Abstract
The nativity composition of the Taiwan population has changed substantially since 1980, which resulted in one in six children being born to foreign-born mothers in 2004. The purpose of this study was to compare the early neonatal mortality rates among babies of foreign-born and Taiwan-born mothers. Data was obtained from the Taiwan Birth Registry Database in 2004 by the Bureau of Health Promotion, Department of Health, Taiwan. Multivariate analysis was used to examine the influence of the different maternal nationalities on early neonatal mortality after adjusting for important maternal and infant variables. Infants born to foreign-born mothers had a lower early neonatal mortality rate (5.6‰) compared to those born to Taiwan-born mothers (9.4‰). Even after adjusting for important maternal and infant variables, newborns of foreign-born mothers still had a lower risk of early neonatal death compared to newborns of Taiwan-born mothers (odds ratio = 0.68, 95% CI = 0.57–0.80). Foreign-born status may serve as an important index of differentiation in early neonatal mortality among the current Taiwan population. Selection, economic and non-economic aspects may explain the paradox of favorable early neonatal mortality outcomes.
Similar content being viewed by others
Explore related subjects
Discover the latest articles, news and stories from top researchers in related subjects.Avoid common mistakes on your manuscript.
Introduction
Neonatal and infant mortality are important indices of a community’s health and social well-being [1]. It is well-understood that a quarter of pediatric deaths occur during the first week after birth [2]. When making international comparisons in maternal and child health, immigrant groups contribute far more complicated effects on neonatal mortality, even after adjusting for maternal health, labor and delivery complications [3].
Much attention has focused on the health of immigrants’ newborns. Surprisingly, newborns of foreign-born mothers seem to display a significantly lower neonatal mortality and infant mortality than their origin-born counterparts in the US and England, even after a number of sociodemographic risk factors have been controlled [1, 4–7]. Such paradoxically favorable outcomes in newborns of immigrants denote a residual protective effect of foreign-born status that cannot be accounted for demographic, socioeconomic, behavioral or medical risk factors [8].
The nativity composition of the Taiwan population has changed substantially since 1980, which resulted in one in six children being born to foreign-born mothers in 2004 [9]. The nature of transnational marriage in Taiwan is different from that of immigrants who seek jobs in developed countries. Many Taiwanese husbands who are married to foreign women are either physically or mentally handicapped, or live in rural areas or near the border of metropolitan areas. Foreign women who are married to a Taiwanese man and reside in Taiwan generally come from lower-class families in developing or underdeveloped countries. These transnational foreign brides are mostly chosen by marriage brokers and their marriages are usually defined as traded marriages [10]. To obtain a residential visa to Taiwan, these foreign brides must pass a physical exam and their health status is just as good as that of Taiwanese women.
In 2004, information of maternal nationality was required in the birth record in hopes that the birth registry could provide raw material to uncover the extent and sources of variation of maternal nationality and to explore their influence on birth outcome. The purpose of this study was to compare early neonatal mortality among newborns of foreign-born and Taiwan-born mothers univariately and multivariately using the 2004 Taiwan Birth Registry.
Methods
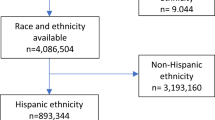
The data for our study was obtained from the Taiwan Birth Registry, Bureau of Health Promotion, Department of Health in Taiwan. Live singletons born in 2004 were included in this study. Live birth is defined as an infant with a gestational age exceeding 20 weeks and vital signs such as respiration, heartbeat, pulsation of umbilical cord and muscular movements right after birth. Neonatal deaths are usually categorized into early neonatal deaths that occur during the first seven days of life (0–6 days) and late neonatal deaths that occur between the seventh and 28th days of life (7–27 days) [3]. In this study, neonatal mortality was defined as the death of a newborn during the first 10 days of life because births are registered in the first ten days of life in Taiwan. In this study, women from Southeast Asia or mainland China were considered foreign-born mothers. Foreign-born mothers from developed countries such as Japan, Korea, South Africa, England, America, etc. (0.21%) were not included in this study.
Variables in the Taiwan Birth Registry include: (1) newborn: gender, gestational age, birth weight, time and date of birth, number of parturition, location of the delivery center, status of birth (alive or dead) and other health problems; (2) mother: date of birth, nationality, address, risk factors of the pregnancy and interventions during pregnancy; (3) delivery: deliverer of the baby (physician or midwife), delivery method and labor complications. Risk factors of the pregnancy include the following: anemia (hematocrit < 30 or hemoglobin < 10), cardiac disease, pulmonary disease, diabetes mellitus, syphilis, gestational diabetes, hydramnion (AFI≧24 cm or DP≧8 cm) or oligohydramnion (AFI≦5 cm or DP≦1 cm), hemoglobinopathy, chronic hypertension, gestational hypertension, toxemia of pregnancy, cervical incompetence, previous delivery of an overweight infant (birth weight ≧4000 g), previous delivery of a preterm (gestational age < 37 weeks) or low birth weight baby (birth weight < 2500 g), nephropathy or Rh factors anaphylaxis. Interventions during pregnancy and labor include amniocentesis, chorionic villus sampling, induction and stimulation of labor, tocolysis, cervix cerclage procedure, exploratory laparotomy (hysteromyomectomy or ovarian cyst removal) and others. Complications of labor include fever of the mother (temperature > 38°C), meconium-stained amniotic fluid (moderate/severe), rupture of water bag (>12 h), premature detachment of placenta, placenta praevia, other hemorrhage (vaginal delivery >500 ml, cesarean section >1000 ml), convulsion of labor, precipitated labor (<3 h), prolonged labor (regular uterine contractions >20 h), difficult labor progress, breech presentation/malpresentation, cephalopelvic disproportion, umbilical cord prolapse, complications of anesthesia, fetal distress and others. In Taiwan, information regarding the pregnancy or delivery is filled out by obstetricians, and information for the newborn is filled out by pediatricians. Hospitals or clinics are obligated to report a birth and provide the above information to the local health department within 10 days of a baby’s delivery.
As preterm and/or low birth weight is an indirect cause of neonatal deaths, grouping birth weight by gestation age (BWGA) is usually done to avoid confounding effects on birth outcome [11]. BWGA is separated into three categories: small for gestation age (SGA), when the newborns’ birth weight is below the 10th percentile; appropriate for gestation age (AGA), when the newborns’ birth weight is between the 10th and 90th percentile; and large for gestation age (LGA), when the newborns’ birth weight is above the 90th percentile [12]. Gestational age in completed weeks was computed from the interval between the first day of the last menstrual period (LMP) and the date of birth. Records that lacked the date of the LMP were imputted when there was a valid month and year. Clinical estimates through ultrasound were used to estimate gestational age in cases where the date of the LMP was not reported or where the LMP date was inconsistent with the birth weight [13].
Statistical analysis
Early neonatal mortality in permillage (‰) along with 95% confidence interval (CI) for Taiwan-born mothers and foreign-born mothers was computed, respectively. The Chi-square test or Fisher’s exact test was used to examine the effects of the pregnancy and labor and delivery characteristics on early neonatal mortality univariately. Logistic regression with forward selection was done to determine which variables were associated with neonatal mortality multivariately, and the adjusted effect of maternal nationality on neonatal mortality was calculated. Odds ratios (OR) with 95% CI were used to estimate the relative risk of a factor on early neonatal death. The significance level of this study was 0.05.
Results
In 2004, there were 213,049 live births of singletons in Taiwan, among which 86.3% were from Taiwan-born mothers and 13.7% were from foreign-born mothers. The early neonatal mortality for Taiwan-born mothers was 9.4‰, and was significantly higher than that among foreign-born mothers (5.6‰). The only exception was the Philippines, where the early neonatal mortality among foreign-born mothers in Taiwan was significantly lower than that in original country [3] based on the coverage of their 95% CI (Table 1).
Since early neonatal death was associated with maternal age [14] and BWGA [12], early neonatal mortality was plotted against maternal age and BWGA for the two mother groups (Table 2 and Figs. 1, 2). A U-shaped relationship between early neonatal mortality and maternal age was seen. Neonatal mortality was highest in babies of the SGA group, followed by the LGA groups or the AGA groups. More importantly, early neonatal mortality remained significantly lower in foreign-born mothers than in Taiwan-born mothers for each maternal age group, except for maternal age ≥35. Significant differences in neonatal mortality for the AGA group were evident between Taiwan-born and foreign-born mothers.
Early neonatal mortality versus gestational age birth weight by maternal nationality in Taiwan, 2004 (Solid and broken lines denote early neonatal mortality for Taiwan-born and foreign-born mothers, respectively) SGA: small for gestational age AGA: appropriate for gestational age LGA: large for gestational age
Besides maternal age and nationality, health condition and delivery characteristics of the pregnant mothers were univariately associated with early neonatal death as well. Among the pregnant risk factors, early neonatal mortality was significantly higher than its corresponding absent group and the rate ranked the highest in babies with cervical incompetence (232.9‰), followed by hydramnion or oligohydramnion (111.5‰), chronic hypertension (96.9‰), Rh factors anaphylaxis (80.0‰), nephropathy (66.7‰), diabetes mellitus (44.7‰), mothers who previously delivered a preterm or a low birth weight baby (41.9‰), toxemia of pregnancy (28.0‰), anemia (20.7‰) and gestational hypertension (20.1‰) (Table 3).
In our analysis of delivery complications, a significantly higher early neonatal mortality was seen in babies with umbilical cord prolapse (132.4‰), premature detachment of placenta (58.9‰), or in mothers with fever (50.6‰), prolonged rupture of water bag (36.2‰), hemorrhage due to either vaginal delivery or cesarean section (27.2‰), breech presentation/malpresentation (15.8‰), univariately. Lower early neonatal mortality was seen in mothers with precipitated labor (4.8‰), difficult labor progress (2.1‰), prolonged labor (1.6‰), univariately. For mothers who received health intervention during pregnancy and labor, induction (285.5‰), chorionic villus sampling (79.4‰), cervix cerclage procedure (55.6‰), tocolysis (39.7‰), amniocentesis (31.0‰) and exploratory laparotomy (19.4‰) were significantly associated with a higher early neonatal mortality compared to mothers who did not receive the corresponding health intervention during pregnancy and labor, univariately (Table 4).
To examine whether the effect of maternal nationality on early neonatal mortality still existed multivariately, multiple logistic regression was performed. Most variables that were significantly associated with early neonatal mortality univariately remained significantly associated with early neonatal mortality multivariately, except for gestational hypertension, toxemia of pregnancy, cervical incompetence, nephropathy, Rh factors anaphylaxis, other hemorrhage and exploratory laparotomy. More importantly, after adjusting for maternal age, BWGA, risk factors of pregnant mother, delivery complications, health interventions during pregnancy and labor, newborns of foreign-born mothers were less likely to die in the first ten days of birth than were newborns of Taiwan-born mothers with an odds ratio of 0.675 (95% CI = 0.570–0.799) (Table 5).
Discussion
Using 2004 data from the Taiwan Birth Registry Database to compare the early neonatal mortality rate between foreign-born and Taiwan-born mothers, we found that newborns of foreign-born mothers were less likely to die in the first ten days of birth compared to newborns of Taiwan-born mothers, univariately. Even after the maternal age and BWGA were stratified, early neonatal mortality in foreign-born mothers was still lower than that in Taiwan-born mothers. Furthermore, multiple logistic regression revealed a significant protective effect in early neonatal death among newborns of foreign-born mothers compared to those of Taiwan-born mothers after adjusting for important factors such as delivery complications and health interventions during pregnancy and labor. Prior studies suggest that selection, economic and non-economic pathways may explain the unexpectedly favorable health outcomes of newborns among immigrants [15].
A possible cause of the selection effect on better health outcomes in newborns could be explained by the “healthy migrant theory” [16]. According to the healthy migrant theory, healthier people who are more able to migrate and be mobile generally have better birth outcomes than those who do not move. To explore whether selection can explain lower early neonatal mortality in foreign-born mothers, we listed the early neonatal mortality with its 95% CI by maternal nationality in Taiwan in our study and the early neonatal mortality of the country of origin by literature search. With the exception of the Philippines, the early neonatal mortality of newborns in foreign-born mothers who resided in Taiwan, such as women from Thailand, Myanmar, mainland China, Vietnam, Cambodia and Indonesia, and Thailand, was lower than in their countries of origin as well as in Taiwan-born groups. Since most foreign-born brides have good health, education, similar cultural background as Taiwan due to selection by marriage brokers, and have passed the physical examination required by the Ministry of Foreign Affairs, selection is one good explanation of the low early neonatal mortality in foreign-born mothers.
Economic pathway, which primarily depends upon access to maternal health care during pregnancy and delivery, is the next concern [17–20]. National Health Insurance in Taiwan (NHIT) contributes a significant amount, which impacts the health of newborns. All expectant mothers under NHIT have 10 free prenatal care visits [21]. Therefore, even if a transnational family is poor, the health of the mother and newborn during pregnancy and delivery is taken care of under the NHIT. In cases where fetal health problems are incurred during the pregnancy, parents can choose either to have an artificial abortion or to receive tocolysis to solve the minor health problem and to maintain the pregnancy. The prenatal care provided by NHIT can partially explain why the early neonatal mortality of foreign-born mothers’ newborns was lower than that of mothers in their countries of origin.
From a non-economic point of view, how well foreign-born mothers adjust to the new environment in terms of acculturation and social support is an important factor linked to favorable birth outcomes [22, 23]. Although the data in the Taiwan Birth Registry lack information on measures of acculturation and social support, one study about Taiwan transnational marriage reported that foreign-born mothers tend to befriend mothers of the same community of origin after residing in Taiwan [24]. Hence, social support for foreign-born mothers should be as good as it is for Taiwan-born mothers.
Limitations of this study deserve discussion. First of all, underreporting of deaths or misclassifications of live births to stillbirths may jeopardize our finding. Babies who die very shortly after birth tend to be less likely to be registered than babies who die later in their life in underdeveloped countries [25]. However, the problem of underreporting deaths should be minimal as we used the Birth Registry, not the household registry. Secondly, the present data lack of information on maternal education, social economic status of the mother and father, and social support. Finally, the Taiwan Birth Registry does not contain information about survival days after birth and cause of deaths, postneonatal care, and community or environmental factors. The effect of these factors on risk of death in the newborns are unable to be studied.
In conclusion, the Taiwan Birth Registry in 2004 showed that foreign-born mothers had a lower early neonatal mortality compared to Taiwan-born mothers after adjusting for important maternal and infant variables. Selection, economic and non-economic mechanisms may explain the paradox of favorable early neonatal outcomes in foreign-born mothers, but such speculations were not possible to examine using the Taiwan Birth Registry.
References
Liu KL, Laraque F. Higher mortality rate among infants of US-born mothers compared to foreign-born mothers in New York City. J Immigrant Health. 2006;8:281–9.
Zupan J, Aahman E. Perinatal mortality for the year 2000: estimates developed by WHO. Geneva: WHO; 2005.
World Health Organization. Neonatal and perinatal mortality: country, regional and global estimates. Geneva: WHO; 2006.
Rosenberg KD, Desai RA, Kan J. Why do foreign-born blacks have lower infant mortality than native-born blacks? new directions in African-American infant mortality research. J Natl Med Assoc. 2002;94:770–8.
Hessol NA, Fuentes-Afflick E. The perinatal advantage of Mexican-origin Latina women. Ann Epidemiol. 2000;10:516–23.
Singh GK, Yu SM. Adverse pregnancy outcomes: differences between US- and foreign-born women in major US racial and ethnic groups. Am J Public Health. 1996;86:837–43.
Balarajan R, Raleigh VS, Botting B. Sudden infant death syndrome and postneonatal mortality in immigrants in England and Wales. BMJ. 1989;298:716–20.
Acevedo-Garcia D, Soobader MJ, Berkman LF. The differential effect of foreign-born status on low birth weight by race/ethnicity and education. Pediatrics. 2005;115:e20–30.
Department of Statistics, Ministry of the Interior, R.O.C., Taiwan. Updated news: interior statistics spouse from foreign country & Mainland China. www.moi.gov.tw/stat/index.asp (accessed February 2005, Chinese).
Hsia HC. Transnational marriage and internationalization of capital - the case of the “Foreign Bride” phenomenon in Taiwan. Radical Q Soc Stud (Chinese). 2000;39:45–92.
Coory M. Does gestational age in combination with birth weight provide better statistical adjustment of neonatal mortality rates than birth weight alone? Paediatr Perinat Epidemiol. 1997;11:385–91.
Goldenberg RL, Cutter GR, Hoffman HJ, Foster JM, Nelson KG, Hauth JC. Intrauterine growth retardation: Standards for diagnosis. Am J Obstet Gynecol. 1989;161:271–7.
Hsieh TT, Hsu JJ, Chen CJ, Chiu TH, Liou JD, Hsieh CC, et al. Analysis of birth weight and gestational age in Taiwan. J Formos Med Assoc. 1991;90:382–7.
Geronimus AT. The effects of race, residence, and prenatal care on the relationship of maternal age to neonatal mortality. Am J Public Health. 1986;76:1416–21.
Frank R. International migration and infant health in Mexico. J Immigrant Health. 2005;7:11–22.
Wingate MS, Alexander GR. The healthy migrant theory: variations in pregnancy outcomes among US-born migrants. Soc Sci Med. 2006;62:491–8.
Mayer SE, Sarin A. Some mechanisms linking economic inequality and infant mortality. Soc Sci Med. 2005;60:439–55.
Oropesa RS, Landale NS, Davila AL. Poverty, prenatal care, and infant health in Puerto Rico. Soc Biol. 2001;48:44–66.
Gorman BK, Landale NS, Oropesa RS. Poverty, insurance, and well-baby care among mainland Puerto Rican children. Soc Biol. 2001;48:67–85.
Oropesa RS, Landale NS, Inkley M, Gorman BK. Prenatal care among Puerto Ricans on the United States mainland. Soc Sci Med. 2000;51:1723–39.
Chie WC, Lai CC. Utilization of preventive service of the national health insurance. Taiwan J Public Health (Chinese). 2001;20:43–51.
Farley T, Galves A, Dickinson LM, de Jesus Diaz Perez M. Stress, coping, and health: a comparison of Mexican immigrants, Mexican-Americans, and non-Hispanic Whites. J Immigrant Health. 2005;7:213–20.
Landale NS, Oropesa RS. Migration, social support and perinatal health: an origin-destination analysis of Puerto Rican women. J Health Soc Behav. 2001;42:166–83.
Xiao ZJ. International migration study: a case of foreign mother in Shetou Township, Changhua county. Master thesis: Department of Geography, College of Literature, National Taiwan University in Taipei, Taiwan (Chinese); 2000.
Lawn JE, Cousens S, Zupan J. 4 Million neonatal deaths: when? where? why? Lancet. 2005;365:891–900.
Acknowledgements
This study was supported by the Public Health Bureau of Taoyuan County (PMRPD3010), National Science Council (NZRPD140171) and the Ministry of Education, Taiwan, (EMRPD160051).
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
See, LC., Shen, YM. & Lin, SR. Lower early neonatal mortality among singletons in transnational marriage families: Taiwan Birth Registry. Eur J Epidemiol 23, 483–489 (2008). https://doi.org/10.1007/s10654-008-9254-2
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s10654-008-9254-2