Summary
Background We examined the efficacy of mirtazapine in preventing delayed nausea and vomiting following highly emetogenic chemotherapy (HEC). Patients and methods Patients who had experienced delayed emesis and would be subsequently scheduled for at least three more cycles of the same chemotherapy were randomly assigned to either a mirtazapine (15 mg daily on days 2–4) or a control group. In addition, both groups received a standard triplet regimen comprising aprepitant, a 5-HT3 receptor antagonist, and dexamethasone (7.5 mg on days 2–4). The chemotherapy regimens were either an epirubicin plus cyclophosphamide regimen or cisplatin-containing regimens. The primary end point was a complete response (no emesis and no rescue treatment) to the delayed phase (25–120 h post-chemotherapy) during Cycle 1. The impact on quality of life (QOL) was assessed using the Functional Living Index–Emesis (FLIE) questionnaire. Results Of 95 enrolled patients, 46 were assigned to the mirtazapine group and 49 to the control group. The complete response rate in the delayed phase during Cycle 1 was significantly higher with mirtazapine than in the control group (78.3% versus 49.0%, P = 0.003). The main adverse effects of mirtazapine were mild to moderate somnolence and weight gain. Mean total FLIE scores were similar between the two arms. Conclusions This is the first randomized prospective study to show that adding mirtazapine has a substantial and statistically significant benefit with good tolerance in patients with breast cancer who have experienced delayed emesis following the same prior HEC. (Trial registration: ClinicalTrials.gov NCT02336750).
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Chemotherapy-induced nausea and vomiting (CINV) is a source of major anxiety for patients with cancer receiving chemotherapy, significantly impairing their quality of life (QOL). It is therefore recognized as one of the most distressing adverse effects (AEs) of chemotherapy [1, 2]. Highly emetogenic chemotherapy regimens (HEC; >90% frequency of emesis) typically include agents such as cisplatin, mechlorethamine, streptozotocin, or high-dose cyclophosphamide. The antiemesis approach to preventing CINV following HEC recommended by multiple international antiemetic guidelines [3,4,5] is a triplet regimen comprising a 5-HT3 receptor antagonist (RA) combined with dexamethasone and aprepitant.
Although many studies have shown that the recommended triplet antiemesis therapy based on palonosetron achieves a more than 80% complete response rate in the acute phase and 70% in the delayed phase [6,7,8,9], there is still a need for additional antiemetic agents.
Olanzapine, an atypical antipsychotic agent [10, 11], blocks multiple neurotransmitter receptors including dopamine (D1, D2, D4), serotonin (5HT2A, 5HT2C, 5HT3), alpha-1 adrenergic, histamine (H1), and multiple muscarinic receptors. Many randomized trials have confirmed the beneficial effect of adding olanzapine to standard antiemetic regimens [12,13,14,15,16]. The National Comprehensive Cancer Network (NCCN) guideline panel has therefore listed olanzapine-containing regimens as another option for HEC antiemesis [5]. However, long-term use of olanzapine is associated with adverse metabolic effects, including weight gain, dyslipidemia, and onset of diabetes mellitus [17].
Like olanzapine, mirtazapine, a new antidepressant [18], has a similar affinity for 5-HT2, 5-HT3, and H1 receptors; however, it has almost no anticholinergic effect. Compared with olanzapine, mirtazapine has been reported to more effectively achieve nausea reduction and appetite increase, with better tolerance, less dizziness, and fewer cardiovascular toxicities [19, 20].
Several small studies have investigated the antiemetic effect of mirtazapine [21,22,23,24] and found that it is a successful and safe antiemetic agent for CINV, post-operative anesthesia-related toxicity, and pregnancy-induced nausea.
To the best of our knowledge, there are no published data concerning the use of mirtazapine as a secondary prophylactic when a conventional antiemetic regimen has failed. This study was conducted to evaluate the efficacy and safety of mirtazapine combined with aprepitant, a 5-HT3 RA, and dexamethasone, when used as a secondary prophylactic, in controlling delayed CINV following HEC.
Methods
Study design
This was an open label, randomized, multicenter phase III trial conducted in five hospitals in China (ClinicalTrials.gov number, NCT02336750). Eligible patients were randomly assigned to either a mirtazapine or control group, both of which received aprepitant, a 5-HT3 RA, and dexamethasone. Patients were assessed for three consecutive cycles of chemotherapy. The ethics committees of the participating centers approved the protocol. Written informed consent was obtained from each patient before enrollment. The stratification factor was EC (epirubicin plus cyclophosphamide) versus cisplatin-containing regimens.
Eligibility and exclusion criteria
Eligible patients were women aged 18 years or older with breast cancer who had experienced delayed emesis after receiving EC (epirubicin at a dose of 80–100 mg/m2 plus cyclophosphamide at a dose of 600 mg/m2) or a cisplatin-containing regimen.
Patients were expected to undergo at least three cycles of the same chemotherapy. Additional eligibility criteria included a European Cooperative Oncology Group (ECOG) performance status of 0–2, a life expectancy of at least 12 weeks, and adequate hematologic, hepatic, and renal function. Women of childbearing age were required to have a negative pregnancy test performed within 7 days before enrollment and agree to use appropriate birth control throughout their participation in the study.
Patients were excluded if they had one of the following: nausea/vomiting in the 24 h before enrollment, administration of aprepitant in the most recent cycle of chemotherapy before enrollment, serious emotional or mental disorders, treatment with benzodiazepines or opioids (including oxycodone/acetaminophen) within 48 h of entry to the study (except for a single daily dose of triazolam, temazepam, or midazolam), concurrent abdominal or pelvic radiotherapy, known hypersensitivity to mirtazapine, known history of myocardial infarction or severe epilepsy, uncontrolled diabetes mellitus or active infection, concurrently receiving CYP3A4 inducers (such as carbamazepine, phenytoin, or phenobarbital), concurrent administration of any other investigational drug, or prior enrollment in other clinical trials within 4 weeks of the start of this study treatment.
Treatment regimen
All participants received aprepitant (125 mg on Day 1 and 80 mg on Days 2 and 3), a 5-HT3 RA (a standard dose of palonosetron, granisetron, or ondansetron intravenously) and dexamethasone (7.5 mg orally on Days 2–4). In addition, patients in the experimental group received oral mirtazapine (15 mg, once daily) on Days 2–4. Rescue therapy was permitted only when patients had breakthrough vomiting.
Study visits and assessment
Daily records (diary cards) of vomiting or retching (number of episodes, severity, and time) between 0 and 120 h were completed by patients. AEs were assessed and graded in accordance with the Common Terminology Criteria for AEs, version 4.0 [25]. In addition, the Functional Living Index--Emesis (FLIE) questionnaire was completed by patients on Days 2 and 6 of each cycle. Investigators recorded AEs until 28 days after the last dose of mirtazapine and recovery to grade 1 or 0 of any acute toxicities associated with mirtazapine.
Outcomes
The primary end point was a complete response (CR, no emesis and no rescue treatment) for the delayed phase (25–120 h post-chemotherapy) during Cycle 1. Secondary end points included CR rates for the delayed phase of Cycles 2 and 3, the acute (0–24 h post-chemotherapy) and overall phases (0–120 h post-chemotherapy) of Cycles 1–3, complete control (CC, no emesis, no rescue medication use, and no more than grade 1 nausea) during the three phases throughout three cycles, toxicities, and impact on QOL.
QOL was assessed by the FLIE questionnaire on Days 2 and 6 of each cycle [26]. No impact on daily life was defined as an average FLIE item score exceeding 6 on the 7-point scale (or total score > 108).
Statistical analysis
On the basis of a previously reported study on mirtazapine [27], the CR rates in the delayed phase were estimated as 64% and 80% in the control and mirtazapine groups, respectively. The study design was two-sided, with α = 0.05 and 80% power. It was calculated that a sample size of 96 per group was required. Assuming that 10% of patients would withdraw or drop out, the target sample size was 212 patients (106 for each group).
All patients who received at least one dose of the study medication were included in the efficacy and safety analysis. The χ2 test was used to compare CR and CC rates between the two arms. Univariable and multivariable logistic regression analyses were performed to evaluate independent risk factors. Differences in FLIE scores between treatment arms were assessed by Student’s t test. A P value of 0.05 was considered to denote statistical significance. All tests are reported as two-sided.
The Statistical Package for the Social Sciences software (SPSS) version 16.0 (IBM SPSS, Chicago, IL, USA) was used for all statistical analyses.
Results
Patients
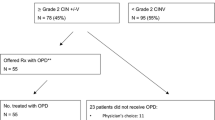
Between 16 January 2015 and 26 September 2017, a total of 100 patients were enrolled in this study and randomized. Ninety-five patients (46 assigned to the mirtazapine group and 49 assigned to the control group) began the study and received at least one cycle of treatment.
Sixty-five and 43 patients entered the second and third cycles, respectively (Fig. 1). Most of the patients (20.4% in the mirtazapine group and 21.7% in the control group before Cycle 2; 16.7% and 14.3%, respectively before Cycle 3) discontinued participation in the study because of difficulties in completing diary cards or FLIE questionnaires. A χ2 test showed that the proportions of patients who received one, two, or three cycles of treatment were similar between the two arms (P = 0.266). The study was closed prematurely in January 2018 because of the slow enrollment.
The baseline clinical characteristics of the 95 enrolled patients are listed in Table 1. There were no significant differences between the two arms in age, chemotherapy regimen administered, ECOG performance status, TNM stage, or 5-HT3 RA received.
Efficacy
Compared with the control group, the CR rates in the first cycle were significantly higher in the mirtazapine group: 78.3% versus (vs.) 49.0% (OR 3.75, 95% CI: 1.529–9.196, P = 0.003) in the delayed phase and 58.7% vs. 34.7% (OR 2.68, 95% CI: 1.165–6.140, P = 0.019) during all phases. The results were similar in the third cycle during the delayed phase: 88.2% vs. 50.0% (OR 7.50, 95% CI: 1.421–39.590, P = 0.010) (Tables 2, 3 and 4), and in the whole study (OR 3.30, 95% CI: 1.414–6.452, P = 0.0033).
The CC rates were also significantly higher with mirtazapine: in the first cycle, 76.1% vs. 49.0% (OR 3.31, 95% CI: 1.376–7.983, P = 0.006) in the delayed phase and 56.5% vs. 32.7% (OR 2.68, 95% CI: 1.164–6.176, P = 0.019) during all phases; in the second cycle, 70.0% vs. 45.7% (OR 2.77, 95% CI: 0.993–7.728, P = 0.049) in the delayed phase and 50.0% vs. 25.7% (OR 2.89, 95% CI: 1.019–8.194, P = 0.043) during all phases; and in the third cycle, 88.2% vs. 50.0% (OR 7.50, 95% CI: 1.421–39.590, P = 0.010) in the delayed phase.
Nonetheless, no significant differences were identified in the incidence of nausea between the two groups (including acute, delayed, and all phases) throughout the three study cycles.
With respect to CR in the delayed phase in the first cycle, subgroup analysis demonstrated that benefits of mirtazapine were most evident in the following subgroups: age ≥ 50 years; those receiving cisplatin-containing regimens; those with an ECOG performance status of 1–2; and those taking palonosetron as a 5-HT3 RA treatment (Table 5). Multivariate analysis demonstrated that, in the first cycle, use of mirtazapine was the only independent risk factor for CR in the delayed phase of vomiting (Table 6).
Adverse events
All AEs were grade 1–2; those that occurred in ≥2% of patients are listed in Table 7. Most of the AEs, including anorexia, fatigue, and dyspepsia, were comparable between the two groups. However, somnolence (17.4% vs. 4.1%, P = 0.035) and weight gain (8.7% vs. 0, P = 0.035) occurred more frequently in the mirtazapine group than in the control group.
Quality of life
During Cycle 1, 86.3% (82/95) of patients completed the FLIE questionnaire on Days 2 and 6. In Cycles 2 and 3, 81.5% (53/65) and 76.7% (33/43) of patients, respectively, completed the questionnaire. Throughout the three cycles, there were no significant differences in mean FLIE total scores between the two arms on either Day 2 or Day 6. As shown in supplemental online Table 8, the proportion of patients who reported no impact on their daily life was similar between the two groups.
Discussion
To the best of our knowledge, this open label, multicenter, phase III trial was the first randomized, prospective study to investigate the efficacy of mirtazapine as a secondary prophylactic agent for delayed CINV following HEC. When used as a secondary prophylactic, a four-drug antiemetic regimen including mirtazapine more effectively prevented delayed CINV in patients with breast cancer who have experienced delayed vomiting than the recommended triplet regimen [3,4,5] without mirtazapine.
All patients in our study had experienced delayed vomiting before enrollment. Among patients in the control arm, the CR rate in the delayed phase was 49.0%–54.3%, whereas it was substantially and significantly better with mirtazapine. Our findings indicate that our new experimental regimen was significantly superior to standard therapy in Cycle 1 (CR rate in the delayed phase 78.3% vs. 49.0%, P = 0.003), and in Cycle 3 (88.2% vs. 50.0%, P = 0.010). Thus, our data demonstrate that addition of mirtazapine provides a benefit that will likely be sustained over several cycles of HEC.
Although in our study addition of mirtazapine substantially improved the CINV outcomes, the CR rates for the delayed phase in the control arm of the study (nearly 50%) were much lower than those reported in previous studies (approximately 70%) [6,7,8,9]. One possible explanation for this difference is that all our patients had already experienced delayed vomiting during the previous chemotherapy cycle, which could reduce the assessed impact of any subsequent antiemesis therapy. Another possible reason could be that we used a lower dose of dexamethasone in this study. In our protocol, the dose of dexamethasone was 7.5 mg orally on Days 2–4, the dose on Day 1 not being specified. In comparison, in several published antiemetic guidelines [3,4,5], the dexamethasone starting dose is higher at 12 mg and starts on Day 1. Dexamethasone can be a very effective antiemetic therapy for controlling both acute and delayed CINV; however, its potential toxicity when used for several days could be problematic. The reported AEs of insomnia (45%), indigestion/epigastric discomfort (27%), agitation (27%), diabetes, and immunosuppression are of particular concern with higher dose dexamethasone therapy [28]. In addition, physicians in China are more cautious about using dexamethasone than are physicians in other countries because of the high incidence of gastritis in China. In the PRACTICE survey [29], which enrolled 648 patients from Australia and five Asia–Pacific countries (China, India, Singapore, South Korea, and Taiwan), details of prophylaxis for the acute and delayed phase of CINV showed that dexamethasone was used less frequently in China than in Korea: 70.1% versus 88.8%, respectively, for the acute phase, and 24.7% versus 76.3%, respectively, for the delayed phase.
Post-chemotherapy nausea is always hard to control, despite significant improvements in vomiting prevention having been reported recently [17, 30]. It has been reported that olanzapine improves nausea control in patients receiving HEC. In a phase III study [31], the proportion of patients with full control of chemotherapy-induced nausea was significantly greater in the olanzapine group for all phases of post-chemotherapy nausea and vomiting than in the placebo group (for the acute phase, 74% vs. 45%, P = 0.002; for the delayed phase, 42% vs. 25%, P = 0.002; and for the overall period, 37% vs. 22%, P = 0.002)].
In this study, patients who received additional mirtazapine treatment had better complete control than the control group for the delayed phases throughout the three study cycles (first cycle: 76.1% vs. 49.0%, P = 0.006; second cycle: 70.0% vs. 45.7%, P = 0.049; third cycle: 88.2% vs. 50.0%, P = 0.010). This may indicate that mirtazapine can potentially control nausea in the delayed phase; the differences in the incidence of nausea were not statistically significant.
We found that the antiemetic regimens in both arms were well tolerated, with no grade 3/4 toxicities or serious adverse events (SAEs) related to mirtazapine. Most AEs were similar between the two groups with the exception of somnolence (17.4% vs. 4.1%, P = 0.035) and weight gain (8.7% vs. 0, P = 0.035), which both occurred more frequently in the mirtazapine group.
Somnolence is commonly induced by psychotropic agents. In previous studies, the incidence of mirtazapine-induced somnolence was 26.5% at a dose of 15 mg/day, the benefits of mirtazapine for nausea control being particularly evident in patients with cancer and sleep disturbance [19, 32]. Weight gain, a typical AE in patients with advanced breast cancer receiving chemotherapy, is paradoxically a potential benefit of mirtazapine, particularly in patients with pronounced weight loss. It remains to be shown whether the mirtazapine-associated weight gain observed in our study is a reflection of better control of chemotherapy-induced nausea and vomiting, and thus better overall nutrition during chemotherapy.
We investigated the impact on QOL using the FLIE questionnaire [26]. Both the mean total scores and the proportion of patients that experienced no impact on their daily life were similar between the two groups, showing that mirtazapine had no adverse impact on overall QOL. While it is unclear why a much smaller proportion of patients reported no impact on their daily life in both arms of our study (7.7%–22.0%) than in other similar studies (59%–75.6%) [33, 34], one possible explanation is that the patients in our study had experienced delayed emesis in the cycle of chemotherapy before enrollment. Thus, their anticipatory anxiety about vomiting prior to entry into the study may have negated the improvement in QOL induced by the higher CR to vomiting resulting from mirtazapine. Thus, it seems that mirtazapine has clear benefits for both acute and delayed nausea and vomiting, with no apparent adverse impact on QOL.
One limitation of our randomized trial is that it did not include a placebo-controlled blind arm. In addition, some patients withdrew consent during the study, mostly because of difficulties in completing the FLIE questionnaire or diary cards. However, it is unlikely that any of these limitations would have substantially influenced the study results.
Conclusions
To the best of our knowledge, this is the first randomized prospective study to show that addition of mirtazapine as a secondary prophylactic against HEC-induced delayed vomiting not only has a substantial and statistically significant benefit, but also has no serious adverse impacts on QOL in women with breast cancer who have had delayed emesis following the same prior HEC.
References
Hesketh PJ (1999) Defining the emetogenicity of cancer chemotherapy regimens: relevance to clinical practice. Oncologist. 4:191–196
Sommariva S, Pongiglione B, Tarricone R (2016) Impact of chemotherapy-induced nausea and vomiting on health-related quality of life and resource utilization: a systematic review. Crit Rev Oncol Hematol 99:13–36
Hesketh PJ, Bohlke K, Lyman GH et al (2016) Antiemetics: American Society of Clinical Oncology focused guideline update. Am Soc Clin Oncol J Clin Oncol 34(4):381–386
Roila F, Herrstedt J, Aapro M et al (2010) ESMO/MASCC guidelines. Working group. Guideline update for MASCC and ESMO in the prevention of chemotherapy and radiotherapy-induced nausea and vomiting: results of the Perugia consensus conference. Ann Oncol 21(suppl 5):232–243
NCCN National Comprehensive Cancer Network. Antiemesis: Clinical Practice Guidelines in Oncology, v 2. 2017. Available at: www.nccn.org. 2017
Takahashi T, Hoshi E, Takagi M et al (2010) Multicenter, phase II, placebo-controlled, double-blind, randomized study of Aprepitant in Japanese patients receiving high-dose cisplatin. Cancer Sci 101(11):2455–2461
Hesketh PJ, Grunberg SM, Gralla RJ et al (2003) The oral neurokinin-1 antagonist Aprepitant for the prevention of chemotherapy-induced nausea and vomiting: a multinational, randomized, double-blind, placebo-controlled trial in patients receiving high-dose cisplatin – the Aprepitant protocol 052 study group. J Clin Oncol 21:4112–4119
Poli-Bigelli S, Rodrigues-Pereira J, Carides AD et al (2003) Aprepitant protocol 054 study group. Addition of the neurokinin 1 receptor antagonist Aprepitant to standard antiemetic therapy improves control of chemotherapy-induced nausea and vomiting. Results from a randomized, double-blind, placebo-controlled trial in Latin America. Cancer 97:3090–3098
Schmoll HJ, Aapro MS, Poli-Bigelli S et al (2006) Comparison of an Aprepitant regimen with a multiple-day Ondansetron regimen, both with dexamethasone, for antiemetic efficacy inhigh-dose cisplatin treatment. Ann Oncol 17:1000–1006
Bymaster FP, Calligaro DO, Falcone JF et al (1996) Radioreceptor binding profile of the atypical antipsychotic olanzapine. Neuropsychopharmacology. 14(2):87–96
Brafford MV, Glode A (2014) Olanzapine: an antiemetic option for chemotherapy-induced nausea and vomiting. J Adv Pract Oncol 5(1):24–29
Navari RM, Aapro M (2016) Antiemetic prophylaxis for chemotherapy- induced nausea and vomiting. N Engl J Med 374(14):1356–1367
Mukhopadhyay S, Kwatra G, Alice KP et al (2017) Role of olanzapine in chemotherapy-induced nausea and vomiting on platinum-based chemotherapy patients: a randomized controlled study. Support Care Cancer 25(1):145–154
Wang X, Wang L, Wang H et al (2015) Effectiveness of olanzapine combined with Ondansetron in prevention of chemotherapy-induced nausea and vomiting of non-small cell lung cancer. Cell Biochem Biophys 72(2):471–473
Tan L, Liu J, Liu X et al (2009) Clinical research of olanzapine for prevention of chemotherapy-induced nausea and vomiting. J Exp Clin Cancer Res 28:131
Navari R, Nagy C, Le-Rademacher J et al (2016) Olanzapine versus fosAprepitant for the prevention of concurrent chemotherapy radiotherapy-induced nausea and vomiting. J Community Support Oncol 14(4):141–147
Navari RM (2013) Management of chemotherapy-induced nausea and vomiting: focus on newer agents and new uses for older agents. Drugs. 73(3):249–262
de Boer T (1996) The pharmacologic profile of mirtazapine. J Clin Psychiatry 57(Suppl 4):19–25
Nutt D (1997) Mirtazapine: pharmacology in relation to adverse effects. Acta Psychiatr Scand Suppl 391:31–37
Kast RE, Foley KF (2007) Cancer chemotherapy and cachexia: mirtazapine and olanzapine are 5-HT3 antagonists with good antiemesis effects. Eur J Cancer Care (Engl) 16(4):351–354
Rohde A, Dembinski J, Dorn C (2003) Mirtazapine (Remergil) for treatment resistant hyperemesis gravidarum: rescue of a twin pregnancy. Arch Gynecol Obstet 268:219–221
Teixeira FV, Novaretti TM, Pilon B et al (2005) Mirtazapine (Remeron) as treatment for non-mechanical vomiting after gastric bypass. Obes Surg 15:707–709
Theobald DE, Kirsh KL, Holtsclaw E et al (2002) An open-label, crossover trial of mirtazapine (15 and 30 mg) in cancer patients with pain and other distressing symptoms. J Pain Symptom Manag 23:442–447
Thompson DS (2000) Mirtazapine for the treatment of depression and nausea in breast and gynecological oncology. Psychosomatics. 41:356–369
Common Terminology Criteria for Adverse Events (CTCAE), Version 4.0, published on May 28, 2009
Lindley CM, Hirsch JD, O'Neill CV et al (1992) Quality of life consequences of chemotherapy-induced emesis. Qual Life Res 1(5):331–340
Hu W, Fang J, Nie J et al (2014) Addition of Aprepitant improves protection against cisplatin-induced emesis when a conventional anti-emetic regimen fails. Cancer Chemother Pharmacol 73(6):1129–1136
Vardy J, Chiew KS, Galica J et al (2006) Side effects associated with the use of dexamethasone for prophylaxis of delayed emesis after moderately emetogenic chemotherapy. Br J Cancer 94(7):1011–1015
Yu S, Burke TA, Chan A et al (2015) Antiemetic therapy in Asia Pacific countries for patients receiving moderately and highly emetogenic chemotherapy--a descriptive analysis of practice patterns, antiemetic quality of care, and use of antiemetic guidelines. Support Care Cancer 23(1):273–382
Ng TL, Hutton B, Clemons M (2015) Chemotherapy-induced nausea and vomiting: time for more emphasis on nausea? Oncologist. 20(6):576–583
Navari RM, Qin R, Ruddy KJ et al (2016) Olanzapine for the prevention of chemotherapy-induced nausea and vomiting. N Engl J Med 375:134–142
Kim SW, Shin IS, Kim JM et al (2008) Effectiveness of mirtazapine for nausea and insomnia in cancer patients with depression. Psychiatry Clin Neurosci 62(1):75–83
Schmitt T, Goldschmidt H, Neben K et al (2014) Aprepitant, granisetron, and dexamethasone for prevention of chemotherapy-induced nausea and vomiting after high-dose melphalan in autologous transplantation for multiple myeloma: results of a randomized, placebo-controlled phase III trial. J Clin Oncol 32(30):3413–3420
Chasen M, Urban L, Schnadig I et al (2017) Rolapitant improves quality of life of patients receiving highly or moderately emetogenic chemotherapy. Support Care Cancer 25:85–92
Acknowledgments
We thank David Warr for assistance with revising the protocol of the study, Yannan Zhao and Zhe Feng for data collection, Enying Cao for following the patients up and H. Nikki March, PhD, and Trish Reynolds, MBBS, FRACP, from Liwen Bianji, Edanz Editing China (www.liwenbianji.cn/ac), for editing the English text of a draft of this manuscript.
Funding
This study was sponsored and funded by MSD China Holding, Shanghai, China.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflicts of interest
All authors declare they have no conflicts of interest.
Ethics approval
All procedures performed in studies involving human participants were in accordance with the ethical standards of the institutional and/or national research committee and with the 1964 Helsinki Declaration and its later amendments or comparable ethical standards. The Fudan University Shanghai Cancer Center Ethic Committee for Clinical Investigation approved the study.
Informed consent
Informed consent was obtained from all study participants.
Additional information
Publisher’s note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
About this article
Cite this article
Cao, J., Ouyang, Q., Wang, S. et al. Mirtazapine, a dopamine receptor inhibitor, as a secondary prophylactic for delayed nausea and vomiting following highly emetogenic chemotherapy: an open label, randomized, multicenter phase III trial. Invest New Drugs 38, 507–514 (2020). https://doi.org/10.1007/s10637-020-00903-8
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s10637-020-00903-8