluded that travel restrictions in West Africa would delay the global spread of the 2013 Ebola outbreak by a few weeks but also compromise the delivery of needed health services and humanitarian aid to affected countries. In the early months of the 2003 severe acute respiratory syndrome (SARS) epidemic, travel to Asia Pacific countries dropped dramatically as a result of travel advisories and aggressive media attention (Abdullah et al. 2004). The disease would eventually lead to some 8000 cases and 700 deaths (WHO 2020) during its cycle, but the economic losses due to travel and tourism disruptions were disproportionately high (~ $30 billion; Peiris et al. 2008). Travel quarantine measures implemented in Wuhan have also been shown to delay the COVID-19 progression within China by only 3–5 days, though the effect on international transmission was more pronounced (Chinazzi et al. 2020). Collectively, these findings emphasize that the timing and scale of travel restrictions during disease outbreaks can alter the trajectory of disease transmission and also disrupt socio-economic activities.
The transmission dynamics of infectious diseases is driven by several factors including population density and mobility, hygiene practices, patient predispositions, nature of pathogens and vectors, and environmental and climatological conditions (Hales et al. 1999; Kroumpouzos 2020), among others. Densely populated urban areas are vulnerable disease hotspots due to greater population mobility and interactions with potentially infected individuals. Many infectious diseases such as the influenza exhibit seasonal patterns (Martinez 2018). For COVID-19, a pertinent question at the beginning of the pandemic was whether infections would decline in the summer season following laboratory evidence of lower SARS-CoV-2 viability at higher temperatures and humidity (Chan et al. 2011). Early reports have been mixed; higher cases have been associated with low humidity (Ward et al. 2020) and low temperature (Sajadi et al. 2020), while others found no evidence of relationships between cases and climatological conditions (Briz-Redón and Serrano-Aroca 2020; Juni et al. 2020). Hence, there is a need for further studies exploring how different factors influence the dynamics and seasonality of COVID-19 to improve surveillance and mitigation measures.
In this paper, we analyzed the association among trends in COVID-19 cases, climate, air quality, and mobility during the first and second waves of the pandemic in five major metropolitan counties in the United States: Maricopa in Arizona, Cook in Illinois, Los Angeles in California, Suffolk in Massachusetts, and New York County in New York. These areas represent a range of climate conditions, geographies, economies, and state-mandated social distancing restrictions. This study combined local epidemiological data with Google mobility data and climate and air data from different sources to examine the strength of associations among these variables across the five counties, and how these associations varied over the two pandemic waves.
2 Methodology
2.1 Case study areas
The five metropolitan areas (Fig. 1) were selected on the basis of their ranking in COVID-19 cases in the United States, and to encompass a range of geographic, economic, climatic, and non-pharmaceutical interventions implemented by the states during the pandemic period. Maricopa County in Arizona is the 4th most populous (CDC 2021) and has the 9th highest Gross Domestic Product (GDP) (BEA 2019) among U.S. counties. Its climate is semi-arid, with an average (24-h mean) temperature of 12 °C during winter and 32 °C in the summer (NOAA 2021) (climate baseline derived from years 1991–2020). Arizona mandated a state-wide school closures on March 15, 2020, followed by orders for closure of non-essential businesses, increased social distancing, and stay-at-home (OGSA 2021) Phased re-opening of businesses begun on May 12, 2020 (OGSA 2021). The state did not impose a mask order, though Maricopa County mandated the use of face coverings in public places beginning June 19, 2020 (Maricopa County 2020). Los Angeles County in California has the top population (US Census 2021) and GDP (BEA 2019) among all U.S. counties. Its climate is dry subtropical with an average temperature of 10 °C in the winter and 24 °C in the summer (NOAA 2021). On March 19, 2020, California issued statewide stay-at-home and social distancing orders, and on June 18, 2020 issued a statewide order requiring use of face masks in public places (OGCA 2021). Phased re-opening of businesses begun on June 12, 2020 (OGCA 2021). Cook County in Illinois is the 2nd most populous (US Census 2021) with the 4th highest GDP (BEA 2019) among U.S. counties. Its climate is humid continental, with an average temperature of − 3 °C in the winter and 22 °C in the summer (NOAA 2021). A statewide stay-at home order in Illinois took effect on March 21, 2020, with phased re-opening of businesses beginning on May 1, 2020 (IL 2021). A statewide mask order was put in place on May 1, 2020 (State of Illinois 2021). Suffolk County in Massachusetts has the 79th highest population (US Census 2021) and 19th highest GDP (BEA 2019) among U.S. counties. Its climate is humid continental, with an average temperature of − 1 °C in the winter and 21 °C in the summer (NOAA 2021). Suffolk was among the early COVID-19 hotspots of the first pandemic wave. Its first statewide stay-at-home and social distancing orders took effect on March 24, 2020 (MA 2021), with phased re-opening of businesses beginning on June 8, 2020. A second statewide and modified stay-at-home order was issued on November 6, 2020 (MA 2021) following a resurgence of COVID cases. Masks were required to be worn in public places in the state beginning May 6, 2020, (MA 2021). New York County in the state of New York is the 21st most populous (US Census 2021) and has the 2nd highest GDP (BEA 2019) among all U.S. counties. Its climate is humid subtropical, with an average temperature of 2 °C in the winter and 24 °C in the summer (NOAA 2021). On March 22, 2020, New York issued statewide stay-at-home and social distancing orders (NYDEP 2020); phased re-opening of businesses begun on June 22, 2020 (NYDEP 2020). New York had a statewide mask mandate that took effect on April 17, 2020 (NYDEP 2020).
United States map indicating COVID-19 rates and socio-economic profile of Metropolitan areas included in this study. Population and demographic data (2020) from (US Census 2021); GDP data (2019) from (BEA 2019); COVID case counts and death data from (JHU 2021); COVID-19 community vulnerability indices (CCVI) from (CDC 2021b) and indicate neighborhood-level vulnerability based on aggregated indicators spanning health, economic, and social metrics (Surgo Ventures 2021)
2.2 Data sources and statistical analyses
This study utilized datasets that were obtained from various sources and covering the period starting from February 15, 2020 to December 15, 2020. An extended analysis of the COVID case waves was carried with mobility and epidemiological data covering the period until April 15, 2021 (to include the second wave of COVID cases). Daily COVID case and death counts were obtained from the U.S. Center for Disease Control (CDC 2021b; JHU 2021) and were converted to 7-day moving averages. Daily climate data were obtained from the Parameter-elevation Regressions on Independent Slopes Model (PRISM) and the Gridded Surface Meteorological Dataset (gridMET) (Daly et al. 2008; Abatzoglou 2013). PRISM is a gridded dataset created with observational in situ point measurements and a weighted regression scheme to account for variations in elevation, topographic facet orientation, rain shadows, and coastal proximity, among other influential physiographic features. The gridMET data combine PRISM data with regional reanalysis data from the National Land Data Assimilation System version 2 (NLDAS-2) (Xia et al. 2012), providing a broader set of gridded climate variables (in our analysis, specific humidity and wind speed are selected from gridMET). The PRISM and gridMET datasets are archived at a 4 km resolution and then spatially averaged at the county level using the cloud computing Climate Engine tool (Huntington et al. 2017). Air quality index (AQI) data were obtained from (USEPA 2021); AQI indicates overall air quality and is based on pollutant measurements in a local area for six parameters (where sensors are available): CO, NO2, O3, SO2, PM2.5, and PM10. Daily index values are calculated for each pollutant; the daily AQI is the highest pollutant index value for that day. Mobility data were obtained from Google’s Community Mobility Report (2021) and are represented as percentage change in community mobility relative to a pre-pandemic baseline (average visitor counts within the 5-week period from January 3-February 6, 2020) for 6 categorical locations: recreation and retail, parks and outdoor spaces, groceries and pharmacies, transit stations, workplaces, and residential. Pearson correlation analyses of datasets for the two pandemic waves (Table 1) were carried out in MatLab (ver. 9.9 R2020b).
3 Results
3.1 Temporal trends in epidemiological, climate, air quality, and mobility datasets
Figure 2 shows the plots of the epi curves (normalized case and death counts), climatic data, air quality, and mobility data for the five metropolitan areas (2/15/20–12/15/20). Within the study period, all areas experienced 2 waves of COVID infections to varying degrees and periods of occurrence. In temperate counties (Cook, Suffolk, and New York), the first wave occurred from April to June 2020, followed by a period of relatively low cases, and then a second wave that began around October 2020 that was still ongoing by December 2020. Among the three temperate counties, case numbers during the first wave were lowest in Cook County, but were highest during the plateau period and the second wave. Death cases in New York and Suffolk tracked the first wave of infections and were highest among the five metropolitan areas, but no such uptick in deaths was observed during the second wave of infections. In warmer Maricopa County, the first wave began relatively later but was almost immediately followed by the onset of the second wave. In Los Angeles County, the first wave period was prolonged but saw fewer cases; however, this period was followed almost immediately by a significant uptick in cases during the second wave. Nonetheless, death counts in the county were comparatively lower than in other counties throughout the two waves of infections.
Temporal epidemiological (population-normalized COVID case and death counts and 7-day moving averages), climate and air quality, and mobility data for the five metropolitan areas in this study. 7-day averages calculated using COVID case counts and death data from (Huntington et al. 2017); climate data from extracted using PRISM interpolation as described in Daly et al. (2008) and Abatzoglou (2013), daily air quality indices obtained from (AQI) from (USEPA 2021), and mobility data from (Google 2021). Figure also indicates spikes in mobility trends during federal holidays that occurred within the covered study period: Memorial Day (MD; 5/25/2020), Independence Day (ID; 7/3/2020), Labor Day (LD; 9/7/2020), and Thanksgiving Weekend (TW;11/26–27/2020)
As indicated by the temporal AQI values, overall air quality in Suffolk and New York was the best among the five metropolitan areas, and poorest in Los Angeles. We note that daily AQI values are determined by the poorest air quality parameter index calculated for that day, and therefore may not track the same air quality parameter throughout the year. Except for Massachusetts where AQI values remained relatively stable throughout the study period, AQI values in the metropolitan areas were highest during late Spring to Fall. In the case of Los Angeles, the AQI values were mostly due to ozone (68% of the time) and PM2.5 (29% of the time).
With respect to mobility patterns, similar and distinct trends were observed in different location categories among the five metropolitan areas. Increased weekday mobility in residences was observed among all metropolitan areas beginning March 2020, coinciding with statewide mandates for social distancing, and indicative of the onset of increased workforce teleworking from home. Weekend residential mobility data in all metropolitan areas differ from the weekday data; initially, there was increased presence in residences up until late Spring 2020, followed by a return to near baseline levels for the remainder of the year. Conversely, as weekday mobility in residences increased, weekday mobility in workplaces and transit stations decreased significantly, and by the end of 2020 had not yet returned to pre-pandemic levels. The greatest decline in weekday workplace mobility (> 50% reduction) was observed in Suffolk and New York. Across the board, mobility in groceries and pharmacies decreased initially in March 2020; but with the exception of New York, mobility in these locations increased to near pre-pandemic levels by summertime (May 2020), most notably in Los Angeles and Cook counties. Mobility in parks and outdoor spaces is distinctly different among counties. In warmer Maricopa and Los Angeles, mobility in parks declined significantly in the initial phase of the pandemic, returned to near baseline in the summer months, and reduced once more thereafter. In Cook and Suffolk counties, mobility in parks rose substantially (~ 100–150% of baseline) over summer and into early fall 2020. Large day-to-day variability in summer park mobility in Cook and Suffolk counties compared with Maricopa and Los Angeles counties likely, in part, reflects greater variability in weather conditions common to the colder northern counties. Warmer summer temperatures are an incentive for increased outdoor activities at parks and trails among locals after the long and cold winter months, especially in the absence of canceled traditional local summer events (e.g., cultural festivals). Anecdotal stories from hikers at our local trails echo similar plans for increased visits to parks as a safer alternative for social interactions given strict advisories on social distancing. Of note is that although mobility in parks and outdoor spaces in New York County has increased on weekends since late spring 2020, it has not yet returned to pre-pandemic levels nor did it increase significantly during the summer or fall season. It is noted that 10-hectare Central Park, which is a famous landmark to both locals and visitors, is located in New York County. When stay-at-home orders were declared in NY state, all parks were inaccessible to the public but have since been reopened since June 2020 (JHUCRC 2021). Lastly, several weekends coinciding with federal holidays occurred during the pandemic period, including Memorial Day (5/25/2020), Independence Day (7/3/2020), Labor Day (9/7/2020), and Thanksgiving (11/26–27/2020). These events marked notable decreases in workplace and transit mobility alongside increases in residential and grocery mobility.
3.2 Distinctions between weekly and weekday trends
Given the observed differences in mobility patterns between weekdays and weekends, separate analyses were carried out to contrast correlation outcomes when using datasets for all days of the week (week-long) and weekdays only (Monday–Friday). Figure 3 shows the corresponding correlation heatmaps for the five metropolitan areas covering the first wave of the pandemic. For the week-long dataset, COVID case and death counts in Maricopa were correlated with temperature (R = 0.60 and 0.75, respectively) and death count was also correlated with humidity (R = 0.69), all at α = 0.01 level. No similar strong correlations (i.e., R < 0.5) were found for cases or death counts with mobility change in any location category. In Los Angeles, case and death counts were correlated with temperature (R = 0.63 and 0.58, respectively, α = 0.01); in addition, case count was correlated with park mobility change (R = 0.66). In Cook, no strong correlations were found for either COVID case or death counts with climate, air quality, and mobility changes. For the colder counties of Suffolk and New York, similar correlation trends were noted. Specifically, case counts were strongly negatively correlated with mobility changes in recreation, grocery, parks, and transit stations (− 0.75 < R < − 0.57; α = 0.01) and only moderately positively correlated with residential mobility change (0.44 < R < 0.47; α = 0.01). We note that the duration of the first COVID case wave is shorter in these counties, and that the gap between the two case waves (i.e., period of lower new infections) was wider compared to the other counties. Generally, the strong correlations found in the week-long datasets were even stronger in the weekday datasets (Fig. 3, bottom heatmaps). Most notably, in Suffolk and New York, the COVID case counts were strongly positively correlated with residential mobility change (0.72 < R < 0.82; α = 0.01) when using only the weekday data.
3.3 Distinctions between metropolitan and rural areas in Massachusetts
We also conducted a subset analysis in Massachusetts to contrast week-long trends between metropolitan and rural areas (i.e., in the context of population density) in the same climate zone. Representative urban counties were Middlesex and Suffolk, both located in the Greater Boston Region. Representative rural counties were Barnstable in Southeastern Massachusetts and Franklin in Western Massachusetts. Their socio-economic profiles are summarized in Fig. 4, and the corresponding correlation heatmaps are shown in Fig. 5. Barnstable and Franklin have comparable population density and total case counts per capita (as of 6/16/2021). Middlesex and Suffolk, respectively, have a population density 20 and 135 times higher than Franklin’s. Both urban counties were among the national COVID-19 hotspots in the early stages of the pandemic (JHU 2021).
Map of the Commonwealth of Massachusetts indicating COVID-19 rates (as of 6/16/2021) and socio-economic profile of the four rural and metropolitan areas included in this study. Population and demographic data (2020) from (Census 2021); GDP data (2019) from (BEA 2019); COVID case counts and death data from (JHU 2021)
Case and death counts were weakly correlated in Barnstable (R = 0.20, α = 0.05) but strongly correlated in the other counties (R > 0.7, α = 0.01). A similar geographic trend was also noted between case counts and mobility change in recreation areas. Case counts were strongly correlated with mobility change in transit areas only in Suffolk (R = − 0.67, α = 0.01) but strongly correlated with mobility change in groceries in all counties. Except for residential areas, mobility changes in categorical locations in Barnstable were positively correlated with each other and follow more closely those of Suffolk. In Franklin, mobility changes were only positively correlated between recreation and grocery, and between transit and workplace. It is worth noting that compared to Barnstable, Franklin is located farther from the state capital and has lower access to public transit. Barnstable has access to more frequent public transit into Boston; however, it also has a relatively higher percentage of older age population (31% > 65 y.o.; US Census 2021).
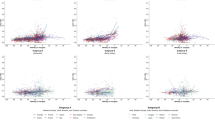
3.4 COVID cases and lagged mobility during pandemic waves
The incubation period for SARS-CoV-2 is estimated to be between 2 and 14 days (Lauer et al. 2020; McAloon et al. 2020; Qin et al. 2020), with a median of 5 days (McAloon et al. 2020). Infected patients may present symptoms 1–14 days after exposure (CDC 2021), thus it may be possible for reported infections to lag behind changes in population mobility. In this study we performed an analysis of variations in coefficients with lagged days to examine how temporal mobility changes (i.e., lagged mobility data) relate to infection cases in the two pandemic waves. Among location categories, there was stronger but greater variability in correlation coefficients across metropolitan areas in the first pandemic wave than in the second wave (indicated by height of vertical bars in Fig. 6), most notably in recreation and parks. Except for grocery, the strongest correlation in the first wave occurred between 12 and 14 days (optimal at 13 days). This period is slightly higher than the optimal lag days reported by Badr et al. (2020) (11 days) for U.S. counties, though their methodology (mobility data and correlation analyses) differed from the one we implemented in this study. In the second wave, there was less variability in correlations over lagged time and geographic locations, as indicated by the vertical bars with near constant height along the x-axis (lagged days).
Correlation values, R, (between 7-day averaged case counts vs mobility changes) as a function of lagged days for the first (top) and second (bottom) waves of the COVID-19 pandemic. Green line represents average R values across 5 metropolitan counties; bars represent range of values among counties. Shaded blue region represents range for strongest R (highest absolute) values. Data inputs included week-long datasets
4 Discussion
Our results indicate site-specific differences in the associations of cases (infections) with temperature and humidity. Though both Maricopa and Los Angeles have lower humidity year-round compared to the other counties, cases were only strongly correlated with humidity in Maricopa. Among all counties, cases were strongly associated with temperature only in Maricopa and Los Angeles, and that these are positive association despite their temperatures being generally higher than the other counties. Strong correlations between cases and windspeed and precipitation were not found. Neither cases nor death counts were strongly correlated with air quality. Overall, we found no conclusive evidence that suggests higher temperatures and humidity were associated with lower cases. This observation is consistent with findings reported for several cities in China (Yao et al. 2020) and globally (Juni et al. 2020). Other studies found contrasting results, for example, Sajadi et al. (2020) concluded that initial outbreaks worldwide occurred in communities with lower temperature and humidity, while Ward et al. (2020) found strong negative correlations between cases and lower humidity in Australia. While we reference these earlier studies to compare findings, we also acknowledge differences in our statistical and modeling methodologies. Recent literature reviews highlight these inconsistencies in modeling methodologies (Briz-Redón and Serrano-Aroca 2020) and findings (Zaitchik et al. 2020), but also emphasized that the impact of high temperature on diseases transmission is insufficient as a control measure (Briz-Redón and Serrano-Aroca 2020). Kubota et al. (2020) further notes that climate, mobility, and region-specific susceptibility drive the case numbers in studied sites, and that case dependencies on these parameters changed over time with pandemic progression.
Our study noted distinct and periodic differences in weekend and weekday mobility trends in residences and workplaces in all metropolitan areas. Throughout the study period, mobility in transit stations was still below baseline levels, but there was a pronounced difference between weekday and weekend trends in Cook County, and to a lesser extent in Suffolk and New York beginning around July 2020. Note that these three counties are among the top 5 metropolitan areas with the highest public transport ridership in the U.S. (Burrows et al. 2021), indicating heavy reliance on public transport to commute to work and for other travels. Public transport functions as congregation nodes where social distancing may be challenging to enforce. Evidently, shifting to remote work affects population densities and mobility patterns in cities, and these can have implications on social distancing policies. Remote work and hard lockdowns can drastically alter movement patterns in metropolitan areas as was observed in this study and in Spain (Perez-Arnal et al. 2021) and Japan (Arimura et al. 2020), where weekends and holidays saw markedly lower densities in business districts as people tended to stay-at-home. Adherence to stringent movement restrictions may be high at the beginning of lockdowns but over time people will naturally seek to return to normal travel routines. Furthermore, we noted in this study the stronger correlation between cases and mobility during the first pandemic wave than in the second wave. There was also a high variability in correlations among counties during the first pandemic wave but significantly less in the second wave. These could be indicative of, among other things: (1) a new mobility normal that is below pre-pandemic baseline but is nonetheless plateau and is less useful in analyzing disease transmission, and (2) the higher prevalence of COVID-19 everywhere regardless of local geographies.
Mobility has often been used as a surrogate for social distancing but there is a need to contextualize its use within local conditions to better interpret the effect of NPIs on disease transmission. For example, the trends in normalized case epi curves during the first pandemic wave (Fig. 2) are similar for Maricopa, Suffolk, and New York. When viewed from the lens of mobility values alone, Maricopa has the least deviation from baseline mobility patterns, while Suffolk and New York have the highest change in mobility. One may misinterpret this as low social distancing effort in Maricopa compared to other counties. However, population-wise, Maricopa has 28 times lesser density than Suffolk, and 147 times lesser density than New York (based on pre-pandemic population, see Methods section and data in Fig. 1). Thus, when the context of population density is factored in, Maricopa is already relatively more socially distant to begin with. Conversely, the large reductions in mobility in densely populated Suffolk and New York imply that people in these counties drastically reduced travel during the first wave of the pandemic and following statewide stay-at-home orders. This behavior may have contributed to the rapid decline of the first wave, and the delayed onset, and lower peaks of the second wave surge. We also note that while the Google mobility data we used in this study are extensive and have high granularity, they should be interpreted within context, namely, that the data represent percentage change from the baseline period (1/3/20–2/6/20) rather than the actual number of people in the categorical locations. Simple correlations of mobility with cases may be a good initial step to screen for effectiveness of mitigation measures, though more comprehensive analysis of compounding factors is needed.
4.1 Study limitations and areas for future work
The case studies presented in this paper have several limitations that may be explored further in future research. Firstly, the five counties included in this paper are only a subset of over three thousand counties in the United States, each with distinct economic, geographic, and demographic profiles. The five counties were selected to investigate regions with differing characteristics such as weather patterns, mobility, as well as GDP and population attributes. The selection also considered representative areas from the various census regions in the U.S., namely West (Maricopa, AZ and Los Angeles, CA), Midwest (Cook, IL), and Northeast (New York, NY and Suffolk, MA). Although the current study provided insights on the potential impacts of variables like weather and mobility patterns on infection and death counts, the approach utilized in this paper can be extended in the analysis of other U.S. counties as well as other factors (e.g., race, age, gender, and political leaning, among others), which were not directly investigated in the current study.
Secondly, the correlation analysis in this paper utilized Google Mobility Index data to assess the extent to which people’s activities in various location categories have changed relative to pre-pandemic levels. The Google mobility data are publicly available at no cost and are collected via mobile phones. However, Google could only collect mobility data from devices where the “Location History” feature is enabled in any Google app (i.e., it is currently turned off by default) (Google 2021). Future analysis may use alternative measures of mobility from other public (e.g., Facebook (2021) and proprietary databases (e.g., as in (Badr et al. 2020).
Thirdly, the analytical methods employed in this study differ from other studies and may have contributed to differences in results. Previous papers found positive correlations between mobility and number of cases (see, for examples, (Badr et al. 2020), Wang et al. 2020), and concluded that reduced mobility outside of residential locations appears to be positively correlated with the decline in cases. In contrast, this paper did not definitively confirm that decreased mobility levels would lead to the reduction in case and death counts. Furthermore, several correlation values in this paper appear counterintuitive; for example, reduced mobility in locations such as recreation, grocery, parks, and transit stations has been associated with an increased number of cases and deaths, even when time lags are imposed. One possible explanation to this is that the viral transmission rates especially near the peak of the epi curves are aberrantly high that reduced mobility levels would not necessarily lead to an immediate flattening of the curve. Hence, a future analysis can be conducted to measure the true efficacy of reduced mobility by comparing the difference of actual recorded case counts against model projections that assume absence of stay-at-home mandates.
Finally, this study did not directly examine the effect of vaccination on the decline of cases particularly near the tail end of the second wave scenarios. The first vaccine dose was given on December 14, 2020 (BBC 2021) to a limited population sector, and a discussion of the subsequent vaccine rollout is documented in the American Journal of Managed Care (AJMC 2021). A future study could perform a multiple regression analysis to determine the combined effects of mobility, vaccination rates, and seasonal factors on the number of cases and deaths.
References
Abatzoglou JT (2013) Development of gridded surface meteorological data for ecological applications and modelling. Int J Climatol 33:121–131
Abdullah AS, Thomas GN, McGhee SM, Morisky DE (2004) Impact of severe acute respiratory syndrome (SARS) on travel and population mobility: implications for travel medicine practitioners. J Travel Med 11(2):107
American Journal of Managed Care (2021) A timeline of COVID-19 vaccine developments in 2021. https://www.ajmc.com/view/a-timeline-of-covid-19-vaccine-developments-in-2021. Accessed 18 June 2021.
Arimura M, Ha TV, Okumura K, Asada T (2020) Changes in urban mobility in Sapporo city, Japan due to the Covid-19 emergency declarations. Transp Res Interdiscip Perspect 7:100212
Badr HS, Du H, Marshall M, Dong E, Squire MM, Gardner LM (2020) Association between mobility patterns and COVID-19 transmission in the USA: a mathematical modelling study. Lancet Infect Dis 20(11):1247–1254
British Broadcasting Corporation (2021) First vaccine given in US as roll-out begins. https://www.bbc.com/news/world-us-canada-55305720. Accessed 18 June 2021.
Briz-Redón Á, Serrano-Aroca Á (2020) A spatio-temporal analysis for exploring the effect of temperature on COVID-19 early evolution in Spain. Sci Tot Environ 728:138811
Burrows M, Burd C, McKenzie B (2021) Commuting by Public Transportation in the United States: 2019. American Community Survey Reports, ACS-48. US Census Bureau. https://www.census.gov/content/dam/Census/library/publications/2021/acs/acs-48.pdf. Accessed 14 May 2021.
Chan KH, Peiris JS, Lam SY, Poon LL, Yuen KY, Seto WH (2011) The effects of temperature and relative humidity on the viability of the SARS coronavirus. Adv Virol 734690.
Chinazzi M et al (2020) The effect of travel restrictions on the spread of the 2019 novel coronavirus (COVID-19) outbreak. Science 368(6489):395–400
Commonwealth of Massachusetts (2021) Massachusetts Executive Orders. https://www.mass.gov/massachusetts-executive-orders. Accessed 24 May 2021.
Daly C et al (2008) Physiographically sensitive mapping of climatological temperature and precipitation across the conterminous United States. Int J Climatol 28:2031–2064
Eubank S, Guclu H, Kumar VA, Marathe MV, Srinivasan A, Toroczkai Z, Wang N (2004) Modelling disease outbreaks in realistic urban social networks. Nature 429(6988):180–184
Facebook Inc. (2021) Data for good: Movement range maps. https://dataforgood.fb.com/tools/movement-range-maps/ Accessed 19 June 2021.
Google (2021) Community mobility report. https://www.google.com/covid19/mobility/. Accessed 16 April 2021
Hales S, Weinstein P, Souares Y, Woodward A (1999) El Niño and the dynamics of vectorborne disease transmission. Environ Health Perspect 107(2):99–102
Huntington JL et al (2017) Climate engine: cloud computing and visualization of climate and remote sensing data for advanced natural resource monitoring and process understanding. Bull Am Meteorol Soc 98:2397–2410
Johns Hopkins University Coronavirus Resource Center (2021) United States Coronavirus Cases by County. https://coronavirus.jhu.edu/us-map. Accessed 15 May 2021.
Jüni P et al (2020) Impact of climate and public health interventions on the COVID-19 pandemic: a prospective cohort study. Can Med Assoc J 192(21):E566–E573
Kroumpouzos G, Gupta M, Jafferany M, Lotti T, Sadoughifar R, Sitkowska Z, Goldust M (2020) COVID‐19: a relationship to climate and environmental conditions?. Dermatol Ther e13399.
Kubota Y, Shiono T, Kusumoto B, Fujinuma J (2020) Multiple drivers of the COVID-19 spread: the roles of climate, international mobility, and region-specific conditions. PLoS ONE 15(9):e0239385
Lauer SA et al (2020) The incubation period of coronavirus disease 2019 (COVID-19) from publicly reported confirmed cases: estimation and application. Ann Intern Med 172(9):577–582
Maricopa County (2020) Amended Regulations Requiring Face Coverings in Maricopa County. https://www.maricopa.gov/DocumentCenter/View/61311/Regulations-on-Face-Coverings. Accessed 5 January 2021.
Martinez ME (2018) The calendar of epidemics: seasonal cycles of infectious diseases. PLoS Pathog 14(11):e1007327
McAloon C et al (2020) Incubation period of COVID-19: a rapid systematic review and meta-analysis of observational research. BMJ Open 10(8):e039652
National Oceanic and Atmospheric Administration Centers for Environmental Information (2021) Climate at a Glance: County Time Series, published June 2021. https://www.ncdc.noaa.gov/cag/ Accessed 17 June 2021
New York State Department of Environmental Conservation (2020) Press Releases. https://www.dec.ny.gov/press/120625.html. Accessed 11 March 2021.
Office of Governor (2021) Executive Orders. https://www.gov.ca.gov/category/executive-orders/. Accessed 24 May 2021.
Office of the Governor State of Arizona (2021) Executive Orders. https://azgovernor.gov/executive-orders. Accessed 24 May 2021.
Peiris M, Anderson LJ, Osterhaus ADME (eds) (2008) Severe Acute Respiratory Syndrome: A Clinical Guide (1). Chichester, Wiley-Blackwell, p 285
Pérez-Arnal R, Conesa D, Alvarez-Napagao S, Suzumura T, Català M, Alvarez-Lacalle E, Garcia-Gasulla D (2021) Comparative analysis of geolocation information through mobile-devices under different Covid-19 mobility restriction patterns in Spain. ISPRS Int J Geo-Inf 10(2):73
Poletto C, Gomes MF, Piontti AP, Rossi L, Bioglio DL, Chao DL, Longini Jr IM, Halloran ME, Colizza V, Vespignani A (2014) Assessing the impact of travel restrictions on international spread of the 2014 West African Ebola epidemic. Eurosurveillance 19(42):20936
Qin J, You C, Lin Q, Hu T, Yu S, Zhou XH (2020) Estimation of incubation period distribution of COVID-19 using disease onset forward time: a novel cross-sectional and forward follow-up study. Sci Adv 6(33):1202
Sajadi MM, Habibzadeh P, Vintzileos A, Shokouhi S, Miralles-Wilhelm F, Amoroso A (2020) Temperature, humidity, and latitude analysis to estimate potential spread and seasonality of coronavirus disease 2019 (COVID-19). JAMA Netw Open 3(6):e2011834
Santos J, Pagsuyoin SA (2021) The impact of “Flatten the Curve” on interdependent economic sectors. In: Linkov I, Keenan JM, Trump BD (eds) COVID-19: Systemic Risk and Resilience. Risk, Systems and Decisions. Springer, Cham.
Sohrabi C, Alsafi Z, O’Neill N, Khan M, Kerwan A, Al-Jabir A, Iosifidis C, Agha R (2020) World Health Organization declares global emergency: a review of the 2019 novel coronavirus (COVID-19). Int J Surg 76:71–76
State of Illinois (2021) Executive orders. https://www2.illinois.gov/government/executive-orders. Accessed 24 May 2021
Surgo Ventures (2021) The US COVID Community Vulnerability Index. https://precisionforcovid.org/ccvi. Accessed 11 March 2021
United States Bureau of Economic Analysis (2019) Gross Domestic Product. https://www.bea.gov/data/gdp. Accessed 4 January 2021.
United States Census Bureau (2021) Quick Facts. https://www.census.gov/quickfacts/. Accessed 12 March 2022
United States Center for Disease Control (2021a) Notification of Exposure: A Contact Tracer’s Guide for COVID-19. https://www.cdc.gov/coronavirus/2019-ncov/php/notification-of-exposure.html. Accessed 21 May 2021a
United States Center for Disease Control (2021b) COVID Data Tracker. https://covid.cdc.gov/covid-data-tracker/#county-view. Accessed 15 April 2021b.
United States Environmental Protection Agency (2021) Air Quality Index Report. https://www.epa.gov/outdoor-air-quality-data/air-quality-index-report. Accessed 20 December 2020
Wang X et al (2020) Quantifying the time-lag effects of human mobility on the COVID-19 transmission: a multi-city study in China. IEEE Access 8:216752–216761
Ward MP, Xiao S, Zhang Z (2020) The role of climate during the COVID-19 epidemic in New South Wales, Australia. Transboundary Emerging Dis 67(6):2313–2317
World Health Organization (2020) Statement on the meeting of the International Health Regulations (2005) Emergency Committee regarding the outbreak of novel coronavirus (2019-nCoV). https://www.who.int/news-room/detail/23-01-2020-statement-on-the-meeting-of-the-international-health-regulations-(2005)-emergency-committee-regarding-the-outbreak-of-novel-coronavirus-(2019-nCoV). Accessed 8 August 2021
Worldometer (2021) COVID-19 Coronavirus Pandemic. https://www.worldometers.info/coronavirus/. Accessed 6 Oct 2021
Xia Y, et al. (2012) Continental-scale water and energy flux analysis and validation for the North American Land Data Assimilation System project phase 2 (NLDAS-2): 1. Intercomparison and application of model products. J Geophys Res: Atmos 117
Yao Y, et al. (2020) No association of COVID-19 transmission with temperature or UV radiation in Chinese cities. Eur Resp J 55(5)
Zaitchik BF et al (2020) A framework for research linking weather, climate and COVID-19. Nature Comm 11(1):1–3
Acknowledgements
This work was partially funded by the National Science Foundation (Grant Nos. 1832635 and (1944157). The views expressed in this paper are those of the authors and do not represent the NSF.
Author information
Authors and Affiliations
Contributions
SP conceptualized the study design, helped in data collection, analysis and interpretation, and in manuscript writing. GS performed data collection, analysis and interpretation, and literature review. JS helped with data interpretation and manuscript writing. CS helped with data collection and manuscript writing.
Corresponding author
Ethics declarations
Conflict of interest
The Authors declare no conflict of interest.
Rights and permissions
About this article
Cite this article
Pagsuyoin, S.A., Salcedo, G., Santos, J.R. et al. Pandemic wave trends in COVID-19 cases, mobility reduction, and climate parameters in major metropolitan areas in the United States. Environ Syst Decis 42, 350–361 (2022). https://doi.org/10.1007/s10669-022-09865-z
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s10669-022-09865-z