Abstract
Background
Irritable bowel syndrome patients have abnormal visceral perception. Probiotic organisms may produce beneficial effects in these patients by reducing visceral hypersensitivity.
Aim
To investigate the effects of the probiotic organism, Bifidobacterium infantis 35624, on post-inflammatory visceral hypersensitivity in rats.
Methods
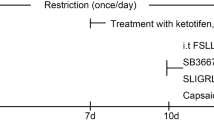
Colitis was induced using intracolonic administration of trinitrobenzenesulfonic acid; control rats received saline (day 0). Myeloperoxidase (MPO) levels and colonic damage scores were determined. From days 15–29, rats (n = 10/group) rats were orally dosed with 2 ml of B. infantis ≥ 108 colony-forming units/ml or vehicle (MRS broth). A second series of rats (n = 10/group) was dosed in the same manner from days 15–59. The level of colonic stimulation during colorectal distension (CRD) was determined by recording a visceromotor response (VMR) to CRD at 30 mmHg pre- and post-treatment. Post-treatment samples of colonic tissue were weighed, graded for morphologic damage, and assayed for MPO levels.
Results
All rats were hypersensitive at day 15. On day 30, hypersensitivity to colorectal distension remained in the vehicle group, but was significantly reduced in the B. infantis group (mean VMR/10 min: vehicle = 15.4 ± 1.0 vs. B. infantis = 7.6 ± 1.0, p < 0.001). A similar, significant effect was observed at day 60. On both day 30 and day 60, tissue weight, colonic damage scores, and MPO levels resembled those of control animals.
Conclusions
Oral administration of Bifidobacterium infantis 35624 normalized sensitivity to colorectal distension in a rat model of post-inflammatory colonic hypersensitivity.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Although the etiology and pathophysiology of irritable bowel syndrome (IBS) are unknown, the symptoms include abdominal cramping and pain that is often concurrent with abnormal bowel habits including diarrhea, constipation, or alternating episodes of both. One important observation is that the symptoms of IBS are due in part to alterations in visceral perception [1–3]. Also important is the observation that as many as 40% of IBS patients can correlate the onset of their symptoms with the resolution of a prior episode of colitis [4, 5]. Since episodes of colitis involve both interactions with bacterial flora and immune reactions within the intestine [6, 7], a therapy that can manipulate both of those factors may be effective at preventing the visceral hypersensitivity.
Probiotic bacteria are defined as harmless organisms that contribute to the overall health of the gastrointestinal (GI) tract [8, 9]. While the exact mechanisms of action are unknown, probiotic bacteria may contribute to GI health by promoting a beneficial immune response or interfering with pathogenic bacteria [9]. Clinical studies have shown positive effects of the probiotic bacterium Bifidobacterium infantis 35624 on immune response and symptoms of IBS [10, 11].
To test the hypothesis that probiotic bacteria have a beneficial effect in IBS patients through a reversal of post-inflammatory visceral hypersensitivity, we examined the effects of ingestion of B. infantis 35624 on colonic hypersensitivity in a validated rodent model in which an acute inflammation of the colon is associated with long-term, visceral hypersensitivity [12–16].
Methods
Animals
Drug-naive adult male Sprague–Dawley rats (Charles River, Wilmington, MA) weighing 200–225 g were housed singly in sterile cages in the V.A. animal facility under controlled conditions of lighting (12 h light–dark cycles) with free access to food and water as approved by the V.A.M.C. Animal Use and Care Sub-committee. During the first 5–8 days after arrival, the animals were acclimatized to the V.A. animal facility. Additionally, 7 days before colonic sensitivity assessment, the rats were brought to the laboratory for 2 h daily between 10:00 AM and 2:00 PM to acclimatize them to the laboratory.
Induction of Colitis
Rats were fasted overnight (12 to 18 h) and then briefly anesthetized with isoflurane (5%). While sedated, the rats received an enema (8.0 cm from anus, flexible tubing ID 3.0 mm) of trinitrobenzenesulfonic acid (TNBS) (50 mg/kg, 0.5 ml, 25% EtOH). Using the same methodology, an additional series of control rats received an enema of saline (0.5 ml). To prevent any loss of the liquid enema, the rats were then held so that the rectum was elevated with relation to the head until they regained consciousness.
Preparation of Bifidobacterium
Freezer stocks of B. infantis 35624 were stored at −86°C until use. Fresh bacterial cultures were prepared from thawed freezer stocks by adding 100 μl to 9 ml MRSB and incubating at 37°C for 48 h in an anaerobic jar. Turbid cultures were then vortex mixed, transferred into sterile 50-ml conical tubes, and centrifuged at 8,000 × g for 10 min at 15°C. The cultures were then concentrated by removing 2.5 ml of broth. The bacterial pellet was then resuspended, divided into aliquots (≥ 108 colony-forming units (CFU)/ml) and stored at 4°C. To verify the purity of each aliquot, each culture was isolation streaked in duplicate. The bacterial concentration was determined in triplicate from 10−6 to 10−9 by serially diluting 1 ml of the stock culture in 9 ml of sterile PBS and spread plating 100 μl. Each culture was sub-cultured once by adding 100 μl to 9 ml MRSB and incubating as above.
Dosing
For dosing, a 16-gauge feeding needle was flame-sterilized and used to prepare a 3-ml syringe to deliver 2 ml of culture (approximately 2 × 108 CFU) or MRS broth. Once all syringes were prepared, rats were briefly placed in a plastic restraint cone and orally dosed. The vehicle group was always dosed first, and gloves were changed between groups to prevent cross-contamination of the groups. Animals in the first series received B. infantis or vehicle daily for days 15 to 29; animals in the second series received B. infantis or vehicle daily for days 15 to 59. The dose of B. infantis was selected to mirror the dosages used in clinical studies [10, 11].
Measurement of Visceromotor Behavioral Response
Rats were fasted overnight (12 to 18 h) and brought to the laboratory for strain-gauge instrumentation. Briefly, under continuous administration of 1.5–3.0% isoflurane, a small incision was made in the rat’s abdomen. A strain-gauge transducer (R B Products, Madison, WI) was then sutured (seven stitches, 3–0 silk) to the right external oblique muscle, 1 cm from the midline. The skin was then sutured over the strain gauge and the lead wires were looped around the rat’s right side where they were secured to the back by a single suture to the skin. A colorectal balloon (5 cm, latex) was then inserted via the anal canal (11 cm) and secured to the base of the tail with tape. Once the animal had recovered from the surgery, the strain gauge was connected via a shielded cable to a Grass Model 7 Polygraph (Astro-Med, Inc., West Warwick, RI) for the recording of abdominal muscle contractions or movement. To determine the visceromotor response (VMR) to colorectal distension (CRD) (30 mmHg), abdominal contractions were recorded during the 10 m distension period. Each VMR experiment consisted of a total of six distensions (10 m at 30 mmHg) separated by a 10 min rest period (0 mmHg).
Following the VMR experiment, the rats were sedated with isoflurane as described previously and the colonic balloon and strain gauge were carefully removed. The incision was closed with 3–0 silk and an analgesic/antibiotic ointment was applied topically to the wound. After completion of the dosing protocol, rats were euthanized through inhalation of isoflurane before removal of instrumentation or colonic tissue.
Morphological Scoring
To verify the absence of gross inflammation at day 30 or day 60 post-enema, after euthanasia, the entire colon was removed from the rat. The distal 2 cm were removed and then the next 5 cm were retained for morphological scoring. The 5-cm colonic tissue sample was opened along the mesenteric border and cleaned with saline. The tissue was weighed and a morphologic score was assigned according to the following scale (adapted from [17]): 0 = no damage; 1 = localized inflammation, no ulcers; 2 = one ulcer, no inflammation; 3 = ulcer with inflammation at one site; 4 = two or more ulcers and/or sites of inflammation; 5 = two or more ulcers and/or sites of inflammation with one site extending >1 cm along the tissue. The colonic tissue samples were frozen in liquid nitrogen for later analysis.
Myeloperoxidase (MPO) Analysis
MPO activity is a rapid, biochemical measurement of neutrophil infiltration that positively correlates with histological scoring systems to represent the extent of inflammation in intestinal tissue [16, 18], and was measured in this study to provide additional evidence of the absence of inflammation at day 30 or day 60 post-enema. Frozen colonic tissue samples were weighted and homogenized at 20 mg tissue in 1 ml of the following buffer: 50 mM KH2PO4, 100 mM Na2HPO4, 0.5% (w/v) hexadecyltrimethylammonium bromide (HTAB), pH 6.0. A portion of the homogenized sample (0.2 ml) was then placed in a cryogenic tube and frozen in liquid nitrogen. Once all the samples were homogenized, they were allowed to thaw at room temperature (30 m). Thawed samples were sonicated for 10 s in an ice bath and re-frozen in liquid nitrogen. The samples were then slowly thawed on ice (60 m) before being re-frozen in liquid nitrogen. Finally, the samples were allowed to slowly thaw on ice (60 m). Once thawed, samples were centrifuged at 12,000 × g and 10 μl aliquots were added in duplicate to a 96-well microplate. A standard curve consisting of horseradish peroxidase (HRP) from 1 to 50 ng/10 μl was also set up in duplicate. Then, 100 μl of 3,3′,5,5′-tetramethylbenzidine (TMB) liquid substrate system was added to each well and allowed to react in the dark for 10 m. The reaction was then stopped by adding 100 μl of 0.1 M H2SO4 and the absorbance at 450 nm was read using a Dynatech MR5000 ELISA reader. Results were expressed as ng MPO/g tissue wet weight.
Statistical Methods
Animals that were hypersensitive to CRD on day 15 were randomly assigned to a treatment group. Five rats were excluded from the study after randomization based on the lack of colonic hypersensitivity on day 15. Each data series was analyzed separately at pre-treatment and post-treatment time points to compare groups with respect to VMR. An unpaired two-sample t test was used to compare treatment groups pre-treatment. Treatment groups were compared post-treatment using analysis of covariance with baseline VMR as the covariate. VMR analysis results were expressed as mean ± standard error of the mean (SEM). Analysis of the colonic damage scores, colonic wet weight and colonic MPO levels were performed with a parametric or non-parametric (Kruskal–Wallis) one-way ANOVA as appropriate. p < 0.05 was considered significant for all tests. Statistical tests were performed using The Statistical Analysis System version 9.2 (SAS Institute, Cary, NC, USA) and GraphPad Prism 4.0c (GraphPad Software, San Diego, CA).
Results
Verification of Post-Inflammatory Colonic Hypersensitivity
In this study, we confirmed that colorectal administration of TNBS resulted in post-inflammatory chronic hypersensitivity to distension of the colorectum, as demonstrated previously [14, 16]. Specifically on day 15 post-enema, colonic sensitivity was assessed in all rats and those with a consistently exaggerated or hypersensitive response to a low level (30 mmHg) of CRD were used in the current study. As illustrated in Fig. 1a, on day 15, rats that received the TNBS enema had a hypersensitive response to non-noxious CRD as measured by VMR (13.3 ± 1.1); a much smaller response was seen in the group that received a saline enema only (6.3 ± 0.8, p < 0.001). This hypersensitivity to non-noxious CRD was still present on day 30 in rats that had received a TNBS enema (TNBS: 12.6 ± 1.0, Saline: 8.1 ± 0.7, p < 0.01).
a Verification of post-inflammatory colonic hypersensitivity. Rats received an enema of either saline (open bars, n = 10) or TNBS (dark grey bars, n = 6) on day 0. Data presented is VMR to CRD (mean ± SEM), measured on day 15 and day 30 post-enema. **p < 0.01, ***p < 0.001 vs. saline. b Effect of 15 days of dosing B. infantis 35624 on post-inflammatory colonic hypersensitivity. All rats received a TNBS enema on day 0. On day 15 post-enema, rats began receiving daily doses (2 ml, p.o.) of either vehicle (MRSB, black bars, n = 10) or B. infantis 35624 (light grey bars, n = 9) until day 30. Data presented is VMR to CRD (mean ± SEM), measured on day 15 and day 30 post-enema. ††† p < 0.001 vs. vehicle. c Effect of 45 days of dosing B. infantis 35624 on post-inflammatory colonic hypersensitivity. All rats received a TNBS enema on day 0. On day 15 post-enema, rats began receiving daily doses (2 ml, p.o.) of either vehicle (MRSB, black bars, n = 10) or B. infantis 35624 (light grey bars, n = 10) until day 60. Data presented is VMR to CRD (mean ± SEM), measured on day 15 and day 60 post-enema. †† p < 0.01 vs. vehicle
Effect of B. infantis 35624 on Colonic Sensitivity
At day 30 post-enema, as on day 15, the vehicle group remained hypersensitive to luminal distension of the colorectum (Fig. 1b). In contrast, the group treated with B. infantis 35624 had a VMR resembling that seen in control rats that were not hypersensitive (treated with a saline enema). Daily dosing of vehicle from days 15 to 30 resulted in a slight decrease (13%) in colorectal hypersensitivity, while daily dosing with B. infantis 35624 resulted in a 57% decrease in the mean VMR. Rats that received 15 days of dosing with B. infantis 35624 had a significantly lower VMR to CRD (30 mmHg) compared to the vehicle group on day 30-post enema (p < 0.001).
Unlike the response at day 30 (Fig. 1b), on day 60 post-enema, the vehicle group was not as consistently hypersensitive to CRD (Fig. 1c). This resulted in a 37% lower mean VMR for the vehicle group, indicating that there was a decrease in colorectal hypersensitivity, however the response remained greater than that seen in a saline enema-treated group at day 30. Concurrent dosing of B. infantis 35624 on days 15 to 60 significantly decreased the mean VMR to CRD (30 mmHg) a further 55% (p < 0.01).
Effect of B. infantis 35624 on Colonic Mucosal Integrity
Summary data for colonic damage score, colonic wet weight (5 cm), and MPO levels are presented in Table 1. Overall, all three parameters demonstrated that the acute colonic inflammation caused by the TNBS enema had resolved by day 30 or day 60, providing additional evidence for post-inflammatory colonic hypersensitivity. Additionally, colons of both B. infantis-treated groups resembled the saline enema-treated control group.
Discussion
IBS is a common, chronic, and relapsing GI disorder that is characterized by abdominal pain and bloating with abnormal bowel habits. The symptoms of IBS are due in part to alterations in visceral perception, manifested by both hyperalgesia and allodynia [1–3]. Consumption of probiotics may reduce symptoms in IBS patients, as shown in studies with B. infantis 35624 [10, 11]. In this study, colorectal administration of TNBS resulted in post-inflammatory chronic hypersensitivity to luminal distension, with rats exhibiting a consistently exaggerated or hypersensitive response to non-noxious CRD on day 15, 30, and 60 post-enema. In contrast, the group who were administered B. infantis 35624 had a normal level of visceral sensitivity, resembling that seen in control rats that were not hypersensitive (treated with a saline enema). Taken together, these data demonstrate that oral administration of B. infantis 35624 reversed post-inflammatory visceral hypersensitivity.
Our findings are consistent with those of other studies of probiotics in animal models of colonic hypersensitivity. One study found that B. infantis 35624 reduced pain behaviors with colorectal distension in two rat strains; this effect was not seen with Lactobacillus salivarius UCC118 or Bifidobacterium breve UCC2003 [19]. Supplementation with Lactobacillus paracasei was found to attenuate increases in visceral sensitivity during antibiotic administration in mice [20], while administration of Lactobacillus farciminis prevented stress-induced colonic hypersensitivity and paracellular permeability in rats [21]. Another study found inhibitory effects of live and heat-killed Lactobacillus reuteri on visceral pain induced by colonic distension in rats [22].
These data are also consistent with the results of clinical trials of B. infantis 35624 in patients with IBS. A pilot study of 77 subjects with IBS treated for 8 weeks with either L. salivarius or B. infantis 35624 (both dosed daily at 1010 CFU in malted milk) showed that B. infantis 35624, but not L. salivarius, alleviated symptoms of IBS (e.g., pain/discomfort, bloating/distension), and normalized the ratio of anti-inflammatory/pro-inflammatory cytokines (IL-10/IL-12) [10]. In a larger study, 362 female IBS patients were dosed daily with B. infantis 35624 (106, 108, or 1010 CFU), or placebo, in a capsule for 4 weeks [11]. The primary treatment group (1010) was not different from placebo for symptoms of IBS, but that dose group was determined to have significant formulation issues. The 108 treatment group was significantly better than placebo for nine of 11 IBS symptom scores.
Knowledge of the brain-gut-microbiome axis, the concept of bi-direction influences between the brain and the commensal bacteria that influence the host’s physiology, is an ever-evolving area of GI research (reviewed by [23]). Interestingly, bacteria can influence colonic epithelial cells to secrete chemokines that target pathogenic bacteria [24], while at the same time promoting immune cell differentiation that promotes tolerance for commensal strains and also targets pathogens for elimination [25, 26]. Thus, disturbances within the colonic microflora are thought to trigger the development of GI diseases. Indeed, two studies have demonstrated that the fecal microbiota of IBS patients is significantly different from healthy controls [27, 28]. Relevant to this study, rodent bacterial flora influences TBNS-colitis in that anaerobic strains are associated with transmural inflammation [29] and there is a positive correlation between macroscopic damage scores and the amount of total colonic flora [30]. Thus, we can anticipate that the commensal flora of the rats in this study influenced the extent of acute TNBS colitis; however, we cannot speculate about the composition of the gut flora at day 30 or day 60 post-enema. Future studies will provide a more rigorous examination of the changes in gut flora in the post-inflammatory state to provided insight into potential mechanisms the efficacy of B. infantis 35624 in preventing post-inflammatory colonic hypersensitivity.
Clinical studies have demonstrated abnormal mucosal function, including enhanced colonic permeability, in post-infectious IBS patients (reviewed by [31, 32]). In rodents, during active TNBS-induced colitis there is increased colonic permeability [33, 34], which persists for at least 1 week following the TNBS enema [35]. TNBS colitis has also been shown to cause a concomitant increase in blood–brain barrier permeability over the same time period [36], which could promote central sensitization and/or stress-axis dysfunction as shown by increased corticotropin-releasing factor expression in the paraventricular nucleus of the hypothalamus at 3 and 30 days post-enema [37]. In the TNBS colitis model of inflammatory bowel disease, the effects of probiotics on colonic permeability have been shown to be strain-specific. Two studies by Lamine et al. [38, 39] showed that when dosed for 15 days before the enema, at 4 days post-enema, Lactobacillus farciminis could prevent both mucosal damage and increased colonic permeability associated with TNBS colitis. In contrast, Lactobacillus plantarum species 299 failed to change the amount of colonic damage or the associated increase in permeability at 1 week post-enema, when dosing was started 24 h after the TNBS enema [40]. While permeability was not measured in this study, using a similar experimental protocol, Sommerfield et al. [41] demonstrated that carbachol-induced colonic secretion on day 30 post-TNBS enema was reduced following 15 days of B. infantis 35624 treatment, supporting a role for B. infantis 35624 in the maintenance of colonic mucosal integrity. There is also evidence that B. infantis can secrete factors that directly improve colonic mucosal integrity. T84 human epithelial cells treated with conditioned media from B. infantis had both increased transepithelial resistance and increased expression of tight junction proteins while the same media decreased histological inflammation scores and significantly reduced mannitol flux in the colon of IL-10 knockout mice [42]. Since increased gut permeability can promote post-infectious IBS symptoms through local release of immune mediators that stimulate visceral afferents [32], future studies will address whether the inhibition of post-inflammatory colonic hypersensitivity by B. infantis 35624 is due to normalization of colonic permeability.
While the exact mechanisms are unknown, current evidence suggests a pathologic crosstalk between the immune and peripheral nervous systems through cytokines and other inflammatory mediators that promote afferent sensitization as a probable cause for the development of post-inflammatory visceral hypersensitivity (reviewed by [43, 44]). In support of a central sensitization mechanism, Zhou and colleges [45] demonstrated that rats with post-inflammatory colonic hypersensitivity at 16 weeks following a TNBS enema have increased expression splice variants of the NR1 subunit of the N-methyl-d-aspartic acid (NMDA) receptor in the superficial lamina of the spinal cord. Those changes at the spinal level are preceded by changes in the expression of NR1 splice variants in the myenteric plexus at 4 weeks post-TNBS enema [46]. However, the effect of B. infantis 35624 on NMDA receptor expression is unknown. Serotonin (5-HT) is another potential mediator of post-inflammatory hypersensitivity that can act both centrally and peripherally. In both a murine model of post-infective visceral hypersensitivity and a rat model of post-inflammatory hypersensitivity, the experimentally induced hypersensitivity could be inhibited by selective 5-HT3 receptor antagonists [47, 48]. Additionally, in both normal and maternally separated Sprague–Dawley rats, chronic B. infantis 35624 treatment decreased the content of the serotonin metabolite, 5-hydroxyindoleacetic acid (5-HIAA), in specific brain regions [49, 50]. Determining whether B. infantis 35624 effects 5-HT content and/or metabolism in this model of post-inflammatory colonic hypersensitivity remains to be explored. Finally, vagal afferents mediate anti-inflammatory effects in TNBS colitis, i.e., inflammation was worse in vagal deafferented animals [34]. A similar vagal-dependent anti-inflammatory mechanism was demonstrated in the murine dextran sulfate sodium model of colitis [51]. However, B. infantis 35624 was able to reduce the disease activity index and tissue markers of inflammation to similar extents in sham and vagotomized mice, which suggests that a vagal antinociceptive mechanism [52, 53] is not mediating the effect of B. infantis in this study.
In conclusion, oral administration of B. infantis 35624 normalized sensitivity to colonic distension in a rat model of post-inflammatory colonic hypersensitivity. Additional studies are planned to explore the multiple potential mechanisms of action for this normalization of colonic hypersensitivity.
References
Mayer EA, Gebhart GF. Basic and clinical aspects of visceral hyperalgesia. Gastroenterology. 1994;107:271–293.
Ritchie J. Pain from distension of the pelvic colon by inflating a balloon in the irritable colon syndrome. Gut. 1973;14:125–132.
Whitehead WE, Holtkotter B, Enck P, et al. Tolerance for rectosigmoid distention in irritable bowel syndrome. Gastroenterology. 1990;98:1187–1192.
Chaudhary NA, Truelove SC. Human colonic motility. A comparative study of normal subjects, patients with ulcerative colitis, and patients with the irritable colon syndrome. Gastroenterology. 1968;54:777–778.
Collins SM. Stress and the gastrointestinal tract IV. Modulation of intestinal inflammation by stress: basic mechanisms and clinical relevance. Am J Physiol Gastrointest Liver Physiol. 2000;280:G315–G318.
Sartor RB, Bond TM, Schwab JH. Systemic uptake and intestinal inflammatory effects of luminal bacterial cell wall polymers in rats with acute colonic injury. Infect Immun. 1988;56:2101–2108.
Shorter RG, Tomasi TB, Huizenga KA, Spencer RJ, Stobo JD. The immunology of chronic ulcerative colitis and Crohn’s disease. Ann N Y Acad Sci. 1976;278:586–591.
Gionchetti P, Rizzello F, Venturi A, Campieri M. Probiotics in infective diarrhoea and inflammatory bowel disease. J Gastoenterol Hepatol. 2000;15:489–493.
Rolfe RD. The role of probiotic cultures in the control of gastrointestinal health. J Nutr. 2000;130:396S–402S.
O’Mahony L, McCarthy J, Kelly P, et al. Lactobacillus and Bifidobacterium in irritable bowel syndrome: symptom responses and relationship to cytokine profiles. Gastroenterology. 2005;128:541–551.
Whorwell PJ, Altringer L, Morel J, et al. Efficacy of an encapsulated probiotic Bifidobacterium infantis 35624 in women with irritable bowel syndrome. Am J Gastroenterol. 2006;101:1581–1590.
Lacheze C, Coelho A-M, Fioramonti J, Bueno L. Influence of trimebutine on inflammation- and stress-induced hyperalgesia to rectal distension in rates. J Pharm Pharmacol. 1998;50:921–928.
Goldhill J, Pichat P, Roome N, Angel I, Arbilla S. Effect of mizolastine on visceral sensory afferent sensitivity and inflammation during experimental colitis. Arzneimittel-Forschung. 1998;48:170–184.
Gibson MS, Greenwood-Van Meerveld B. An acute inflammatory insult induces long term colonic hypersensitivity. Am J Gastroenterol. 2000;95:2534. [abstract].
Diop L, Raymond F, Fargeau H, Petoux F, Chovet M, Doherty AM. Pregabaline (CI-1008) inhibits the trinitrobenzene sulfonic acid acid-induced chronic colonic allodynia in the rat. J Pharmacol Exp Ther. 2002;302:1013–1022.
Greenwood-Van Meerveld B, Johnson AC, Foreman RD, Linderoth B. Spinal cord stimulation attenuates visceromotor reflexes in a rat model of post-inflammatory colonic hypersensitivity. Auton Neurosci. 2005;122:69–76.
Morris GP, Beck PL, Herridge MS, Depew W, Szewczuk MR, Wallace JL. Hapten-induced model of chronic inflammation and ulceration in the rat colon. Gastroenterology. 1989;96:795–803.
Krawisz JE, Sharon P, Stenson WF. Quantitative assay for acute intestinal inflammation based on myeloperoxidase activity. Assessment of inflammation in rat and hamster models. Gastroenterology. 1984;87:1344–1350.
McKernan DP, Fitzgerald P, Dinan TG, Cryan JF. The probiotic Bifidobacterium infantis 35624 displays visceral antinociceptive effects in the rat. Neurogastroenterol Motil. 2010;22:1029–1035. e268.
Verdú EF, Bercik P, Verma-Gandhu M, et al. Specific probiotic therapy attenuates antibiotic induced visceral hypersensitivity in mice. Gut. 2006;55:182–190.
Ait-Belgnaoui A, Han W, Lamine F, et al. Lactobacillus farciminis treatment suppresses stress induced visceral hypersensitivity: a possible action through interaction with epithelial cell cytoskeleton contraction. Gut. 2006;55:1090–1094.
Kamiya T, Wang L, Forsythe P, et al. Inhibitory effects of Lactobacillus reuteri on visceral pain induced by colorectal distension in Sprague-Dawley rats. Gut. 2006;55:191–196.
Collins SM, Bercik P. The relationship between intestinal microbiota and the central nervous system in normal gastrointestinal function and disease. Gastroenterology. 2009;136:2003–2014.
Sibartie S, O’Hara AM, Ryan J, et al. Modulation of pathogen-induced CCL20 secretion from HT-29 human intestinal epithelial cells by commensal bacteria. BMC Immunol. 2009;10:54.
O’Mahony L, O’Callaghan L, McCarthy J, et al. Differential cytokine response from dendritic cells to commensal and pathogenic bacteria in different lymphoid compartments in humans. Am J Physiol Gastrointest Liver Physiol. 2006;290:G839–G845.
Davies JM, Sheil B, Shanahan F. Bacterial signalling overrides cytokine signalling and modifies dendritic cell differentiation. Immunology. 2009;128:e805–e815.
Kassinen A, Krogius-Kurikka L, Mäkivuokko H, et al. The fecal microbiota of irritable bowel syndrome patients differs significantly from that of healthy subjects. Gastroenterology. 2007;133:24–33.
Tana C, Umesaki Y, Imaoka A, Handa T, Kanazawa M, Fukudo S. Altered profiles of intestinal microbiota and organic acids may be the origin of symptoms in irritable bowel syndrome. Neurogastroenterol Motil. 2010;22:512–519. e114-e115.
García-Lafuente A, Antolín M, Guarner F, et al. Incrimination of anaerobic bacteria in the induction of experimental colitis. Am J Physiol. 1997;272:G10–G15.
Hernández GA, Appleyard CB. Bacterial load in animal models of acute and chronic ‘reactivated’ colitis. Digestion. 2003;67:161–169.
Spiller R, Garsed K. Postinfectious irritable bowel syndrome. Gastroenterology. 2009;136:1979–1988.
Barbara G, Cremon C, Pallotti F, De Giorgio R, Stanghellini V, Corinaldesi R. Postinfectious irritable bowel syndrome. J Pediatr Gastroenterol Nutr. 2009;48:S95–S97.
Szepes Z, Kiss J, Molnár T, Lamarque D, Jancsó G, László F. Capsaicin-sensitive mechanisms in the modulation of rat colonic vascular permeability under physiological and pathological conditions. J Physiol Paris. 1997;91:123–126.
Mazelin L, Theodorou V, More J, Fioramonti J, Bueno L. Protective role of vagal afferents in experimentally-induced colitis in rats. J Auton Nerv Syst. 1998;73:38–45.
Stein J, Ries J, Barrett KE. Disruption of intestinal barrier function associated with experimental colitis: possible role of mast cells. Am J Physiol. 1998;274:G203–G209.
Natah SS, Mouihate A, Pittman QJ, Sharkey KA. Disruption of the blood-brain barrier during TNBS colitis. Neurogastroenterol Motil. 2005;17:433–446.
Greenwood-Van Meerveld B, Johnson AC, Schulkin J, Myers DA. Long-term expression of corticotropin-releasing factor (CRF) in the paraventricular nucleus of the hypothalamus in response to an acute colonic inflammation. Brain Res. 2006;1071:91–96.
Lamine F, Fioramonti J, Bueno L, et al. Nitric oxide released by Lactobacillus farciminis improves TNBS-induced colitis in rats. Scand J Gastroenterol. 2004;39:37–45.
Lamine F, Eutamène H, Fioramonti J, Buéno L, Théodorou V. Colonic responses to Lactobacillus farciminis treatment in trinitrobenzene sulphonic acid-induced colitis in rats. Scand J Gastroenterol. 2004;39:1250–1258.
Kennedy RJ, Hoper M, Deodhar K, Kirk SJ, Gardiner KR. Probiotic therapy fails to improve gut permeability in a hapten model of colitis. Scand J Gastroenterol. 2000;35:1266–1271.
Sommerfield D, O’Brien N, Kiely B, et al. Influence of Bifidobacterium infantis feeding on secretagogue response and gut barrier function in rats recovering from colitis. Gastroenterology 2003;124:A311. M1113 [abstract].
Ewaschuk JB, Diaz H, Meddings L, et al. Secreted bioactive factors from Bifidobacterium infantis enhance epithelial cell barrier function. Am J Physiol Gastrointest Liver Physiol. 2008;295:G1025–G1034.
Vergnolle N. Postinflammatory visceral sensitivity and pain mechanisms. Neurogastroenterol Motil. 2008;20:73–80.
Hughes PA, Brierley SM, Blackshaw LA. Post-inflammatory modification of colonic afferent mechanosensitivity. Clin Exp Pharmacol Physiol. 2009;36:1034–1040.
Zhou Q, Price DD, Caudle RM, Verne GN. Spinal NMDA NR1 subunit expression following transient TNBS colitis. Brain Res. 2009;1279:109–120.
Zhou Q, Caudle RM, Price DD, Del Valle-Pinero AY, Verne GN. Selective up-regulation of NMDA-NR1 receptor expression in myenteric plexus after TNBS induced colitis in rats. Mol Pain. 2006;2:3.
Keating C, Beyak M, Foley S, et al. Afferent hypersensitivity in a mouse model of post-inflammatory gut dysfunction: role of altered serotonin metabolism. J Physiol. 2008;586:4517–4530.
Choi YD, Sung TS, Kim HJ, La JH, Kim TW, Yang IS. Increased 5-hydroxytryptamine mediates post-inflammatory visceral hypersensitivity via the 5-hydroxytryptamine 3 receptor in rats. Dig Dis Sci. 2008;53:2909–2916.
Desbonnet L, Garrett L, Clarke G, Bienenstock J, Dinan TG. The probiotic Bifidobacteria infantis: an assessment of potential antidepressant properties in the rat. J Psychiatr Res. 2008;43:164–174.
Desbonnet L, Garrett L, Clarke G, Kiely B, Cryan JF, Dinan TG. Effects of the probiotic Bifidobacterium infantis in the maternal separation model of depression. Neuroscience. 2010;170:1179–1188.
van der Kleij H, O’Mahony C, Shanahan F, O’Mahony L, Bienenstock J. Protective effects of Lactobacillus reuteri and Bifidobacterium infantis in murine models for colitis do not involve the vagus nerve. Am J Physiol Regul Integr Comp Physiol. 2008;295:R1131–R1137.
Diop L, Rivière PJ, Pascaud X, Dassaud M, Junien JL. Role of vagal afferents in the antinociception produced by morphine and U-50, 488H in the colonic pain reflex in rats. Eur J Pharmacol. 1994;257:181–187.
Gschossmann JM, Mayer EA, Miller JC, Raybould HE. Subdiaphragmatic vagal afferent innervation in activation of an opioidergic antinociceptive system in response to colorectal distension in rats. Neurogastroenterol Motil. 2002;14:403–408.
Acknowledgments
This study was supported by a research grant from the Procter & Gamble Company.
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Johnson, A.C., Greenwood-Van Meerveld, B. & McRorie, J. Effects of Bifidobacterium infantis 35624 on Post-Inflammatory Visceral Hypersensitivity in the Rat. Dig Dis Sci 56, 3179–3186 (2011). https://doi.org/10.1007/s10620-011-1730-y
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s10620-011-1730-y