Abstract
Background and Aims
Liver transplant patients with primary sclerosing cholangitis often present with concurrent inflammatory bowel disease. The effect of comorbid conditions on post-transplant prognosis was evaluated.
Methods
The 2005–2019 United Network of Organ Sharing Standard Transplant Analysis and Research database was used to identify patients with primary sclerosing cholangitis. Patients were categorized as having Crohn’s Disease, ulcerative colitis, unclassified inflammatory bowel disease, or no inflammatory bowel disease. Baseline characteristics were assessed between cohorts, and outcomes were examined using Cox regression. Outcomes included all-cause mortality, graft failure, infection-induced mortality, and organ system-delineated mortality. Supplementary analyses with unique exclusion and stratification criteria were also performed.
Results
Among 2829 patients undergoing transplant, 1360 were considered to have ulcerative colitis, 372 were considered to have Crohn’s Disease, and 69 were considered to have an unclassified form of inflammatory bowel disease. Primary sclerosing cholangitis patients with some form of inflammatory bowel disease had no increased risk for any outcomes. However, patients with ulcerative colitis had lower risks of general infectious (aHR 0.65 95%CI 0.44–0.95) and sepsis-induced (aHR 0.56 95%CI 0.35–0.91) mortality, whereas patients with Crohn’s Disease had higher risks of sepsis-induced mortality (aHR 2.13 95%CI 1.22–3.70). Supplementary analyses showed effect modification by abdominal surgery history and era.
Conclusion
The type of inflammatory bowel disease in liver transplant patients with primary sclerosing cholangitis was found to portend risk difference for infection-induced mortality, with ulcerative colitis found to be protective and Crohn’s Disease predictive of increased mortality secondary to infectious etiologies. These associations warrant further investigation.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Patients with primary sclerosing cholangitis (PSC) suffer from autoimmune destruction of the hepatobiliary tracts, which culminates in ductal damage, ductopenia, lymphocytic infiltration of hepatobiliary tracts, parenchymal inflammation, and fibrosis [1]. There is currently no effective intervention in controlling the natural history of this condition, and it often results in cirrhosis and end-stage liver disease [2]. Liver transplant (LT) stands as the therapeutic intervention of choice to reverse liver failure [3]. However, LT is well known to have tremendous operative risk, and various recipient and donor risk factors alter the post-transplant prognosis [4,5,6]. Primary sclerosing cholangitis has a unique overlap with inflammatory bowel disease (IBD), classically associated with ulcerative colitis (UC), though Crohn’s Disease (CD) is also seen [1, 7]. Inflammatory bowel disease, depending on phenotype severity, can likewise affect the post-transplant prognosis by increased luminal penetrance, intestinal and portal bacterial translocation, endotoxemia, and increased risk of sepsis and infections in the setting of peri and post-LT immunosuppression [7,8,9].
Previously, there had been concerns around initiating certain immunosuppressive regimens among PSC-IBD subtypes, given the potential risk of immunosuppression-induced IBD flare or colitis [10]. However, more recent studies suggest that this may not be true with certain agents, namely TNF-alpha inhibitors [10,11,12]. However, in a different perspective, the subacute to long-term prognosis of the post-LT course with respect to PSC recurrence, graft viability and survival, rejection, and system-specific causes of death have been seldomly evaluated. Further, there has been a paucity of literature evaluating the individual impact of PSC-UC and PSC-CD. Hence, a comprehensive examination of the prognostic relationships that exist between PSC-IBD subtypes and post-LT outcomes is needed to characterize the impact of IBD-subtypes on post-LT outcomes of PSC patients.
Methods
Database
The United Network for Organ Sharing (UNOS) Standard Transplant and Analysis Research (STAR) database was used for this cohort study. This database contains patient outcome and follow up information for transplant patients across the United States. For this study, data from 2005 to 2019 were queried. All patient data are deidentified, and confidentiality is established via data-use agreements and safety mechanisms. This initiative was also facilitated by the Health Resources and Services Administration Contract 234-2005-370011C; however, the contents of this study are not endorsed by any governmental body and solely represent author’s viewpoints.
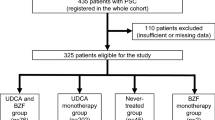
Study Population—Main and Supplementary Analyses
A total of 99,987 patients who received a liver transplant (LT) between 2005 and 2019 were identified. From this cohort, patients lost to follow up (n = 3445) and patients who underwent retransplantation (n = 4310) were excluded. Further exclusions include patients with impossible biological values (e.g., negative serum creatinine) (n = 5), patients under 18 years of age (n = 6872), patients with non-heart-beating organ donation (n = 4427), patients with living donors (n = 3081), patients with non-whole liver (n = 1012), and patients with multiorgan transplant (n = 6462). To focus on only patients with diagnosis of PSC, patients without the diagnosis of PSC were also excluded (n = 62,107). This yields a final cohort of 2829 patients who received LT with the diagnosis of PSC with reported IBD data. This cohort was then stratified by whether they had CD, UC, or no IBD for analysis. Comparisons were conducted between the following cohorts: those with UC versus those without UC, those with CD versus those without CD, those with inflammatory bowel disease versus those without inflammatory disease, and those with UC versus those with CD.
Additional cohorts were generated to further describe the different relationships between IBD and outcomes of the transplanted PSC patient population. A supplementary study pool was produced according to the same procedure outlined above, and patients with hepatocellular carcinoma or cholangiocarcinoma were excluded. A second supplementary analysis stratified the main study population based on their abdominal surgical history. Again, using the main study population, a third analysis divided the time period into LT cases occurring before and after 2012. Similar to the main analysis, comparisons between UC-positive and UC-negative, CD-positive and CD-negative, IBD-positive ad IBD-negative, and UC and CD were conducted for each supplementary analysis. The results of these evaluations are included in Supplementary Tables 3–12 through 13.
Covariates and Study Endpoints
Covariates were chosen to better characterize patient overall health status and donor variables. These included recipient demographics, comorbidities, relevant hepatic laboratory markers, immunosuppressant medications, critical care and life-supporting assistive devices, and donor demographics and laboratory markers. The ‘assistance’ variable was a proxy for functional status based off the Karnofsky score, in which 1 represented scores between 80 and 100% (high functional status), 2 represented 50–70% (intermediate functional status), 3 represented 10–40% (low functional status), and 0 represented no data [13]. The primary outcomes of this study were all-cause mortality and graft failure, whereas secondary outcomes consisted of infectious-related mortality. The general infectious outcome was a composite of several pathogenic entities, including sepsis, viruses, spontaneous bacterial peritonitis, aspergillosis, pneumocystis pneumonia, and other opportunistic pathogens. These pathogenic entities were delineated for the main cohort only, provided that a sufficient number of deaths occurred for Cox regression to be conducted. Furthermore, mortality from cardiac, graft complications (including biliary, recurrent disease, rejection, and vascular dysfunction), gastrointestinal hemorrhage, respiratory, and renal causes were also sampled.
Statistical Analysis
To establish baseline characteristics for our cohort, a series of statistical tests were conducted. For nominal variables, Fisher’s or Chi-squared tests were conducted. Student’s t tests were used to evaluate parametric factors while Whitney-U tests were used to evaluate non-parametric factors.
Multivariable Cox regression analyses were conducted to evaluate the primary and secondary outcomes. For this, four successive models were generated, with each successive model incrementally adjusting for covariates as follows: Model 1—recipient demographics, Model 2—Model 1 covariates and recipient comorbidities, Model 3—Model 2 covariates and recipient liver status and laboratory markers, Model 4—Model 3 covariates and donor characteristics (donor age, gender, race, and BMI). For each iteration of the Cox regression model, an adjusted hazard ratio, 95% confidence interval, and p value were calculated. For each strata-outcome relationship, incidence rates were calculated and expressed in units of per 1000 person-years. Additionally, cumulative hazard analyses were run for our primary and secondary outcomes, and log-rank test was used to evaluate significance for these plots.
To evaluate for competing risks of all-cause mortality and graft failure, a modified version of Fine and Gray’s cumulative incidence functionality was used to create a proportional subdistribution hazard model [14]. Using a similar regression model as described above, a Competing-risks regression model was produced. Random forest iterations were used to offset missingness and therefore enhance statistical power [15].
All statistical tests were conducted utilizing RStudio version 1.2.5042, using R code version 3.6.3.
Results
Main Analysis: Baseline Characteristics
A total of 1360 individuals were identified as having UC compared to 1469 individuals without this diagnosis. Patients with UC were younger (48.3 vs. 49.4 years, p = 0.01), more likely to be male (73.2 vs. 63.2%, p < 0.001), and had lower BMIs (25.2 vs. 25.8 kg/m2, p = 0.02). The racial make-up of the UC-positive group was also significantly different than that of the UC-negative group (p < 0.001). Diabetes and alcoholic liver disease were significantly more prevalent in the non-UC group (diabetes: 13.00 vs. 9.49%, p = 0.004; alcoholic liver disease: 1.29 vs. 0.37%, p = 0.01). Tacrolimus-containing regimens were used more often in the UC-diagnosed group (95.5 vs. 93.1%, p = 0.007).
Meanwhile, there were 372 cases considered to have CD, which were evaluated against 2457 cases without this diagnosis. A higher proportion of white patients was observed in the CD-positive cohort (84.70 vs. 74.60%), among other ethnic differences (p < 0.001). Diabetes was again more prominent in the non-CD group (11.80 vs. 8.06%, p = 0.04). Cases diagnosed with CD had a higher proportion of patients without ascites (35.5 vs. 31.7%, p = 0.04) and lower MELD scores (21.4 vs. 22.7, p = 0.005). Total bilirubin was also lower in the CD group (12.1 mg/dL vs. 13.9 mg/dL, p = 0.001), as well as assistance levels (p = 0.04).
When compared based on IBD presence (1801 patients with IBD versus 1028 without), those with IBD were again younger (48.4 vs. 49.7 years, p = 0.005), more likely to be male (71.3 vs. 62.2%, p < 0.001), and had lower BMIs (25.2 vs. 26.1 kg/m2, p < 0.001). The IBD-positive and -negative cohorts also had different racial distribution (p < 0.001). Comorbidities were significantly different between groups—IBD-negative patients were more likely to present with simultaneous hepatitis C virus (4.96 vs. 3.22%, p = 0.03), alcoholic liver disease (1.85 vs. 0.28%, p < 0.001), and diabetes (15.30 vs. 9.05%, p < 0.001). Again, the IBD-positive group exhibited lower rates of ascites (p = 0.03) and hepatic encephalopathy (p = 0.03). There was a significantly higher proportion of male donors in the IBD-positive group (59.6 vs. 54.6%, p = 0.01) (see Fig. 1).
CD and PSC-UC patients were then compared, and significant differences were found among the cohorts’ racial profile (p = 0.04) and sex profile (73.2% males in PSC-UC vs. 63.4% males in PSC-CD, p < 0.001). MELD scores were higher in the PSC-UC group (22.5 vs. 21.4, p = 0.02). The PSC-UC group was more likely to use tacrolimus (95.5 vs. 91.9%, p = 0.009) and have a higher total bilirubin (13.9 vs. 12.1 mg/dL, 0.002). This data and additional analyses are summarized in Tables 1, 2, 3, 4.
Main Analysis: Clinical Outcomes
The results of the sequential Cox regression analysis showed no statistical differences in the primary outcomes of all-cause mortality and graft failure between patients for any of the comparison (UC-positive vs. UC-negative, CD-positive vs. CD-negative, IBD-positive vs. IBD-negative, and UC-positive vs. CD-positive). Tables 5, 6, 7 through 8 show these results in tabular format, along with case-incidence rates. Cumulative hazards for all-cause mortality and graft failure were graphed in Fig. 2, and the adjusted hazard ratios (aHRs) from the aforementioned Cox regressions are shown in Supplementary Figs. 1–7 through 8, consisting of the Cox model covariates. When considering infectious-related mortality, those with PSC-UC had lower rates of mortality from general infectious causes (aHR 0.65 95% CI 0.44–0.95, p = 0.03, case-incidence rates: 5.86 deaths vs. 9.29 deaths per 1000 person-years) and sepsis (aHR 0.56 95% CI 0.35–0.91, p = 0.02, case-incidence rates: 3.63 deaths vs. 6.67 deaths per 1000 person-years). In contrast to PSC-UC, PSC-CD was found to increase the risk of death for sepsis (aHR 2.13 95% CI 1.22–3.70, p = 0.008, case-incidence rates: 8.57 deaths vs. 4.68 deaths). No differences in risk were found for general infectious causes of death, although case-incidence rates were elevated in PSC-CD (10.09 deaths per 1000 person-years) versus 7.25 deaths per 1000 person-years of the CD-negative group. Comparing the PSC-UC and PSC-CD cohorts, general infectious death risk was relatively reduced in PSC-UC patients (aHR 0.58 95% CI 0.33–1.00, p = 0.05, case-incidence rates: 10.09 deaths vs. 5.86 deaths per 1000 person-years), as well as sepsis-induced death risk (aHR 0.38 95% CI 0.20–0.73, p = 0.003, case-incidence rates: 8.57 deaths vs. 3.63 deaths per 1000 person-years). When combining IBD subtypes, no differences in risk for infectious death were detected between IBD-positive and IBD-negative cases. These regression models are included in Tables 9, 10, 11 through 12. Cumulative hazard curves for infection-related death are shown in Fig. 3, and several curves showed early divergence and significant cumulative risk differences.
Other organ system-based and infection subtype-related mortality outcomes were evaluated via Cox regression. No differences in risk were reported, apart from a decreased risk of death from renal causes in PSC-IBD patients (aHR 0.30 95% CI 0.12–0.76, p = 0.01, case-incidence rates: 0.84 deaths per 1000 person-years vs. 2.47 deaths per 1000 person-years). These analyses are presented in Supplementary Tables 1.1–1.3 through 4. Supplementary Table 2 includes Competing-risks regression models for the primary outcomes, conducted for each of the aforementioned comparisons. No analyses showed significant differences in risk.
Supplementary Analysis—Excluding Primary Liver Cancer
The main study population was refined by excluding patients with hepatocellular carcinoma or cholangiocarcinoma, and baseline characteristics and outcomes were again assessed. Similar results to those of the main cohort were observed—all-cause mortality and graft failure showed no differences in risk between cohorts. However when compared to UC-negative or CD-negative patients, PSC-UC patients experienced lower risk of mortality secondary to general infectious causes (aHR 0.61 95% CI 0.41–0.91, p = 0.02) and due to sepsis (aHR 0.52 95% CI 0.32–0.86, p = 0.01), and PSC-CD patients demonstrated a higher risk of mortality secondary to sepsis (aHR 2.09 95%CI 1.18–3.69, p = 0.01). Combining IBD subtypes led to these associations falling out of significance. Analyses comparing PSC-UC and PSC-CD patients saw those with UC experiencing lower rates of general infectious mortality (aHR 0.54 95% CI 0.31–0.95, p = 0.03) and sepsis mortality (aHR 0.37 95% CI 0.19–0.71, p = 0.003). Supplementary Tables 3, 4 through 5 show these findings, along with case-incidence rates.
Supplementary Analysis—Cases Between 2005–2012 and 2012–2019
The main study population was modified a second time to include cases before and after 2012. Outcomes of these cohorts demonstrated no risk differences for all-cause mortality and graft failure for LT occurring before 2012. However, when considering cases after 2012, PSC-UC cases had lower risk for graft failure (aHR 0.45 95% CI 0.22–0.91, p = 0.03), and PSC-CD cases had higher risk for both graft failure (aHR 2.84 95% CI 1.34–6.04, p = 0.006) and all-cause mortality in the final model only (aHR 1.58 95% CI 1.00–2.47, p = 0.05). Graft failure risk was also comparatively reduced in the PSC-UC group compared to the PSC-CD group (aHR 0.25 95% CI 0.10–0.60, p = 0.002). When isolating cases occurring from 2012 and earlier, infectious-driven mortality was not significantly increased or decreased for any of the final models, for any of the comparisons. The post-2012 era only saw a decreased risk of general infection mortality for PSC-UC patients compared to PSC-CD patients (aHR 0.28 95% CI 0.09–0.85, p = 0.02). These assessments in which the 2005–2019 time period is partitioned into 2 components are included in Supplementary Tables 6–8 through 9.
Supplementary Analysis—Cases Stratified by Abdominal Surgery History
A third inquiry of the main study population involved stratifying cases by having a positive or negative history of abdominal surgery. Cases that had a prior history of abdominal surgery experienced no differences in risk for all-cause mortality, graft failure, or infectious mortality subtypes. Considering the cohort of patients that did not have past abdominal surgery, no risk differences were identified for the primary outcomes. However, these PSC-CD cases did have increased risks for general infectious mortality (aHR 2.50 95% CI 1.20–5.23, p = 0.01) and sepsis (aHR 3.38 95% CI 1.49–7.63, p = 0.003). Similar associations persisted when comparing these PSC-CD patients to PSC-UC patients without prior abdominal surgery, with lower risks of general infectious mortality (aHR 0.32 95% CI 0.13–0.75, p = 0.009) and sepsis mortality (aHR 0.20 95% CI 0.07–0.57, p = 0.002) observed for the PSC-UC group. Data for these analyses (including case-incidence rates) are presented in Supplementary Tables 10–12 through 13.
Discussion
This is the first study to investigate the prognostic implication of IBD in post-LT outcomes, stratified by the IBD subtypes of CD versus UC. Prior literature has clearly delineated the clinical phenotype of PSC-IBD vs IBD alone, but the impact of PSC-IBD versus PSC alone is less understood 7. A retrospective review of a single center in London noted a significant risk associated with active IBD at the time of LT and future graft failure, most commonly due to recurrent PSC 16. They also found a higher numerical incidence of thrombotic events in the PSC-IBD cohort compared to the isolated PSC cohort, though a statistically significant association was not found 16. Recently, Irles-Depe et al. published a retrospective study on 4 LT centers in France regarding graft survival and complications post-LT in PSC-IBD vs PSC alone, finding no significant association with comorbid IBD 17. Our analysis of PSC-IBD vs PSC alone is concordant with the primary findings of their study. Our PSC-UC versus PSC-CD had no differences in primary outcomes in the overall analysis. We further stratified our study cohort by history of abdominal surgery, to potentially account for higher severity of IBD activity, and found no difference in rates of all-cause mortality or graft failure.
When the primary analysis was partitioned by time period to account for potential era effect, we noted a significantly higher rate of graft failure in patients with PSC-CD after the year 2012. When considering recurrent PSC as a leading indication for graft failure, our findings are inconsistent with prior studies on IBD-PSC. In a massive retrospective study on data from 1980 to 2010, Weismuller et al. found PSC-CD to have a milder clinical course compared to PSC-UC 18. Inadequate control of IBD-related disease activity post-LT has been identified as a major risk factor for recurrence of PSC 19. We may potentially be observing a transition in immunosuppressive practices during this latter era that is contributing to increased risk of infection- and sepsis-related mortality in patients with PSC-CD.
When delineating the post-LT outcomes using the IBD subtypes, our results demonstrate that patients with PSC-CD have increased rates of post-LT infection-related mortality. The cumulative hazard curves show that the highest rates of these deaths among PSC-CD appear within the first few months. The rates begin to plateau around years 2–3. When looking to control for confounders of this relationship, the increased rates persisted even when excluding patients with primary liver cancer, such as hepatocellular carcinoma and cholangiocarcinoma. Interestingly, PSC-CD patients without a history of abdominal surgery would further have disproportionate rates of fatal infection. This may suggest that a history of surgical complications of CD did not contribute to this relationship. It may also suggest that surgical management, perhaps for an area of disease refractory to medical treatment, is protective against certain infectious complications. There is also contribution of an era effect to these findings, with no differences detected in the early cohort, though general infection-related mortality was significantly increased in PSC-CD after the year 2012. Consistent with the above discussion on graft failure, this may potentially be due to the evolution of immunosuppressive regimens.
In 2011, a Cochrane review was published on the adverse effects of biologics, including TNF-α inhibitors. This was not a study for IBD specifically, but adalimumab, golimumab, certolizumab, and infliximab were associated with risk of serious infection 20. In 2017, Westwerouen van Meeteren et al. published a meta-analysis investigating the safety of TNF-inhibitors in IBD post liver transplant, and found no significant difference in infection risk based on TNF-inhibitor exposure. However, the conclusions from this study are significantly limited by study size. In 2018, Kirchgesner et al. published a large retrospective cohort study in France assessing infection risk in IBD, stratified according to exposure to thiopurine monotherapy, anti-TNF monotherapy, both, or neither. They found significantly higher risk of serious infection with anti-TNF monotherapy exposure compared to thiopurine monotherapy or therapy with neither, and an even higher risk with the use of both agents compared to either monotherapy 21. Therefore, the increasing prevalence of biologic therapy for IBD is our leading explanation for the observed era effect on infection.
We were unable to assess what type of infection was most prevalent in PSC-CD, but are able to report no significant differences in respiratory, viral, or fungal infections when analyzing the whole cohort. The above-mentioned study by Irles-Depe noted an increased rate of CMV infections in PSC-IBD, though we did not find any association with PSC-CD specifically 17. A retrospective cohort study published in 2022 evaluating risk of serious infection with vedolizumab versus TNF inhibitors in IBD subtypes noted a higher risk in CD patients treated with vedolizumab22. This included a higher rate of gastrointestinal infections in CD, including Clostridium difficile, possibly reflecting a direct complication of inadequately controlled disease activity. As mentioned above, there is a significant risk of flare-up of IBD activity in patients post-LT. It is therefore plausible that a phenotypic difference in PSC-CD is accounting for difficulties in controlling disease activity post-LT, which may directly lead to gastrointestinal infection or any infection secondary to increased need for immunosuppression including corticosteroids.
Limitations
Our study is limited by both retrospective design and the data available in the UNOS database. We could not isolate any specific infectious etiology after 2012 to characterize our findings in the PSC-CD cohort. Our study was also limited in that we could not specify baseline IBD disease activity or site of involvement, such as ileal CD, due to lack of endoscopic or histologic markers. We also lacked data on IBD-related pharmacotherapy in the baseline population. This baseline data will be necessary for further investigation into the higher rates of graft failure in PSC-CD. A prospective study that details the severity and phenotype of IBD in patients with PSC who undergo LT will be helpful in categorizing IBD subtypes and specific IBD-related complications and their impact on post-LT prognosis.
Conclusion
To our knowledge, this is the largest study of post-LT outcomes in patients with PSC-IBD and it is the only study to examine these outcomes in patients with PSC-CD compared to PSC-UC. A broad implication of our study is that PSC-CD and PSC-UC represent distinct clinical entities with potential differences in their pathogenesis, phenotypes, and outcomes. It therefore may be important for future research to address these two entities independently, as opposed to PSC-IBD as a whole. Overall, we found no difference in primary outcomes between the PSC-CD and PSC-UC. However, we found PSC-CD patients to suffer from a higher rate of fatal infections post-LT, especially when analyzing the cohort strictly after the year 2012.
References
Fosby B, Karlsen TH, Melum E. Recurrence and rejection in liver transplantation for primary sclerosing cholangitis. World J Gastroenterol 2012;18:1–15.
Karlsen TH, Folseraas T, Thorburn D, Vesterhus M. Primary sclerosing cholangitis - a comprehensive review. J Hepatol 2017;67:1298–1323.
Lazaridis KN, LaRusso NF. Primary sclerosing cholangitis. N Engl J Med 2016;375:1161–1170.
Durand F, Levitsky J, Cauchy F, Gilgenkrantz H, Soubrane O, Francoz C. Age and liver transplantation. J Hepatol 2019;70:745–758.
Barman PM, VanWagner LB. Cardiac risk assessment in liver transplant candidates: current controversies and future directions. Hepatology 2021;73:2564–2576.
Feng S, Goodrich NP, Bragg-Gresham JL et al. Characteristics associated with liver graft failure: the concept of a donor risk index. Am J Transplant 2006;6:783–790.
Ricciuto A, Kamath BM, Griffiths AM. The IBD and PSC Phenotypes of PSC-IBD. Curr Gastroenterol Rep 2018;20:16.
Linares R, Francés R, Gutiérrez A, Juanola O. Bacterial translocation as inflammatory driver in Crohn’s disease. Front Cell Dev Biol 2021;9:703310.
Mammadov RA, Selten JW, Roest HP, et al. Intestinal Bacteremia After Liver Transplantation is a Risk Factor for Recurrence of Primary Sclerosing Cholangitis. Transplantation. Published online March 29, 2023.
Altwegg R, Combes R, Laharie D et al. Effectiveness and safety of anti-TNF therapy for inflammatory bowel disease in liver transplant recipients for primary sclerosing cholangitis: a nationwide case series. Dig Liver Dis 2018;50:668–674.
van Meeteren WMJ, Hayee B, Inderson A et al. Safety of anti-TNF treatment in liver transplant recipients: a systematic review and meta-analysis. J Crohns Colitis 2017;11:1146–1151.
Jørgensen KK, Lindström L, Cvancarova M et al. Immunosuppression after liver transplantation for primary sclerosing cholangitis influences activity of inflammatory bowel disease. Clin Gastroenterol Hepatol 2013;11:517–523.
Thuluvath PJ, Thuluvath AJ, Savva Y, Zhang T. Karnofsky performance status following liver transplantation in patients with multiple organ failures and probable acute-on-chronic liver failure. Clin Gastroenterol Hepatol 2020;18:234–241.
Fine JP, Gray RJ. A proportional hazards model for the subdistribution of a competing risk. J Am Stat Assoc 1999;94:496–509.
Stekhoven DJ, Bühlmann P. MissForest–non-parametric missing value imputation for mixed-type data. Bioinformatics 2012;28:112–118.
Joshi D, Bjarnason I, Belgaumkar A et al. The impact of inflammatory bowel disease post-liver transplantation for primary sclerosing cholangitis. Liver Int 2013;33:53–61.
Irlès-Depé M, Roullet S, Neau-Cransac M et al. Impact of preexisting inflammatory bowel disease on the outcome of liver transplantation for primary sclerosing cholangitis. Liver Transpl 2020;26:1477–1491.
Weismüller TJ, Trivedi PJ, Bergquist A et al. Patient age, sex, and inflammatory bowel disease phenotype associate with course of primary sclerosing cholangitis. Gastroenterology 2017;152:1975-1984.e8.
Ravikumar R, Tsochatzis E, Jose S et al. Risk factors for recurrent primary sclerosing cholangitis after liver transplantation. J Hepatol 2015;63:1139–1146.
Singh JA, Wells GA, Christensen R et al. Adverse effects of biologics: a network meta-analysis and Cochrane overview. Cochrane Database Syst Rev 2011;2011:CD008794.
Kirchgesner J, Lemaitre M, Carrat F, Zureik M, Carbonnel F, Dray-Spira R. Risk of serious and opportunistic infections associated with treatment of inflammatory bowel diseases. Gastroenterology. 2018;155:337-346.e10.
Singh S, Heien HC, Herrin J et al. Comparative risk of serious infections with tumor necrosis factor α antagonists vs vedolizumab in patients with inflammatory bowel diseases. Clin Gastroenterol Hepatol 2022;20:e74–e88.
Funding
This study was funded by NIH NIDDK T32 DK067872-17.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of interest
The authors of this manuscript certify they share no affiliation or involvement with any organization or entity with any financial interest or non-financial interest in the subject matter or materials discussed in this manuscript. None declared.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Supplementary Information
Below is the link to the electronic supplementary material.
Rights and permissions
Springer Nature or its licensor (e.g. a society or other partner) holds exclusive rights to this article under a publishing agreement with the author(s) or other rightsholder(s); author self-archiving of the accepted manuscript version of this article is solely governed by the terms of such publishing agreement and applicable law.
About this article
Cite this article
Lee, D.U., Menegas, S., Lee, K.J. et al. Impact of Inflammatory Bowel Disease Subtypes on the Post-liver Transplant Outcomes of Patients with Primary Sclerosing Cholangitis. Dig Dis Sci 68, 3781–3800 (2023). https://doi.org/10.1007/s10620-023-08023-y
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s10620-023-08023-y