Abstract
Background
Urban–rural differences in IBD-specific health care utilization at the national level have not been examined in the USA.
Aims
We compared urban and rural rates of IBD-related office visits and IBD-specific (Crohn’s disease (CD) or ulcerative colitis (UC)) hospitalizations and emergency department (ED) visits.
Methods
From multiple national data sources, we compared national rates using Z test and compared estimates of patient and hospital characteristics and hospitalization outcomes between urban and rural areas using Chi-square and t tests.
Results
In 2015 and 2016, digestive disease-related office visit rates, per 100 adults, were 3.1 times higher in urban than in rural areas (8.7 vs 2.8, P < 0.001). In 2017, age-adjusted rates per 100,000 adults were significantly higher in rural than urban areas for CD-specific hospitalizations (26.3 vs 23.6, P = 0.03) and ED visits (49.3 vs 39.5, P = 0.002). Compared with their urban counterparts, rural adults hospitalized for CD or UC in 2017 were more likely to be older and non-Hispanic white, have lower household income, Medicare coverage, and an elective admission, and were discharged from hospitals that were large, non-federal government owned, and in the Midwest or South. There were no significant urban–rural differences in length of stay and 30-day readmission rate.
Conclusions
While IBD or digestive disease-related office visit rates were lower in rural compared to urban areas, CD-specific hospitalization and ED visit rates were higher. Strategies that improve office-based care among rural patients with IBD may help to avoid more costly forms of health care use.
Similar content being viewed by others
Explore related subjects
Discover the latest articles, news and stories from top researchers in related subjects.Avoid common mistakes on your manuscript.
Introduction
Inflammatory bowel disease (IBD), encompassing Crohn’s disease (CD) and ulcerative colitis (UC), is characterized by chronic inflammation of the gastrointestinal tract [1]. Based on the 2015 National Health Interview Survey (NHIS), three million (1.3%) US adults reported having either CD or UC [2]. IBD treatment has advanced in recent decades that includes complex medication regimens and therapeutic strategies [3]. Therefore, regular interactions with a gastroenterologist and timely outpatient follow-up are crucial to maintain treatment regimens, which may decrease the likelihood of unplanned acute care such as emergency department (ED) visits. For example, a Canadian study found that limited access to outpatient care was associated with IBD-related ED visits [4], while another study found that visits to a gastroenterologist in the prior year could significantly lower the likelihood of ED visits [5]. Routine specialist care to help closely monitor patient symptoms and timely adjust IBD medications has been demonstrated to improve patient outcomes, especially within the first year of diagnosis [6].
Findings from previous research suggest adults living in rural areas may have disproportionate health care utilization with lower rates of outpatient specialist care and higher rates of acute care services compared with their urban counterparts [7,8,9,10,11,12,13]. A systematic review evaluating differences in overall health care utilization found that frequencies of office visits, diagnostic or imaging tests, medical procedures, and seeing a medical specialist were significantly lower in rural areas than urban areas [12]. A previous study found that patients with IBD living in urban areas were more likely to visit specialists than those living in rural areas because urban areas have a higher density of specialists [11]. In addition, the barriers to health care access that rural residents often encounter, such as no insurance or underinsurance, long distance travel to visit a doctor’s office, and lack of access to medical specialists [14], may influence patterns of health care utilization.
There are no current national estimates of urban–rural differences in health care utilization related to IBD in the USA. Given that the prevalence of IBD in 2015 was similar in urban areas (1.4% in metropolitan statistical area [MSA] non-central city and 1.0% in MSA central city) and in rural areas (1.2% in micropolitan or non-core) [2], examining national level urban–rural differences in health care utilization related to IBD may help identify health equity issues related to health care utilization access in rural areas and help inform potential strategies to address them. In this study, we sought to compare between urban and rural areas the national rates of digestive disease-related office visits and IBD-specific hospitalizations and ED visits, overall and by age group and sex. We also examined differences in IBD-specific inpatient and hospital characteristics and outcomes for CD and UC between urban and rural areas.
Methods
Data Sources and Measures
We used the following data sources to produce estimates in this study: 2015 and 2017 Area Health Resource File (AHRF), 2011–2016 National Ambulatory Medical Care survey (NAMCS), and Healthcare Cost and Utilization Project (HCUP) databases [2010–2017 National Inpatient Sample (NIS); 2010–2017 Nationwide Emergency Department Sample (NEDS); 2017 Nationwide Readmission Database (NRD)] (Table 1). For estimating IBD-specific office-based visit rate, we used the weighted number of adults with IBD by urban and rural areas based on a previously published report, estimated from 2015 NHIS [2]. In addition, we used 2018 Vintage postcensal population files to obtain population totals at the county level for the corresponding years [15].
The AHRF, sponsored by the Health Resources and Services Administration, includes information such as health care professions, population characteristics, and economics at the county and state level [16]. This dataset contains, for each county, the number of gastroenterologists (patient care-based, office-based, hospital-based) and population characteristics including distribution of age groups (18‒44, 45‒64, and ≥ 65 years) and sex, and the number of adults living below the poverty level, the number of adults with less than a high school diploma, and the number of adults aged younger than 65 years who were uninsured (per 100 population) [16].
The NAMCS, conducted by the National Center for Health Statistics (NCHS), CDC, is an annual national survey to collect information about use of ambulatory care services based on sample visits to non-federally employed office-based physicians [17]. The dataset contains patient visit weights used to generate national estimates of total visits. We identified digestive disease-related office-based visits based on the first-listed IBD diagnosis codes (CD: International Classification of Diseases, Clinical Modification (ICD-9-CM): 555 and ICD-10-CM: K50; UC: ICD-9-CM: 556 and ICD-10-CM: K51) or based on digestive disease-related based on reason of office visit to physician’s location including disease of digestive system code (26,500‒26,990) according to Visit Classification for Ambulatory Care defined in the public use file documentation [18]. To increase sample size, we calculated average office-based visit rates (per 100 adult population) from two-year combined data (2011–2012, 2013–2014, 2015–2016) based on the corresponding US populations [16]. We also calculated average IBD-specific office-based visit rates (per 100 adults with IBD) from three-year combined data (2014–2016) based on first-listed IBD diagnosis codes and weighted number of adults with IBD by urban–rural status from the 2015 NHIS [2].
HCUP, sponsored by the Agency for Healthcare Research and Quality, is a collection of all-payer, encounter-level health care databases that include health services utilization, outcomes, and costs [19]. HCUP’s NIS contains data on hospitalizations, and the NEDS and NRD contain data on ED visits and hospital readmissions, respectively. These samples are designed to produce national estimates of health care utilization based on the survey design and weights. We used NIS and NEDS to identify US adults aged 18 years or older with Crohn’s disease (ICD-10-CM: K50) or ulcerative colitis (ICD-10-CM: K51). Information on age group (18‒44, 45‒64, and ≥ 65 years) and sex is available from NIS and NEDS.
For CD- or UC-specific hospitalizations from 2017 NIS, we defined additional variables including quartiles of median household income at zip code, payer (Medicare, Medicaid, Private insurance, self-pay, and others or no charge), mental illness (depression or anxiety) with algorithm derived elsewhere [20], severity of illness subclass as a measure of loss of function (minor, moderate, major or extreme) according to patients’ extent of physiologic decompensation or organ system loss of function and likelihood of death [21], elective admissions, hospital bed size (small, medium, and large), hospital ownership (government non-federal, private non-profit, private investor-owned), hospital region (northeast, midwest, south, and west), hospital location/teaching status (rural, urban non-teaching, and urban teaching), and hospitalization outcomes including length of stay (days) and total costs ($). We calculated the other hospitalization outcome, 30-day readmission rate, from the NRD, which we defined as all-cause readmissions from the index admission with CD or UC as the primary diagnosis.
According to the NCHS Urban–Rural Classification Scheme for Counties [22], large central metro, large fringe metro, medium metro, and small metro were grouped as urban areas, and micropolitan and non-core were grouped as rural areas. The NCHS urban–rural classification is available in NAMCS, NHIS, and all HCUP nationwide databases. The AHRF and population files were merged by county FIPS code and then merged with the crosswalk file containing county FIPS code and urban–rural classification scheme.
Statistical Analysis
Table 1 describes the study measures from the corresponding data sources. As the main analysis, we estimated the distribution of select demographic characteristics, number of gastroenterologists, ratio of adults with IBD to number of gastroenterologists, and rates of digestive disease-related or IBD-specific office visits in urban and rural areas in 2017. We also estimated overall crude rates of hospitalizations and ED visits in urban and rural areas. Age-adjusted rates were based on the 2000 US Standard Population [23]. Crude rates were also estimated stratified by age group and sex. We used Z tests to compare distributions and rates between urban and rural areas at the 0.05 significance level.
For inpatient and hospital characteristics in 2017, we estimated weighted percentages with 95% confidence intervals for categorical variables and weighted means with standard errors for continuous variables. Length of stay was transformed using a natural logarithm to achieve normality to fit a linear regression. To compare estimates between urban and rural areas, we used Chi-square for categorical variables and t tests for continuous variables.
To compare 2017 rates of hospitalizations and ED visits, we performed a sensitivity analysis to calculate age-adjusted rates from 2010 to 2016. To examine the rate change from 2010 to 2017, we performed a trends analysis, by constructing weighted linear models on the inversed standard errors from annual estimates, regressing rates (natural logarithm transformed) on year, rural residency (yes or no), and an interaction term between rural residency and year. Based on the coefficients from rural residency and the interaction term, we plotted predicted rate ratios (rural vs. urban, back transformed) to assess rate ratio changes across years.
We used SAS-callable SUDAAN 11.0.3 (Research Triangle Institute, Research Triangle Park, North Carolina), SAS 9.4 (SAS Institute, Cary, North Carolina), accounting for weights and complex survey design, and R 4.0.3.
Ethical Considerations
The AHRF, population files, and NAMCS data are publicly available databases. The HCUP data are limited data sets in which direct identifiers, as specified in the Health Insurance Portability and Accountability Privacy Rule, have been removed. Institutional Review Board approval was not required for this study.
Results
Population Characteristics and IBD-Related Office-Based Visits by Urban and Rural Residency
Compared with adults living in urban areas, rural residents were more likely to be aged 65 years or older, men, live below the poverty level, have less than a high school diploma, and have no health insurance among adults younger than 65 years (Table 2, P < 0.001). Per 100,000 population, the total number of gastroenterologists was 4.7 times higher in urban compared to rural areas (P < 0.001). The ratio of adults with IBD to total gastroenterologists in 2015 was about 4.7 times higher in rural than urban areas. The average weighted numbers of UC-specific office-based visits (2014–2016 combined) were 1.5 and 4.6 times higher than CD-specific office-based visits in urban and rural areas, respectively. The two-year average digestive disease-related office-based visit rates from 2011 to 2016 (per 100 adult population) were 2.1–3.1 times higher in urban than rural areas (P < 0.001). The three-year (2014–2016) average IBD-specific office visit rate (per 100 adults with IBD) was 8.8 times higher in urban than rural areas (P < 0.001).
National Rates of IBD-Specific Hospitalizations and ED Visits by Age, Sex, and Urban and Rural Residency, 2017
The weighted numbers of hospitalizations and ED visits were about 1.6–2.1 times as high for CD as for UC regardless of urban–rural status. Rural areas had higher age-adjusted rates per 100,000 population compared to urban areas for CD-specific hospitalizations (26.3 vs 23.6, P = 0.03), and ED visits (49.3 vs 39.5, P = 0.002) (Table 3). Compared with those in urban areas, CD-specific hospitalization rates were higher in rural areas among women (P = 0.002) and among adults aged 45–64 years (P = 0.02); CD-specific ED rates were higher in rural areas among women and among adults younger than 65 years (P ≤ 0.005). Overall, there were no significant urban–rural differences in overall or stratified estimates of acute care use for UC.
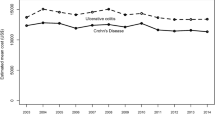
Sensitivity Analysis and Trends Analysis
The sensitivity analysis confirmed that for each time point, the CD-specific ED visit rate was generally higher in rural than urban areas from 2010 to 2017 (differences were significant except for 2010 and 2012) and that the UC-specific ED visit rate did not differ by urban–rural status (Supplementary Table). CD-specific hospitalization rates tended to be higher in rural than urban areas, and UC-specific hospitalization rates were generally higher in urban than rural areas; however, differences only reached significance in 2013, 2016, and 2017 for CD and 2015 and 2016 for UC. When assessing predicted hospitalization rate ratios (rural vs. urban) across years, we found that they were higher for CD but lower for UC (Supplementary Figure). For CD, the magnitude of the predicted ED visit rate ratio (rural vs urban) was larger in more recent years. Over time, the predicted UC-specific ED visit rate ratio changed from below 1 to above 1 although the difference was not significant in more recent years.
Characteristics and Outcomes of IBD-Specific Hospitalization by Urban and Rural Residency, 2017
Among those hospitalized for CD (49,590 discharges in urban areas and 8,875 discharges in rural areas) or UC (30,275 discharges in urban areas and 4,910 discharges in rural areas), compared with their urban counterparts, rural patients were more likely to be older and non-Hispanic white, have lower median household income and Medicare coverage, have an elective admission, and be discharged from a hospital characterized as large, non-federal government owned, and located in the Midwest or South region (P < 0.05, Table 4). Rural patients hospitalized for CD compared to their urban counterparts were more likely to be women (P = 0.002) and have depression (P = 0.02). There were no urban–rural differences in hospitalization outcomes, including length of stay, and 30-day readmission for both CD- and UC-specific hospitalizations (Table 5). However, urban patients hospitalized for CD were more likely to have higher mean total costs than their rural counterparts (P < 0.001).
Discussion
To the best of our knowledge, this is the first study assessing urban–rural differences in national estimates of health care utilization among patients with IBD in the US. The study highlighted that while IBD-specific or digestive disease-related office visit rates were consistently lower in rural than urban areas over time, CD-specific rates of hospitalization and ED visits were generally higher, and the difference was more pronounced for the ED visit rate.
The current study indicated different patterns in health care utilization by urban–rural status and IBD disease type. In 2017, acute care utilization was higher in rural than urban areas for CD, but it was not different for UC by urban–rural status. The weighted numbers of hospitalizations and ED visits were 1.6–2.1 times higher for CD than for UC in 2017, regardless of urban–rural status. However, the weighted number of CD-specific office-based visits was 32% lower than UC-specific office-based visits in urban areas and much lower (78%) in rural areas in 2014–2016. Meanwhile, the study also showed that rural residents younger than 65 years were more likely to be uninsured than their urban counterparts and that patients hospitalized for CD or visiting ED tended to be younger than patients with UC in 2017. Although this study did not assess health care insurance coverage by disease type, age might be associated with status of health care insurance and adequacy of insurance coverage, which might subsequently affect specialist care access. The trends analysis confirmed that predicted rates of acute care utilization stayed higher in rural than urban areas for CD over time. The magnitude of ED visit rate ratio for both CD and UC between rural and urban areas over time indicated a temporal trend of IBD-specific ED utilization burden in rural areas which was consistent with the findings from a previous study assessing trends of all ED utilizations by urban–rural status [10]. Future studies are warranted to assess urban–rural differences in other IBD routine care such as outpatient visits and medication use during the biologic era to understand the pattern of overall health care utilization by disease type.
Several potential factors may be associated with observed rural–urban differences in utilization and outcomes. One barrier for patients with IBD in rural areas is a shortage of gastroenterologists. The current study found fewer gastroenterologists in rural compared to urban areas. This finding is supported by a systematic review that identified a shortage of specialists in areas with smaller populations [9]. Under this circumstance, rural patients may rely more on primary care physicians and not receive sufficient IBD-specific care. A previous study reported that patients with IBD in rural areas in Germany were less likely to see a gastroenterologist and subsequently more likely to receive fewer medications than those in urban areas [11]. Routine office visits to gastroenterologists and maintaining medication regimens are critical in IBD management.
Longer travel distances needed to see a gastroenterologist may also explain the lower utilization of office-based visits and higher acute care utilization related to CD that were observed in rural adults compared to their urban counterparts. A single referral center including over 2,000 patients with IBD showed that longer distance may affect the timing of initiation of medication therapy, which could impact the need for subsequent hospitalization [8]. While longer travel distance could be a barrier for seeking outpatient care, we found that almost 60% of IBD-specific hospital discharges associated with rural residency were from urban hospitals and that rural patients were more likely to have an elective admission than urban patients. An ad-hoc analysis further showed that rural patients with IBD who were admitted in urban hospitals were more likely to have an elective admission than those admitted in rural hospitals and that 30% IBD-specific ED visits associated with rural residency were in urban hospitals in 2017 (results not shown). It is unclear whether it was due to transfer or patients’ choice, although a previous study showed that almost 50% of rural patients bypassed local facilities to have elective surgeries performed in urban hospitals, most of which are operations on musculoskeletal and digestive systems [24]. Another study reported that rural patients with IBD traveled long distance to urban hospitals because they were not confident in rural health care professionals on IBD management [25].
Financial challenges may be a more prevalent barrier to accessing office-based care in rural compared to urban areas. The current study showed higher percentages of poverty or not having health insurance among adults younger than 65 years of age in rural than urban areas. During the era of biologic therapy, health care costs have increased largely due to medications [26]. Because of underinsurance or no insurance, patients may not be able to afford out-of-pocket expenses for outpatient services such as office visits, medications, and laboratory or imaging facilities. A previous study showed that socioeconomic status was highly associated with patterns of IBD-specific health care utilization, where patients with private insurance were more likely to have outpatient access, office visits, and prescribed medications than patients with low income [27]. Furthermore, the current study confirmed that the median household income level was lower among rural patients who were hospitalized for IBD and that rural patients hospitalized for CD were less likely to have private insurance than their urban counterparts. Besides hospitalization, a previous study examining patterns of overall ED visits also found a disproportionate rise in ED visit in rural communities from 2005 to 2016, especially among socioeconomically disadvantaged populations [10]. In addition, rural hospitals have experienced financial viability challenges [28]. Therefore, the lack of health care resources combined with the financial challenges that rural patients with IBD may be more likely to experience may provide one explanation for the higher acute care utilization related to IBD observed in rural compared to urban areas.
The current study also found some distinct demographic characteristics associated with health care utilization that differed by urban–rural status. For example, women or patients younger than 65 years with CD in rural areas had greater acute care use than their urban counterparts. These findings may inform health care providers in identifying subpopulations in certain rural areas to focus on to increase IBD awareness and advocacy, health literacy, and education for overall disease management. In addition, compared with their urban counterparts, rural patients hospitalized for IBD were more likely to be 65 years or older or have Medicare, which was consistent with the findings in a previous study where older rural residents had a higher percentage of overall inpatient care than their counterparts [29]. Patients with IBD usually have more comorbidities including mental illnesses than those without IBD [30]. The current study found that rural patients hospitalized for CD were more likely to have depression than their urban counterparts. A previous NHIS study reported that depression was significantly higher in rural than urban areas [31]. Interestingly, the association was no longer significant after urban–rural characteristics were controlled for [31]. Our findings that a slightly elevated proportion of depression among rural patients hospitalized for CD may warrant future investigation.
Despite the differences by urban–rural status in certain patient characteristics, there was no difference in hospitalization outcomes in terms of length of stay and 30-day readmission by urban–rural setting, except for higher mean total costs among urban patients with CD. The findings showed that 77.8% urban patients and 46.8% rural patients were admitted to urban teaching hospitals. Teaching hospitals usually have more severe or emergent cases that involve more complicated procedures. For instance, a previous study showed that urban patients incurred higher total costs than rural patients did on deep brain stimulation surgery [32]. Another previous study also demonstrated higher direct costs in teaching hospitals than non-teaching or rural hospitals [33]. In the current study, mean total costs tended to be higher among urban than rural patients with UC as well although it was not significant. In addition, the findings showed that urban patients were less likely to have an elective admission than rural patients, indicating they were more likely to have an urgent or emergent admission which may influence mean total costs. Nonetheless, it is unclear whether urban patients with IBD tended to be sicker or not without detailed information about baseline disease severity and medication use.
The study findings highlight several public health implications. First, state and county health policy makers might consider ways to improve access to specialty care, especially in rural populations, which may help improve disease management and avoid more expensive acute care. Second, preventive care is important for patients with IBD [34] and efforts to improve IBD-specific care among primary care providers may improve IBD outcomes and utilization. In areas where gastroenterologist supply is low (e.g., rural areas), training of primary care physicians resulted in increased knowledge of treating patients with IBD from an educational intervention [35]. Because IBD care is complex, multidisciplinary care coordination among physicians is important for effective IBD management. Third, it is important to better understand the role of social determinants of health in patients with IBD, especially those adults in the rural setting, and how these may influence IBD management. An improved understanding of the role of financial challenges and lack of adequate insurance as barriers to regular IBD care can help identify strategies to address these issues. Finally, expanding telehealth and enhancing remote monitoring in rural areas have been shown to be treatment effective and cost efficient, improve patients’ adherence, enhance patient and physician communications to address IBD-specific issues as well as comorbidities, and ultimately improve patient quality of care [36, 37].
A strength of this study is the use of data from multiple national surveys to generate health care utilization rates at the national level. At least four limitations in this study are recognized. First, NIS is at discharge level, not patient level. Therefore, multiple discharges by the same patient cannot be accounted for. Second, the national estimates of health care utilizations were not estimated by race/ethnicity due to inaccurate or missing race/ethnicity values from NIS or the lack of such information from NEDS. Third, office-based visits defined using NAMCS were based on physicians' locations rather than patient residential locations due to restricted access to the latter information. Information regarding rural patients bypassing local clinics was unavailable for office visit. Therefore, we were unable to identify rural patients’ office visit in urban areas. Finally, one of the major limitations is that the HCUP data do not have measures about IBD severity and medication use. Therefore, we were not able to assess differences of health care utilization use by patients’ baseline conditions.
In conclusion, patterns of health care utilization for IBD differ by urban–rural status and by disease type. IBD or digestive disease-related office visit rates were lower in rural compared to urban areas. Our findings suggest that disparities exist in access to and use of routine office-based health care exist for adults with IBD residing in rural areas. Strategies to increase routine office-based care among rural patients with IBD may help to promote better disease management and thereby avoid more costly forms of health care use.
References
Abraham C, Cho JH. Inflammatory bowel disease. N Engl J Med. 2009;361:2066–2078.
Dahlhamer JM, Zammitti EP, Ward BW, Wheaton AG, Croft JB. Prevalence of inflammatory bowel disease among adults aged ≥18 years - United States, 2015. MMWR Morb Mortal Wkly Rep. 2016;65:1166–1169.
Grevenitis P, Thomas A, Lodhia N. Medical therapy for inflammatory bowel disease. Surg Clin North Am. 2015;95:1159–1182.
Nguyen GC, Bouchard S, Diong C. Access to specialists and emergency department visits in inflammatory bowel disease: a population-based study. J Crohns Colitis. 2019;13:330–336.
Nugent Z, Singh H, Targownik LE, Strome T, Snider C, Bernstein CN. Predictors of emergency department use by persons with inflammatory bowel diseases: a population-based study. Inflamm Bowel Dis. 2016;22:2907–2916.
Nguyen GC, Nugent Z, Shaw S, Bernstein CN. Outcomes of patients with Crohn’s disease improved from 1988 to 2008 and were associated with increased specialist care. Gastroenterology. 2011;141:90–97.
Benchimol EI, Kuenzig ME, Bernstein CN et al. Rural and urban disparities in the care of Canadian patients with inflammatory bowel disease: a population-based study. Clin Epidemiol. 2018;10:1613–1626.
Borren NZ, Conway G, Tan W et al. Distance to specialist care and disease outcomes in inflammatory bowel disease. Inflamm Bowel Dis. 2017;23:1234–1239.
Cyr ME, Etchin AG, Guthrie BJ, Benneyan JC. Access to specialty healthcare in urban versus rural US populations: a systematic literature review. BMC Health Ser Res. 2019;19:974.
Greenwood-Ericksen MB, Kocher K. Trends in emergency department use by rural and urban populations in the United States. JAMA Netw Open. 2019;2:e191919.
Lange A, Prenzler A, Bachmann O et al. Regional differences in health care of patients with inflammatory bowel disease in Germany. Health Econ Rev. 2015;5:29.
Spoont M, Greer N, Su J, Fitzgerald P, Rutks I, Wilt TJ. VA evidence-based synthesis program reports. In: Rural vs. Urban Ambulatory Health Care: A Systematic Review. Washington DC: Department of Veterans Affairs (US); 2011.
Kuenzig ME, Nguyen GC, Benchimol EI. Rural and Urban differences in the risk of inflammatory bowel disease and subsequent health services utilization in Ontario. Healthc Q. 2019;22:6–9.
Center for Disease Control and Prevention. Health, United States, 2001 urban and rural health chartbook. 2001; Available from https://www.cdc.gov/nchs/data/hus/hus01cht.pdf. Accessed March 4, 2021.
National Center for Health Statistics. Vintage 2018 bridged-race postcensal population estimates. 2018; Available from https://www.cdc.gov/nchs/nvss/bridged_race/data_documentation.htm#Vintage2018. Accessed March 4, 2021.
Health Resources & Services Administration. Area Health Resource Files. 2017; Available from https://www.hcup-us.ahrq.gov/. Accessed March 4, 2021.
National Center for Health Statistics. About the Ambulatory Health Care Surveys. 2015; Available from https://www.cdc.gov/nchs/ahcd/about_ahcd.htm#NAMCS. Accessed March 4, 2021.
National Center for Health Statistics. 2015 NAMCS micro-data file documentation. 2015; Available from ftp://ftp.cdc.gov/pub/Health_Statistics/NCHS/Dataset_Documentation/NAMCS/doc2015.pdf. Accessed May 14, 2021.
Agency for Healthcare Research and Quality. Healthcare Cost and Utilization Project (HCUP). 2017; Available from https://www.hcup-us.ahrq.gov/. Accessed March 4, 2021.
Chronic Conditions Data Warehouse. Conditon categories. 2020; Available from https://www2.ccwdata.org/web/guest/condition-categories. Accessed March 4, 2021.
Agency for Healthcare Research and Quality. Overview of disease severity measures disseminated with Nationwide Inpatient Sample (NIS) and Kids' Inpatient Database (KID). Available from https://www.hcup-us.ahrq.gov/db/nation/nis/OverviewofSeveritySystems.pdf. Accessed March 4, 2021.
National Center for Health Statistics. NCHS Urban-Rural Classification Scheme for Counties. 2017; Available from https://www.cdc.gov/nchs/data_access/urban_rural.htm. Accessed January 11, 2021.
Klein RJ, Schoenborn CA. Age adjustment using the 2000 projected U.S. population. Healthy People 2000 Stat Notes. 2001:1–9.
Weigel PAM, Ullrich F, Finegan CN, Ward MM. Rural bypass for elective surgeries. J Rural Health. 2017;33:135–145.
Rohatinsky N, Boyd I, Dickson A et al. Perspectives of health care use and access to care for individuals living with inflammatory bowel disease in rural Canada. Rural Remote Health. 2021;21:6358.
Pillai N, Dusheiko M, Maillard MH et al. The evolution of health care utilisation and costs for inflammatory bowel disease over ten years. J Crohns Colitis. 2019;13:744–754.
Park MD, Bhattacharya J, Park K. Differences in healthcare expenditures for inflammatory bowel disease by insurance status, income, and clinical care setting. PeerJ. 2014;2:e587.
Kaufman BG, Thomas SR, Randolph RK et al. The rising rate of rural hospital closures. J Rural Health. 2016;32:35–43.
Hall MJ, Owings M. Rural and urban hospitals’ role in providing inpatient care, 2010. NCHS Data Brief. 2014;147:1–8.
Xu F, Dahlhamer JM, Zammitti EP, Wheaton AG, Croft JB. Health-risk behaviors and chronic conditions among adults with inflammatory bowel disease - United States, 2015 and 2016. MMWR Morb Mort Wkly Rep. 2018;67:190–195.
Probst JC, Laditka SB, Moore CG, Harun N, Powell MP, Baxley EG. Rural-urban differences in depression prevalence: implications for family medicine. Fam Med. 2006;38:653–650.
Fana M, Everett G, Fagan T, Mazzella M, Zahedi, Clements JM. Procedural outcomes of deep brain stimulation (DBS) surgery in rural and urban patient population settings. J Clin Neurosci. 2020;72:310–315
Dalal RS, Vajravelu RK, Lewis JD, Lichtenstein GR. Hospitalization outcomes for inflammatory bowel disease in teaching vs nonteaching hospitals. Inflamm Bowel Dis. 2019;25:1974–1982.
Farraye FA, Melmed GY, Lichtenstein GR, Kane SV. ACG Clinical Guideline: Preventive care in inflammatory bowel Disease. Am J Gastroenterol. 2017;112:241–258.
Alharbi R, Almahmudi F, Makhdoom Y, Mosli M. Knowledge and attitudes of primary healthcare physicians toward the diagnosis and management of inflammatory bowel disease following an educational intervention: A comparative analysis. Saudi J Gastroenterol. 2019;25:277–285.
George LA, Dominic MR, Cross RK. Integration of telemedicine into clinical practice for inflammatory bowel disease. Curr Opin Gastroenterol. 2020;36:304–309.
Ruf B, Jenkinson P, Armour D, Fraser M, Watson AJ. Videoconference clinics improve efficiency of inflammatory bowel disease care in a remote and rural setting. J Telemed Telecare. 2020;26:545–551.
Acknowledgments
The findings and conclusions in this report are those of the authors and do not necessarily represent the official position of the Centers for Disease Control and Prevention.
Funding
No financial disclosures were reported by the authors of this paper.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of interest
All authors have no conflicts of interest to disclose. All authors received no funding for this work.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Supplementary Information
Below is the link to the electronic supplementary material.
Rights and permissions
About this article
Cite this article
Xu, F., Carlson, S.A., Liu, Y. et al. Urban–Rural Differences in Health Care Utilization for Inflammatory Bowel Disease in the USA, 2017. Dig Dis Sci 67, 3601–3611 (2022). https://doi.org/10.1007/s10620-021-07264-z
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s10620-021-07264-z