Abstract
Background
A higher circulating vitamin D level is inversely associated with the risk of colorectal cancer, but the association with adenoma risk is less clear.
Aims
We examined the association between the circulating 25-hydroxyvitamin D3 [25(OH)D3] concentration and colorectal adenoma in asymptomatic average-risk participants undergoing initial screening colonoscopy.
Methods
The study subjects were comprised of 143 cases of colorectal adenomas and 143 age- and gender-matched controls with normal colonoscopy among the 586 asymptomatic average-risk subjects (median age, 58 years; range, 50–73 years) who underwent first screening colonoscopy and measurement of the serum 25(OH)D3 between December 2009 and April 2010, consistent with winter months of the region.
Results
The mean concentration of serum 25(OH)D3 in the adenoma and control groups was 20.0 ± 11.0 ng/ml and 25.0 ± 20.0 ng/ml, respectively (P = 0.009). Using multivariate analysis, higher levels of 25(OH)D3 were associated with a statistically significant decreased risk of colorectal adenoma after multivariable adjustment (highest vs. lowest quartile OR 0.38, 95% CI 0.18–0.80, P trend = 0.012). The inverse association of circulating 25(OH)D3 with colorectal adenoma was stronger among the patients with proximal adenoma than that among the patients without proximal adenoma (highest vs. lowest quartile OR 0.29, 95% CI 0.13–0.66, P trend = 0.001).
Conclusions
The present study suggests that high levels of circulating vitamin D are associated with a decreased risk of colorectal adenoma, and especially adenoma located in the proximal colon.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
The protective role of vitamin D in colorectal carcinogenesis has recently been suggested based on the ecologic patterns of colorectal cancer (CRC) mortality according to latitude as an indication of the regional variation in solar radiation, which is required for vitamin D synthesis [1]. The hypothesis has been supported by animal and in vitro studies that vitamin D induces cell differentiation and apoptosis and inhibits proliferation, angiogenesis and metastasis of CRC cells [2–5]. In epidemiologic studies, the vitamin D status was inversely associated with the risk of CRC, but the association with the risk of colorectal adenoma, which is a well established precursor of CRC, was less clear.
The findings from the studies that have investigated the vitamin D–colorectal adenoma association have been null or inconsistent. Although 90–95% of all vitamin D is produced in the skin by the action of sunlight [6–8], most observational studies were limited to assessing only poorly measured dietary vitamin D intake and the findings from these studies have mostly been null [9–21]. Most of the studies that measured the circulating vitamin D concentration have had also some limitations of the enrolled study population, such as the enrolled participants were evaluated for the status of only the distal colorectum using sigmoidoscopy [12, 13, 22, 23], they were taking chemopreventive agents or placebo for a chemoprevention trial [20, 24], they had symptoms that needed colonoscopic evaluations [4, 25] or they were all of one gender [22, 26]. Therefore, even though the studies showed a trend that a better vitamin D status lowered the risk of colorectal adenoma, the findings from these studies have remained inconsistent [12, 13, 20, 22–27]. To our knowledge, there has been no previous study that has investigated the association between the circulating vitamin D levels and the risk of colorectal adenoma in an asymptomatic, average-risk, screened population.
Therefore, we investigated the association between the circulating vitamin D level and risk of colorectal adenomas in asymptomatic, average-risk individuals who underwent first screening colonoscopy.
Patients and Methods
Study Participants
We conducted a cross-sectional case–control study using a consecutive series of subjects who underwent health screening examinations during November 2009 to April 2010 at the Healthcare Center of Konkuk University Medical Center in Seoul, Korea. The details of the health examination have been described previously [28]. The examinees received written information about the screening program, including a toll-free telephone number to call to obtain more information about the program or to schedule an appointment for screening. Telephone interviews were conducted to establish that the examinees who called to make an appointment for screening were asymptomatic (i.e., they reported no visible rectal bleeding, no recent change in bowel habits and no recent lower abdominal pain). The persons with symptoms were urged to seek medical care. This study was approved by the Institutional Review Board of Konkuk University Medical Center.
The flow diagram of the study is shown in Fig. 1. A consecutive series of 586 asymptomatic, average-risk subjects aged 50–74 years and who underwent first screening colonoscopy and who had their serum 25-hydroxyvitamin D3 [25(OH)D3] level measured were eligible. All colonoscopies successfully reached to the base of cecum. We excluded a total of 41 subjects: five for refusal to answer the questionnaire; 34 patients had an increased risk of CRC, including a family history of CRC in a first degree relative; and two had a history of colorectal surgery. One hundred forty-three patients were found to have at least one histologically confirmed adenoma without invasive cancer. Among the 402 subjects with normal colonoscopy, 143 age- and gender-matched subjects were randomly selected as controls.
Colonoscopy
All the colonoscopies were performed with a CF-H260AI (Olympus, Tokyo, Japan) or an EC-3490Fi (Pentax, Tokyo, Japan) by experienced endoscopists accredited by the Korean Society of Gastrointestinal Endoscopy. During colonoscopy, the location, size and number of colorectal adenomas were recorded. The boundary between the proximal colon and the distal colon was defined as the junction of the splenic flexure and the descending colon, as assessed by the endoscopists. The polyp size was estimated using open-biopsy forceps. For the patients with multiple adenomas, the size and appearance of the adenoma with advanced pathology or the largest adenoma were reported.
Laboratory Assays
Fasting serum was obtained for measurement of 25(OH)D3, the total calcium and the albumin at the day of colonoscopy. The serum 25(OH)D3 concentrations were measured by direct competitive electrochemiluminescence immunoassay (Vitamin D3 (25-OH) kit, Roche Diagnostics, Mannheim, Germany) on an automated immunoassay analyzer (Elecsys 2010, Roche Diagnostics). The assay employs a monoclonal antibody directed against 25(OH)D3, which was labeled with ruthenium. In brief, 25(OH)D3 in the sample competes with the biotin labeled vitamin D and the remaining amount of the complex is dependent upon the analyte concentration [29]. This method can measure the concentration of 25(OH)D3 in the range of 4–100 ng/ml. The serum levels of the corrected total calcium were calculated by the most commonly used formula in clinical practice: the corrected serum calcium = serum calcium + (0.8) × (4 − serum albumin) [30].
Lifestyle and Anthropometric Data
The eligible subjects received a standard questionnaire that included questions regarding the patients’ personal medical history (including a history of colorectal cancer or polyps), the present medications, the family history (including colorectal cancer or polyps), physical activity (using the International Physical Activity Questionnaire) [31] and lifestyle habits (smoking and alcohol consumption). The body weight and height were recorded, and the body mass index (BMI) was calculated as weight in kilograms divided by the square of height in meters.
Statistical Analysis
Continuous variables are expressed as means ± standard deviations, while the categorical variables are presented as absolute values and percentages. The differences between the continuous variables were analysed using the unpaired Student’s t test, and differences between the categorical variables were analysed using χ2 tests and Fisher’s exact tests, as appropriate. Study-specific quartiles of the serum 25(OH)D3 concentrations were calculated based on the distribution in the cases and the controls. Logistic regression analysis was used to obtain the odds ratios (OR) and 95% confidence intervals (CI) of colorectal adenomas according to the quartiles of 25(OH)D3 (the lowest quartile as the reference group) and each 10 ng/ml increment of 25(OH)D3. In addition, we investigated the association between the 25(OH)D3 quartiles and the adenoma characteristics, including location (proximal colon, distal colon), size (<10 mm, ≥10 mm) and number (1, ≥2). To examine the potential confounders for colorectal adenoma, the multivariate models were adjusted for age, gender, the body mass index, current smoking, alcohol consumption (≥20 g/day during the previous 12 months), physical activity (inactive, minimally active and active) and the corrected calcium level. In addition, subgroup analysis was performed according to gender and age. Age was divided into two groups using the median age of 58 years as the cutoff age. A P value less than 0.05 was considered to indicate statistical significance. The analyses were performed with SPSS (version 12.0 K; SPSS Inc., Chicago, IL).
Results
The characteristics of the study population are presented in Table 1. The mean age was 58.7 ± 6.0 years (median, 58 years; range, 50–73 years) and 68% were male. The cases and controls did not differ considerably with regard to obesity, alcohol, smoking and physical activity. However, the serum 25(OH)D3 was significantly lower in the subjects with colorectal adenoma than that in the controls (20.0 ± 10.0 ng/dl vs. 25.0 ± 20.0 ng/dl, P = 0.001).
Table 2 shows the univariate and multivariate analyses on the association of the circulating 25(OH)D3 concentration with colorectal adenoma. On the logistic regression analysis, higher levels of 25(OH)D3 were associated with a statistically significant decreased risk of colorectal adenoma after multivariable adjustment (highest vs. lowest quartile OR 0.38, 95% CI 0.18–0.80, P trend = 0.012). Similar inverse associations with colorectal adenoma per 10 ng/ml increment of the 25(OH)D3 were observed on the analysis for circulating 25(OH)D3 as a continuous variable in the multivariable model (highest vs. lowest quartile OR 0.78, 95% CI 0.65–0.95, P trend = 0.014).
Among the adenoma group, 82 patients had at least one adenoma located in the proximal colon, 63 patients had two or more adenomas and 30 patients had one or more adenoma that was ≥1 cm in diameter. The inverse association of circulating 25(OH)D3 with colorectal adenoma was stronger among the patients with proximal adenoma than among the patients without proximal adenoma (highest vs. lowest quartile OR 0.29, 95% CI 0.13–0.66, P trend = 0.001). However, the inverse association of circulating 25(OH)D3 with adenoma did not substantially differ according to the adenoma size and number, although the sample size was relatively small for these analyses (Table 3).
Subgroup analysis was performed according to gender and age. Table 4 shows the association of circulating 25(OH)D3 concentration with the overall adenoma and the location of adenoma according to the gender. The relationship between circulating vitamin D level and proximal adenoma showed a significant association in male participants, while there was a similar trend in women participants. Table 5 shows the association of circulating 25(OH)D3 concentration with the overall adenoma and the location of adenoma according to the age group. The relationship between circulating vitamin D level and proximal adenoma showed a significant association in the older group (≥58 years), while there was a similar trend in the younger group (<58 years).
Discussion
There is growing awareness of the role of vitamin D not only for its role in metabolic bone disease, but also for its association with a variety of chronic diseases such as colorectal cancer and adenomas. Recent studies have found that normal colonic epithelium and colorectal cancer cells express the vitamin D receptor and a key vitamin D metabolizing enzyme called 1α-hydroxylase, which converts 25-hydroxyvitamin D [25(OH)D] to the active 1,25-(OH)2 vitamin D [1,25(OH)2D] [2, 3, 32, 33]. When activated by 1,25(OH)2D, the vitamin D receptor is a transcription factor that has been shown to decrease epithelial cell proliferation and to induce differentiation and apoptosis in colorectal neoplasia [2–5]. Thus, the colon can produce 1,25(OH)2D from 25(OH)D locally to control the genes that inhibit and suppress carcinogenesis. If a cell becomes malignant, then 1,25(OH)2D can induce apoptosis and inhibit angiogenesis, thereby reducing the potential for the malignant cell to survive [26].
Although 1,25(OH)D is the biologically active form of vitamin D, the half life of circulating 1,25(OH)D is only 4–6 h and the circulating levels of 1,25(OH)D are a thousand-fold less than 25(OH)D [34]. Moreover, in one previous study, when a patient becomes vitamin D deficient or had insufficient vitamin D, the increase in parathyroid hormone levels induced renal 1α-hydroxylase activity and this resulted in normal or elevated levels of 1,25(OH)D [34]. Thus, the measures of circulating 25(OH)D levels must consider the surrogates or determinants of vitamin D, including the region of residence, the vitamin D intake and the estimated sun exposure, or a combination of these [35]. Of particular interest is a recent observation that an inverse association between plasma 25(OH)D and colorectal neoplasia was confined to the individuals with blood drawn during the winter months, whereas no measurable association was noted for those individuals with blood drawn in the summer months [26, 36]. Thus, in the present study, we measured the serum 25(OH)D concentration by only using blood drawn during the winter months. In addition, of the two forms of 25(OH)D measured in blood (D2 and D3), we used 25(OH)D3 as the primary measure of the vitamin D status in our analysis. Although 25(OH)D2 contributes to the total circulating 25(OH)D, we expect this contribution to be minimal. Unlike vitamin D3, vitamin D2 cannot be synthesized by humans and is present mostly in fungus-derived/yeast-derived products [25, 34]. In addition, compared with vitamin D3, vitamin D2 may have lower bioefficacy, which may be due to the lower binding affinities of vitamin D2 and its metabolites to the vitamin D receptor, vitamin D binding protein and CYP27A1 enzyme [37]. A previous study reported the total 25(OH)D levels were consistent with those reported for 25(OH)D3 [25]. Therefore, the potential misclassification of participants’ vitamin D status due to excluding circulating 25(OH)D2 concentrations can be considered to be negligible [25].
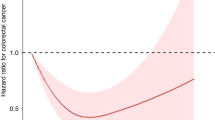
Since the hypothesis that vitamin D is protective against CRC in humans was proposed on the basis of a geographical correlation between sunlight exposure and the CRC mortality [1], numerous cohort and case–control studies have observed a fairly consistent, protective association between vitamin D intake or the circulating 25(OH)D levels and CRC [35, 38, 39]. Furthermore, an inverse linear dose–response relation has been shown for both the dietary intake of vitamin D and the circulating levels of 25(OH)D with the CRC risk. The recent studies that include a meta-analysis of vitamin D exposure and CRC risk have estimated there is a 50% decrease in the incidence of colorectal cancer for individuals with a vitamin intake ≥1,000 IU/day or ≥33 ng/ml circulating 25(OH)D [38, 39].
With regard to colorectal adenomas, one cross-sectional study, six case–control studies and two cohort studies that all used randomly selected subjects in chemoprevention trials have addressed the association of adenoma with the plasma or serum concentrations of 25(OH)D (Table 6), and they reported an inconsistent association with the prevalence of adenoma [12, 13, 22, 23, 25–27] and recurrence [20, 24]. Three studies reported a statistically significant inverse association [12, 25, 27], while the other three studies did not find any significant association [13, 22, 26]. In the remaining studies, a statistically significant inverse association was observed only in women [20, 23] or in the calcium supplement groups [24]. In our opinion, such differences between the adenoma and cancer studies could have been caused by limitations in the selection of eligible subjects in the adenoma studies. Most of the case–control studies investigated only the distal colorectal adenoma risk for a selected population [12, 13, 22, 23]. Two large nested case–control studies from the Nurses’ Health Study and the Self Defence Forces Health Study were performed on only female or male patients [22, 26]. The other studies analyzed the data from the subjects who were enrolled in urso-deoxycholic acid (UDCA) trials [20] and a Calcium Polyp Prevention Study [24], which could have affected the development of adenoma or the circulating 25(OH)D levels, although they showed no effect of chemopreventive agents on adenoma recurrence. Interestingly, in a colonoscopy-based cross-sectional study and a pooled case–control study, the circulating 25(OH)D or 25(OH)D3 was inversely associated with the risk of colorectal adenoma [4, 25]. However, most of the participants in both these studies were symptomatic and/or high-risk individuals that needed colonoscopic evaluations [4, 25, 40]. The issues for the enrolled subjects are important because they can affect the scientific results. Therefore, to our knowledge, the present study is a first report that has focused on the association of vitamin D and colorectal adenoma in average-risk, asymptomatic individuals who underwent colonoscopy.
In the present colonoscopy-based, case–control study of an asymptomatic average-risk population who underwent first screening colonoscopy, we found that a high level of circulating 25(OH)D3 during the winter season was associated with a decreased risk of colorectal adenomas in the proximal colon. Interestingly, the finding that the proximally located adenoma showed a significant inverse association with a higher level of circulating 25(OH)D3 was reported in the pooled case–control study by Fedirko et al. In addition, a pooled analysis of a large male cohort study (Health Professionals Follow-Up Study) and a large female cohort study (Nurses’ Health Study) reported that higher plasma 25(OH)D levels were associated with decreased risks of colon cancer, but not rectal cancer [36].
The risk of proximal adenomas was different regarding gender and age group. On the subgroup analysis, the inverse association of circulating 25(OH)D3 with proximal adenoma was significant in males and the older group. However, women and the younger group also showed similar trends and the reason for failure to reach statistical significance appeared to be small numbers of those groups. Thus, we thought that it was difficult to conclude the effect of gender and age group on vitamin D levels and colorectal adenomas in our study results.
A recent study reported that the reduction of CRC mortality using colonoscopy appears to be limited to distal CRC, and not the proximal forms of the disease [41]. Thus, if vitamin D could reduce the risk of proximal colorectal adenoma, vitamin D might be used as a useful chemopreventive agent. However, previous daily supplementation of calcium with vitamin D for 7 years had no effect on the incidence of colorectal cancer among postmenopausal women [42]. Future large-scale randomized controlled trials of vitamin D supplementation are required to determine the efficacy of vitamin D as a chemopreventive agent.
The present study had several limitations. First, the sample size was relatively small. Second, inverse causality is a concern when interpreting the findings from cross-sectional studies, although the presence of colorectal adenoma probably did not influence the circulating vitamin D. Third, the serum 25(OH)D3 level was determined at only one time point during the winter season. The one-time measurement may not have captured each individual’s long-term vitamin D levels. Fourth, the extent to which the results of this analysis can be applied to populations of a similar age with different sociodemographic characteristics is unclear as this study was performed at a single center with a cohort comprised of ethnic Korean individuals. Finally, we did not obtain complete estimations of nutrients from our dietary questionnaire, which could have affected the serum 25(OH)D3 levels.
We conclude that the asymptomatic, average-risk Korean screenees who have low levels of circulating 25(OH)D3 may have a higher risk of colorectal adenoma, and especially adenoma located in the proximal colon. Future randomized controlled trials may be needed to establish a causal association.
References
Garland CF, Garland FC. Do sunlight and vitamin D reduce the likelihood of colon cancer? Int J Epidemiol. 1980;9:227–231.
Matusiak D, Murillo G, Carroll RE, Mehta RG, Benya RV. Expression of vitamin D receptor and 25-hydroxyvitamin D3–1{alpha}-hydroxylase in normal and malignant human colon. Cancer Epidemiol Biomarkers Prev. 2005;14:2370–2376.
Tangpricha V, Flanagan JN, Whitlatch LW, et al. 25-hydroxyvitamin D-1alpha-hydroxylase in normal and malignant colon tissue. Lancet. 2001;357:1673–1674.
Miller EA, Keku TO, Satia JA, Martin CF, Galanko JA, Sandler RS. Calcium, vitamin D, and apoptosis in the rectal epithelium. Cancer Epidemiol Biomarkers Prev. 2005;14:525–528.
Diaz GD, Paraskeva C, Thomas MG, Binderup L, Hague A. Apoptosis is induced by the active metabolite of vitamin D3 and its analogue eb1089 in colorectal adenoma and carcinoma cells: possible implications for prevention and therapy. Cancer Res. 2000;60:2304–2312.
Holick MF, Chen TC. Vitamin D deficiency: a worldwide problem with health consequences. Am J Clin Nutr. 2008;87:1080S–1086S.
Hanley DA, Davison KS. Vitamin D insufficiency in North America. J Nutr. 2005;135:332–337.
Prentice A, Goldberg GR, Schoenmakers I. Vitamin D across the lifecycle: physiology and biomarkers. Am J Clin Nutr. 2008;88:500S–506S.
Wei MY, Garland CF, Gorham ED, Mohr SB, Giovannucci E. Vitamin D and prevention of colorectal adenoma: a meta-analysis. Cancer Epidemiol Biomarkers Prev. 2008;17:2958–2969.
Whelan RL, Horvath KD, Gleason NR, et al. Vitamin and calcium supplement use is associated with decreased adenoma recurrence in patients with a previous history of neoplasia. Dis Colon Rectum. 1999;42:212–217.
Boutron MC, Faivre J, Marteau P, Couillault C, Senesse P, Quipourt V. Calcium, phosphorus, vitamin D, dairy products and colorectal carcinogenesis: a French case–control study. Br J Cancer. 1996;74:145–151.
Peters U, McGlynn KA, Chatterjee N, et al. Vitamin D, calcium, and vitamin D receptor polymorphism in colorectal adenomas. Cancer Epidemiol Biomarkers Prev. 2001;10:1267–1274.
Levine AJ, Harper JM, Ervin CM, et al. Serum 25-hydroxyvitamin D, dietary calcium intake, and distal colorectal adenoma risk. Nutr Cancer. 2001;39:35–41.
Boyapati SM, Bostick RM, McGlynn KA, et al. Calcium, vitamin D, and risk for colorectal adenoma: dependency on vitamin D receptor Bsmi polymorphism and nonsteroidal anti-inflammatory drug use? Cancer Epidemiol Biomarkers Prev. 2003;12:631–637.
Kampman E, Giovannucci E, van’t Veer P, et al. Calcium, vitamin D, dairy foods, and the occurrence of colorectal adenomas among men and women in two prospective studies. Am J Epidemiol. 1994;139:16–29.
Martinez ME, Marshall JR, Sampliner R, Wilkinson J, Alberts DS. Calcium, vitamin D, and risk of adenoma recurrence (United States). Cancer Causes Control. 2002;13:213–220.
Lieberman DA, Prindiville S, Weiss DG, Willett W. Risk factors for advanced colonic neoplasia and hyperplastic polyps in asymptomatic individuals. JAMA. 2003;290:2959–2967.
Kesse E, Boutron-Ruault MC, Norat T, Riboli E, Clavel-Chapelon F. Dietary calcium, phosphorus, vitamin D, dairy products and the risk of colorectal adenoma and cancer among French women of the e3n-epic prospective study. Int J Cancer. 2005;117:137–144.
Hartman TJ, Albert PS, Snyder K, et al. The association of calcium and vitamin D with risk of colorectal adenomas. J Nutr. 2005;135:252–259.
Jacobs ET, Alberts DS, Benuzillo J, Hollis BW, Thompson PA, Martinez ME. Serum 25(oh)d levels, dietary intake of vitamin D, and colorectal adenoma recurrence. J Steroid Biochem Mol Biol. 2007;103:752–756.
Oh K, Willett WC, Wu K, Fuchs CS, Giovannucci EL. Calcium and vitamin D intakes in relation to risk of distal colorectal adenoma in women. Am J Epidemiol. 2007;165:1178–1186.
Platz EA, Hankinson SE, Hollis BW, et al. Plasma 1, 25-dihydroxy- and 25-hydroxyvitamin D and adenomatous polyps of the distal colorectum. Cancer Epidemiol Biomarkers Prev. 2000;9:1059–1065.
Peters U, Hayes RB, Chatterjee N, et al. Circulating vitamin D metabolites, polymorphism in vitamin D receptor, and colorectal adenoma risk. Cancer Epidemiol Biomarkers Prev. 2004;13:546–552.
Grau MV, Baron JA, Sandler RS, et al. Vitamin D, calcium supplementation, and colorectal adenomas: results of a randomized trial. J Natl Cancer Inst. 2003;95:1765–1771.
Fedirko V, Bostick RM, Goodman M, Flanders WD, Gross MD. Blood 25-hydroxyvitamin D3 concentrations and incident sporadic colorectal adenoma risk: a pooled case–control study. Am J Epidemiol. 2010;172:489–500.
Takahashi R, Mizoue T, Otake T, et al. Circulating vitamin D and colorectal adenomas in Japanese men. Cancer Sci. 2010;101:1695–1700.
Miller EA, Keku TO, Satia JA, Martin CF, Galanko JA, Sandler RS. Calcium, dietary, and lifestyle factors in the prevention of colorectal adenomas. Cancer. 2007;109:510–517.
Hong SN, Kim JH, Choe WH, et al. Prevalence and risk of colorectal neoplasms in asymptomatic, average-risk screenees 40 to 49 years of age. Gastrointest Endosc. 2010;72:480–489.
Wagner D, Hanwell HE, Vieth R. An evaluation of automated methods for measurement of serum 25-hydroxyvitamin D. Clin Biochem. 2009;42:1549–1556.
Bushinsky DA, Monk RD. Electrolyte quintet: calcium. Lancet. 1998;352:306–311.
Craig CL, Marshall AL, Sjostrom M, et al. International physical activity questionnaire: 12-country reliability and validity. Med Sci Sports Exerc. 2003;35:1381–1395.
Matusiak D, Benya RV. Cyp27a1 and cyp24 expression as a function of malignant transformation in the colon. J Histochem Cytochem. 2007;55:1257–1264.
Ahearn TU, McCullough ML, Flanders WD, Long Q, Sidelnikov E, Fedirko V, Daniel CR, Rutherford RE, Shaukat A, Bostick RM. A randomized clinical trial of the effects of supplemental calcium and vitamin D3 on markers of their metabolism in normal mucosa of colorectal adenoma patients. Cancer Res. 2011;71:413–423.
Holick MF. Vitamin D status: measurement, interpretation, and clinical application. Ann Epidemiol. 2009;19:73–78.
Giovannucci E. Epidemiology of vitamin D and colorectal cancer: casual or causal link? J Steroid Biochem Mol Biol. 2010;121:349–354.
Wu K, Feskanich D, Fuchs CS, Willett WC, Hollis BW, Giovannucci EL. A nested case control study of plasma 25-hydroxyvitamin D concentrations and risk of colorectal cancer. J Natl Cancer Inst. 2007;99:1120–1129.
Houghton LA, Vieth R. The case against ergocalciferol (vitamin D2) as a vitamin supplement. Am J Clin Nutr. 2006;84:694–697.
Gorham ED, Garland CF, Garland FC, et al. Optimal vitamin D status for colorectal cancer prevention: a quantitative meta analysis. Am J Prev Med. 2007;32:210–216.
Gorham ED, Garland CF, Garland FC, et al. Vitamin D and prevention of colorectal cancer. J Steroid Biochem Mol Biol. 2005;97:179–194.
Connelly AE, Satia-Abouta J, Martin CF, et al. Vitamin C intake and apoptosis in normal rectal epithelium. Cancer Epidemiol Biomarkers Prev. 2003;12:559–565.
Baxter NN, Goldwasser MA, Paszat LF, Saskin R, Urbach DR, Rabeneck L. Association of colonoscopy and death from colorectal cancer. Ann Intern Med. 2009;150:1–8.
Wactawski-Wende J, Kotchen JM, et al. Calcium plus vitamin D supplementation and the risk of colorectal cancer. N Engl J Med. 2006;354:684–696.
Acknowledgments
This work was supported by Konkuk University in 2011.
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Hong, S.N., Kim, J.H., Choe, W.H. et al. Circulating Vitamin D and Colorectal Adenoma in Asymptomatic Average-Risk Individuals Who Underwent First Screening Colonoscopy: A Case–Control Study. Dig Dis Sci 57, 753–763 (2012). https://doi.org/10.1007/s10620-011-1926-1
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s10620-011-1926-1