Summary
Ispinesib (SB-715992) inhibits the mitotic kinesin spindle protein (KSP), a novel target for anticancer therapy. A phase II study was conducted to examine the efficacy of ispinesib in recurrent or metastatic head and neck squamous cell carcinoma (RMHNSC). Patients with up to one prior line of chemotherapy for RMHNSC were treated with ispinesib 18 mg/m2 IV over 1 hour every 21 days. Twenty-one patients were enrolled onto this study with a target stage I sample size of 19. Of 20 evaluable patients, no objective responses were seen and stable disease > 2 cycles was observed in five patients (25%). The median time to progression was 1.4 (95% CI 1.3–2.3) months, median survival was 3.5 (95% CI 2.8–7.8) months, and 1 year overall survival was 20% (95% CI 8.3–48.1%). The most frequent attributable grades III–V adverse events were neutropenia (60% of patients) and leukopenia (55%). The pharmacokinetic profile was consistent with results from phase I studies. Archival tissues (n = 14) demonstrated low to moderate KSP expression by immunohistochemistry. In addition, no pharmacodynamic changes were observed in peripheral blood mononuclear cells. We detected no antitumor activity of ispinesib in RMHNSC on this dosing schedule.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Recurrent or metastatic head and neck squamous cell cancer (RMHNSC) is a challenging clinical problem with an extremely poor prognosis. Median survival for patients with recurrent or metastatic disease is 5–8 months [1–5]. Platinum-based systemic therapy is a standard treatment. Randomized trials have shown superior response rates but failed to show a survival benefit for combination chemotherapy over single-agent cisplatin [1–3, 5, 6]. Thus, patients with RMHNSC are suitable candidates for clinical trials.
Mitosis is a highly regulated series of events in which identical copies of the genome are moved into two discrete locations within the dividing cell through the formation of a bipolar mitotic spindle. Kinesin spindle protein (KSP), also known as hsEg5, is encoded by the gene KNSL1. KSP is a novel target for anticancer therapy. The catalytic domain of KSP hydrolyzes adenosine triphosphate (ATP) to produce directed mechanical force along microtubules of the emerging mitotic spindle, thereby driving formation of a bipolar spindle [7, 8]. KSP has no known role outside of mitosis, and is abundantly expressed in tumor tissue compared with normal adjacent tissue [9]. Ispinesib (SB-715992) is a polycyclic, nitrogen-containing heterocycle. It is a highly selective inhibitor of KSP. Through allosteric inhibition of the KSP motor domain ATPase, ispinesib inhibits ADP release and locks the KSP motor in a state loosely bound to microtubules [10]. Ispinesib prevents the formation of a bipolar mitotic spindle, causing cells to arrest in mitosis with unseparated centrosomes [11]. It demonstrated broad spectrum anti-tumor activity in a variety of in vitro tumor cell lines and human tumor xenografts [11]. In phase I studies evaluating a variety of schedules, common toxicities included fatigue, leukopenia, and anemia; the dose limiting toxicity was neutropenia [12–14]. The best response observed was prolonged stable disease, including two patients with RMHNSC [12, 13].
Innovative therapies are clearly needed for this devastating disease. This phase II study was conducted to evaluate the efficacy, as measured by response rate, of ispinesib in patients with RMHNSC who have received up to one prior line chemotherapy regimen for recurrent or metastatic disease. We also evaluated: toxicity and time to event parameters, pharmacokinetics, archival tumor tissue expression of KSP as a predictive marker for clinical response, and pharmacodynamic effects of ispinesib on peripheral blood mononuclear cells (PBMCs).
Patients and methods
Eligibility
Patients enrolled onto this study had histologically or cytologically confirmed RMHNSC and had received up to one prior chemotherapy regimen for RMHNSC. Prior platinum-based chemotherapy delivered concurrently with radiotherapy, and prior platinum-based induction chemotherapy was permitted. Other eligibility criteria included: age ≥18 years; radiographically measurable disease; Eastern Cooperative Oncology Group (ECOG) performance of 0 to 2; neuropathy ≤ grade 1 at study entry; life expectancy of at least 12 weeks; and adequate hematologic, hepatic, and renal functions. A four week interval was required between any chemotherapy, radiotherapy, or surgery and study entry as well as recovery from all relevant toxicities. Patients who received local therapy prior to study entry were required to have either progression of measurable disease documented within the treatment field, or measurable disease outside the treatment field. Ispinesib is a moderate to significant in vitro inhibitor of CYP3A4, therefore, the use of CYP3A4 inhibitors and inducers within 14 days (≥ 6 months for amiodarone) was prohibited. The research ethics board at each participating institution approved the protocol and all patients enrolled on study gave written informed consent in accordance with federal and institutional guidelines before treatment.
Drug administration
Ispinesib was administered by intravenous infusion at an initial dose of 18 mg/m2 over 1 hour every 21 days in an outpatient setting [13]. Concomitant D5W infusion and heating pads were used to minimize local irritation and pain at the infusion site.
Dose delays or modifications were specified for hematologic and neurologic toxicities. Hematological requirements for subsequent cycles included an absolute neutrophil count ≥ 1,500/mm3 and a platelet count of ≥ 100,000/mm3 on day 1 of treatment. Treatment was held until recovery to these values. Ispinesib doses were reduced 25% for: grade 4 thrombocytopenia, thrombocytopenic bleeding, grade 4 neutropenia persisting longer than 3 days, or for febrile neutropenia requiring hospitalization and intravenous antibiotics. Grade 2 neurotoxicity and other grade 3 non-hematological major organ toxicity required a 25% dose reduction. Treatment was discontinued for ≥ grade 3 neurotoxicity or other grade 4 non-hematologic major organ toxicities. Cycle length was 3 weeks and treatment was continued until disease progression, intercurrent illness that prevented further administration of treatment, unacceptable toxicity, patient refusal, or physician’s decision to withdraw the patient.
On-study evaluation
Patients were evaluated with a complete history and physical every 3 weeks, as well as a complete blood count and biochemical profile weekly while on treatment. Toxicities were evaluated using the National Cancer Institute Common Terminology Criteria for Adverse Events (CTCAE) version 3.0. Objective tumor responses were determined by computerized tomography every 6 weeks according to Response Evaluation Criteria in Solid Tumors (RECIST) [15].
Pharmacokinetic analysis
In consenting patients, blood samples (3 ml/sample) were collected from a peripheral vein in potassium EDTA tubes at the following time points during cycle 1: pre-ispinesib administration, immediately following completion of ispinesib administration, at 30–60 minutes, 90–150 minutes, 4–6 hours, 20–29 hours, and 36–48 hours post ispinesib infusion. Ispinesib levels were determined using validated high performance liquid chromatography-mass spectrometry/ mass spectrometry methods (Appendix 1).
A population pharmacokinetic analysis was conducted using NONMEM (Globomax LLC; Hanover, MD) on phase I ispinesib data following an 18 mg/m2 dose [13]. The final model was validated using the posterior predictive check method and was used to simulate plasma ispinesib concentration-time profiles resulting from a dose of 18 mg/m2. A post-hoc median profile with 90% confidence interval was created based on this model. Observed data from the current study were overlaid on the simulated profile to determine if the observed data exhibit the central tendency and variability of the phase I data obtained at the same dose level.
Molecular correlates
Archival tumoral tissue was analyzed at the central laboratory for tumoral expression of KSP by immunohistochemistry (IHC). Formalin-fixed, paraffin-embedded tissue was cut in 4-μm sections and placed onto positively charged slides. Slides were deparaffinized in xylene, and rehydrated in decreasing ratios of ethanol/water. Following antigen retrieval and blocking, sections were incubated for 30 minutes with a highly specific anti-KSP monoclonal antibody (kindly provided by Dr. Yun-Fu Hu, GlaxoSmithKline) at a dilution of 1:5000. Immunohistochemical staining was performed using an Envision+ polymer (rabbit) and the Dako Autostainer Universal Staining System (Dako North America Inc., Carpenteria, CA). Slides were counterstained with 50% Mayer’s hematoxylin. Human tonsillar tissue was used as positive control for KSP staining. There is no standard IHC scoring method for KSP. The KSP stained slides were scored as positive or negative by two independent pathologists who were blinded to clinical outcomes. Staining intensity was scored in a semi-quantitative manner from no staining (0) to strongly positive (3+). In cases where there were multiple sections or where there were varying levels of intensity within a section, the final score represented the area of highest staining intensity.
For analysis of cytoskeletal morphologic changes following drug treatment, PBMCs were isolated from whole blood at the following times around dose 1 of cycle 1; pre-treatment, immediately prior to the end of the infusion, and then 1, 4, and 24 hours after the end of the infusion. At each of the indicated times, 8 ml of blood was drawn in CPT® tubes (Becton Dickinson cat. # 362753) for isolation of PBMCs. Cytospins were made and fixed at each of the treating institutions before being shipped to the central laboratory for analysis.
Analysis consisted of simultaneous fluorescent immunohistochemical assessment of alpha-tubulin, phosphohistone H3, and chromatin. Briefly, PBMCs were incubated with primary antibodies (e.g. alpha-tubulin, and phosphohistone H3) for 1 hour at room temperature (Appendix 1). After thorough washing, slides were incubated with fluorescent-labeled secondary antibodies for 1 hour at room temperature (Appendix 1). After another round of washing, slides were incubated with propidium iodide for labeling of chromatin. Finally, the partially dried slides were covered with glass cover slips using VectaShield (Vector Laboratories, Burlingame, CA) mounting media.
Stained slides were imaged using an Olympus IX81 inverted digital fluorescent microscope fitted with a Spot RT (real time) digital camera, and image analysis was performed using Image Pro software (Media Cybernetics, Inc., Silver Spring, MD). Separate images were acquired for the specific target protein (e.g. tubulin, and phosphohistone H3) and DNA, and the final image was obtained by merging the separate data files. With each set of slides to be analyzed, human cultured cell line controls (Hela cells), both positive (i.e. with 1° antibody) and negative (i.e. without 1° antibody), were included to assess the adequacy and specificity of the staining procedure.
Statistical methods
The primary endpoint was objective response rate (partial and complete response). Simon’s optimal two-stage design was used [16]. This design allowed for early termination after 19 patients if 3 or fewer responses were observed. After accrual of 33 patients, the drug is considered to be active if 8 or more responses are seen. This sample size calculation was based on the null hypothesis (p0) that the response rate was 15% or lower, versus the alternate hypothesis (p1) that the response rate was 35% or higher, and error rates were set at α ≤ 0.10 and β ≤ 0.10. After the 20th evaluable patient was accrued, an interim analysis was performed and no responses were observed, thus, the early stopping rule was met and accrual stopped.
Summary statistics, such as the mean, median and frequency, were used to describe the characteristics of the patients enrolled to this study. Time to progression (TTP) was defined as the time from enrolment onto the study until progression or death. Overall survival was defined as the time from enrolment until death due to any cause. The Kaplan–Meier method was used to estimate overall survival and TTP. All tests were two-sided and a p-value of less than 0.05 was considered statistically significant. All statistical calculations were performed in SAS v.8 (SAS Institute, Cary, NC, USA) and S-plus 2000 (Insightful Corp., Seattle, WA, USA).
Results
Patient characteristics
A total of 21 patients were enrolled onto the study between February 2005 and June 2006 (Table 1). One patient was ineligible due to disease progression prior to treatment.
Treatment administration
A total of 50 cycles were administered, with a median of two cycles (range 1–5). Four patients required at least one dose reduction and 2 patients had a treatment delay. Dose reductions were primarily due to myelosuppression while dose delays were for logistical reasons.
Objective response
Of 20 eligible patients enrolled on this study, there were no complete or partial responses seen. Eight patients had objective stable disease at cycle 2; however, 3 of these had symptomatic progressive disease at that time in the opinion of the investigator and came off study. Therefore, five patients had both clinical and objective stable disease, experiencing disease progression after cycles 3, 4, 4, 5 and 5 respectively. One of the five patients who experienced stable disease had received prior treatment for RMHNSC (cisplatin and docetaxel). Fourteen patients had progressive disease as their best response. One patient died of pneumonia (possibly related to ispinesib) and was inevaluable for response.
Time to disease progression and overall survival
The median TTP was 1.4 (95% CI 1.3–2.3) months. The median survival was 3.5 (95% CI 2.8–7.8) months and the 1-year survival was 20% (95% CI 8.3–48.1%).
Toxicity
The most common toxicities deemed at least possibly attributable to ispinesib were leukopenia in 16 patients over 35 cycles (70% of cycles), and neutropenia in 15 patients over 31 cycles (62%) (Table 2). One patient died of progressive disease after cycle 2 of treatment. Two other patients died while on study: one due to a fatal pneumonia (grade 5) in the setting of grade 4 neutropenia lasting 4 days; the other died of upper airway obstruction due to progressive disease and non-neutropenic infection (grade 3). Both of these events were considered possibly related to ispinesib. The most common grades 3–5 adverse events were neutropenia in 12 patients (60%) and leukopenia in 11 patients (55%). No patient had treatment discontinued due to a non-fatal adverse event.
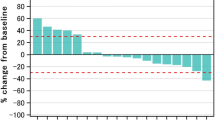
Pharmacokinetics
Four patients consented to pharmacokinetic sampling. Ispinesib plasma concentrations following an 18 mg/m2 dose were comparable to those observed in phase I studies, as shown in Fig. 1. The fixed and random effects of the population pharmacokinetic model adequately describe the central tendency and variability of the observed data.
Pharmacodynamics
Tumor
Archival tumor tissue was collected from 14 patients and analyzed for KSP expression by IHC. Low to moderate KSP expression was detected in all of the cases evaluated. A representative tumor specimen is shown in Fig. 2. As depicted in the figure, areas of tumor stained moderately positive relative to adjacent stroma. Staining intensity was highest at the basal edge of the tumor nests where the proliferative activity is expected to be highest. The KSP staining was primarily cytoplasmic, except for in the few cells that were undergoing mitotic cell division where staining was strongly nuclear. Normal human tonsil tissue also showed areas of moderate KSP expression that stained less intensely than tumor specimens. Similar to the tumor, staining was cytoplasmic with a few dividing cells displaying intense nuclear staining. However, given that there was no objective response seen, correlation of this endpoint was not made with KSP expression.
PBMC Studies
Serial PBMCs were collected from 17 patients for determination of the effects of ispinesib on cytoskeletal morphology. A total of 7 complete sets of cytospins were analyzed. Despite the expected results seen in cultured Hela cells grown in vitro in the presence and absence of ispinesib (Fig. 3a, b), no monopolar spindles were observed in any of the PBMCs collected and analyzed from patients on this trial (Fig. 3c–f). To further investigate the negative results of the PBMC studies, additional experiments were performed in donor lymphocytes that were mitogen-stimulated in the presence or absence of ispinesib. Phytohemaglutinin (PHA)-stimulated lymphocytes grown in the presence of the drug were found to have the distinct morphologic appearance (i.e. monasters) that were seen in the Hela cell positive controls (data not shown).
Fluorescent immunohistochemical analysis of the pharmacodynamic effects ispinesib on cultured Hela cells grown in vitro in the presence and absence of 10 nM ispinesib (a and b) and in peripheral blood lymphocytes from a patient collected before and then 1, 2 and 24 hours after drug treatment (c–f). Cells were stained separately for tubulin (green), phosphohistone H3 (red), and chromatin (blue) and the composite images are shown (40×)
Discussion
This phase II study examined the efficacy and safety of ispinesib, an inhibitor of KSP, in RMHNSC. Similar to what was observed in phase I studies, leukopenia and neutropenia were the most common adverse events [12–14]. Although only four patients participated in pharmacokinetic sampling, the profile was consistent with data from phase I studies performed in patients with advanced solid tumors. The best response was stable disease in 5 patients. The median overall survival was 3.5 months (95% CI 2.8–7.8) compared to a median overall survival of 5–8 months observed with conventional cytotoxic chemotherapy in this patient population [1–5]. Due to the lack of activity, this study was stopped after the first stage. Additional evaluation of ispinesib at this dose and schedule is not warranted in RMHNSC.
Circulating PBMCs from patients treated with ispinesib failed to display the expected drug-induced morphologic changes. However, when these same circulating PBMCs are mitogen-stimulated in the presence of the drug, the characteristic monasters are formed. Therefore, one might conclude that non-dividing cells are unaffected by ispinesib, and the lack of pharmacodynamic effects seen in the PBMCs likely reflects the absence of dividing cells in circulation at the time of sampling. Tumoral tissues would likely have been more appropriate for the pharmacodynamic evaluation of this agent, since other surrogate tissues such as skin or buccal mucosa may have similar problems as PBMCs due to their low intrinsic mitotic rates. Besides the possibility that PBMCs may not be the ideal surrogate tissues in this setting, the timing of the sampling may provide another explanation for the absence of pharmacodynamic effects. Based on the observed pharmacokinetic profile, the PBMCs were assayed for pharmacodynamic effects during the time interval when peak ispinesib plasma concentration (Cmax) was reached. Hence, the lack of such effects in our study suggests that pharmacokinetically, the duration of exposure above a required threshold concentration, rather than Cmax, may be a more relevant parameter for ispinesib activity.
KSP is a novel anticancer target, and only one other published study in lung cancer has examined KSP by IHC [17]. The tumor staining pattern in the current study (primarily cytoplasmic with occasional strong nuclear staining) is consistent with their findings. Furthermore, the current study is part of a broader clinical development program for ispinesib. The results of the other studies are not yet available. Similar patterns of KSP staining have been seen across a range of tumor histologies, however, the percentage of KSP positive tumors and overall staining intensity appears to be higher for head and neck cancers than for most of the other tumor types evaluated (unpublished data).
Despite high KSP expression in archival tumors, only a very small number of tumor cells would actually be undergoing mitosis at a particular point in time. Since ispinesib acts during mitosis, only a small fraction of the tumor cells would be affected at any one time. This suggests that the efficacy of this agent may be optimized by increasing the exposure time above threshold drug concentration to enable more cells to enter the drug-sensitive phase. Therefore, alternate schedules of ispinesib administration, such as repeated infusions on an intermittent schedule, or a more prolonged infusion, may theoretically have greater therapeutic effects. The schedule of administration may prove to be critical for other novel mitosis-specific agents such as aurora and polo-like kinase inhibitors.
Despite ongoing evaluation of regimes containing newer cytotoxics, survival for patients with RMHNSC remains poor. Treatments with greater efficacy, tolerability and convenience are clearly needed to improve palliation in this population.
References
A phase III randomised trial of cisplatinum, methotrextate, cisplatinum + methotrexate and cisplatinum + 5-FU in end stage squamous carcinoma of the head and neck (1990) Liverpool Head and Neck Oncology Group. Br J Cancer 61:311–315
Clavel M, Vermorken JB, Cognetti F, Cappelaere P, de Mulder PH, Schornagel JH, Tueni EA, Verweij J, Wildiers J, Clerico M, Dalesio O, Kirkpatrick A, Snow GB (1994) Randomized comparison of cisplatin, methotrexate, bleomycin and vincristine (CABO) versus cisplatin and 5-fluorouracil (CF) versus cisplatin (C) in recurrent or metastatic squamous cell carcinoma of the head and neck. A phase III study of the EORTC Head and Neck Cancer Cooperative Group. Ann Oncol 5:521–526
Forastiere AA, Metch B, Schuller DE, Ensley JF, Hutchins LF, Triozzi P, Kish JA, McClure S, VonFeldt E, Williamson SK, Von Hoff DD (1992) Randomized comparison of cisplatin plus fluorouracil and carboplatin plus fluorouracil versus methotrexate in advanced squamous-cell carcinoma of the head and neck: a Southwest Oncology Group study. J Clin Oncol 10:1245–1251
Gibson MK, Li Y, Murphy B, Hussain MH, DeConti RC, Ensley J, Forastiere AA (2005) Randomized phase III evaluation of cisplatin plus fluorouracil versus cisplatin plus paclitaxel in advanced head and neck cancer (E1395): an intergroup trial of the Eastern Cooperative Oncology Group. J Clin Oncol 23:3562–3567
Williams SD, Velez-Garcia E, Essessee I, Ratkin G, Birch R, Einhorn LH (1986) Chemotherapy for head and neck cancer. Comparison of cisplatin + vinblastine + bleomycin versus methotrexate. Cancer 57:18–23
Jacobs C, Lyman G, Velez-Garcia E, Sridhar KS, Knight W, Hochster H, Goodnough LT, Mortimer JE, Einhorn LH, Schacter L, Cherng N, Dalton T, Burroughs J, Rozencweig M (1992) A phase III randomized study comparing cisplatin and fluorouracil as single agents and in combination for advanced squamous cell carcinoma of the head and neck. J Clin Oncol 10:257–263
Wood KW, Cornwell WD, Jackson JR (2001) Past and future of the mitotic spindle as an oncology target. Curr Opin Pharmacol 1:370–377
Vale RD, Milligan RA (2000) The way things move: looking under the hood of molecular motor proteins. Science 288:88–95
Mak J, Freedman R, Beraud C (2002) Utilization of gene expression profiles to identify mitotic kinesins (Abstract). Annu Meet Am Assoc Cancer Res Proc 43:A5375
Sakowicz R, Finer JT, Beraud C, Crompton A, Lewis E, Fritsch A, Lee Y, Mak J, Moody R, Turincio R, Chabala JC, Gonzales P, Roth S, Weitman S, Wood KW (2004) Antitumor activity of a kinesin inhibitor. Cancer Res 64:3276–3280
Johnson RK, McCabe FL, Caulder E, Innlow L, Whitacre M, Winkler JD, Bergnes G, Feng B, Smith WW, Morgans D, Wood K, Jackson JR (2002) SB-715992, a potent and selective inhibitor of the mitotic kinesin KSP, demonstrates broad-spectrum activity in advanced murine tumors and human tumor xenografts (Abstract). Annu Meet Am Assoc Cancer Res Proc 43:A1355
Burris HA, Lorusso P, Jones S, Guthrie TM, Orr JB, Williams DD, Hodge JP, Bush M, Sabry J (2004) Phase I trial of novel kinesin spindle protein (KSP) inhibitor SB-715992 IV days 1, 8, 15 q 28 days. J Clin Oncol (Meeting Abstracts) 22:2004
Chu QS, Holen KD, Rowinsky EK, Wilding G, Volkman JL, Orr JB, Williams DD, Hodge JP, Kerfoot CA, Sabry J (2004) Phase I trial of novel kinesin spindle protein (KSP) inhibitor SB-715992 IV Q 21 days. J Clin Oncol (Meeting Abstracts) 22:2078
Heath EI, Alousi A, Eder JP, Valdivieso M, Vasist LS, Appleman L, Bhargava P, Colevas AD, LoRusso PM, Shapiro G (2006) A phase I dose escalation trial of ispinesib (SB-715992) administered days 1–3 of a 21-day cycle in patients with advanced solid tumors. J Clin Oncol (Meeting Abstracts) 24:2026
Therasse P, Arbuck SG, Eisenhauer EA, Wanders J, Kaplan RS, Rubenstein L, Verweij J, Van Glabbeke M, van Oosterom AT, Christian MC, Gwyther SG (2000) New guidelines to evaluate the response to treatment in solid tumors. European Organization for Research and Treatment of Cancer, National Cancer Institute of the United States, National Cancer Institute of Canada. J Natl Cancer Inst 92:205–216
Simon R (1989) Optimal two-stage designs for phase II clinical trials. Control Clin Trials 10:1–10
Saijo T, Ishii G, Ochiai A, Yoh K, Goto K, Nagai K, Kato H, Nishiwaki Y, Saijo N (2006) Eg5 expression is closely correlated with response of advanced non-small cell lung cancer to antimitotic agents combined with platinum chemotherapy. Lung Cancer 54:217–225
Acknowledgements
This work was supported by NCI contract number N01-CM-62203, and Translational Research Initiative contract number 24XS146.
Author information
Authors and Affiliations
Corresponding author
Appendix 1
Appendix 1
Pharmacokinetic Analysis
Blood samples were centrifuged at 2500 × g for 10 minutes at 5°C. Plasma samples were stored in a polypropylene storage tube at −20°C until shipment. The high performance liquid chromatography-mass spectrometry/ mass spectrometry method used in this study has been validated over the range 0.1 to 100 ng/mL. Ispinesib was extracted from 50 μL of human plasma by protein precipitation using 75/25 acetonitrile/10 mM ammonium formate (pH 3) containing an isotopically labeled internal standard ([2H4]-SB-715992). Extracts were analyzed by HPLC-MS/MS using a TurboIonSpray™ interface and multiple reaction monitoring.
Molecular Correlates
Primary antibodies:
Sigma T4026: Monoclonal Anti-β-Tubulin antibody produced in mouse
Sigma H9908: Monoclonal Anti-phospho-Histone H3 (pSer28) antibody produced in rat
Secondary antibodies:
Sigma F2883: Anti-Mouse IgG (whole molecule) F(ab′)2 fragment–FITC antibody produced in sheep
Biomeda R06: Anti-Rat IgG (Mouse Ads.)- Rhodamine antibody produced in goat
Nuclear stain:
Sigma D9542: 4′,6-Diamidino-2-phenylindole dihydrochloride (DAPI)
The slides were mounted with Vector H-1400: VECTASHIELD HardSet Mounting Medium
Rights and permissions
About this article
Cite this article
Tang, P.A., Siu, L.L., Chen, E.X. et al. Phase II study of ispinesib in recurrent or metastatic squamous cell carcinoma of the head and neck. Invest New Drugs 26, 257–264 (2008). https://doi.org/10.1007/s10637-007-9098-8
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s10637-007-9098-8