Summary
Salinomycin (Sal) is potentially useful for the treatment of cancer. The present study examined a novel mechanism of Sal sensitization in cancer cells. Sal sensitized radiation-treated cancer cells by inducing G2 arrest and causing DNA damage. Sal treatment also reduced p21 levels in radiation-treated cells. Considering that Sal sensitizes doxorubicin (DOX)- or etoposide (ETO)-treated cancer cells by causing DNA damage and reducing p21 expression, the results from our study suggest that the mechanism underlying Sal sensitization is conserved in both chemo- and radiation-treated cells. We also tested the ability of Sal to inhibit p-glycoprotein (P-gp), which plays a role in the efflux of anti-cancer drugs to reduce cellular damage. In particular, we compared Sal to verapamil (Ver), a well-known P-gp inhibitor. Sal inhibits P-gp with a different substrate distinct from that of Ver. In addition, Sal sensitized Ver-resistant cells, indicating that this compound is more effective for sensitizing than Ver. Taken together, the results from our study may contribute to the development of Sal-based therapy for cancer patients treated with P-gp-inhibiting drugs or radiation therapy.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Salinomycin (Sal) was originally used to kill bacteria, fungi, and parasites [1, 2]. More recently, it has been shown to inhibit tumor stem cells [3]. Sal is currently considered to be a potential anti-cancer drug for cancer chemoprevention.
Multidrug resistance (MDR) is one of the major failures of drug-based therapy [4]. Efflux pump p-glycoprotein (P-gp) can increase the removal of anti-cancer drugs from the cell to reduce cellular damage [5, 6]. Sal also functions as a P-gp inhibitor to overcome apoptosis resistance in human cancer cells, including leukemia stem cell-like cells [7–11]. Sal also inhibits chemoresistant cancer cells [12, 13] and sensitizes DOX- or ETO-treated cancer cells by increasing apoptosis by causing DNA damage and reducing p21 protein levels through increased proteasome activity [14].
Identifying another mechanism(s) underlying Sal sensitization of cancer cells would be an important step in developing Sal-based pharmacological combination cancer chemotherapy. It is also of interest to examine the effects of Sal sensitization in combination with non-chemotherapeutic agents such as radiation. Here, we demonstrate that Sal can sensitize radiation-treated cancer cells through a mechanism similar to the one seen in DOX- or ETO-treated cells. Sal could also utilize another type of P-gp substrate independent of verapamil (Ver), a well-characterized P-gp inhibitor. These results may contribute to the development of Sal-based therapy for cancer patients.
Materials and methods
Reagents
Sal, Ver, and 5(6)-carboxyfluorescein diacetate (CFDA) were purchased from Sigma-Aldrich (St. Louis, MO). Rhodamine123 (Rho) was purchased from Santa Cruz Biotechnology (Santa Cruz, CA).
Antibodies
Antibody against p21 was obtained from Cell Signaling Technology (Danvers, MA). Antibody against glyceraldehyde 3-phosphate dehydrogenase (GAPDH) was purchased from Santa Cruz Biotechnology. Antibodies against p53BP1 and pH2AX were obtained from Abcam (Cambridge, UK).
Cell culture
Previously described human cancer cell lines [14–16] were used. MCF7 cells were acquired from Dr. Kim Hyung Sik (Pusan University, South Korea). The Hs578T breast cancer cell line was obtained from the Korean Cell Line Bank (Seoul, South Korea). The cell lines were cultured in DMEM or RPMI1640 containing 10% fetal bovine serum (FBS), 100 U/mL penicillin, and 100 μg/mL streptomycin (WelGENE, Daegu, South Korea).
Radiation treatment
Cells grown in 60 mm-diameter dishes or chamber slides were irradiated with graded doses of γ-rays using a Gammacell 1000 Elan system (MDS Nordion, Inc., Ontario, Canada) at a dose of 2 Gy or 4 Gy as determined by thermoluminescence dosimetry for the specific system employed. After irradiation, the cells were treated with the indicated drugs for the prescribed times.
Trypan blue dye exclusion test
Trypan blue staining was performed to determine the number of viable cells and cellular proliferation. Briefly, cells grown in 60 mm-diameter dishes were washed with 5 mL of phosphate buffered saline (PBS), trypsinized, and pelleted by centrifugation for 1 min at 3000 rpm. The pellet was suspended in 500 μL of cell culture medium and Trypan blue was added to the cell suspension. The number of dye-excluding (viable) cells and stained (dead) cells were counted using a hematocytometer. All experiments were performed more than twice in triplicate.
Immunocytochemistry
Cells were plated in chamber slides, incubated for 24 h, and treated as indicated in the text. They were then re-incubated. The cells were then fixed for 10 min with 3% formaldehyde, and permeabilized for 20 min at room temperature (RT) in PBS containing Triton X-100 and bovine serum albumin (BSA). The permeabilized cells were incubated with pH2AX and p53BP1 primary antibodies overnight at 4°C. They were then incubated with Green-fluorescent Alexa Fluor 488 secondary antibody (Invitrogen, Carlsbad, CA), Orange-Red-fluorescent Alexa Fluor 568 secondary antibody (Invitrogen), and staining with 4′-6-diamidino-2-phenylindole (DAPI) for 1 h at 37°C. The stained cells were examined using a LSM 510 META inverted confocal microscope (Carl Zeiss, Oberkochen, Germany) with a 40× water immersion objective lens (Carl Zeiss C-Apochromat NA 1.2) coupled with three optical zoom [14, 15]. We performed more than two independent tests.
Fluorescence-activated cell sorting (FACS) analysis
Cells grown in 60 mm-diameter dishes were treated with the indicated drugs for the prescribed times. The cells were then dislodged by trypsin, and the entire volume was centrifuged to collect the cells. The pelleted cells were washed thoroughly with PBS, suspended in 75% ethanol for at least 1 h at 4°C, washed again with PBS, and re-suspended in a cold propidium iodide (PI) staining solution (100 μg/mL RNase A and 50 μg/mL PI in PBS) for 40 min at 37°C. The stained cells were analyzed for relative DNA content using a FACSCalibur flow cytometry system (BD, Franklin Lakes, NJ). We performed more than two independent tests.
Western blot analysis
Total cellular proteins were extracted using a previously described trichloroacetic acid (TCA) method [17]. Briefly, cells grown in 60 mm-diameter dishes were washed three times with 5 mL PBS. Next, 500 μL of 20% trichloroacetic acid (TCA) were added to each plate. The cells were then dislodged by scraping and transferred to Eppendorf tubes. Proteins were pelleted by centrifugation for 5 min at 3000 rpm and resuspended in 1 M Tris-HCl (pH 8.0) buffer. The total protein concentrations were estimated. The proteins were resolved by sodium dodecyl sulfate-polyacrylamide gel electrophoresis (SDS-PAGE) and subjected to Western blot analysis as previously described [17].
Rho and CFDA uptake tests
Tests to measure the inhibition of P-gp were performed using a previously described method [18–20]. Briefly, cells grown in wells of 6-well plates were treated with the indicated drugs for 24 h at 37°C. The cells were then incubated with 1 μg/mL Rho or 10 μM CFDA for 90 min at 37°C. The medium was removed and the cells were washed twice with PBS. The stained cells were subsequently examined using an inverted fluorescence microscope. The stained cells were also analyzed using a FACSCalibur flow cytometry system. We performed more than two independent tests.
Annexin V analysis
Annexin V-fluorescein isothiocynate (FITC) staining was performed using a commercial Annexin V-FITC kit (BD Bioscience). Briefly, cells were harvested as described for the FACS analysis. Cells (1 × 105) in 100 μL binding buffer were incubated with 5 μL of Annexin V-FITC and 5 μl of PI (50 μg/mL) for 15 min at RT. The stained cells were analyzed using a FACSCalibur flow cytometry system.
Terminal transferase dUTP nick end labeling (TUNEL) Assay
TUNEL analysis was conducted with FITC-anti-BrdU staining using a commercial APO-BRDU kit (Phoenix Flow Systems, San Diego, CA). Briefly, cells were harvested as described for the FACS analysis. Cells (1 × 106) were fixed in 1% paraformaldehyde with PBS (pH 7.4). Next, 5 mL of 70% ethanol was added and the cells were stored for 20 h at −20°C. The cells were harvested by centrifugation, washed in buffer, resuspended in a DNA labeling solution consisting of TdT Reaction Buffer, TdT Enzyme, and BrdUTP; and incubated for 60 min at 37°C. The cells were rinsed with 1.0 mL of rinse buffer, and incubated with FITC-anti-BrdU antibody for 30 min at RT. After the incubation, 0.5 mL of a PI/RNase A staining solution was added and the cells were incubated for 15 min at RT. The stained cells were analyzed using a FACSCalibur flow cytometry system.
Statistical analysis
The data are presented as the mean ± standard deviation (S.D.). Statistical analysis was conducted using Student’s t-test and a one-way analysis of variance (ANOVA) followed by a multiple-comparison test. Results were considered to be statistically significant compared to the control (*) when P < 0.05.
Results
Sal sensitizes radiation-treated cancer cells and increases the G2 phase
We tested whether co-treatment with Sal reduces the proliferation of radiation-treated cancer cells. Reduced proliferation was evident in irradiated Hs578T cells treated with both 2.5 μM and 5 μM of Sal (4 Gy+Sal -2.5 and 4 Gy+Sal -5) compared to corresponding cells treated solely with either radiation or Sal (Fig. 1a). This result was confirmed by observing decreased numbers of co-treated Hs578T cells (Fig. 1b). Sal also reduced the number of irradiated MCF7 cells (Fig. 1b), indicating that Sal generally sensitizes radiation-treated cancer cells with an additive effect.
Sal sensitizes radiation-treated cancer cells and increases the G2 phase. a Upper panels: Hs578T were grown and treated with 4 Gy of radiation, 2.5 μM Sal (Sal-2.5), 2.5 μM Sal with 4 Gy of radiation (4 Gy+Sal-2.5), or DMSO (Con). Lower panels: Hs578T were grown and treated with 4 Gy of radiation, 5 μM Sal (Sal-5), 5 μM Sal with 4 Gy of radiation (4 Gy+Sal-5), or DMSO (Con). After 24 h, all cells were observed using an inverted microscope with 10× objective lens. b Hs578T and MCF7 cells were grown on 60 mm-diameter dishes and then treated with 4 Gy of radiation (grey bar), 5 μM Sal (Sal-5; white bar with dots), 5 μM Sal with 4 Gy of radiation (4 Gy+Sal-5; white bar), or DMSO (Con; black bar). After 24 h, cell proliferation was assessed using the Trypan blue dye exclusion test. The data represent the mean ± S.D. of at least three experiments; *P < 0.05 compared to the corresponding control. c Hs578T (upper panels) and MCF7 cells (lower panels) were grown on 60 mm-diameter dishes and treated with 4 Gy of radiation, 5 μM Sal (Sal-5), 5 μM Sal with 4 Gy of radiation (4 Gy+Sal-5), or DMSO (Con). After 24 h, FACS analysis was performed
FACS analysis demonstrated that co-treatment with radiation and Sal greatly increased the G2 interval in both Hs578T and MCF7 cells (Fig. 1c), suggesting that cellular division arrest in the G2 phase contributes to the sensitization of Sal in irradiated cells. Annexin V staining and a TUNEL assay were also performed to measure apoptosis. Co-treatment with 4 Gy and Sal increased both annexin V and TUNEL staining (Supplementary Fig. 1A and B).
Co-treatment with radiation and Sal increases DNA damage
Next, we examined the mechanism underlying the sensitization of Sal in radiation-treated cells. Since radiation and Sal can cause DNA damage [14], we investigated the ability of Sal to increase DNA damage in irradiated cells. The influence of Sal on the activation of DNA damage-related proteins (e.g. H2AX and 53BP1) was assessed in cells treated with radiation. These proteins are important representative factors that indicate the degree of DNA damage [21, 22]. Increased phosphorylation of these proteins is associated with greater degrees of DNA breakage and damage [21, 22].
Increased pH2AX levels were detected following a single treatment of either radiation or Sal (Fig. 2a). pH2AX levels increased to an even greater degree (Fig. 2a) following co-treatment with radiation and Sal (2 Gy+Sal and 4 Gy+Sal). The results suggest that DNA damage plays a role in Sal sensitization in irradiated cells.
Co-treatment with radiation and Sal increases DNA damage. a Hs578T and MCF7 cells were grown on 60 mm-diameter dishes and then stimulated with 2 Gy of radiation, 4 Gy of radiation, 5 μM Sal, 5 μM Sal with 2 Gy of radiation (2 Gy+Sal), 5 μM Sal with 4 Gy of radiation (4 Gy+Sal), or DMSO (Con). After 1 h, Western blotting was performed using antibodies against pH2AX or GAPDH. b Hs578T cells were grown to 50% confluence and stimulated with 5 μM Sal (left and lower panels: Sal), 5 μM Sal with 4 Gy of radiation (right and lower panels: 4 Gy+Sal), DMSO (left and upper panels: Con), or DMSO with 4 Gy of radiation (right and upper panels: Con). After 30 min, immunocytochemistry was performed. Immunocytochemical staining for pH2AX is shown by green fluorescence and p53BP1 is shown by red fluorescence. DAPI nuclear staining (blue) is also shown. The forth image is a merged image (Merge) of the three stains. c and d Hs578T cells were grown to 50% confluence and treated with 5 μM Sal, 5 μM Sal with 4 Gy of radiation, DMSO (Con), or DMSO with 4 Gy of radiation. After 1 h (c) or 3 h (d), immunocytochemistry was performed. Immunocytochemical staining for p53BP1 is shown by red fluorescence. DAPI nuclear staining (blue) is also shown
Immunocytochemistry demonstrated that Sal increased the number of both pH2AX and p53BP1 foci in radiation-treated cells (Fig. 2b–d), suggesting that increased DNA damage is important for Sal sensitization in these cells. Interestingly, the intensity of the p53BP1 foci was largely increased over time with co-treatment. Treatment with either radiation or Sal alone did not increase the foci in a time-dependent manner. These results indicate that the sensitization effect by co-treatments results from continuous DNA damage.
Co-treatment with radiation and Sal reduces p21 levels
Previously, we found that p21 levels increased by DOX or ETO are reduced by Sal [14]. In the present study, we tested whether this was also the case in radiation-treated cells. The levels of p21 were similar in cells irradiated with low (2 Gy) or high (4 Gy) doses (Fig. 3), suggesting that increased p21 levels were easily saturated by lower levels of radiation. p21 levels increased in the presence of radiation were effectively reduced by Sal (Fig. 3). Collectively, these results indicate that Sal sensitizes radiation-treated cells by increasing DNA damage and reducing p21 levels, similar to DOX and ETO.
Co-treatment with radiation and Sal reduces p21 levels. Hs578T cells were grown on 60 mm-diameter dishes. They were then stimulated with 2 Gy of radiation, 4 Gy of radiation, 5 μM Sal, 5 μM Sal with 2 Gy of radiation (2 Gy+Sal), 5 μM Sal with 4 Gy of radiation (4 Gy+Sal), or DMSO (Con). After 6 h, Western blot analyses were performed with antibodies against p21 and GAPDH
Sal inhibits another type of P-gp substrate, independent of Ver
We investigated to identify a novel role of Sal in sensitizing cancer cells. Sal inhibits P-gp activity [7–9]. In order to more clearly define the mechanism underlying P-gp inhibition by Sal, we investigated the differences between Sal and the P-gp inhibitor, Ver. Both Rho and CFDA were used to test whether Sal and Ver increased the inhibition of P-gp substrate efflux. These two factors are well-known substrates that are used to measure P-gp inhibition [18–20]. In this experiment, cellular accumulation of red or green fluorescence was indicative of Rho or CFDA intracellular concentration. Sal increased Rho staining in both Hs578T and MCF7 cells (Fig. 4a and b), suggesting that Sal contributes to P-gp inhibition. However, no increased CFDA staining was evident in cells treated with Sal. We also tested whether the P-gp inhibitor Ver could increase Rho and CFDA staining. Contrary to Sal, Ver increased CFDA staining but not Rho staining (Fig. 4a and b). The collective results imply that Sal can utilize another type of P-gp substrate independent of Ver. These results were confirmed by quantifying Rho and CFDA staining using FACS analysis (Supplementary Fig. 2A and B). Since increased concentrations of Sal can increase cellular death, we further tested whether increased concentration of Sal enhanced Rho staining. No such increase was evident (Supplementary Fig. 3A and B). This finding was consistent with the hypothesis that increased apoptosis by higher Sal concentrations does not proportionally contribute to increase P-gp inhibition.
Sal and Ver inhibit different P-gp substrates. a Hs578T cells were grown and stimulated for 24 h with 80 μM Ver (Ver-80), 5 μM Sal (Sal-5), or DMSO (Con). The cells were then stained with CFDA or Rho as described in the “Materials and method” section. The stained cells were subsequently examined using an inverted fluorescence microscope with a 10× objective lens. b MCF7 cells were grown and stimulated for 24 h with 40 μM Ver (Ver-40), 5 μM Sal (Sal-5), or DMSO (Con). The cells were then stained with CFDA or Rho. The stained cells were subsequently examined using an inverted fluorescence microscope with a 10× objective lens
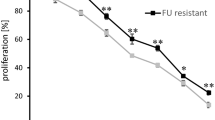
When the cytotoxic effects of Sal and Ver were compared, 5 μM of Sal had an effect comparable to that of >40 μM Ver (Supplementary Fig. 4A and B). Hs578T cells displayed a relatively Ver-resistant phenotype when the Ver concentration was increased (Supplementary Fig. 4A). Sal reduced the proliferation of both Hs578T and MCF7 cells (Supplementary Fig. 4B), suggesting it can be used against Ver-resistant cancers.
Discussion
Sal is a potential anti-cancer drug used for sensitizing drug-resistant cancer stem cells [3, 7–14]. The present study aimed to identify both new combination treatment methods to improve Sal sensitization and novel mechanisms of Sal sensitization. A more complete understanding of the Sal sensitization mechanism could facilitate the therapeutic use of Sal in cancer patients.
The present study demonstrates that Sal sensitizes radiation-treated cancer cells. Sal sensitizes cancer cells with DNA damage caused by DOX and ETO [14]. However, it has been unclear whether Sal is useful for sensitizing cells treated with non-chemotherapeutic agents. Radiation is particularly useful for use in combination with chemotherapeutic agents [23, 24]. The present results demonstrate the clinical utility of Sal in combination with any agent (i.e., radiation or chemical) that causes DNA damage. While seeking a definitive mechanism of Sal action, we observed that G2 arrest was greatly increased in co-treated cells. Since both radiation and Sal damage DNA [14, 23, 24], we tested whether DNA damage is increased by co-treatment. pH2AX protein levels and cellular foci formation were increased in co-treatment cells. In addition, p53BP1 foci formation with co-treatment was highly increased in a time-dependent manner, suggesting that the effects of co-treatments can persist. This may be clinically useful. Taken together, our results imply that increased DNA damage caused by co-treatment is responsible for the prolonged G2 phase.
In this study, we assumed that the sensitization effects for co-treatments resulted from two different DNA damage pathways via treatment with radiation or Sal. Since it is reported that DOX- or ETO-mediated increased p21 expression is reduced by co-treatment with Sal [14], we also tested whether Sal could reduce increased p21 levels resulting from radiation. Previously, the p21 tumor suppressor protein was shown to exert an anti-apoptotic effect, thereby promoting cell survival following DNA damage [25–29]. We found that Sal also reduced p21 levels in radiation-treated cells, suggesting that the mechanism of Sal sensitization is conserved in non-chemotherapeutic DNA damaging drug action. Conservation of a sensitization mechanism assumes that Sal targets the same molecules, even when Sal is used in different combinations of various anti-cancer treatments. Identifying molecules consistently targeted by Sal would be beneficial for developing effective anti-cancer treatments. It will be interesting to investigate whether Sal sensitizes cells in combination with non-DNA damaging agents such as paclitaxcel, and whether the sensitization mechanism involves both an increase of DNA damage and reduction of p21 levels. Collectively, the data suggest that increased DNA damage and reduced p21 levels are major effects associated with reducing proliferation and G2 arrest following co-treatments.
Monitoring the accumulation of Rho and CFDA demonstrated that Sal and Ver inhibited different P-gp substrates. These observations support the idea that Sal is another kind of P-gp inhibitor that acts differently than Ver, a well-known P-gp inhibitor [4–6]. Inhibition was achieved with a markedly lower concentration of Sal, suggesting that Sal more effectively inhibits P-gp in cancer cells than Ver. Sal also sensitized relatively Ver-resistant cancer cells, indicating that Sal may be useful for treating Ver-resistant cancers. These results show that sensitization by Sal may involve mechanisms not utilized by Ver. Previously, it was reported that Sal increases DNA damage and reduces p21 levels [14]. It is possible that these effects may contribute to the sensitization of Ver-resistant cancer cells.
Overall, the results from our study demonstrate that Sal can sensitize radiation-treated cancer cells by increasing DNA damage and reducing p21 protein levels. This is accomplished through a conserved mechanism similar to DOX- and ETO-sensitization. Sal also sensitized Ver-resistant cells. Our findings may contribute to developing Sal-based combination therapies for cancer patients treated with agents that induce DNA damage or P-gp inhibitors.
Abbreviations
- DOX:
-
doxorubicin
- DMSO:
-
dimethylsulfoxide
- ETO:
-
etoposide
- Sal:
-
salinomycin
- Ver:
-
verapamil
- MDR:
-
multi-drug resistance
- P-gp:
-
p-glycoprotein
- FACS:
-
fluorescence-activated cell sorting
- Rho:
-
rhodamin123
- CFDA:
-
carboxyfluorescein diacetate
- DAPI:
-
4′-6-diamidino-2-phenylindole
- FBS:
-
fetal bovine serum
- BSA:
-
bovine serum albumin
- TCA:
-
trichloroacetic acid
- PBS:
-
phosphate buffered saline
- SDS-PAGE:
-
sodium dodecyl sulfate-polyacrylamide gel electrophoresis
- TUNEL:
-
terminal transferase dUTP nick end labeling
References
Miyazaki Y, Shibuya M, Sugawara H, Kawaguchi O, Hirsoe C (1974) Salinomycin, a new polyether antibiotic. J Antibiot 27:814–821
Mahmoudi N, de Julián-Ortiz JV, Ciceron L, Gálvez J, Mazier D, Danis M, Derouin F, Garcia-Domenech R (2006) Identification of new antimalarial drugs by linear discriminant analysis and topological virtual screening. J Antimicrob Chemother 57:489–497. doi:10.1093/jac/dki470
Gupta PB, Onder TT, Jiang G, Tao K, Kuperwasser C, Weinberg RA, Lander ES (2009) Identification of selective inhibitors of cancer stem cells by high-throughput screening. Cell 138:645–659. doi:10.1016/j.cell.2009.06.034
O’Connor R (2007) The pharmacology of cancer resistance. Anticancer Res 27:1267–1272
Yang K, Wu J, Li X (2008) Recent advances in the research of P-glycoprotein inhibitors. Biosci Trends 2:137–146
Shukla S, Wu CP, Ambudkar SV (2008) Development of inhibitors of ATP-binding cassette drug transporters: present status and challenges. Expert Opin Drug Metab Toxicol 4:205–223. doi:10.1517/17425255.4.2.205
Fuchs D, Heinold A, Opelz G, Daniel V, Naujokat C (2009) Salinomycin induces apoptosis and overcomes apoptosis resistance in human cancer cells. Biochem Biophys Res Commun 390:743–749. doi:10.1016/j.bbrc.2009.10.042
Fuchs D, Daniel V, Sadeghi M, Opelz G, Naujokat C (2010) Salinomycin overcomes ABC transporter-mediated multidrug and apoptosis resistance in human leukemia stem cell-like KG-1a cells. Biochem Biophys Res Commun 394:1098–1104. doi:10.1016/j.bbrc.2010.03.138
Riccioni R, Dupuis ML, Bernabei M, Petrucci E, Pasquini L, Mariani G, Cianfriglia M, Testa U (2010) The cancer stem cell selective inhibitor salinomycin is a p-glycoprotein inhibitor. Blood Cells Mol Dis 45:86–92. doi:10.1016/j.bcmd.2010.03.008
Wang Y (2011 Jan 11) Effects of salinomycin on cancer stem cell in human lung adenocarcinoma A549 cells. Med Chem [Epub ahead of print]
Dong TT, Zhou HM, Wang LL, Feng B, Lv B, Zheng MH (2011 Jan 26) Salinomycin selectively targets ‘CD133+’ cell subpopulations and decreases malignant traits in colorectal cancer lines. Ann Surg Oncol [Epub ahead of print]. doi:10.1245/s10434-011-1561-2
Gong C, Yao H, Liu Q, Chen J, Shi J, Su F, Song E (2010) Markers of tumor-initiating cells predict chemoresistance in breast cancer. PLoS ONE 5:e15630. doi:10.1371/journal.pone.0015630
Bardsley MR, Horvàth VJ, Asuzu DT, Lorincz A, Redelman D, Hayashi Y, Popko LN, Young DL, Lomberk GA, Urrutia RA, Farrugia G, Rubin BP, Ordog T (2010) Kitlow stem cells cause resistance to Kit/platelet-derived growth factor alpha inhibitors in murine gastrointestinal stromal tumors. Gastroenterology 139:942–952. doi:10.1053/j.gastro.2010.05.083
Kim JH, Chae MJ, Kim WK, Kim YJ, Kang HS, Kim HS, Yoon S (2011) Salinomycin sensitizes cancer cells to the effects of doxorubicin and etoposide treatment by increasing DNA damage and reducing p21 protein. Br J Pharmacol 162:773–784. doi:10.1111/j.1476-5381.2010.01089.x
Kim JH, Lee SC, Ro J, Kang HS, Kim HS, Yoon S (2010) Jnk signaling pathway-mediated regulation of Stat3 activation is linked to the development of doxorubicin resistance in cancer cell lines. Biochem Pharmacol 7:373–380. doi:10.1016/j.bcp.2009.09.008
Kim JH, Kim TH, Kang HS, Ro J, Kim HS, Yoon S (2009) SP600125, an inhibitor of Jnk pathway, reduces viability of relatively resistant cancer cells to doxorubicin. Biochem Biophys Res Commun 387:450–455. doi:10.1016/j.bbrc.2009.07.036
Lee KH, Moon KJ, Kim HS, Yoo BC, Park S, Lee H, Kwon S, Lee ES, Yoon S (2008) Increased cytoplasmic levels of CIS, SOCS1, SOCS2, or SOCS3 are required for nuclear translocation. FEBS Lett 582:2319–2324. doi:10.1016/j.febslet.2008.05.039
Dogan AL, Legreand O, Faussat AM, Perrot JY, Marie JP (2004) Evaluation and comparison of MRP1 activity with three fluorescent dyes and three modulators in leukemic cell lines. Leuk Res 28:619–622. doi:10.1016/j.leukres.2003.10.015
Kim YK, Song YJ, Seo DW, Kang DW, Lee HY, Rhee DK, Han JW, Ahn CM, Lee S, Kim SN (2007) Reversal of multidrug resistance by 4-chloro-N-(3-((E)-3-(4-hydroxy-3-methoxyphenyl)acryloyl)phenyl)benzamide through the reversible inhibition of P-glycoprotein. Biochem Biophys Res Commun 355:136–142. doi:10.1016/j.bbrc.2007.01.117
Kweon SH, Song JH, Kim TS (2010) Reveratrol-mediated reversal of doxorubicin resistance in acute myeloid leukemia cells via downregulation of MRP1 expression. Biochem Biophys Res Commun 395:104–110. doi:10.1016/j.bbrc.1010.03.147
Kawabe T (2004) G2 checkpoint abrogators as anticancer drugs. Mol Cancer Ther 3:513–519
Solier S, Sordet O, Kohn KW, Pommier Y (2009) Death receptor-induced activation of the Chk2- and histone H2AX-associated DNA damage response pathways. Mol Cell Biol 29:68–82. doi:10.1128/MCB.00581-08
Inskip PD, Robison LL, Stovall M, Smith SA, Hammond S, Mertens AC, Whitton JA, Diller L, Kenney L, Donaldson SS, Meadows AT, Neglia JP (2009) Radiation dose and breast cancer risk in the childhood cancer survivor study. J Clin Oncol 27:3901–3907. doi:10.1200/JCO.2008.20.7738
Shin HJ, Kim JY, Hampson L, Pyo H, Baek HJ, Roberts SA, Hendry JH, Hampson IN (2010) Human papillomavirus 16 E6 increases the radiosensitivity of p53-mutated cervical cancer cells, associated with up-regulation of aurora A. Int J Radiat Biol 86:769–779. doi:10.3109/09553002.2010.484477
Weiss RH (2003) p21Waf1/Cip1 as a therapeutic target in breast and other cancers. Cancer Cell 4:425–429. doi:10.1016/S1535-6108(03)03308-8
Radhakrishnan SK, Bhat UG, Halasi M, Gartel AL (2008) P-TEFb inhibitors interfere with activation of p53 by DNA-damaging agents. Oncogene 27:1306–1309. doi:10.1038/sj.onc.1210737
Park SH, Wang X, Liu R, Lam KS, Weiss RH (2008) High throughput screening of a small molecule one-bead-one-compound combinatorial library to identify attenuators of p21 as chemotherapy sensitizers. Cancer Biol Ther 7:2015–2022. doi:10.4161/cbt.7.12.7069
Idogawa M, Sasaki Y, Suzuki H, Mita H, Imai K, Shinomura Y, Tokino T (2009) A single recombinant adenovirus expressing p53 and p21-targeting artificial microRNAs efficiently induces apoptosis in human cancer cells. Clin Cancer Res 15:3725–3732. doi:10.1158/1078-0432.CCR-08-2396
Lee EW, Lee MS, Camus S, Ghim J, Yang MR, Oh W, Ha NC, Lane DP, Song J (2009) Differential regulation of p53 and p21 by MKRN1 E3 ligase controls cell cycle arrest and apoptosis. EMBO J 28:2100–2113. doi:10.1038/emboj.2009.164
Acknowledgements
This work was supported by research grant (NCC0910170) from the National Cancer Center, South Korea.
Author information
Authors and Affiliations
Corresponding author
Additional information
Won Ki Kim and Ju-Hwa Kim contributed equally to this work.
Electronic Supplementary Materials
Below is the link to the electronic supplementary material.
Supplementary Fig. 1
Co-treatment with radiation and Sal increases apoptosis. (A-B) Hs578T cells were grown on 60 mm-diameter dishes and then treated with 4 Gy of radiation, 5 μM Sal, 5 μM Sal with 4 Gy of radiation (4 Gy+Sal), or DMSO (Control). After 48 h, Annexin V (A) and TUNEL analyses (B) were performed as described in the “Materials and method” section. (JPEG 16 kb)
Supplementary Fig. 2
Quantification of CFDA and Rho staining confirms that Sal and Ver inhibit different P-gp substrates. (A-B) MCF7 cells were grown and treated for 24 h with 40 μM Ver, 5 μM Sal, or DMSO (Con). The cells were then stained with CFDA (A) or Rho (B). The stained cells were subsequently analyzed using a FACSCalibur flow cytometry system as described in the “Materials and method” section. (JPEG 18 kb)
Supplementary Fig. 3
Higher Sal concentrations do not contribute to increased Rho staining. (A-B) Hs578T and MCF7 cells were grown and treated for 24 h with 5 μM Sal (Sal-5), 10 μM Sal (Sal-10), 15 μM Sal (Sal-15), or DMSO (Con). The cells were then stained with Rho as described in the “Materials and method” section. The stained cells were subsequently examined using an inverted fluorescence microscope with 10× (A) and 16× (B) objective lenses. (JPEG 31 kb)
Supplementary Fig. 4
Sal sensitizes relatively Ver-resistant cancer cells. (A-B) Hs578T and MCF7 cells were grown and treated for 24 h with 20 μM Ver (Ver-20), 40 μM Ver (Ver-40), 80 μM Ver (Ver-80), 5 μM Sal (Sal-5), or DMSO (Con). They were subsequently observed using an inverted microscope with a 10× objective lens. (JPEG 35 kb)
Rights and permissions
About this article
Cite this article
Kim, W.K., Kim, JH., Yoon, K. et al. Salinomycin, a p-glycoprotein inhibitor, sensitizes radiation-treated cancer cells by increasing DNA damage and inducing G2 arrest. Invest New Drugs 30, 1311–1318 (2012). https://doi.org/10.1007/s10637-011-9685-6
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s10637-011-9685-6