Abstract
Background
The World Health Organization has recently developed the Fracture Risk Assessment Tool (FRAX) based on clinical risk factors and bone mineral density (BMD) for evaluation of the 10-year probability of a hip or a major osteoporotic fracture. The aim of this study was to evaluate the use of the FRAX tool in Greek patients with inflammatory bowel disease (IBD).
Methods
FRAX scores were applied to 134 IBD patients [68 Crohn’s disease (CD); 66 ulcerative colitis (UC)] who underwent dual-energy X-ray absorptiometry scans at the femoral neck and lumbar spine during the period 2007–2012. Calculation of the FRAX scores, with or without BMD, was made through a web-based probability model used to compute individual fracture probabilities according to specific clinical risk factors.
Results
The median 10-year probability of a major osteoporotic fracture for IBD patients based on clinical data was 7.1 %, and including the BMD was 6.2 %. A significant overestimation with the first method was found (P = 0.01). Both scores with and without BMD were significantly higher in CD patients compared with UC patients (P = 0.02 and P = 0.005, respectively). The median 10-year probability of hip fracture based on clinical data was 0.8 %, and including the BMD was 0.9 %. The score with use of BMD was significantly higher in CD compared with UC patients (P = 0.04).
Conclusions
CD patients have significantly higher FRAX scores and possibly fracture risk compared with UC patients. The clinical FRAX score alone seems to overestimate the risk of osteoporotic fracture in Greek IBD patients.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
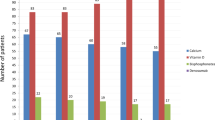
It is well known that patients with inflammatory bowel disease (IBD) have low bone mineral density (BMD) and are at increased fracture risk. The overall risk of fractures is 40 % greater than that of the general population and increases with age [1–3]. The pathogenetic mechanism of osteoporosis in IBD patients is only partially understood. Possible causes include: chronic inflammation, lack of vitamin D, steroid use, sex hormones deficiency, abnormalities in calcium homeostasis, smoking, and low body mass index (BMI) [4–6]. Use of steroids is associated with inhibition of osteoblastogenesis and promotion of osteoblast apoptosis leading to a significant reduction in bone formation. Poor nutritional status and malabsorption (particularly affecting vitamin D, vitamin K, and Ca2+ homeostasis), common conditions in IBD, are associated with renal calcium reabsorption and bone resorption. There is evidence that mediators involved in chronic inflammation such as tumor necrosis factor (TNF)-α, interleukin (IL)-1, IL-6, interferon (IFN)-γ, receptor activator of nuclear factor kappa-B (RANK) and its ligand RANKL or osteoprotegerin regulate bone remodeling, activate osteoclasts, and finally contribute to the development of osteoporosis [4, 5].
The most common and widely used technique for evaluation of fracture risk in everyday practice is dual-energy X-ray absorptiometry (DXA). This technique measures the BMD mainly in the femoral neck and the lumbar spine. The measurements are expressed as Z-score, reflecting the number of standard deviations (SDs) above or below the mean for an age-matched population, and T-score, reflecting the number of SDs above or below the mean for a young adult population [7, 8]. There is evidence that low BMD is not in direct proportion with the fracture risk and most fractures occur in individuals with a BMD T-score above the operational threshold [9, 10]. The correlation between BMD and fracture risk is in dispute in different patient populations including IBD [11–14], suggesting that we need to include more factors than BMD prior to commencing any antiosteoporotic treatment [15].
The World Health Organization (WHO) has recently developed a Fracture Risk Assessment Tool (FRAX) based on clinical risk factors with or without measurement of BMD [16]. This algorithm is based on meta-analyses from population-based cohort studies and provides two main results: firstly, the 10-year probability of a major osteoporotic fracture (clinical spine, hip, forearm or shoulder), and secondly, the 10-year probability of a hip fracture alone. The algorithm is available through the web at: http://www.shef.ac.uk/FRAX/index. The Osteoporosis Guidelines Group [17] recommends use of the FRAX score to set thresholds for medical treatment and the necessity for DXA in patients with osteoporosis [18, 19].
Our aim is to evaluate the accuracy of pre-BMD FRAX score in Greek IBD population in order to identify the patients who need medical therapy, scanning with DXA, or just close follow-up/reassurance. We also evaluated and compared the fracture risk in patients with Crohn’s disease (CD) and ulcerative colitis (UC).
Methods
Patients
We evaluated FRAX score with and without BMD in 134 consecutive IBD patients who underwent DXA scanning from January 2007 to March 2012 at the University Hospital of Heraklion, Crete, Greece. The following exclusion criteria were applied: age under 18 years old, celiac disease, diabetes mellitus, malabsorption syndromes, concurrent liver disease, renal disease, hypogonadism, parathyroid disorders or untreated disorders of the thyroid. The Montreal classification was used for CD and UC, respectively [20]. The activity of the CD patients was assessed by the CD Activity Index (CDAI) [21]. For the patients with UC, we used the Simple Clinical Colitis Activity Index [22]. A written informed consent was obtained from all patients, and the protocol of the study has been approved by the Ethics Committee of the University Hospital of Heraklion.
In this study we recorded age, sex, body mass index (BMI), type, location and severity of the disease, medical therapy, current smoking and alcohol use, menopausal status, and corticosteroid use both at present and in the past. IBD patients who had undergone surgery were also included in this study. Baseline characteristics of the patients at time of DXA scanning are presented in Table 1. Twenty-eight IBD patients (13 UC, 15 CD, 20.9 %) under corticosteroid treatment, and 73 (29 UC, 44 CD, 54.5 %) with past history of corticosteroid treatment were included in this study. The mean number of cycles of corticosteroid use was 4.8 ± 3.1, and the mean duration of this treatment was 21.7 ± 14.8 months.
BMD was recorded by the same Lunar Prodigy dual-energy X-ray absorptiometry system (Lunar Prodigy, GE, USA) in the lumbar spine (L1–L4) and in the femoral neck. WHO guidelines were used for the definition of osteopenia and osteoporosis: T-score > −1 SD at both lumbar spine and hip according to the guidelines was the threshold for normal BMD; T-score between −1.0 and −2.5 SD at either lumbar spine or hip or both was considered osteopenic; and finally T-score < −2.5 SD at either lumbar spine or hip or both suggested an osteoporotic status.
FRAX Score
Fracture probability was estimated using the FRAX score tool based on the Italian algorithm. This algorithm demands the completion of the following fields: age (years), height (cm), weight (kg), history of trauma fracture (spontaneous or arising from trauma which in healthy controls would not have resulted in a fracture), history of parental hip fracture, current smoking, drinking three or more units of alcohol per day, current glucocorticoid use (defined as more than 7.5 mg prednisolone, or equivalent, in the last 3 months), a diagnosis of concomitant rheumatoid arthritis, and the existence of a secondary cause of osteoporosis. IBD is one of the causes of secondary osteoporosis, thus all patients were considered as having a secondary cause of osteoporosis. The output of FRAX is the 10-year probability of a major osteoporotic fracture (hip, clinical spine, humerus or wrist fracture) and the 10-year probability of hip fracture. The questionnaire was completed by telephone interview. We calculated FRAX scores for all patients twice: the first time without using the BMD measurements, and the second time we recalculated all FRAX scores including the measurement of T-score at the femoral neck.
Statistical Analysis
The Kolmogorov–Smirnov test was used to assess the normality of the data. Since the values were not normally distributed, results are presented as median values and their ranges. The interquartile range (IQR) was calculated as the distance between the 25th percentile and the 75th percentile. Box and whisker plots are used to summarize and display data. Comparisons between two groups were made by Student’s t test or Mann–Whitney’s U test. Correlations between the examined parameters were analyzed with the Pearson’s correlation method. Bland–Altman plot is used to provide graphical representation of the comparison of pre-FRAX and FRAX scores. A level of P < 0.05 was considered statistically significant. All statistical calculations were processed using the MedCalc software package (MedCalc Software, Belgium).
Results
T-scores at the lumbar spine and femoral neck of CD patients were not significantly different compared with UC patients (P = 0.31 and P = 0.13, respectively). Similarly Z-scores at the lumbar spine and femoral neck were not different between UC and CD patients (P = 0.37 and P = 0.11, respectively). Using the WHO’s diagnostic criteria, 57 IBD patients (30 UC; 27 CD) were classified as normal, 62 (33 UC; 29 CD) were osteopenic, and 15 (3 UC; 12 CD) were classified as osteoporotic.
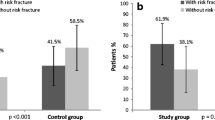
The median 10-year probability of a major osteoporotic fracture for IBD patients based on clinical data was found as 7.1 % (IQR 4.5–9.0 %), and including the BMD as 6.2 % (IQR 3.7–9.4 %) with a significant difference among them in the paired analysis (P = 0.01). Both scores were significantly higher in females (P = 0.01), but when the postmenopausal women were excluded both sexes had similar scores (P = 0.76). The 10-year risk of a major osteoporotic fracture calculated without and with BMD was significantly higher in CD patients compared with UC patients (P = 0.02 and P = 0.005, respectively) (Fig. 1). The bias between the FRAX score estimations with and without BMD was 1.0 % (Fig. 2). The FRAX score without using the BMD information resulted in an overestimation of fracture probability in comparison with the FRAX score estimated taking BMD into account. The 95 % limits of agreement were: 7.9 (lower limit) and 9.8 (upper limit). Ten data points were outside the calculated confidence intervals. This analysis shows that estimation of FRAX score using BMD is preferable compared with that without BMD.
Distribution of 10-year probability of a major osteoporotic fracture with and without bone mineral density (BMD) in inflammatory bowel disease patients. Boxes indicate the interquartile range with median value. Bars show the 5th and 95th percentiles, and data points representing the 1st and 99th percentiles are shown as stars
The median 10-year probability of hip fracture for IBD patients based on clinical data was 0.8 % (IQR: 0.4–2.2 %) and including the BMD was 0.9 % (IQR: 0.2–2.5 %). No significant difference between pre-BMD and including BMD score was found (P = 0.87). These scores were similar in both sexes (P = 0.15). The 10-year probability of hip fracture based on clinical data was higher in CD compared with UC patients, but the difference was not statistically significant (P = 0.18). On the other hand the score with use of BMD was significantly higher in CD compared with UC patients (P = 0.04) (Fig. 3).
Distribution of 10-year probability of hip fracture with and without bone mineral density (BMD) in inflammatory bowel disease patients. Boxes indicate the interquartile range with median value. Bars show the 5th and 95th percentiles, and data points representing the 1st and 99th percentiles are shown as stars
Six CD patients (8.8 %) had a high risk for a major osteoporotic fracture (10-year probability >20 %). No significant associations between FRAX scores and clinical characteristics (localization, history of surgery, treatment) of IBD patients were found.
Discussion
In daily practice most physicians use the T-score as the only marker in decision-making for antiosteoporotic treatment in IBD patients. However, with this practice they often under- or overestimate the need for treatment. It seems that the FRAX score is a much more integrated approach in assessing fracture risk, since it takes into account factors such as age, sex, BMI, smoking, alcohol consumption, and previous fractures, related with higher fracture risk. The present study showed that the clinical (pre-BMD) FRAX score rather overestimates the fracture risk in Greek IBD patients. Therefore, the pre-BMD FRAX score could be used in order to categorize the patients at risk but it is not able to replace the including BMD FRAX score. In a study from the UK, Goodhand et al. [23] found that the clinical FRAX score alone can accurately (sensitivity 100 %) predict the risk of osteoporotic fracture. However, our results showed that estimation of FRAX score using BMD is preferable compared with that without BMD. Based on the existing data, we could suggest use of the clinical FRAX as a first test to select the patients who need DXA scan, and the included BMD FRAX in order to consider specific treatment for osteoporosis. The use of clinical FRAX could reduce the need and the cost of DXA scans, and the use of FRAX with BMD could help in treatment decisions especially in CD patients who have high clinical risk of fracture. We think, however, that these data are rather preliminary to dictate specific treatment decisions, and that the application of the guidelines written by the National Osteoporosis Guideline Group (NOGG) [17] in IBD patients merits future investigation.
The findings of our study confirm our previous reports where no significant differences between CD and UC patients concerning T- and Z-scores were found [24, 25]. The present study, the first one with a comparison of FRAX scores between UC and CD patients, showed that the 10-year probability of a major osteoporotic fracture and of hip fracture (mainly the score with use of BMD) were significantly higher in CD compared with UC. There is evidence from epidemiological studies that the prevalence of fractures and fracture risk is more elevated in CD than UC patients [26, 27]. It could be suggested that the systemic inflammatory response and abnormalities in calcium homeostasis may induce increased BMD loss in CD compared with UC. Our observations are in agreement with the findings of Hyams et al. [28], who reported disorders in bone formation and architecture in children with CD but not in those with UC.
Six CD patients (8.8 %) showed a high risk of major osteoporotic fracture (10-year probability >20 %), which alerted us to follow them up more closely with DXA scanning annually and aggressive treatment with diphosphonates and calcium supplement, since vertebral fractures can be either asymptomatic or underdiagnosed by physicians in 20 % of the patients [29, 30]. Preexistence of vertebral fracture is an independent risk factor for fracture relapses [31].
A limitation of our study is the absence of country-specific data on osteoporosis in the general Greek population. Since it has been suggested that in this case a regional model might be constructed [32–34], we used the existing data of Italy in the calculation of FRAX score. Another limitation is that the FRAX tool was designed for assessing osteoporosis in the general population and for ages older than 40 years and not specifically for IBD patients. Considering that a large proportion of IBD patients are younger than 40 years the FRAX tool may overestimate the fracture risk in these patients, because of the age-related BMD loss. Finally, the duration and dose of corticosteroid use, necessary in the FRAX calculations, cannot always be measured accurately, thereby leading to inaccuracies.
In conclusion, the clinical FRAX score alone cannot replace the FRAX score with BMD measurement for the evaluation of the risk of osteoporotic fracture in Greek IBD patients. Possibly it could be used only as a screening tool in order to identify patients who need DXA. Furthermore, CD patients have a significantly higher fracture risk than UC patients, possibly due to the involvement of their systemic inflammatory response which leads to a greater loss of bone mass. It seems that CD patients are in need of closer follow-up including measurement of clinical FRAX score and, if confirmed by larger prospective studies also taking into account the potential applicability of NOGG recommendations in these patients, FRAX with DXA might be a useful tool to prevent future major osteoporotic fractures.
References
Bernstein CN. Osteoporosis in patients with inflammatory bowel disease. Clin Gastroenterol Hepatol.. 2006;4:152–156.
Bernstein CN, Blanchard JF, Leslie W, Wajda A, Yu BN. The incidence of fracture among patients with inflammatory bowel disease. A population-based cohort study. Ann Intern Med. 2000;133:795–799.
Loftus EV Jr, Crowson CS, Sandborn WJ, Tremaine WJ, O’Fallon WM, Melton LJ 3rd. Long-term fracture risk in patients with Crohn’s disease: a population-based study in Olmsted County, Minnesota. Gastroenterology. 2002;123:468–475.
Ghishan FK, Kiela PR. Advances in the understanding of mineral and bone metabolism in inflammatory bowel diseases. Am J Physiol Gastrointest Liver Physiol. 2011;300:G191–G201.
Tilg H, Moschen AR, Kaser A, Pines A, Dotan I. Gut, inflammation and osteoporosis: basic and clinical concepts. Gut. 2008;57:684–694.
Pollak RD, Karmeli F, Eliakim R, Ackerman Z, Tabb K, Rachmilewitz D. Femoral neck osteopenia in patients with inflammatory bowel disease. Am J Gastroenterol. 1998;93:1483–1490.
Lewis NR, Scott BB, Guidelines for osteoporosis in inflammatory disease and coeliac disease. Available at: http://www.bsg.org.uk/images/stories/clinical/ost_coe_ibd.pdf; 2007.
American Gastroenterological Association Medical Position Statement. Guidelines on osteoporosis in gastrointestinal diseases. Gastroenterology. 2003;124:791–794.
Cranney A, Jamal SA, Tsang JF, Josse RG, Leslie WD. Low bone mineral density and fracture burden in postmenopausal women. CMAJ. 2007;177:575–580.
Siris ES, Chen YT, Abbott TA, et al. Bone mineral density thresholds for pharmacological intervention to prevent fractures. Arch Intern Med. 2004;164:1108–1112.
Kanis JA. Diagnosis of osteoporosis and assessment of fracture risk. Lancet. 2002;359:1929–1936.
Stockbrugger RW, Schoon EJ, Bollani S, et al. Discordance between the degree of osteopenia and the prevalence of spontaneous vertebral fractures in Crohn’s disease. Aliment Pharmacol Ther. 2002;16:1519–1527.
van Staa TP, Cooper C, Brusse LS, Leufkens H, Javaid MK, Arden NK. Inflammatory bowel disease and the risk of fracture. Gastroenterology. 2003;125:1591–1597.
Card T, West J, Hubbard R, Logan RF. Hip fractures in patients with inflammatory bowel disease and their relationship to corticosteroid use: a population based cohort study. Gut. 2004;53:251–255.
Lichtenstein GR, Sands BE, Pazianas M. Prevention and treatment of osteoporosis in inflammatory bowel disease. Inflamm Bowel Dis. 2006;12:797–813.
WHO. Fracture risk assessment tool. Available at: http://www.shef.ac.uk/FRAX.
NOGG recommendations. Pocket guide for healthcare professionals. Available at: http://www.shef.ac.uk/NOGG/downloads.html.
Kanis JA, McCloskey EV, Johansson H, Oden A. Approaches to the targeting of treatment for osteoporosis. Nat Rev Rheumatol. 2009;5:425–431.
Kanis JA, McCloskey EV, Johansson H, Strom O, Borgstrom F, Oden A. Case finding for the management of osteoporosis with FRAX–assessment and intervention thresholds for the UK. Osteoporos Int. 2008;19:1395–1408.
Satsangi J, Silverberg MS, Vermeire S, Colombel JF. The Montreal classification of inflammatory bowel disease: controversies, consensus, and implications. Gut. 2006;55:749–753.
Best WR, Becktel JM, Singleton JW, Kern F Jr. Development of a Crohn’s disease activity index. National Cooperative Crohn’s Disease Study. Gastroenterology. 1976;70:439–444.
Walmsley RS, Ayres RC, Pounder RE, Allan RN. A simple clinical colitis activity index. Gut. 1998;43:29–32.
Goodhand JR, Kamperidis N, Nguyen H, Wahed M, Rampton DS. Application of the WHO fracture risk assessment tool (FRAX) to predict need for DEXA scanning and treatment in patients with inflammatory bowel disease at risk of osteoporosis. Aliment Pharmacol Ther. 2011;33:551–558.
Koutroubakis IE, Zavos C, Damilakis J, et al. Low bone mineral density in Greek patients with inflammatory bowel disease: prevalence and risk factors. Ann Gastroenterol. 2011;24:41–46.
Koutroubakis IE, Zavos C, Damilakis J, et al. Role of ghrelin and insulin-like growth factor binding protein-3 in the development of osteoporosis in inflammatory bowel disease. J Clin Gastroenterol. 2011;45:e60–e65.
Vestergaard P, Krogh K, Rejnmark L, Laurberg S, Mosekilde L. Fracture risk is increased in Crohn’s disease, but not in ulcerative colitis. Gut. 2000;46:176–181.
Jahnsen J, Falch JA, Aadland E, Mowinckel P. Bone mineral density is reduced in patients with Crohn’s disease but not in patients with ulcerative colitis: a population based study. Gut. 1997;40:313–319.
Hyams JS, Wyzga N, Kreutzer DL, Justinich CJ, Gronowicz GA. Alterations in bone metabolism in children with inflammatory bowel disease: an in vitro study. J Pediatr Gastroenterol Nutr. 1997;24:289–295.
Heijckmann AC, Huijberts MS, Schoon EJ, et al. High prevalence of morphometric vertebral deformities in patients with inflammatory bowel disease. Eur J Gastroenterol Hepatol. 2008;20:740–747.
Siffledeen JS, Siminoski K, Jen H, Fedorak RN. Vertebral fractures and role of low bone mineral density in Crohn’s disease. Clin Gastroenterol Hepatol. 2007;5:721–728.
Donaldson MG, Palermo L, Schousboe JT, Ensrud KE, Hochberg MC, Cummings SR. FRAX and risk of vertebral fractures: the fracture intervention trial. J Bone Miner Res. 2009;24:1793–1799.
Kanis JA, Hans D, Cooper C, et al. Interpretation and use of FRAX in clinical practice. Osteoporos Int. 2011;22:2395–2411.
Czerwinski E, Kanis JA, Osieleniec J, et al. Evaluation of FRAX to characterise fracture risk in Poland. Osteoporos Int. 2011;22:2507–2512.
Cheng CK, McDonald-Blumer H, Boire G, et al. Care gap in patients with early inflammatory arthritis with a high fracture risk identifies using FRAX. J Rheumatol. 2010;37:2221–2225.
Acknowledgments
This study was partly supported by a grant from the Hellenic Society of Gastroenterology.
Conflict of Interest
None.
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Terzoudis, S., Zavos, C., Damilakis, J. et al. Increased Fracture Risk Assessed by Fracture Risk Assessment Tool in Greek Patients with Crohn’s Disease. Dig Dis Sci 58, 216–221 (2013). https://doi.org/10.1007/s10620-012-2326-x
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s10620-012-2326-x