Abstract
Background
Mucosal healing (MH) has emerged as a therapeutic goal in the treatment of inflammatory bowel disease; however, little is known about the impact of MH on the prognosis of intestinal Behçet’s disease (BD).
Aim
We investigated whether MH could predict the prognosis of intestinal BD.
Methods
We retrospectively reviewed the medical records of 80 patients with intestinal BD who underwent colonoscopy within 3 months after clinical remission. The clinical recurrence rate according to the presence or absence of MH was evaluated using the Kaplan–Meier method and the log-rank test. In order to evaluate MH as an independent prognostic factor, a multivariate analysis using Cox proportional hazards regression model was performed including other potential factors for the relapse of intestinal BD.
Results
The number of patients with active ulcers at the time of clinical remission was 57 (71.3 %), while 23 patients (28.7 %) were experiencing MH. In the active ulcer group, 39 patients (68.4 %) experienced recurrence during the follow-up period, whereas 7 patients (30.4 %) recurred in the MH group. The cumulative recurrence rate was significantly higher in the active ulcer group than in the MH group (P < 0.001). A multivariate analysis identified active ulcers at the time of clinical remission as an independent predictive factor for relapse.
Conclusion
Our study demonstrates that MH is an independent factor predictive of long-term prognosis of intestinal BD. MH might be the ultimate therapeutic goal in the treatment of intestinal BD.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Behçet’s disease (BD) is a multi-systemic disorder characterized by repeated oral and genital ulcerations, ocular lesions, skin manifestations, arthritis, vasculitis, and gastrointestinal involvements [1, 2]. Intestinal BD is a specific subtype of BD, which is clinically diagnosed when endoscopic examinations reveal typically shaped ulcers in the gastrointestinal tract, mainly in the ileocecal area of patients with systemic BD [3, 4]. Although the incidence of intestinal BD is relatively low, affecting about 3–16 % of all patients with BD, its predominant symptoms such as abdominal pain, diarrhea, hematochezia, fistula tract formation, and perforation often limit patient quality of life [5, 6].
Similar to inflammatory bowel disease (IBD), intestinal BD is considered to be a chronic inflammatory disease characterized by a heterogeneous range of clinical courses and symptoms [7]. A considerable number of patients with intestinal BD are unresponsive to treatment and often have to undergo surgery; the long-term prognosis is relatively poor in these cases. Therefore, it is of paramount importance to investigate the prognostic factors of the disease so that administration of early and proper treatment can be achieved.
Over the past few years, mucosal healing (MH) has emerged as a major therapeutic goal in various clinical trials for IBD. Accumulating evidence indicates that MH may change the natural course of the disease by decreasing the need for surgery and reducing hospitalization rates in both ulcerative colitis (UC) and Crohn’s disease (CD) [8–13]. Although MH is one of the most important prognostic factors for IBD, little is known about the effects of MH on the clinical course of intestinal BD. To the best of our knowledge, an investigation of the relationship between MH and intestinal BD has not yet been reported. Therefore, the aim of our study was to evaluate the effects of MH on the long-term outcome of intestinal BD.
Materials and Methods
Study Subjects
We reviewed the medical records of intestinal BD patients who were diagnosed at Severance Hospital, Yonsei University College of Medicine, Seoul, Korea, between January 1986 and December 2011. The diagnosis of intestinal BD was made in accordance with previously established criteria based on colonoscopic features and clinical manifestations using a modified Delphi process [14]. Patients were classified as experiencing definite, probable, or suspected intestinal BD [14].
Intestinal ulcerations were divided into “typical” and “atypical” ulcerations based on colonoscopic findings. Lesions with fewer than five ulcers, which were round or oval in shape, deep, with discrete borders, and located in the ileocecal area were defined as typical ulcerations. Ulcerations that did not fulfill all of these characteristics were defined as atypical ulcerations [15]. As there is no pathognomonic finding that can be used to definitively diagnose intestinal BD, the sequential elimination of differential diagnoses for intestinal lesions remains the current method for diagnosing patients with BD. Enteropathies from other causes such as NSAIDs were ruled out, and if there was any uncertainty, we postponed the final diagnosis of intestinal BD.
For this study, we recruited patients who had been confirmed to have intestinal BD by colonoscopy and underwent follow-up colonoscopy within 3 months after clinical remission by searching our internal electronic medical record database system. In our experience, ulcerations of intestinal BD heal slowly and are relatively indolent; therefore, we accepted the time difference of <3 months between clinical remission and endoscopic remission. Clinical remission was defined as a Disease Activity Index for Intestinal BD (DABID) score <20 [16].
This study was approved by the Severance Hospital Institutional Review Board. The Strengthening the Reporting of Observational Studies in Epidemiology Statement was used as a reference for guidelines related to study design and reporting.
Clinical and Colonoscopic Evaluations at the Time of Remission
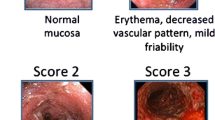
We investigated demographic factors as well as gastrointestinal and systemic symptoms at the time of clinical remission. All colonoscopic findings of ulcerative lesions and other mucosal findings were reviewed by two experienced endoscopists (J. H. Cheon and D. H. Kim). In discordant cases, investigators ranked the priority of decision according to shape and location of those ulcerations and determined the type of ulcerations by discussion until reaching an agreement. The distribution was described as localized, segmental, or diffuse. Lesions involving only one segment of the bowel were considered as having localized involvement, while lesions involving two or more segments were considered as having diffuse involvement. We analyzed the segment of the intestine in which predominant ulcers were located, and the number of ulcers was classified solitary, two to five, or more than five. The depth was described as shallow or deep, and the shape was categorized as either round, oval, geographic, or volcano-shaped [17]. The margin of ulcers was divided into two categories, discrete or ill-defined. MH was defined as endoscopic complete resolution of all inflammatory and ulcerative lesions (except focal hyperemic lesions) at the time of clinical remission [18–20].
Follow-Up Evaluations at the Time of Disease Relapse
The patients’ medical records were followed until they had a disease relapse or until their last visit. Relapse was defined as a change in the physician’s global assessment (PGA), admission to the hospital, surgery related to the disease, or addition of medications such as corticosteroids or immunomodulators after clinical remission of intestinal BD. The PGA includes four categories: remission, mild, moderate, and severe disease activity. Disease activities were defined by DABID. If a patient’s DABID score was <20, the disease activity was considered to be in remission, a DABID score from 20 to 39 indicated the disease activity was mild, a score of 40–74 indicated the disease activity was moderate, and a DABID score greater than 75 was considered severe [16]. If a patient was admitted to the hospital, due to aggravation of intestinal BD after colonoscopy or radiologic examinations and needed to be treated with intravenous corticosteroids or immunomodulators, he/she was reported as a relapse in this study. Oral azathioprine as an immunomodulator was administered up to 2–2.5 mg/kg per day if well tolerated by the patients. Immunomodulator therapy was indicated in cases of steroid refractoriness or dependency [21]. If the patient received only conservative management or was hospitalized because of other diseases, the admission was not recorded for the purposes of this study.
Predictors of Disease Relapse and Statistical Analysis
We conducted our analyses using SPSS Window release Version 18.0 (SPSS Inc., Chicago, IL, USA). Continuous variables were compared by Mann–Whitney U test and are presented in this paper as median values (range). Categorical variables were analyzed using Fisher’s exact test. The clinical recurrence rate, according to the presence or absence of MH, was evaluated using the Kaplan–Meier method and the log-rank test. To explore the variable “MH” as an independent prognostic factor, a multivariate analysis using Cox proportional hazards regression model was performed and included other potential factors for the relapse of intestinal BD. P values <0.05 were considered statistically significant.
Results
Clinical Characteristics of Patients with Active or Healed Ulcers at the Time of Clinical Remission
A total of 80 patients with intestinal BD in clinical remission were included in the study. There were 32 males and 48 females whose median follow-up duration was 10.5 months (1–89 months), and the median age at diagnosis was 41 years (15–64 years). There were no patients who were treated with biologic agents. Baseline clinical and colonoscopic characteristics of patients are summarized in Table 1.
At the time of confirmed clinical remission, 23 patients were experiencing MH and 57 patients still had active ulcerations. A majority of intestinal lesions were distributed locally (52 patients, 91 %), but some lesions were segmentally (3 patients, 5.3 %) or diffusely (2 patients, 3.5 %) distributed. Thirty-one patients (54.4 %) experienced solitary intestinal ulcers, 20 patients (35.1 %) had between two and five ulcers, and 6 patients (10.5 %) were documented to have more than 5 ulcers. The shapes of ulcers were round or oval in 32 cases (56.1 %), geographic in 21 (36.8 %), and volcano-shaped in 4 (7.0 %) patients. Thirty-two ulcers (56.1 %) had discrete margins, and 16 (28 %) ulcers were classified as “typical” (Table 2).
Cumulative Probabilities of Clinical Relapse According to Ulcer State at the Time of Clinical Remission
As aforementioned, we defined clinical relapse as a change in the PGA, hospital admission due to aggravation of intestinal BD, surgery related to the disease, or addition of medications after clinical remission of intestinal BD. After clinical remission was achieved, 39 patients (68.4 %) in the active ulcer group showed clinical relapse, while only seven patients (30.4 %) in the MH group relapsed. The cumulative recurrence rate was significantly higher in the active ulcer group than in the MH group (P < 0.001; Fig. 1). Considering the number of relapse-qualifying events, the change in PGA from remission to mild, moderate, or severe disease state showed a higher relapse rate in the active ulcer group than in the MH group (P < 0.001; Fig. 2a). Cumulative probability of admission was also revealed to be statistically higher in the active ulcer group than in the MH group (P = 0.004; Fig. 2b). Cumulative surgery rate and cumulative rate of change in medications showed similar results (P = 0.017 and P = 0.002, respectively; Fig. 2c, d, respectively).
Variables Affecting Relapse of Intestinal BD
In order to identify the independent variables affecting relapse of intestinal BD, we performed univariate and multivariate analyses. In univariate analysis, the state of ulcers at the point of clinical remission (P < 0.001) and medications used during the maintenance of remission (5-aminosalicylic acids (5-ASA) and immunomodulators vs. 5-ASA only, P < 0.001) were significantly associated with relapse. In multivariate analysis, the active ulcerations at the time of clinical remission and the use of immunomodulators during the maintenance of remission were shown to be independent predictive factors for disease relapse (Table 3). Alternatively, age at intestinal BD diagnosis, sex, treatment method leading to clinical remission (medical treatment vs. surgery), type of intestinal BD (definite vs. probable), ulcer morphology (typical vs. atypical), steroid treatment before achieving remission, and history of surgery related to intestinal BD before clinical remission were not related to disease recurrence.
Discussion
Endoscopic MH is becoming more widely accepted as an important endpoint in clinical studies of IBD [9, 10, 22–24], although the role of MH in clinical practice is still debatable. MH predicts a higher probability of maintaining clinical remission and lower rates of hospital admissions and operations associated with IBD [8–12]. Unfortunately, there is very little information available about the relationship between endoscopic MH and clinical outcomes in patients with intestinal BD. In this study, several important points are discussed.
First, 71 % of patients with intestinal BD in clinical remission state still had active ulcerations. One study about endoscopic inflammations during surveillance in IBD patients reported that 37 % of UC and 27 % of CD patients without clinical symptoms showed endoscopic and histological inflammations [25]. Considering the poor response to medical treatment and complications related to ulcers, such as perforations and bleeding, a relatively high incidence of asymptomatic ulcerations implies the necessity for more rapid intervention and aggressive treatment plans for managing patients with intestinal BD.
Second, lower cumulative admission rates, PGA aggravation rates, medication change rates, and surgery rates in intestinal BD patients with MH at the time of clinical remission suggest that achieving MH could be a potential treatment goal. A recent observational study that followed 214 CD patients after infliximab treatment reported a significantly reduced need for major abdominal surgery in the MH group [8]. Additionally, a subgroup analysis of the Active Ulcerative Colitis Trial (ACT)-1 and (ACT)-2 revealed that the grade of MH was significantly associated with lower colectomy rate in patients with UC [9]. Our results showed similar significance in the cumulative surgery rate after clinical remission in accordance with several prior studies about IBD patients. Moreover, other prognostic variables, including symptomatic aggravation, also showed better outcomes in the MH group. Recognizing the relatively small sample size of this study and lower surgery rate in Asian patients, these results still highlight the clinical importance of MH in treating intestinal BD.
Third, the presence of active ulcerations at clinical remission and concomitant use of immunomodulators were identified as significant predictors for disease relapse by multivariate analysis. Although clinical remission in patients with intestinal BD can arise spontaneously, immunomodulators such as azathioprine were evaluated in previous studies and showed a significant effect in the facilitation of MH in IBD [26–29]. However, the present study demonstrated an adverse role of immunomodulators in the scope of long-term outcomes. A possible explanation is that patients who were treated with immunomodulators may have had more serious initial disease activity than those treated with 5-ASA alone. We cannot exclude another important possibility that although many clinicians treat intestinal BD as a kind of IBD, the general stepwise therapeutic strategies for IBD are ineffective in terms of intestinal BD management. This perspective suggests that there is an increasing need for novel treatment plans to achieve therapeutic goals, such as MH, in patients with intestinal BD.
This report is the first study to evaluate the long-term clinical outcome of MH in patients with intestinal BD. Our results clearly demonstrate the clinical importance of achieving MH at the time of clinical remission, although several limitations remain, such as subjective measurement of clinical parameters, small sample size, and timing difference between remission and endoscopy because of the study’s retrospective manner. One of the strengths of the current study, however, is that every patient with IBD, including intestinal BD, treated by our hospital has been evaluated with a standardized IBD activity questionnaire form, and the records from each visit since the 1970s were uniformly scanned. Therefore, we were able to minimize biases relating to study method.
In conclusion, MH in patients with intestinal BD at the time of clinical remission was significantly associated with a lower risk of disease relapse. MH might be the ultimate therapeutic goal in the treatment of intestinal BD.
References
James DG. Behcet’s syndrome. N Engl J Med. 1979;301:431–432.
Kaklamani VG, Vaiopoulos G, Kaklamanis PG. Behcet’s disease. Semin Arthritis Rheum. 1998;27:197–217.
Kasahara Y, Tanaka S, Nishino M, et al. Intestinal involvement in Behcet’s disease: review of 136 surgical cases in the Japanese literature. Dis Colon Rectum. 1981;24:103–106.
Baba S, Maruta M, Ando K, et al. Intestinal Behcet’s disease: report of five cases. Dis Colon Rectum. 1976;19:428–440.
Bayraktar Y, Ozaslan E, Van Thiel DH. Gastrointestinal manifestations of Behcet’s disease. J Clin Gastroenterol. 2000;30:144–154.
Sakane T, Takeno M, Suzuki N, et al. Behcet’s disease. N Engl J Med. 1999;341:1284–1291.
Ebert EC. Gastrointestinal manifestations of Behcet’s disease. Dig Dis Sci. 2009;54:201–207.
Schnitzler F, Fidder H, Ferrante M, et al. Mucosal healing predicts long-term outcome of maintenance therapy with infliximab in Crohn’s disease. Inflamm Bowel Dis. 2009;15:1295–1301.
Colombel JF, Rutgeerts P, Reinisch W, et al. Early mucosal healing with infliximab is associated with improved long-term clinical outcomes in ulcerative colitis. Gastroenterology. 2011;141:1194–1201.
Rutgeerts P, Diamond RH, Bala M, et al. Scheduled maintenance treatment with infliximab is superior to episodic treatment for the healing of mucosal ulceration associated with Crohn’s disease. Gastrointest Endosc. 2006;63:433–442.; quiz 464.
Allez M, Lemann M. Role of endoscopy in predicting the disease course in inflammatory bowel disease. World J Gastroenterol. 2010;16:2626–2632.
van Assche G, Vermeire S, Rutgeerts P. Mucosal healing and anti TNFs in IBD. Curr Drug Targets. 2010;11:227–233.
Cheon JH, Kim WH. Recent advances of endoscopy in inflammatory bowel diseases. Gut Liver. 2007;1:118–125.
Cheon JH, Kim ES, Shin SJ, et al. Development and validation of novel diagnostic criteria for intestinal Behcet’s disease in Korean patients with ileocolonic ulcers. Am J Gastroenterol. 2009;104:2492–2499.
Lee CR, Kim WH, Cho YS, et al. Colonoscopic findings in intestinal Behcet’s disease. Inflamm Bowel Dis. 2001;7:243–249.
Cheon JH, Han DS, Park JY, et al. Development, validation, and responsiveness of a novel disease activity index for intestinal Behcet’s disease. Inflamm Bowel Dis. 2011;17:605–613.
Kim JS, Lim SH, Choi IJ, et al. Prediction of the clinical course of Behcet’s colitis according to macroscopic classification by colonoscopy. Endoscopy. 2000;32:635–640.
Pineton de Chambrun G, Peyrin-Biroulet L, Lemann M, et al. Clinical implications of mucosal healing for the management of IBD. Nat Rev Gastroenterol Hepatol. 2010;7:15–29.
D’Haens G, Sandborn WJ, Feagan BG, et al. A review of activity indices and efficacy end points for clinical trials of medical therapy in adults with ulcerative colitis. Gastroenterology. 2007;132:763–786.
D’Haens GR, Fedorak R, Lemann M, et al. Endpoints for clinical trials evaluating disease modification and structural damage in adults with Crohn’s disease. Inflamm Bowel Dis. 2009;15:1599–1604.
Lee HW, Kim WH, Cheon JH. The medical treatments of intestinal Behçet’s disease: an update. Intest Res. 2013;11:155–160.
Rutgeerts P, Van Assche G, Sandborn WJ, et al. Adalimumab induces and maintains mucosal healing in patients with Crohn’s disease: data from the EXTEND trial. Gastroenterology. 2012;142:1102–1111. e1102.
Rutgeerts P, Sandborn WJ, Feagan BG, et al. Infliximab for induction and maintenance therapy for ulcerative colitis. N Engl J Med. 2005;353:2462–2476.
Colombel JF, Sandborn WJ, Reinisch W, et al. Infliximab, azathioprine, or combination therapy for Crohn’s disease. N Engl J Med. 2010;362:1383–1395.
Baars JE, Nuij VJ, Oldenburg B, et al. Majority of patients with inflammatory bowel disease in clinical remission have mucosal inflammation. Inflamm Bowel Dis. 2012;18:1634–1640.
Mantzaris GJ, Christidou A, Sfakianakis M, et al. Azathioprine is superior to budesonide in achieving and maintaining mucosal healing and histologic remission in steroid-dependent Crohn’s disease. Inflamm Bowel Dis. 2009;15:375–382.
D’Haens G, Geboes K, Rutgeerts P. Endoscopic and histologic healing of Crohn’s (ileo-) colitis with azathioprine. Gastrointest Endosc. 1999;50:667–671.
Ardizzone S, Maconi G, Russo A, et al. Randomised controlled trial of azathioprine and 5-aminosalicylic acid for treatment of steroid dependent ulcerative colitis. Gut. 2006;55:47–53.
Neurath MF, Travis SP. Mucosal healing in inflammatory bowel diseases: a systematic review. Gut. 2012;61:1619–1635.
Acknowledgments
This work was supported by a Grant of the Korean Health Technology R&D Project, Ministry of Health and Welfare, Republic of Korea (Grant Number A111428), the “Kiturami” Faculty Research Assistance Program of Yonsei University College of Medicine for 2012 (6-2012-0150), a faculty research Grant of Yonsei University College of Medicine for 2012(6-2012-0135 and 6-2012-0163), and a Grant of the Korean Health Technology R&D Project, Ministry of Health and Welfare, Republic of Korea (Grant Number A120176).
Conflict of interest
None.
Author information
Authors and Affiliations
Corresponding author
Additional information
Sun Mie Yim and Duk Hwan Kim have contributed equally to this work.
Rights and permissions
About this article
Cite this article
Yim, S.M., Kim, D.H., Lee, H.J. et al. Mucosal Healing Predicts the Long-Term Prognosis of Intestinal Behçet’s Disease. Dig Dis Sci 59, 2529–2535 (2014). https://doi.org/10.1007/s10620-014-3198-z
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s10620-014-3198-z