Summary
Introduction MSC1992371A is an aurora kinase inhibitor with potential antitumor activity. Methods This trial established the maximum tolerated dose (MTD) and dose-limiting toxicities (DLTs) of oral MSC1992371A given before or after gemcitabine (1,000 mg/m2) in a 21-day cycle in patients with advanced malignancies. In schedule 1 (n = 31), gemcitabine was administered on days 1 and 8 followed by escalating doses of MSC1992371A on days 2 and 9. In schedule 2 (n = 35), MSC1992371A was given on days 1 and 8 followed by gemcitabine on days 2 and 9. Patients had a range of solid tumors, the most frequent of which was colorectal (n = 19). Results In both schedules, the 37 mg/m2 dose level was defined as the MTD. The main DLT was grade 4 neutropenia. Adverse events consisted of neutropenia, thrombocytopenia, asthenia, fatigue, nausea, vomiting, anorexia, and diarrhea. Administration of MSC1992371A prior to gemcitabine had no effect on the metabolism or elimination of gemcitabine. Time to reach maximum plasma concentration and area under the plasma concentration-time curve for MSC1992371A increased proportionally with dose. Exploration of drug-target-related and tumor biomarkers did not identify predictors of biologic activity or response. Two patients (1 with lung carcinoma and 1 with hepatocellular carcinoma) had durable partial responses in schedule 2, and 5 patients had stable disease (SD) lasting 6 − 14 months. Conclusion Oral MSC1992371A can be administered at a MTD of 37 mg/m2 in combination with the standard 1,000 mg/m2 dose of gemcitabine, but hematologic toxicity requires careful monitoring. Preliminary signs of efficacy were indicated by durable responses and SD.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Aurora kinase-A, -B, and -C are specialized serine/threonine kinases that play essential roles in spindle assembly, centrosome maturation, chromosomal segregation, cytokinesis, and the tight regulation of mitosis [1, 2]. Within the aurora kinase family, the expression, distribution, and function of aurora kinase-A and -B differ according to cell cycle stage. Aurora kinase-A co-localizes with the centrosome throughout the cell cycle, whereas aurora kinase-B localizes to the centromere in prometaphase and metaphase, followed by transportation to the spindle midzone in anaphase. The aurora kinases are overexpressed in many solid tumors and aurora-kinase inhibitors (AKIs) have been recognized as potential novel anticancer agents [3, 4].
MSC1992371AFootnote 1 (formally AS703569) is an oral, adenosine triphosphate-competitive inhibitor of all 3 mammalian aurora-kinase isoforms (A, B, and C). MSC1992371A blocks cell separation by disrupting the mitotic spindle, leading to polyploidy and, ultimately, cell death. In vitro, MSC1992371A is a potent inhibitor of tumor cell growth, with half-maximal inhibitory concentration (IC50) values typically less than 100nM [5]. In vivo, the compound has demonstrated significant antitumor activity in several xenograft models including those of the pancreas, breast, colon, kidney, lung, and ovary [5]. Studies in MiaPaca-2 pancreatic and Colo-205 colorectal xenografts showed that a weekly dosing schedule offered the best therapeutic window. This type of schedule has the added advantage of flexibility in combination therapy.
Several preclinical studies (Merck Serono, data on file) evaluated the potential of combining MSC1992371A with drugs that are standards of care in the treatment of different tumors. When combined with gemcitabine, MSC1992371A showed either additive or synergistic effects in vitro in breast and lung cancer models and in vivo in pancreatic cancer models. In MiaPaca-2 pancreatic xenografts, the schedule of treatment affected the efficacy and tolerability of the combination. Oral administration of MSC1992371A 24 h before or after gemcitabine resulted in additive or synergistic antitumor activity, an effect that was not seen with concomitant dosing. Slight differences in tolerability were seen depending on whether MSC1992371A was given before or after gemcitabine.
A phase I monotherapy study of oral MSC1992371A in patients with advanced solid tumors established a maximum tolerated dose (MTD) of 74 mg/m2 per 21-day cycle [6]. The MTD was the same whether the study drug was given on days 1 and 8 every 3 weeks, or on days 1, 2, and 3 every 3 weeks. The main dose-limiting toxicity (DLT) was grade 4 neutropenia or febrile neutropenia. Maximum plasma concentrations of the drug (Cmax) and area under the concentration-time curve (AUC) increased with dose, and Cmax was reached 1.5–4 h after administration. Signs of antitumor activity were limited, with a few minor tumor responses, but no confirmed complete or partial responses were reported.
This paper presents the results of a phase I, dose-escalation, pharmacokinetics (PK), and pharmacodynamics (PD) study of MSC1992371A combined with gemcitabine in 2 different sequences in patients with advanced solid tumors.
Patients and methods
Patients
Eligible patients had a histologically or cytologically confirmed diagnosis of a solid tumor, for which gemcitabine is either approved or considered the standard of care, or a tumor for which there was no standard treatment available. All patients had measurable or assessable disease. Patients were required to be older than 18 years of age, with an Eastern Cooperative Oncology Group Performance Status (ECOG PS) of less than 2, and adequate renal, hepatic, and bone marrow function. Prior treatment with gemcitabine was permitted. Other inclusion and exclusion criteria routinely used in phase I studies were also applied.
Study objectives
The primary objective of this phase I trial was to determine the MTD of MSC1992371A when given in combination with a standard fixed dose of 1,000 mg/m2 gemcitabine. As a result of preliminary evidence of schedule-dependent tolerability in preclinical models, this trial investigated 2 sequences of drug administration: oral MSC1992371A was administered 24 h after gemcitabine infusion (schedule 1), or 24 h before gemcitabine infusion (schedule 2). Secondary objectives included preliminary evaluation of safety, PK, PD, and antitumor activity of the agents administered according to the 2 dosing schedules.
Study design
This was a phase I, open-label, 2-schedule trial with escalating doses of MSC1992371A and a fixed dose of gemcitabine. The trial was conducted in 2 centers in France and 1 center in Belgium.
Sequential cohorts of 3–6 patients were enrolled in parallel in 2 schedules (Fig. 1). In schedule 1, gemcitabine was administered on days 1 and 8 and MSC1992371A on days 2 and 9. In schedule 2, the sequence was reversed, with MSC1992371A being administered on days 1 and 8 and gemcitabine on days 2 and 9. Patients were assigned to each schedule centrally. The dose of gemcitabine was fixed at 1,000 mg/m2, given as a 30-min infusion. MSC1992371A was administered orally at a starting dose of 10 mg/m2/day. Dose escalation proceeded with an increment of 50 % to the second dose level and 40 % to the third level, followed by increments of 30 % to the fourth and subsequent levels until DLTs occurred and the MTD could be defined. When DLTs occurred, the dose of MSC1992371A was reduced to the preceding dose level. The protocol did not allow for further dose reductions. The dose of gemcitabine could be reduced or omitted, if required due to toxicity, according to instructions in the Summary of Product Characteristics. Treatment with MSC1992371A and gemcitabine was continued until the patient experienced progressive disease and/or unacceptable toxicity, or withdrew consent. If there were no further DLTs, dose escalation proceeded and was conducted independently for each schedule based on the observed DLTs.
The trial was conducted in accordance with the International Conference on Harmonization guidelines for Good Clinical Practice, the Declaration of Helsinki, and applicable local regulations. The study, including the patient-information and consent forms used, was approved by the independent ethics committees of participating centers. Patients provided written informed consent. The study sponsor was Merck Serono S.A., Geneva.
Definition of dose-limiting toxicities and maximum tolerated dose
DLTs were evaluated during the first cycle. A DLT, graded according to Common Terminology Criteria for Adverse Events (CTCAE) version 3.0, was defined as any of the following: grade 4 neutropenia lasting at least 7 days; grade 4 thrombocytopenia (or grade 3 with bleeding); febrile neutropenia and any other grade 3 or 4 non-hematologic toxicity (excluding grade 3 increase in alanine aminotransferase, aspartate aminotransferase, or alkaline phosphatase reversible within 7 days, and grade 3 vomiting and/or nausea if encountered with non-optimal therapy); or any grade 2 or greater neurologic toxicity.
If more than 1 out of 3 (or 1 out of 6) patients experienced a DLT at a given dose during cycle 1, up to 12 additional patients were enrolled at the preceding dose level, which was considered to be the MTD.
Safety assessments
In addition to DLTs, adverse events (AEs) were recorded according to CTCAE v.3.0 criteria throughout the period of treatment until 31 ± 3 days after the last administration of the study drug. Treatment-emergent adverse events (TEAEs) were defined as AEs that started or worsened in the period from the first day of drug administration to 28 days after the last drug administration (inclusive). Changes from baseline were assessed for laboratory parameters, vital signs, physical exam, ECG, and echocardiography (or multiple gated acquisition scans).
Pharmacokinetic and pharmacodynamic assessments
To investigate PK, plasma and urine concentrations of MSC1992371A and gemcitabine (including its inactive metabolite dFdU and main active metabolite dFdCTP) were determined at pre-specified time points after the first dose in each schedule. For schedule 1, blood samples were collected immediately prior to dosing and 1, 2, 3, 4, 6, and 8 h after administration of oral MSC1992371A. For schedule 2, blood samples were collected immediately prior to dosing and 1, 2, 3, 4, 6, 8, 24, 28, and 32 h after administration of oral MSC1992371A. The renal excretion of MSC1992371A was determined from urine samples collected at 0–4 and 4–8 h in schedule 1 and 0–4, 4–8, 8–24, and 24–32 h in schedule 2. Plasma concentrations of gemcitabine were determined from blood samples taken before and at 0.25, 0.5, 0.75, 1, 2, and 8 h following infusion.
Plasma and urine concentrations of MSC1992371A were determined using a validated liquid chromatography-mass spectrometry (LC-MS) method with a lower limit of quantification (LLoQ) of 0.05 ng/mL and a linearity ranging from 0.05 to 10.00 ng/mL for human plasma and urine. Plasma concentration of gemcitabine was calculated using a validated high performance LC-MS/MS method with a LLoQ of 0.05 ng/mL and a linearity ranging from 0.5 to 1,000 ng/mL. PK parameters were calculated using non-compartmental methods (Kinetica™ Program Version 4.4.1).
A series of PD parameters was assessed to explore early markers and potential predictors of toxicity and response. Levels of circulating tumor cells (CTCs) were measured in whole blood and gene expression profiles were obtained from peripheral blood mononuclear cells (PBMCs). Markers of cell death (cytokeratin 18 and cleaved cytokeratin 18) and levels of phosphorylated ERK downstream of FLT3 were also measured in PBMCs to obtain evidence of target-related drug activity. Archived tissue from the primary tumor and/or metastases (where available) was analyzed by immunohistochemistry to determine the levels of expression of aurora kinase-A and -B and p53. The copy number of the aurora kinase-A and -B genes and p53 gene deletion were assessed by fluorescence in situ hybridization.
Tumor response
Tumor response was evaluated at the end of every second cycle according to Response Evaluation Criteria In Solid Tumors (RECIST) v1.0 [7].
Statistical methods
The trial design followed the well-established methodology used in dose-finding studies in oncology [8]. The main analytic tools used were descriptive statistics and graphical representations (SAS® version 9.1.3). Continuous variables were tabulated using the following summary statistics: number of values, mean, standard deviation, median, and minimum and maximum. Continuous variables were categorized, when applicable, into grouped intervals for analysis with frequencies and percentages. Categorical variables were tabulated using frequencies and percentages.
Results
Patient characteristics
A total of 66 patients were enrolled; 31 patients assigned to schedule 1 received treatment over 6 dose levels that rose progressively from 10–49 mg/m2, and 35 patients assigned to schedule 2 were treated at 5 dose levels that increased from 10–37 mg/m2. The median age was 60 years (range 20–80 years), 72 % of patients were male, and 55 % had an ECOG PS of 0 (Table 1). Patient characteristics were comparable in both groups, with a higher proportion of patients with ECOG PS 1 in schedule 1 (58 %) than in schedule 2 (34 %). The median time from diagnosis of the primary tumor was 2 years, and the median time from last relapse or tumor progression was less than 2 months. Patients had various malignancies, the most frequent being colorectal (29 %) and pancreatic adenocarcinoma (12 %), which were represented comparably in both schedules. The number of prior lines of chemotherapy (including neoadjuvant and adjuvant treatment) ranged from 1 to 8, with a median of 3 prior regimens in both schedules.
Dose-limiting toxicities and maximum tolerated dose
Full data are presented in Table 2.
Schedule 1
At a dose of 37 mg/m2/day of MSC1992371A, 1 out of 3 patients experienced grade 4 neutropenia lasting more than 7 days, and grade 4 thrombocytopenia during cycle 1. The cohort was therefore expanded to 6 patients; as no further DLTs occurred, dose escalation proceeded. At a dose of 49 mg/m2/day, 2 patients had grade 4 neutropenia lasting more than 7 days. In line with the study protocol, the previous dose level (37 mg/m2) was defined as the MTD and a further 6 patients were recruited to better define the tolerability of MSC1992371A. Of these patients, 2 experienced febrile neutropenia in cycle 1. In summary, a total of 5 patients experienced severe hematologic toxicity in cycle 1, defined as grade 4 neutropenia lasting for more than 7 days or febrile neutropenia; this toxicity occurred at a dose of 49 mg/m2 in 2 out of 6 patients and at 37 mg/m2—the defined MTD—in 3 out of 12 patients.
Schedule 2
Of the first 3 evaluable patients who received 10 mg/m2/day of MSC1992371A, 1 developed grade 4 neutropenia on day 3 and died as a consequence of multi-organ failure, suggesting severe sepsis from a pre-existing condition. An additional 3 patients were recruited at this dose, none of whom experienced a DLT. At the next dose levels (15 mg/m2 and 28 mg m2), 1 of 6 patients had a DLT at each dose (grade 3 worsening of performance status and asthenia at 15 mg/m2, grade 4 neutropenia lasting for more than 7 days at 28 mg/m2 ). At 37 mg/m2, 1 of the first 3 patients developed a DLT of grade 4 neutropenia lasting more than 7 days. In the expanded cohort of 6 patients, 3 patients experienced grade 4 neutropenia in cycle 1 lasting less than 7 days, and therefore, not meeting the DLT criteria. These cases of hematologic toxicity were considered clinically significant and dose escalation was stopped. In addition, 1 episode of grade 4 febrile neutropenia was observed in this dose cohort. Therefore, similar to schedule 1, 37 mg/m2 was defined as the MTD for schedule 2.
Safety evaluation across cycles
Patients treated according to schedule 1 received a total of 92 complete cycles, with a median of 2 cycles (range 0–16 cycles). In schedule 2, a total of 124 cycles were delivered, with a median of 3 cycles (range 0–11 cycles). The median overall compliance with gemcitabine was 99 % in schedule 1 and 92 % in schedule 2. Twelve patients in schedule 1 and 18 patients in schedule 2 did not receive either drug (gemcitabine or MSC1992371A) on day 8/9 in at least 1 cycle. Neutropenia was the main reason for toxicity-related dose omission. No consistent pattern of increased need for gemcitabine dose reduction or omission with escalating doses of MSC1992371A was found.
In both schedules, grade 3–4 hematologic toxicity, in particular grade 4 neutropenia, was predominant at doses of 28 mg/m2, or higher, of MSC1992371A. Grade 3–4 neutropenia occurred in 10 out of 12 (83 %) patients treated at 37 mg/m2 according to schedule 1, and in 5 out of 6 (83 %) patients treated at 28 mg/m2 according to schedule 2.
Hematologic toxicity by schedule is summarized in Table 3. Overall, the occurrence of grade 4 neutropenia was similar for both schedules, affecting 39 % and 34 % of patients on schedule 1 and 2, respectively. Febrile neutropenia was reported in 4 patients on schedule 1 (2 at 39 mg/m2 and 2 at 49 mg/m2) and in 1 patient on schedule 2 (at 37 mg/m2). Grade 3–4 anemia was less frequent, occurring in 19 % of patients on schedule 1 and 17 % of patients on schedule 2; grade 4 anemia occurred in only 1 (3.2 %) patient on schedule 1. Grade 3 thrombocytopenia occurred in 13 % of patients on schedule 1, while no patients experienced grade 4 neutropenia. With schedule 2, 6 % of patients had grade 3 thrombocytopenia and 11 % had grade 4. Although most cases occurred at a dose of 28 mg/m2 or higher, there was no clear dose effect.
Table 4 shows non-hematologic treatment-emergent AEs (TEAEs) experienced by 10 % or more of patients in at least 1 schedule. The majority of TEAEs were grade 1 or 2. The most common grade 3–4 TEAEs were asthenia and dyspnea. Grade 3 or 4 asthenia occurred more frequently in patients on schedule 1 (26 %) than on schedule 2 (9 %).
Six patients died during the trial. Two patients treated according to schedule 1 died due to disease progression while on study treatment. Two patients on schedule 2 died while on treatment; both deaths were due to sepsis and were considered related to study treatment (MSC1992371A 10 mg/m2/day). In addition, 2 patients died in the 28-day post-treatment follow-up period from ischemic stroke and upper gastrointestinal hemorrhage; both deaths were not considered to be treatment related.
Pharmacokinetics
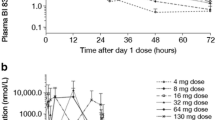
The mean plasma concentration-time curves for the first dose of MSC1992371A at each dose level (in schedule 2) are shown in Fig. 2. Maximal plasma concentrations were reached between 1 and 3 h (range 1–6 h) after administration. Cmax and drug exposure (area under the plasma concentration curve from administration to last observed concentration at t [AUC 0−t]) increased with increasing doses of MSC1992371A. The interindividual variability in rate of absorption (Cmax and time to maximum concentration [tmax]) and extent of exposure (AUC 0−t) was 54 %, 70 %, and 51 % for schedule 1 and 52 %, 69 %, and 58 % for schedule 2.
Mean (SD) plasma concentrations over time after a single dose of MSC1992371A (schedule 2, day 1). SD, standard deviation
For schedule 1, PK samples were obtained only up to 8 h post-administration. Applying non-compartmental analysis, the terminal half-life, area under the concentration-time curve from zero to infinity (AUC0−∞), clearance, and volume of distribution of MSC1992371A could not be estimated reliably, as the extrapolated part of the exposure (AUCextra) exceeded 20 % of the total exposure. For schedule 2, PK samples were obtained up to 32 h post-administration, which enabled the estimation of further relevant PK parameters. In a subset of patients with evaluable PK profiles treated according to schedule 2, MSC1992371A had a geometric mean terminal half-life in the range 9.4–13.7 h, geometric mean apparent clearance (CL/f) of 50–213 L/h, and an apparent volume of distribution (Vz/f) of 988–3594 L by dose group. Urinary PK data implied that renal excretion was only of minor importance in the elimination of MSC1992371A (data not shown).
Mean calculated PK parameters for MSC1992371A administered at the MTD of 37 mg/m2/day (both schedules) are summarized in Table 5. For gemcitabine, the plasma concentration profiles and other relevant PK parameters in patients treated according to schedule 2 were similar to those in patients treated on schedule 1, indicating that administration of MSC1992371A prior to gemcitabine has no effect on the metabolism or elimination of the drug.
Pharmacodynamics
Analysis of blood and tissue biomarkers described in the Methods section did not provide any consistent evidence of modulation by MSC1992371A either in the study population as a whole or in individual patients. This could be attributed partly to the inability to fully investigate those markers as a result of the limited number of samples, technical difficulties related to sample quality, and lack of appropriate validation for some of the assays used. Since few patients showed a tumor response, potential predictors of the activity of MSC1992371A in combination with gemcitabine could not be explored.
Antitumor activity
Signs of antitumor activity were observed in patients with different types of tumors, with 5 patients showing substantial tumor shrinkage.
Two (7 %) patients treated according to schedule 2 had a partial response (PR) as per RECIST v1.0. One patient, with non-small cell lung cancer (NSCLC) that had responded previously to gemcitabine in combination with oxaliplatin, who was treated for 10 cycles at 15 mg/m2/day had a PR in cycle 2 lasting for 6 months. Another patient, with hepatocellular carcinoma with liver and lymph-node lesions, who received 11 cycles of MSC1992371A at the MTD of 37 mg/m2/day, had a PR after 6 cycles of treatment. In addition, 2 patients had significant tumor shrinkage with prolonged stable disease (SD). One patient, with adenocarcinoma of the gastroesophageal junction, had SD for over 9 months (12 cycles) and sustained tumor shrinkage (maximum −29 % by RECIST). The second patient, with locally advanced pancreatic adenocarcinoma, had SD for more than 7 months (11 cycles) and sustained tumor shrinkage (maximum of −22 % by RECIST). In schedule 1, one patient with locally advanced spinocellular skin carcinoma invading the eye treated at 37 mg/m2 MSC1992371A had an unconfirmed PR after 3 cycles of treatment.
In addition, there were 3 cases of prolonged tumor stabilization, with patients remaining on treatment for between 6 and 14 months. Although these patients had tumor types that are generally considered slow-growing (parotid cylindroma, chondrosarcoma, and cholangiocarcinoma) and no substantial tumor shrinkage was noted, such prolonged periods of SD in patients with documented progression at study entry are indicative of drug activity and are clinically relevant.
Discussion
The family of aurora kinases has been linked to tumorigenesis through its role in regulating mitosis, and the aurora kinase inhibitor, MSC1992371A, has shown some evidence of antitumor activity in single-agent phase I studies [6, 9]. Preclinical data suggested additive or synergistic effects when combined with gemcitabine, and the possibility that these effects are schedule dependent. This study was therefore designed to determine the MTD when administering MSC1992371A 24 h before or after gemcitabine at the same dose once per week for the first 2 weeks of a 21-day treatment cycle. While the dose of MSC1992371A was escalated until the occurrence of DLTs, that of gemcitabine remained at the standard dose of 1,000 mg/m2/day (unless dose reduction was required due to toxicity).
When given with a fixed dose of gemcitabine, the MTD of MSC1992371A, defined as the dose below the one at which more than 1 out of 3, or 1 out of 6, patients had a protocol-defined DLT in the first cycle, was 37 mg/m2 in both schedules. This MTD is the same as that obtained for MSC1992371A given as a single agent, however, clinically significant hematologic toxicity with febrile and grade 4 neutropenia was observed in patients treated at this dose.
Single-agent gemcitabine is not considered particularly hematotoxic. The neutropenia seen in combination with the AKI may, therefore, indicate an additive or synergistic effect on bone marrow cells. Overall, the main toxicities observed, including asthenia, fatigue, and neutropenia, did not show a strong relationship to the dose of MSC1992371A.
Although exposure to MSC1992371A increased overall with rising dose, the PK profiles showed moderate to high variability between patients, as has been seen for other oral anticancer drugs including kinase inhibitors [10]. The hematologic toxicity reported with the combination of MSC1992371A and gemcitabine was not associated with any significant change in the PK of either drug. The PK of gemcitabine, in particular, seemed unaffected by prior administration of the AKI.
A number of PD parameters including markers of pathway modulation and cell death, circulating tumor cells, and gene expression were assessed with the aim of exploring drug activity and potential predictors of toxicity and response. However, the study found no consistent evidence of PD activity associated with the administration of MSC1992371A.
Several other AKIs have been investigated in phase I trials in both solid and hematologic malignancies. Recently, Schoffski et al assessed the aurora kinase-A and -B inhibitor PF-03814735 in patients with advanced solid tumors [11]. They found that the agent had manageable toxicities, but produced very limited evidence of antitumor effects as assessed by FDG-PET or clinical activity. Similar to the present study, the DLT was neutropenia. Neutropenia was also dose limiting in the phase I study of danusertib in patients with advanced or metastatic solid tumors [12].
In patients with a range of advanced hematologic malignancies, MSC1992371A achieved clinically meaningful responses. However, these responses occurred at doses associated with severe neutropenia and gastrointestinal toxicities, leading to dose reductions [9]. Other AKIs have shown a comparable toxicity profile, although with the selective aurora kinase-B inhibitor barasertib, complete responses and PRs in acute myeloid leukemia patients were obtained at tolerable doses [13, 14].
Patients enrolled in this phase I study had a range of advanced solid tumor types; 42 % had tumors (such as cancer of the pancreas, NSCLC, and sarcomas) for which gemcitabine is indicated or has demonstrable activity. Others had refractory disease with no other options for therapy. In this extensively pretreated population, there were signs of antitumor activity with the gemcitabine/MSC1992371A combination, irrespective of prior gemcitabine treatment. Among the 66 patients enrolled, there were 2 confirmed PRs, one unconfirmed PR, and 5 cases of SD lasting for at least 6 months. In 2 of these cases, significant tumor shrinkage was noted. Cases of disease control were not confined to patients with tumors known to be sensitive to gemcitabine. However, there was no clear association between the dose of study drug administered and signs of clinical benefit.
In summary, this phase I study in patients with solid tumors showed that MSC1992371A can be administered safely at its MTD before or after a standard 1,000 mg/m2 dose of gemcitabine. The combination did not lead to a significant PK interaction. Hematologic toxicities predominated but were generally reversible; grade 4 neutropenia was the main DLT. In an effort to limit this toxicity, further trials could investigate either a lower dose of the AKI or the supportive use of hematopoietic growth factors (HGF). One concern with using a lower dose, however, is that (given the large PK variability observed) a subset of patients may not experience therapeutic drug levels. The addition of HGF was tested with another AKI and allowed only minor dose escalation, without obvious clinical benefit [15]. In terms of antitumor activity, signals were observed indicating that the combination of MSC1992371A with gemcitabine may have clinically meaningful activity. However, while this study reached its stated objectives by establishing the MTD and defining the safety of the gemcitabine/MSC1992371A combination, it did not identify a tumor type that is particularly sensitive and suited to further investigation.
Notes
The compound is also known as R763. Rights to this compound are currently owned by Rigel Pharmaceuticals Inc, South San Francisco, CA, USA.
References
Karthigeyan D, Prasad SB, Shandilya J, Agrawal S, Kundu TK (2011) Biology of Aurora A kinase: implications in cancer manifestation and therapy. Med Res Rev 31:757–793
Katayama H, Brinkley WR, Sen S (2003) The Aurora kinases: role in cell transformation and tumorigenesis. Cancer Metastasis Rev 22:451–464
Keen N, Taylor S (2004) Aurora-kinase inhibitors as anticancer agents. Nat Rev Cancer 4:927–936
Kollareddy M, Zheleva D, Dzubak P, Brahmkshatriya PS, Lepsik M, Hajduch M (2012) Aurora kinase inhibitors: progress towards the clinic. Invest New Drugs 30:2411–2432
McLaughlin J, Markovtsov V, Li H et al (2010) Preclinical characterization of Aurora kinase inhibitor R763/AS703569 identified through an image-based phenotypic screen. J Cancer Res Clin Oncol 136:99–113
Mita M, Gordon M, Gianella-Borradori A, Longerey B, Rejeb N, Mendelson D (2009) Phase I study of 2 dosing regimens of AS703569, an oral Aurora kinase inhibitor, in patients with solid tumors. Mol Cancer Ther 8 Suppl 1: Abstract C195
Therasse P, Arbuck SG, Eisenhauer EA et al (2000) New guidelines to evaluate the response to treatment in solid tumors. European Organization for Research and Treatment of Cancer, National Cancer Institute of the United States, National Cancer Institute of Canada. J Natl Cancer Inst 92:205–216
Storer BE (2001) Choosing a phase I design. In: Crowley J (ed) Handbook of statistics in clinical oncology, 1st edn. Dekker, New York, pp 73–91
Sonet A, Graux C, Maertens J, et al (2008) Phase 1, dose-escalation study of 2 dosing regimens of AS703569, an inhibitor of aurora and other kinases, administered orally in patients with advanced haematological malignancies. Blood (ASH Annual Meeting Abstracts) 112: Abstract 2963
van Erp NP, Gelderblom H, Guchelaar HJ (2009) Clinical pharmacokinetics of tyrosine kinase inhibitors. Cancer Treat Rev 35:692–706
Schoffski P, Jones SF, Dumez H et al (2011) Phase I, open-label, multicentre, dose-escalation, pharmacokinetic and pharmacodynamic trial of the oral aurora kinase inhibitor PF-03814735 in advanced solid tumors. Eur J Cancer 47:2256–2264
Steeghs M, Eskens FA, Gelderblom H et al (2009) Phase I pharmacokinetic and pharmacodynamic study of the aurora kinase inhibitor danusertib in patients with advanced or metastatic solid tumors. J Clin Oncol 27:5094–5101
Löwenberg B, Muus P, Ossenkoppele G et al (2011) Phase 1/2 study to assess the safety, efficacy, and pharmacokinetics of barasertib (AZD1152) in patients with advanced acute myeloid leukemia. Blood 118:6030–6036
Tsuboi K, Yokozawa T, Sakura T et al (2011) A Phase I study to assess the safety, pharmacokinetics and efficacy of barasertib (AZD1152), an Aurora B kinase inhibitor, in Japanese patients with advanced acute myeloid leukemia. Leuk Res 35:1384–1389
Cohen RB, Jones SF, Aggarwal C et al (2009) A phase I dose-escalation study of danusertib (PHA-739358) administered as a 24-hour infusion with and without granulocyte colony-stimulating factor in a 14-day cycle in patients with advanced solid tumors. Clin Cancer Res 15:6694–6701
Acknowledgments
The trial was sponsored by Merck Serono S.A., Geneva. Currently, Rigel Pharmaceuticals Inc, CA, USA, owns the rights to MSC1992371A (R763). The authors would like to thank the patients and their families, and the many staff at the hospitals involved, who contributed such valuable work. Editorial and writing assistance was provided by Rob Stepney, TRM Oncology, The Hague, The Netherlands, funded by Merck KGaA, Darmstadt, Germany.
Ethical standards
The trial was conducted in accordance with the International Conference on Harmonization guidelines for Good Clinical Practice, the Declaration of Helsinki, and applicable local regulations. The study, including the patient-information and consent forms used, was approved by the independent ethics committees of participating centers. Patients provided written informed consent.
Conflict of interest
E Raymond, J Alexandre, S Faivre, T Besse-Hammer, and A Awada have no relevant interests to disclose. F Goldwasser is consultant for Merck Serono S.A., Geneva, Switzerland. A Gianella-Borradori and L Trandafir were employees of Merck Serono S.A., Geneva, Switzerland. N Rejeb and V Jego are current employees of Merck Serono S.A., Geneva, Switzerland.
Financial support
The study was sponsored by Merck Serono S.A. – Geneva, Geneva, Switzerland. Editorial and writing assistance was funded by Merck KGaA, Darmstadt, Germany.
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Raymond, E., Alexandre, J., Faivre, S. et al. A phase I schedule dependency study of the aurora kinase inhibitor MSC1992371A in combination with gemcitabine in patients with solid tumors. Invest New Drugs 32, 94–103 (2014). https://doi.org/10.1007/s10637-013-9950-y
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s10637-013-9950-y