Abstract
Background
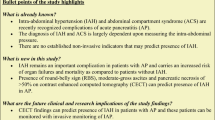
Hypotension and intestinal mucosal ischemia lead to bacterial translocation from the gut lumen into systemic circulation.
Aim
The purpose of this study was to determine the strength of association between different types of organ failure (OF): hypotension (cardiovascular system failure), renal failure, respiratory failure, CNS failure and coagulopathy in the first week of acute pancreatitis (AP) and the subsequent development of infected pancreatic necrosis (IN).
Methods
Consecutive patients with AP were evaluated for OF and its severity in the first week of hospital admission. Modified multiple organ failure score (MOFS) was used to identify and grade severity of OF. MOFS of ≥2, lasting for more than 48 h was defined as OF. Occurrence of IN (isolation of bacteria in necrosectomy specimen or image guided fine needle aspiration of pancreatic necrosis) was compared between groups with and without OF.
Results
Of the 81 patients, mean age was 40.1 ± 14.4 years and 55 were males; 60 (74 %) patients had OF and 13 (16 %) patients had IN. Occurrence of IN was not significantly different between patients with OF (18.3 %) and without OF (14.3 %), p = 0.48. However IN occurred in 10 % of patients without and 33.7 % patients with hypotension, p = 0.01. The rest of the organ systems analyzed did not show any significant difference in occurrence of infected necrosis. On multivariate analysis independent predictors of occurrence of IN were hypotension (odds ratio, OR 2.5, p < 0.001) and APACHE II score at 24 h of hospital admission (OR 4.77, p < 0.001).
Conclusion
Hypotension in the first week of AP and APACHE II score predict development of IN.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
In spite of better understanding of pathogenesis of acute pancreatitis (AP) and development of multidisciplinary management protocols, AP remains as important medical and surgical problem. Mild AP has a low mortality rate of <1 % [1, 2], whereas the death rate for severe AP can vary from 10 to 30 % depending on the presence or absence of organ failure (OF) and infected pancreatic necrosis (IN) [3]. Early evaluation and risk stratification of patients with AP are important to identify patients with predicted severe disease. AP is a disease with bimodal course, the first phase characterized by systemic inflammatory response syndrome (SIRS) and the second phase characterized by infection of pancreatic/peripancreatic necrosis. Several studies over the last decade have reported that patients with IN develop OF more often than those with sterile pancreatic necrosis [4–8]. These studies suggested that infection of pancreatic necrosis is a major determinant of severity in AP [4–8]. In contrast, some studies have found that OF is a risk factor for development of IN and a major determinant of severity [9–11]. Among patients with OF, identifying the subset of patients who are at an increased risk of IN can help us to tailor appropriate therapy. Aggressive therapy can include organ system support and possible use of antibiotics. Use of antibiotics is a double-edged sword as it can help patients with actual infection on the one hand or lead to infection with resistant organisms and fungi on the other hand. Therefore identification of patients with OF who are at an increased risk of IN can be helpful in devising appropriate therapeutic strategy.
Pancreatic necrosis, defined as diffuse or focal areas of nonviable pancreatic parenchyma, is an important complication that develops during the first few days of pancreatitis [12]. Development of necrosis is associated with pancreatic inflammation, hypovolemia, and hypotension resulting from circulatory pathway changes, vascular spasm, hemoconcentration and microthrombi formation [13]. It is associated with late complications and death if the necrotic tissue becomes infected [3]. Infection of the pancreatic necrosis is believed to occur from translocation of bacteria from the colon [14–16]. It has been suggested that intestinal barrier dysfunction occurs as a result of intestinal hypoperfusion [17] which can lead to bacterial translocation and sepsis [15]. Products and toxins from intestinal flora enter blood stream across the damaged intestinal barrier leading to sepsis and IN [18]. We hypothesized that hypotension in the early course of AP could be contributing to development of IN. The aim of this study was to test this hypothesis by studying the association between different types of organ failure (OF): hypotension, renal failure and respiratory failure in the first week of AP with subsequent development of IN.
Methods
This prospective study was conducted in the departments of Gastroenterology and General Surgery in our Institute, a tertiary care referral centre, between January 2009 and December 2010. Eighty-one consecutive patients with AP were included after an informed consent. The study was approved by the institute’s ethics committee and Indian Council of Medical Research (ICMR) guidelines for conducting a research were followed. The inclusion criteria were (1) patients more than 12 years of age, (2) AP as defined by (any two of the three) (a) acute abdominal pain, (b) elevated serum amylase (more than thrice upper limit of normal range) and (c) typical appearance on ultrasound (USG) and/or contrast-enhanced computed tomography (CECT) and (3) patients presenting within 7 days of onset of abdominal pain. Severe acute pancreatitis (SAP) was diagnosed if patients had any of the following: (1) OF, (2) local complications (necrosis, abscess, pseudocyst) or (3) APACHE II ≥8 [19]. Patients known to have chronic pancreatitis were excluded from the study.
All patients underwent detailed clinical examination and relevant investigations. APACHE II score and hematocrit levels were calculated for all patients within 24 h of hospital admission and C-reactive protein (CRP) levels were measured at 48 h. Patients were monitored for presence and severity of OF (as per modified multiple organ failure score, MOFS; Table 1), every day during the first week [20]. Patients with MOFS of ≥2 and lasting for >48 h in any organ system were recorded as having OF. As per MOFS, hypotension (cardiovascular system failure) was defined as systolic blood pressure <90 mmHg, despite adequate fluid resuscitation, lasting for >48 h. This definition was used to test the hypothesis we had proposed.
All patients were managed according to a standard protocol in a high dependency unit which included intensive resuscitation, fluid (up to 200–250 ml/h of normal saline in the initial 24 h followed by the volume dictated by clinical and hemodynamic parameters) and electrolyte monitoring, nutritional support (nasojejunal feeding or total parenteral nutrition) and supportive care. No prophylactic antibiotics were used. IN was diagnosed if image-guided (USG/CECT) fine needle aspiration of necrotic pancreatic tissue (considered when persistent fever and/or leucocytosis were present and after excluding other causes) or the operative specimen of pancreatic tissue showed isolates on bacterial culture and/or Gram staining. Blood cultures were sent periodically if the patient had persistent fever or leucocytosis. Patients with large or infected fluid collection(s) were subjected to endoscopic drainage or radiologically-guided percutaneous catheter drainage (PCD) as per the technique described earlier [21]. PCD size was upgraded when there was residual collection that was not freely drained by small bore catheters. Surgery in the form of necrosectomy and closed lesser sac drainage was offered on evidence of IN or worsening OF not responding to the above-mentioned minimally invasive modalities. The clinical course of these patients was followed until the completion of their hospital stay. Parameters evaluated for the hospital course and outcome included occurrence of IN, blood stream infection, need for PCD insertion, need for surgery, total hospital stay and mortality. Data were analyzed to correlate occurrence of IN in patients with and without different types of OF.
Statistical Analysis
The data was analyzed using SPSS software (version 21). Data was explored for any outliers, errors and missing values. When data was normally distributed, continuous variables were compared using Student t test. For more than two groups one-way ANOVA was used. For skewed data Mann–Whitney test was used. Quantitative data was described as mean and standard deviation with 95 % confidence intervals. Categorical data was shown as proportions. Comparison of OF and no OF groups was carried out for various categorical variables using chi-square test of association to find out any statistical association between these.
Results
We analysed 81 patients (55 males, mean age of 40.1 ± 14.4 years) presenting with AP (mean duration of pain before admission in our hospital, 3.6 ± 2.1 days) (Table 2). Alcohol (49.3 %) was the most common etiology of AP followed by gall stones (35.8 %) and others (14.9 %; idiopathic pancreatitis, n = 5; traumatic pancreatitis, n = 3; post-endoscopic retrograde cholangiopancreatography pancreatitis, n = 3; and hyperparathyroidism associated pancreatitis, n = 1). As per the modified multiple organ failure score [20] for defining and grading severity of OF, 21 (25.9 %) patients had no OF, while 60 (74.1 %) had OF (Table 3).
Renal failure was the most common type of OF (n = 57; 70.4 %) followed by respiratory failure (n = 36; 44.5 %), cardiovascular failure (n = 21; 26 %), coagulation failure (n = 20; 24.7 %) and central nervous system failure (n = 3; 3.7 %). Twenty-one patients had two organ failures and 16 patients had >2 organ failures. Thirteen of 81 (16 %) patients had IN, of which six were proven by Gram stain/culture sensitivity of image-guided aspiration and seven by culture of necrosectomy specimen. IN was diagnosed in four patients in week 3, seven patients in week 4 and one patient each in weeks 6 and 7. IN developed in 3/21 (14.3 %) patients without OF and 10/60 (16.7 %) with OF, p = 0.79. Six of 60 (10.0 %) patients without hypotension and 7/21 (33.3 %) with hypotension developed IN, p = 0.01 (Table 4). However there was no difference in the occurrence of IN among those with and without renal failure (p = 0.57), respiratory failure (p = 0.09), coagulation failure (p = 0.58) and central nervous system failure (p = 0.41). In addition, there was a significant correlation between hypotension and blood stream infection, five (20 %) patients without hypotension and 20 (76.2 %) patients with hypotension developed blood stream infection, p < 0.001. There was no difference in the occurrence of blood stream infection among those with and without renal failure (p = 0.24), respiratory failure (p = 0.23), coagulation failure (p = 0.09) and central nervous system failure (p = 0.23). Body mass index (BMI), CRP levels, APACHE II score, MOFS (day1), computerized tomography severity index (CTSI), and hypotension were predictors of IN by univariate analysis. On multivariate analysis the independent predictors for occurrence of IN were APACHE II score with an odds ratio of 4.77, 95 % CI 3.14–7.24, p < 0.001 and hypotension with an odds ratio of 2.5, 95 % CI 1.7–24.7, p = 0.01.
The most common organism isolated from IN was Enterococcus species (n = 7, 34 %) followed by Escherichia coli (n = 5, 23 %). Most of the isolates from IN were enteric in origin (Table 5). Antibiotic sensitivity pattern showed that most bacteria were sensitive to quinolones and third generation cephalosporins: ceftriaxone and ceftazidime.
Sixteen (19.8 %) patients underwent surgery. The mean duration of hospitalization before surgical necrosectomy was 32.4 ± 14.6 days. Indications for surgery included failure of conservative management (n = 7), sepsis and MODS (n = 6), pseudoaneurysmal bleed (n = 2) and emphysematous pancreatitis with sepsis (n = 1). The requirement of surgery was significantly higher in patients with IN, p = 0.01. The overall mortality was 19.8 %. Causes of death included sepsis and/or multiple organ dysfunction syndrome (MODS) in 13 patients, postoperative bleed in two and unrelated causes (acute myocardial infarction) in one. Only 6 (8.8 %) patients without IN died whereas 10 (76.9 %) patients with IN died, p = 0.01. The mean duration of illness before death was 24.1 ± 8.4 days. Five patients with hypotension died early in the course of illness (the mean duration of illness before death was 12.4 ± 6.7 days) due to SIRS and MODS. Of the patients with hypotension who survived the initial phase of SIRS and then developed IN (n = 7), five succumbed to illness (the mean duration before death was 24.3 ± 8.2 days, p = 0.04). Two patients died of postoperative bleed (fourth week) and one patient had acute onset myocardial infarction (second week). Three patients died due to sepsis and late onset multiorgan dysfunction (died in fourth, fifth and ninth weeks, respectively). The early mortality observed in our study was mostly due to MODS and SIRS and those with IN succumbed to illness later.
Discussion
We prospectively studied 81 patients of AP of which 74 % had OF in the first week. Renal failure was the most common(70.4 %) type of OF, followed by respiratory failure (44.5 %) and cardiovascular failure (26 %). IN developed in 16 % of them. We hypothesized that hypotension during the early phase of AP could predispose to IN and blood stream infections. A significantly greater number of patients with hypotension in the first week developed IN as compared to those without hypotension (p = 0.01). There was no difference in the occurrence of IN among those with and without renal failure, respiratory failure, coagulation failure and central nervous system failure. Patients with hypotension in the first week also had higher incidence of blood stream infections. APACHE II score was also found to be a predictor of IN. Mean arterial pressure was a component of APACHE II score, but even as a single parameter hypotension could suggest subsequent occurrence of IN.
A number of reports have suggested an association between OF and IN. Isenmann et al. [6] in a retrospective review of 273 patients with severe AP found that OF occurred more often (89 %) in patients with IN than in those with sterile necrosis (73 %), p = 0.002. In a study by Wig et al. [21] on 276 patients, IN was seen more often (51.3 %) in patients with OF than in those without OF (16.4 %), p < 0.001. However there are some studies suggesting a lack of association between OF and IN [22]. As to the relationship between specific single OF and sterile and infected necrosis, previous studies have shown contradictory results. Isenmann et al. showed that the incidence of pulmonary failure was increased in patients with IN compared to those with sterile necrosis, but there was no difference in the prevalence of renal and cardiovascular failure in IN versus sterile necrosis [6]. Zhu et al. [22], in a study of 74 patients with SAP, reported that there was no difference in the prevalence of specific single OF in IN versus sterile necrosis. In the present study, though there was no correlation between OF in general and IN, we found a significant correlation between hypotension in the first week and development of IN. We also observed higher blood stream infections in patients with hypotension in the first week of hospitalization.
In the natural history of AP, IN occurs with increasing frequency as the disease duration increases [22, 23]. Enteric organisms are documented to be the most common organisms causing IN and altered intestinal permeability is incriminated to be responsible for this phenomenon [15]. Impairment of colonic perfusion [14, 15] and cytotoxic oxygen free radicals [14] are the possible factors causing increased intestinal permeability. Apart from bacterial translocation in the gut, other sources of infection in AP are intravenous lines, urinary and other catheters, endotracheal intubation and radiological or surgical intervention. Our data shows that patients with hypotension in the first week of illness are more likely to develop IN. Hypotension leads to decreased splanchnic blood supply, thus compromising intestinal integrity. Compounded by cytotoxic oxygen free radical storm, this could lead to bacterial translocation and infection of the devitalized pancreatic tissue. Indeed a majority of the isolates from IN in our study were enteric in origin.
It has recently been shown that patients with severe AP have increased levels of serum diamine oxidase (DAO), endotoxin, and increased epithelial permeability when compared with normal controls, and that this increase was more pronounced in patients with organ dysfunction (p < 0.01) [24, 25]. The authors showed that 24 h of continuous veno-venous hemofiltration improved APACHE II score and SOFA (Sequential OF Assessment) score significantly and levels of serum DAO, endotoxin, and epithelial permeability decreased (p < 0.05). This study not only signifies the role of impaired bowel mucosal permeability but also suggests the role of therapeutic options targeted at countering mucosal translocation in AP and subsequent complications. We postulate that aggressive treatment of hypotension in early stages of AP should decrease development of IN and subsequent complications.
There are a few limitations to our study. As our centre is a referral centre, most of the patients were managed briefly (referral delay of 3.6 ± 2.1 days) at other hospitals. We have not correlated IN with any objective measures of bacterial translocation. Future studies correlating intestinal bacterial translocation and IN and hypotension can validate our observations. Future studies that can improve the understanding of hypotension, bacterial translocation and IN can be directed towards (a) studying an association between markers of intestinal permeability and IN, and (b) monitor the change in levels of these biomarkers with progression of OF (hypotension).
To conclude, we found significant correlation between APACHE II score (24 h) and hypotension in the first week of AP and development of IN. Hypotension in the first week is a harbinger of IN, which in turn leads to increased morbidity and mortality. We propose that this subgroup of patients may benefit from more aggressive fluid replacement and prophylactic administration of antibiotics.
References
Russo MW, Wei JT, Thiny MT, et al. Digestive and liver diseases statistics, 2004. Gastroenterology. 2004;126:1448–1453.
Triester SL, Kowdley KV. Prognostic factors in acute pancreatitis. J Clin Gastroenterol. 2002;34:167–176.
Dervenis C, Johnson CD, Bassi C, et al. Diagnosis, objective assessment of severity, and management of acute pancreatitis. Santorini consensus conference. Int J Pancreatol. 1999;25:195–210.
Garg PK, Madan K, Pande GK, et al. Association of extent and infection of pancreatic necrosis with organ failure and death in acute necrotizing pancreatitis. Clin Gastroenterol Hepatol. 2005;3:159–166.
Remes-Troche JM, Uscanga LF, Peláez-Luna M, et al. When should we be concerned about pancreatic necrosis? Analysis from a single institution in Mexico City. World J Surg. 2006;30:2227–2233.
Isenmann R, Rau B, Beger HG. Bacterial infection and extent of necrosis are determinants of organ failure in patients with acute necrotizing pancreatitis. Br J Surg. 1999;86:1020–1024.
Götzinger P, Sautner T, Kriwanek S, et al. Surgical treatment for severe acute pancreatitis: extent and surgical control of necrosis determine outcome. World J Surg. 2002;26:474–478.
Bhansali SK, Shah SC, Desai SB, Sunawala JD. Infected necrosis complicating acute pancreatitis: experience with 131 cases. Indian J Gastroenterol. 2003;22:7–10.
Perez A, Whang EE, Brooks DC, et al. Is severity of necrotizing pancreatitis increased in extended necrosis and infected necrosis? Pancreas. 2002;25:229–233.
Rau BM, Bothe A, Kron M, Geger HG. Role of early multisystem organ failure as major risk factor for pancreatic infections and death in severe acute pancreatitis. Clin Gastroenterol Hepatol. 2006;4:1053–1061.
Tao HQ, Zhang JX, Zou SC. Clinical characteristics and management of patients with early acute severe pancreatitis: experience from a medical centre in China. World J Gastroenterol. 2004;10:919–921.
Mofidi R, Patil PV, Suttie SA, Parks RW. Risk assessment in acute pancreatitis. Br J Surg. 2009;96:137–150.
Zhang XP, Li ZJ, Zhang J. Inflammatory mediators and microcirculatory disturbance in acute pancreatitis. Hepatobiliary Pancreat Dis Int. 2009;8:351–357.
Wang XD, Wang Q, Andersson R, Ihse I. Alterations in intestinal function in acute pancreatitis in an experimental model. Br J Surg. 1996;83:1537–1543.
Jovonen PO, Tenhunen JJ, Heino AA, et al. Splanchnic tissue perfusion in acute experimental pancreatitis. Scand J Gastroenterol. 1999;34:308–314.
Hotz HG, Foitzik T, Rohweder J, et al. Intestinal microcirculation and gut permeability in acute pancreatitis: early changes and therapeutic implications. J Gastrointest Surg. 1998;2:518–525.
Rahman Sh, Ammori BJ, Holmfield J, Larwin M, McMahon MJ. Intestinal hypoperfusion contributes to gut barrier failure in severe acute pancreatitis. J Gastrointest Surg. 2003;7:26–35.
Cicalese L, Sahai A, Sileri P, et al. Acute pancreatitis and bacterial translocation. Dig Dis Sci. 2001;46:1127–1132.
Bradley EL III. A clinically based classification system for acute pancreatitis. Summary of the international symposium on acute pancreatitis, September 11 through 13, 1992. Arch Surg. 1993;128:586–590.
Buter A, Imrie CW, Carter CR, Evans S, McKay CJ. Dynamic nature of early organ dysfunction determines outcome in acute pancreatitis. Br J Surg. 2002;89:298–302.
Wig JD, Kishore GSB, Kochhar R, et al. Correlates of organ failure in severe acute pancreatitis. JoP. 2009;10:271–275.
Zhu A-J, Shi J-S, Sun X-J. Organ failure associated with severe acute pancreatitis. World J Gastroenterol. 2003;9:2570–2573.
Besselink MG, van Santvoort HC, Boermeester MA, et al. Timing and impact of infections in acute pancreatitis. Br J Surg. 2009;96:267–273.
Liu H, Li W, Wang X, et al. Early gut mucosal dysfunction in patients with acute pancreatitis. Pancreas. 2008;36:192–196.
Zhang J, Yuan C, Hua G, Tong R, Luo X, Ying Z. Early gut barrier dysfunction in patients with severe acute pancreatitis: attenuated by continuous blood purification treatment. Int J Artif Organs. 2010;33:706–715.
Conflict of interest
None.
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Thandassery, R.B., Yadav, T.D., Dutta, U. et al. Hypotension in the First Week of Acute Pancreatitis and APACHE II Score Predict Development of Infected Pancreatic Necrosis. Dig Dis Sci 60, 537–542 (2015). https://doi.org/10.1007/s10620-014-3081-y
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s10620-014-3081-y