Summary
Legumain is a newly discovered lysosomal cysteine protease that can cleave asparagine bonds and plays crucial roles in regulating immunity and cancer metastasis. Legumain has been shown to be highly expressed in various solid tumors, within the tumor microenvironment and its levels are directly related to tumor metastasis and poor prognosis. Therefore, legumain presents as a potential cancer therapeutic drug target. In this study, we have identified esomeprazole and omeprazole as novel legumain small molecule inhibitors by screening an FDA approved-drug library. These compounds inhibited enzyme activity of both recombinant and endogenous legumain proteins with esomeprazole displaying the highest inhibitory effect. Further molecular docking analysis also indicated that esomeprazole, the S- form of omeprazole had the most stable binding to legumain protein compared to R-omeprazole. Transwell assay data showed that esomeprazole and omeprazole reduced MDA-MB-231 breast cancer cell invasion without effecting cell viability. Moreover, an in vivo orthotopic transplantation nude mouse model study showed that esomeprazole reduced lung metastasis of MDA-MB-231 breast cancer cells. These results indicated that esomeprazole has the exciting potential to be used in anti-cancer therapy by preventing cancer metastasis via the inhibition of legumain enzyme activity.
Graphical abstract

Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Legumain is a newly discovered lysosomal cysteine protease that can specifically cleave asparagine bonds and has been shown to play crucial roles in regulating immunity and cancer metastasis [1]. The human Legumain gene encodes an inactive proenzyme of 433 amino acids, and the 56 kDa pro-enzyme undergoes a low pH dependent autocatalytic activation to release the active endopeptidase of 46 kDa and 36 kDa molecular weights [2, 3]. Legumain protein is highly conserved amongst biological species and is localized mainly to the endo-lysosomal system, but also found located on the cell surface and extracellular matrix. Overexpression of legumain was observed in many kinds of solid tumors and with a low to zero level background expression in normal tissue. Overexpression of legumain in cancer cells increases their migratory and invasive activity [1, 4,5,6], which suggests that legumain may play an important role in the processes of tumor invasion and metastasis.
As a protease, legumain can also hydrolyse and activate certain precursor proteins such as pro-enzymes and pro-hormones, and then participate in a variety of physiological processes [7, 8]. Legumain was recently found to be over-expressed in the tumor microenvironment, tumor-associated endothelial and stromal cells, as well as in tumor-associated macrophages (TAMs) [9, 10]. Expression of legumain was shown to be induced during tumor development, which indicates its important role in regulating the tumor microenvironment [5].
Many studies have showed that legumain can act as a prognostic factor in breast cancer, colorectal cancer and gastric carcinoma [11,12,13]. These findings were compared with the clinical outcome and other established cancer specific properties to reveal its prognostic significance. Legumain was found to be highly expressed in breast cancer compared to non-cancerous tissues, and its expression significantly correlated to an overall shorter life span in patients [14, 15]. Legumain was also highly expressed in tumor samples from colorectal cancer patients, with its expression being significantly associated with poorer differentiation, a higher degree of necrosis and apoptosis and subsequent poorer prognosis [11, 16]. The cytoplasmic immunoreactivity staining of legumain was increased in gastric cancer compared with paired normal gastric mucosal samples. Patients with legumain-positive localized tumors had a lower 5-year overall survival than those with legumain-negative tumors and multivariate survival analysis have implicated legumain as an independent prognostic marker for overall survival [13].
The connection of legumain to tumor development and its potential as an anti-cancer drug target has already led others to develop inhibitors [6]. A cysteine protease inhibitor, Cystatin E/M, was shown to down-regulate legumain activity in metastatic versus primary breast cancer cells [17]. A novel series of highly potent, tractable and structure-activity relationship (SAR) robust compounds, which showed good inhibition of legumain enzyme activity in vitro have been previously described [18]. Through SAR analysis and high throughput inhibitor screening, an optimized lead compound was identified as a legumain inhibitor, and a subsequent in vivo study showed that this compound repressed breast cancer cell invasion, migration and blocks breast cancer cell lung metastasis [19]. The numbers of studies however reporting the screening of small molecule inhibitors of legumain are relatively few and there is a continuous need for the continuing improvement of the physiochemical properties of the compounds.
We have previously produced highly active recombinant human legumain protein in the yeast Pichia pastoris system and established its suitability for high-throughput screening of legumain small molecule inhibitors [20]. In this study, we have identified novel legumain inhibitors by screening compounds from a FDA approved-drug library. In vitro and in vivo studies indicated that esomeprazole was shown to most effectively inhibit legumain enzyme activity, as well as blocking breast cancer cell invasion and lung metastasis.
Materials and methods
Cell culture and reagents
All cell lines were obtained from the American Type Culture Collection (ATCC). Human breast cancer cell lines MDA-MB-231 were cultured in DMEM (Gibco, Cat. No. 12100046) supplemented with 10% FBS (EVERY GREEN) and 100 U/ml penicillin/0.1 mg/ml streptomycin (Beyotime) in a humidified atmosphere with 5% CO2 at 37 °C. All chemicals were purchased from Sigma Aldrich (St. Louis, MO, USA) unless stated otherwise.
Western blot
Cell lysates were extracted and separated on 8% SDS-PAGE gels and transferred to PVDF membranes. After blocking with 5% non-fat milk in Tris-buffered saline containing 0.1% Tween-20 (TBST), the membrane was incubated with goat anti-Legumain primary antibody (1:200 dilution, Santa Cruz Biotechnology, sc-133,234) diluted in blocking solution at 4 °C overnight. After washing with TBST, the membrane was incubated for an additional 2 h with the appropriate secondary antibodies conjugated to HRP (Tianjin Sungene Biotech). The immunoblot bands were visualized using a chemiluminescence detection system (GE Healthcare). The density of the bands were analyzed using ImageJ software (Wayne Rasband, NIH, Bethesda, MD, USA).
Screening of legumain small molecule inhibitors
The activity of legumain protease was measured by cleaving a synthetic fluorescent substrate Z-Ala-Ala-Asn-AMC (R&D Systems) [20]. To screen small molecule inhibitors of legumain, 30 μl of 1 ng/μl activated legumain (Diluted recombinant legumain protein in 50 mM NaOAc, 0.1 M NaCl at pH 3.5 for 2 h at 37 °C) and 30 μl of 10 μM compounds (FDA-Approved-Drug-Library, Selleck, USA) were combined and then added into a black well plate for 30 min. Afterwards, 30 μl of 150 μM Substrate Z-Ala-Ala-Asn-AMC (R&D Systems) was added, including a control containing 60 μl Assay Buffer (50 mM MES, 250 mM NaCl, pH 5.0) and 30 μl of 150 μM substrate. Enzymatic activity was measured using a microplate reader (Bio-tek) at 380 and 430 nm respectively, reading every two minutes for 20 cycles. Simultaneously, legumain was incubated with AMC to exclude the possibility that the compound quenched the AMC directly.
HPLC analysis
Chromatographic separations were performed using a C18 Reverse-phase chromatographic column (HC-C18(2), 4.6 × 150 mm, 5 μm, Agilent) maintained at 25 °C. Isocratic elution was set at a flow rate of 1 ml/min for HPLC/UV. The quantification of compounds was carried out using a UV detector operating at 290 nm. The HPLC/UV mobile phase was acetonitrile-0.01 M hydrogen phosphate (30:70, v/v; pH 7.5). The run time was 30 min, and the injection volume was 10 μl for the UV detections. Esomeprazole magnesium was incubated at room temperature for two hours in Assay Buffer at pH 3.0, 5.0 and 7.0 respectively. DMSO was used as the control group.
Molecular docking analysis
Free energy binding estimations was performed using AutoDock version 4.2 software with a standard protocol. The 3D structure of legumain protein was obtained from the Protein Data Bank (code 4aw9), while small molecular compounds were obtained from PubChem. A PDBQT file of legumain protein containing a protein structure with hydrogens in all polar residues was created. All compound bonds were set to be rotatable. All calculations were done using the Lamarckian Genetic Algorithm (LGA) method. For docking studies, the global search exhaustiveness was set up at 100, and the docking poses predictions of each compound towards legumain protein was calculated from each energy minima. The average affinity for best poses was taken as the final affinity value.
Cell viability assay
Cells were seeded in 96-well plates at a density of 5 × 103 cells per well. After drug or vehicle control treatment, cell viability was assessed using 3-(4,5-dimethylthiazol-2-yl)-2,5-diphenyl tetrazolium bromide (MTT) (Solarbio, Beijing, China) dye absorbance and expressed as the percentage of non-treated cells. Briefly, MTT solution (20 μl, 0.5 mg/mL in PBS) was added into the cell dish and incubated at 37 °C for 4 h. Then, DMSO (200 μl/well) was added to dissolve the formazan dyes and the absorbance was measured at 490 nm using a microplate reader (Bio-Rad, USA).
Generation of a stable cell line overexpressing legumain
The pLVX-IRES-puro-Legumain recombinant plasmid was constructed and verified by DNA sequencing. Lentivirus particles were generated by transfecting HEK-293 T cells with pLVX-IRES-puro-Legumain (3 μg), psPAX2 (2.25 μg) and pMD2.G (0.75 μg) using Lipofectamine 2000 (Invitrogen, Carlsbad, CA, USA) according to the manufacturer’s instructions. Viruses were collected 48 h post-transfection, and used for infection overnight in the presence of 8 μg/mL polybrene. MDA-MB-231 cells were infected with pLVX-IRES-puro-Legumain lentiviruses and selected in 1 μg/ml puromycin for at least two weeks.
Transwell cell invasion assay
Invasion of cancer cells through Matrigel was determined using a Transwell system (8 μm PET with polycarbonate membrane, Millicell Hanging). 5 × 104/cells (200 μl) in DMEM (containing 10% FBS) with different concentrations of drug were seeded onto the Matrigel-coated transwell chamber. DMEM (containing 20% FBS) was used as a chemoattractant in the lower chambers. After incubation for 32 h at 37 °C, cells that had penetrated to the bottom side of the membrane were then fixed in 4% Paraformaldehyde, stained with 1% crystal violet in 25% methanol and then quantified under an inverted microscope. The invasion index measured as relative migration of cells across the Matrigel was calculated.
Breast cancer cell in vivo metastasis assay
6–8 week old female BALB/c nude mice (China’s food and drug research institute, Beijing). MDA-MB-231 cells (2.5 × 107/ml) in serum free media were implanted into the mammary fat pad of the mice (100 μl/mouse). When the volume of the tumors reached 100 mm3 (length×width2)/2), mice were then divided into control groups (6 mice/group) and two test groups (6 mice/group). Different concentrations of Esomeprazole magnesium (3 mg/kg, 10 mg/kg) were intraperitoneally injected into mice every day for 39 days. 24 h after the last drug injection, the animals were sacrificed and tumors/organs were collected. For lung metastasis analysis, the lungs were removed and fixed in Bouin’s solution for 24 h and the number of tumor nodules on the whole surface of the lungs were counted by microscopy. Sections of the lungs were stained with hematoxylin and eosin (HE) to confirm the formation of metastases. All animal experiments were approved by the Tianjin University of Science and Technology’s Policy on the Care and Use of Laboratory Animals.
Statistical analysis
Data are presented as the mean ± standard deviation. P values were determined using a student’s t test. One-way ANOVA followed by the Bonferroni post hoc correction were used for multiple comparisons. A P value <0.05 was considered significant.
Results
Expression of legumain in cancer
The expression of legumain in cancer cells was determined by Western blot (Fig. 1a) and Real time-PCR (Fig. 1b). legumain has been shown to be highly expressed in many cancer cell lines including the metastatic breast cancer cell MDA-MB-231 and correlates with a poor breast cancer prognosis [14, 15]. We analyzed the Cancer Genome Atlas (TCGA) gene expression data and found that high expression of legumain was associated with poorer overall survival in the triple negative breast cancer patients (Basal type), and that the 10 year survival ratio drops significantly (Fig. 1c).
Expression of legumain in cancer. a Detection of the expression of legumain in a panel of selected cell lines, including human hepatic cell line HL-7702, hepatoma cell line HepG2, cervical cancer cell line HeLa, breast cancer cell line MDA-MB-231, breast cancer cell line MCF7 and gastric cancer cell lines MGC803, by Western blot and densitometric analysis of Western blot by ImageJ software. The Legumain protein levels were normalized to β-actin. b Detection of the expression of legumain in cell lines by QRT-PCR. The results from at least three replicates are presented as means ± SD. c Kaplan-Meier analysis of survival of the triple negative breast cancer patients (Basal type) with different Legumain expression levels. The expression level of Legumain (LGMN) gene was estimated using Cufflinks in fragments per kilobase of exon model per million mapped reads (FPKM)
Screening and identification of legumain small molecule inhibitors
To screen for small molecule inhibitors of legumain, we established a legumain enzymatic activity assay method for high-throughput screening using functional recombinant human Legumain protein expressed in Pichia pastoris [20]. By screening a 2697 compound library set (FDA Approved-Drug-Library, Selleck, USA), three compounds, Esomeprazole magnesium, Omeprazole and Lansoprazole, were found to competitively inhibit the legumain enzyme activity (Fig. 2a). In addition, these three compounds importantly did not affect the fluorescence of AMC (Fig. 2b), which excluded the possibility that they quenched AMC directly.
Screening and identification of legumain small molecule inhibitors. a By screening a compound library (FDA Approved-Drug-Library, Selleck, USA), esomeprazole magnesium, omeprazole and lansoprazole were identified as inhibiting the legumain enzyme activity, 10 μM of compounds were incubated with recombinant legumain (0.33 ng/ml) and the fluorogenic substrate for the enzyme activity assay. Data are presented as the mean ± SD of three independent experiments. b Specificity testing of the identified inhibitors. 1 or 10 μM of compounds were incubated with different concentrations of AMC (0–64 μM) alone and fluorescence measured every 2 min for 20 cycles. Data are presented as mean ± SD of three independent experiments
Interestingly, these three compounds, esomeprazole, omeprazole and lansoprazole are all proton pump inhibitors, which reduce stomach acid and widely used to treat gastroesophageal reflux and peptic ulcer diseases. Omeprazole is a mixture of two mirror-imaged molecules (S- and R- configuration), esomeprazole magnesium is made of two S-omeprazole combined with Mg2+ (Fig. 3a). Inhibition of legumain activity was further tested with varying concentrations of the three compounds (Fig. 3b) and SPSS statistics analysis revealed IC50 values of 83 nM, 693 nM and 310 nM respectively for treatment with esomeprazole magnesium, omeprazole and lansoprazole. These results indicate Esomeprazole to be the most potent inhibitor of legumain enzyme activity.
Esomeprazole, omeprazole and lansoprazole inhibit the enzymatic activity of recombinant legumain. a Molecular structures of compounds esomeprazole magnesium, omeprazole and lansoprazole. The three proton pump inhibitors contain the same parent nucleus. b Different doses of compounds were incubated with recombinant legumain (0.33 ng/ml) for the enzyme activity assay, the results were used to measure the IC50 of enzyme activity inhibition. Data are presented as mean ± SD of three independent experiments. c HPLC analysis of the esomeprazole magnesium pre-treated under different pH conditions. A: DMSO as the control, B: pH 3, C: pH 5, D: pH 7; E: without pre-treatment. d Esomeprazole magnesium (17 nM) pretreated at different pH was incubated with recombinant legumain (0.83 ng/ml) for enzyme activity assay studies. Data are presented as mean ± SD of three independent experiments
It has been reported that omeprazole can be converted to the sulfonamide form at pH 3 and below to be active as a proton pump inhibitor [21]. To further verify whether the esomeprazole magnesium-induced inhibitory activity of legumain was related to a molecular conformational change in the acidic buffer, esomeprazole magnesium was incubated in buffer with a different pH for two hours before HPLC analysis and enzyme activity testing. At pH 3 the molecular conformation of esomeprazole was dramatically altered, partially converted at pH 5, but with no change at the pH 7 (Fig. 3c). Interestingly, the pH 7-pretreated esomeprazole magnesium showed the highest inhibition of legumain activity, similar to without pretreatment, while the pH 3 and pH 5-pretreated esomeprazole magnesium only showed partial inhibition (Fig. 3d). These results indicated that the esomeprazole-induced inhibitory activity of legumain is mainly mediated by its physiological pH unaltered molecular state.
To further determine the molecular mechanism of how these compounds inhibit legumain enzyme activity, the binding mode and interaction of legumain protein with esomeprazole (S-omeprazole), R-omeprazole or lansoprazole were estimated using molecular docking analysis. The binding modes were visualized using PyMOL (version 5.10.130.0) and Ligplot software (version 2.1) [22] in Three- and Two-dimensional representations respectively. Although these compounds were all bound to legumain near its three active sites, the amino acids residues involved in the interaction with each ligand were different. Ligplot analysis revealed that residues Arg44, Cys189, Ser216, Tyr217 and Ala218 were common residues of legumain interacting with all three compounds, while His45, Asp147, Asp231 were interacting residues only in the case of formation of the legumain-esomeprazole or legumain-lansoprazole complexes (Fig. 4). The major bond of conjugation in the formation of these three complexes were presumably hydrophobic interactions. The binding energy value (ΔG) and inhibitory constant of legumain-esomeprazole, legumain-R-omeprazole and legumain-lansoprazole complex are −4.33, −3.31, −4.09 kcal/mol and 0.67, 3.72, 1 mM respectively. These data indicates that Esomeprazole has the most stable binding with legumain protein, followed by lansoprazole and R-omeprazole, which is consistent with the in vitro legumain enzyme activity inhibition data (Fig. 3b).
The molecular docking analysis of the three identified legumain inhibitors with legumain protein using AutoDock software. Structure of legumain-esomeprazole (S-omeprazole), legumain-R-omeprazole and legumain-lansoprazole complex (left). Three active sites of legumain are shown as Asn42, His148 and Cys189. Interaction plot by LIGPLOT (right) (Dotted red and dotted green lines represent hydrophobic contacts and hydrogen bonds with its length respectively)
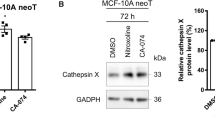
Esomeprazole and omeprazole inhibit the endogenous activity of legumain in breast cancer cell extracts
The cytotoxicity of the three novel legumain inhibitors against breast cancer cell line MDA-MB-231 was firstly assessed by MTT assay. As shown in Fig. 5a, Esomeprazole magnesium and Omeprazole had no significant effect on cancer cell viability with 30 μM treatment for 48 h, while the Lansoprazole showed a low level of cytotoxicity at the higher concentration treatment. To further verify whether Esomeprazole magnesium and Omeprazole can effectively inhibit the endogenous enzyme activity of legumain, cell lysates extracted from MDA-MB-231 cells or MDA-MB-231 stable cell line overexpressing legumain were incubated with different concentrations of esomeprazole magnesium or omeprazole. As shown in Fig. 5b, esomeprazole magnesium and omeprazole inhibited the enzyme activity of endogenous legumain in a dose-dependent manner. MDA-MB-231 stable cell line overexpressing legumain showed a high legumain enzyme activity compared to the MDA-MB-231 cells alone, and treatment with esomeprazole magnesium and omeprazole showed effective inhibition of legumain enzyme activity in a dose-dependent manner (Fig. 5c). These cellular tests further demonstrate that esomeprazole and omeprazole are specific inhibitors of legumain and interestingly that Esomeprazole which is the R-omeprazole has a superior inhibitory effect on legumain enzyme activity than a mixture of the two mirror-image molecules of omeprazole.
Esomeprazole and omeprazole inhibit the activity of endogenous legumain in breast cancer cells. a Effects of esomeprazole magnesium, omeprazole and lansoprazole on the viability of MDA-MB-231 breast cancer cells. Cells were incubated with different concentrations of compounds for 48 h and the cell viability was determined by MTT assay. Adriamycin (200 nM) was used as the positive control. The normalized value of cell viability from the untreated cells was arbitrarily set as 1.0. The results from at least three replicates are presented as mean ± SD (* P < 0.05). b Different doses of Esomeprazole magnesium or Omeprazole were incubated with cell lysates extracted from the MDA-MB-231 cells and the fluorogenic substrate for the enzyme activity assay. Data are presented as mean ± SD of three independent experiments. c Different doses of Esomeprazole magnesium or Omeprazole were incubated with cell lysates extracted from the MDA-MB-231 stable cell line overexpressing legumain and the fluorogenic substrate for the enzyme activity assay. Data are presented as mean ± SD of three independent experiments
Esomeprazole and omeprazole reduce breast cancer cell invasion
To assess the effects of the identified legumain inhibitors, esomeprazole magnesium and omeprazole on cancer cell invasion, a Transwell assay was performed. MDA-MB-231 is a highly invasive triple-negative breast cancer cell line and is well established as a tool for breast cancer metastasis studies. MDA-MB-231 cells were added to matrigel-coated inserts, which were placed above the wells as the chemoattractant, and various concentrations of inhibitors were added to each insert. The number of invading cells were counted and data showed that treatment with esomeprazole magnesium and omeprazole reduced cancer cell invasion in a dose-dependent manner (Fig. 6a, b). MTT assay analysis showed that treatment with esomeprazole and omeprazole (at least at the concentration below 10 μM) did not affect cell viability, which indicates that the reduction of cancer cell invasion treated by esomeprazole and omeprazole is not simply due to cytotoxicity (Fig. 6b).
Esomeprazole and omeprazole reduce breast cancer cell invasion. a Transwell assay was used to measure the invasion of MDA-MB-231 cells treated with esomeprazole magnesium or omeprazole at different concentrations of 2.5 μM, 5 μM, 10 μM. (b) Quantitation of the invaded cancer cells of results in (a), the invasion index measured as relative migration of cells across the Matrigel was calculated. In the meantime, MTT assay was used to measure the cell viability after treatment with esomeprazole magnesium or omeprazole at different concentrations of 2.5 μM, 5 μM, 10 μM. Scale bar, 100 μm. The results from at least three replicates are presented as means ± SD (* P < 0.05, ** P < 0.01)
Esomeprazole prevents breast cancer metastasis in vivo
The effect of the most promising legumain inhibitor, esomeprazole magnesium, on its ability to reduce breast cancer cells metastasis in vivo was further examined. A mice model of breast cancer metastasis was developed by injecting MDA-MB-231 cells into the mammary fat pad of nude mice. Esomeprazole magnesium was administered by intraperitoneal injection into the two mice groups with doses of 3 mg/kg and 10 mg/kg treatment respectively with normal saline being given to the control group. After 39 days of treatment, the lungs were assessed for the presence of metastatic nodules, as lung metastasis is one of the most common distant metastases of breast cancer [23]. The number of metastatic nodules on the lungs were significantly decreased with 10 mg/kg treatment. The 3 mg/kg dosage also decreased the number of lung metastasis (Fig. 7a, b). No clear metastatic nodules were detected on the livers. Moreover, the body weight was tested between the control group and drug-treated mice, and no significant toxicity was observed (Fig. 7c). The volume and masses of the tumors in the treated mice did not change dramatically in comparison with the control. These results further indicate that esomeprazole specifically reduces breast cancer cell metastasis in vivo.
Esomeprazole prevents lung metastasis of breast cancer cell using an orthotopic transplantation nude mouse model. a Representative mouse lungs of mice treated with 3 or 10 mg/kg esomeprazole magnesium or normal saline as the control. Lower panels indicate IHC staining. The arrows show the metastatic nodules. b Quantification of the metastasized cancer nodules found on the 3 or 10 mg/kg esomeprazole magnesium treated and untreated mouse lungs. * P < 0.05. c The body weight changes of treated mice were measured on day 4, 8, 12, 16, 20, 24, 28, 32, 36 and 40. Scale bar, 1 mm
Discussion
Breast cancer has the highest incidence of disease among women in the world with metastasis resulting in 90% of deaths of breast cancer patients [15, 24, 25]. Cancer cell metastasis is a complex process that involves changes to the tumor induced microenvironment leading to increased invasiveness and migratory character of cancer cells [26]. The over-expression of legumain in cancer cells significantly influences the processes of tumor invasion and metastasis [27]. Increasing the expression of legumain in cancer cells enhances the metastasis and invasive capabilities of cancer cells via the activation of matrix metalloproteinases (MMPs) and cathepsins stimulated by legumain mediated proteolytic cleavage [28, 29]. MMPs and cathepsins are involved in the degradation and breakdown of extracellular matrix (ECM), which allows cancer cells to migrate out of the primary tumor to form metastases. In addition, MMPs have been shown to proteolytically activate Transforming growth factor beta (TGF-β, which has been shown to promote epithelial mesenchymal transition (EMT), a key process involved in cancer metastasis. It has been demonstrated that MMP-2 contributes migration and invasion of human breast cancer cells [19].
Studies have suggested that legumain may act as a biomarker for the diagnosis of various cancers [30]. Legumain expression could act as a prognostic factor in patients with breast cancer as well as a potential target for directed tumor therapy. Legumain inhibitors therefore are promising treatment tools for oncotherapy [31]. Although compounds targeting legumain have been reported, their toxicity and stability remain to be determined [19, 32, 33]. Here, we have screened and identified three FDA-approved drugs, esomeprazole magnesium, omeprazole and lansoprazole, as specific inhibitors of legumain protease. We have demonstrated that esomeprazole magnesium has a more potent inhibitory effect, with an IC50 value of 83 nM, which is half that of a recently reported legumain inhibitor compound 38u [18]. Cell and animal based models study further demonstrated that esomeprazole magnesium most efficiently reduced cancer cell invasion and metastasis, but without impacting on proliferation. Therefore, as an FDA-approved low toxic, low cost drug and newly identified efficient legumain inhibitor, esomeprazole may have potential to be used as an anti-cancer drug using the drug repurposing strategy. However, considering legumain is a lysosomal protease, to avoid any possible side effects of using legumain inhibitors by affecting the natural function of lysosome, then potentially only patients with elevated expression levels of legumain may have the most benefit for this particular cancer therapy treatment.
Interestingly, the three novel legumain inhibitors identified here, esomeprazole, omeprazole and Lansoprazole, all belong to the class of proton pump inhibitors. Proton pump inhibitors have been previously suggested as anticancer agents due to their ability in targeting and inactivating proton pumps to effectively increase the extracellular acidic pH within tumors [34, 35]. A clinical trial study showed that an intermittent high dose of esomeprazole enhanced the antitumor effects of docetaxel and cisplatin regimen in patients with metastatic breast cancer [36]. The inhibition of H, K-ATPase enzyme activity by the 2-pyridylmethylsulfinyl benzimidazoles including Omeprazole and Lansoprazole was studied and the mode of action proposed as the conversion of the drug molecules under acidic conditions. The compounds protonate and accumulate in an acid space and undergo an acid-catalyzed conversion to a tetracyclic sulfenamide, which then reacts with cysteines in the α subunit of the H, K-ATPase (21). Recently it has been reported that Lansoprazole inhibited the cysteine protease Legumain by direct interaction with the SH group in its active site [37]. In this study, we have identified esomeprazole (S-omeprazole), omeprazole and lansoprazole as specific inhibitors of legumain enzymatic activity. Interestingly, esomeprazole showed a more effective degree of inhibition, about 8-fold and 4-fold compared to that of omeprazole and lansoprazole respectively. Further molecular docking analysis indicated that esomeprazole, omeprazole, lansoprazole were all bound to legumain near its three active sites. Esomeprazole has the most stable binding to legumain protein, following by lansoprazole and the least to R-omeprazole. Moreover, the effect of pH on the esomeprazole-induced inhibition of legumain activity was investigated, interestingly, esomeprazole magnesium showed the greater inhibition compared to the converted molecules. These results suggest that esomeprazole can interact with legumain directly to inhibit enzyme activity and that the converted tetracyclic sulfenamide in low pH conditions contributes to the inhibition. However, it is also important to mention that due to esomeprazole also acting as a proton pump inhibitor then for it to be used as an oral drug, the enteric-coated formulation type of esomeprazole should be used to maximize its effect on cancer treatment.
In summary, we have identified novel legumain inhibitors by screening compounds from a FDA approved-drug Library. In vitro and in vivo studies show that esomeprazole inhibited Legumain enzyme activity and prevented breast cancer cell invasion and lung metastasis. The novel anticancer feature of esomeprazole is likely to be mediated through inhibition of legumain enzyme activity and by regulating the tumor microenvironment. Therefore, we propose that esomeprazole has the exciting potential to be used in cancer therapy treatment by preventing cancer metastasis via the inhibition of legumain protease enzyme activity.
References
Dall E, Brandstetter H (2015) Structure and function of legumain in health and disease. Biochimie 122(12):126–150
Barrett AJ, Rawlings ND (2001) Evolutionary lines of cysteine peptidases. Biol Chem 382(5):727–733
Dall E, Brandstetter H (2013) Mechanistic and structural studies on legumain explain its zymogenicity, distinct activation pathways, and regulation. Proc Natl Acad Sci U S A 110(27):10940–10945
Chen JM, Dando PM, Rawlings ND et al (1997) Cloning, isolation, and characterization of mammalian legumain, an asparaginyl endopeptidase. J Biol Chem 272(12):8090–8098
Liu C, Sun C, Huang H et al (2003) Overexpression of legumain in tumors is significant for invasion/metastasis and a candidate enzymatic target for prodrug therapy. Cancer Res 63(11):2957–2964
Mai CW, Chung FF, Leong CO (2017) Targeting legumain as a novel therapeutic strategy in cancers. Curr Drug Targets 18(11):1259–1268
Munoz Najar UM, Neurath KM, Vumbaca F, Claffey KP (2006) Hypoxia stimulates breast carcinoma cell invasion through MT1-MMP and MMP-2 activation. Oncogene 25(16):2379–2392
Zhang Z, Song M, Xia L et al (2015) Delta-secretase cleaves amyloid precursor protein and regulates the pathogenesis in Alzheimer’s disease. Nat Commun 6:8762
Liu Z, Xiong M, Gong J et al (2014) Legumain protease-activated TAT-liposome cargo for targeting tumours and their microenvironment. Nat Commun 5:4280
Reisfeld RA (2013) The tumor microenvironment: a target for combination therapy of breast cancer. Crit Rev Oncog 18(1–2):115–133
Murthy RV, Arbman G, Gao J et al (2005) Legumain expression in relation to clinicopathologic and biological variables in colorectal cancer. Clin Cancer Res 11(6):2293–2299
Luo Y, Zhou H, Krueger J et al (2006) Targeting tumor-associated macrophages as a novel strategy against breast cancer. J Clin Invest 116(8):2132–2141
Guo P, Zhu Z, Sun Z et al (2013) Expression of legumain correlates with prognosis and metastasis in gastric carcinoma. PLoS One 8(9):e73090
Lin Y, Qiu Y, Xu C et al (2014) Functional role of asparaginyl endopeptidase ubiquitination by TRAF6 in tumor invasion and metastasis. J Natl Cancer Inst 106(4):dju012
Wu M, Shao GR, Zhang FX, Wu WX, Xu P, Ruan ZM (2014) Legumain protein as a potential predictive biomarker for Asian patients with breast carcinoma. Asian Pac J Cancer Prev 15(24):10773–10777
Haugen MH, Boye K, Nesland JM et al (2015) High expression of the cysteine proteinase legumain in colorectal cancer - implications for therapeutic targeting. Eur J Cancer 51(1):9–17
Briggs JJ, Haugen MH, Johansen HT et al (2010) Cystatin E/M suppresses legumain activity and invasion of human melanoma. BMC Cancer 10:17
Eddie SL, Gregson A, Graham E et al (2019) Identification and SAR exploration of a novel series of Legumain inhibitors. Bioorg Med Chem Lett 29(12):1546–1548
Qi Q, Obianyo O, Du Y, Fu H, Li S, Ye K (2017) Blockade of asparagine endopeptidase inhibits Cancer metastasis. J Med Chem 60(17):7244–7255
Zhao T, Li Z, Guo Z et al (2018) Functional recombinant human Legumain protein expression in Pichia pastoris to enable screening for Legumain small molecule inhibitors. Protein Expr Purif 150:12–16
Besancon M, Simon A, Sachs G, Shin JM (1997) Sites of reaction of the gastric H,K-ATPase with extracytoplasmic thiol reagents. J Biol Chem 272(36):22438–22446
Laskowski RA, Swindells MB (2011) LigPlot+: multiple ligand-protein interaction diagrams for drug discovery. J Chem Inf Model 51(10):2778–2786
Smid M, Wang Y, Zhang Y et al (2008) Subtypes of breast cancer show preferential site of relapse. Cancer Res 68:3108–3114
Weigelt B, Peterse JL, van 't Veer LJ (2005) Breast cancer metastasis: markers and models. Nat Rev Cancer 5(8):591–602
Rustogi A, Budrukkar A, Dinshaw K, Jalali R (2005) Management of locally advanced breast cancer: evolution and current practice. J Cancer Res Ther 1(1):21–30
Coghlin C, Murray GI (2010) Current and emerging concepts in tumour metastasis. J Pathol 222(1):1–15
Edgington LE, Verdoes M, Ortega A et al (2013) Functional imaging of legumain in cancer using a new quenched activity-based probe. J Am Chem Soc 135(1):174–182
Chen JM, Fortunato M, Stevens RA, Barrett AJ (2001) Activation of progelatinase a by mammalian legumain, a recently discovered cysteine proteinase. Biol Chem 382(5):777–783
Kessenbrock K, Plaks V, Werb Z (2010) Matrix metalloproteinases: regulators of the tumor microenvironment. Cell 141(1):52–67
Wang L, Chen S, Zhang M et al (2012) Legumain: a biomarker for diagnosis and prognosis of human ovarian cancer. J Cell Biochem 113(8):2679–2686
Gawenda J, Traub F, Lück HJ, Kreipe H, von Wasielewski R (2007) Legumain expression as a prognostic factor in breast cancer patients. Breast Cancer Res Treat 102(1):1–6
Loak K, Li DN, Manoury B et al (2003) Novel cell-permeable acyloxymethylketone inhibitors of asparaginyl endopeptidase. Biol Chem 384(8):1239–1246
Ovat A, Muindi F, Fagan C et al (2009) Aza-peptidyl Michael acceptor and epoxide inhibitors--potent and selective inhibitors of Schistosoma mansoni and Ixodes ricinus legumains (asparaginyl endopeptidases). J Med Chem 52(22):7192–7210
Lu ZN, Tian B, Guo XL (2017) Repositioning of proton pump inhibitors in cancer therapy. Cancer Chemother Pharmacol 80(5):925–937
Spugnini EP, Citro G, Fais S (2010) Proton pump inhibitors as anti vacuolar-ATPases drugs: a novel anticancer strategy. J Exp Clin Cancer Res 29(1):44
Wang BY, Zhang J, Wang JL et al (2015) Intermittent high dose proton pump inhibitor enhances the antitumor effects of chemotherapy in metastatic breast cancer. J Exp Clin Cancer Res 34(1):85
Bosnjak T, Solberg R, Hemati PD, Jafari A, Kassem M, Johansen HT (2019) Lansoprazole inhibits the cysteine protease legumain by binding to the active site. Basic Clin Pharmacol Toxicol 125(2):89–99
Funding
The work was supported by the Scientific and Technological Research Program of Tianjin Municipal Education Commission, Tianjin Natural Science Foundation grant (18JCZDJC97500).
Author information
Authors and Affiliations
Corresponding authors
Ethics declarations
Conflict of interest
All authors declare no conflict of interest.
Ethical approval
All applicable international, national, and/or institutional guidelines for the care and use of animals were followed. All procedures performed in the studies involving human participants were in accordance with the ethical standards of the institutional and/or national research committee and with the 1964 Helsinki declaration and its later amendments or comparable ethical standards.
Informed consent
Informed consent was obtained from all individual participants included in the study.
Additional information
Publisher’s note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
About this article
Cite this article
Zhao, T., Liu, Y., Hao, Y. et al. Esomeprazole inhibits the lysosomal cysteine protease legumain to prevent cancer metastasis. Invest New Drugs 39, 337–347 (2021). https://doi.org/10.1007/s10637-020-01011-3
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s10637-020-01011-3