Abstract
Intestinal permeability and the effect of NSAIDs on permeability were investigated in 14 irritable bowel syndrome (IBS) patients and 15 healthy subjects. In the study, 24-h urinary recoveries of orally administered polyethylene glycols (PEGs 400, 1500, and 4000) were not significantly different in healthy subjects and IBS patients before or after NSAID ingestion. Lactulose mannitol ratios in healthy subjects and IBS patients were not significantly different. Only time-dependent monitoring of PEG excretion showed that NSAIDs enhanced intestinal permeability for PEG 4000 in healthy subjects (P = 0.050) and for PEGs 400, 1500, and 4000 in IBS patients (P = 0.012, P = 0.041, and P = 0.012, respectively). These results show that intestinal permeability in IBS patients is not different from that in healthy subjects; NSAIDs compromise intestinal permeability in IBS patients to a greater extent than in healthy subjects, which suggests that IBS is associated with an altered response of the intestinal barrier to noxious agents.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Irritable bowel syndrome (IBS) is characterized by abdominal pain and altered bowel habits. Changes in intestinal microbiota, inflammatory cells, and permeability have been suggested to be involved in the pathophysiology of IBS [1–3]. An increase in intestinal permeability will expose the subject to intraluminal antigens, microbiota, and bacterial toxins.
Whether permeability is increased in IBS patients is still a matter of controversy. Intestinal permeability was reported enhanced in 16–50% of post-infectious IBS patients [4, 5] (post-infectious IBS patients make up 16% of the IBS population [6, 7]). In post-infectious and non-post-infectious diarrhea-predominant IBS patients, permeability of the (proximal) small intestine was increased in comparison to healthy subjects and with constipation-predominant IBS patients [8]. On the other hand, in some studies containing relatively large groups of IBS patients, no indication of enhanced intestinal permeability was found [9, 10]. A decrease of intestinal permeability in IBS patients was also reported [11].
IBS is significantly associated with the use of analgesics [12, 13]. Visceral hypersensitivity is thought to play a pivotal role in IBS symptom generation [14]. Non-steroidal anti-inflammatory drugs (NSAIDs) tend to decrease the initial perception threshold and reduce the basal nerve discharge rate causing visceral hypersensitivity [15, 16]. Interaction between luminal aggressive factors like NSAIDs, and mucosal defense may lead to low-grade inflammation [17, 18]. Low-grade inflammation is known in (post-infectious) IBS patients and may contribute to visceral hypersensitivity [3, 4, 19]. The majority of IBS patients use NSAIDs without experiencing apparent exacerbation of their symptoms. Nevertheless, IBS patients who use NSAIDs are likely to have persistent IBS [13]. NSAIDs are known to increase intestinal permeability [17, 20]. We hypothesize that the use of NSAIDs by IBS patients sustains a condition of low-grade inflammation which, even at low dosage of NSAIDs, is mediated by increased intestinal permeability. To test this hypothesis, we studied the effect of limited administration of NSAIDs on intestinal permeability in IBS patients. Healthy subjects received the same treatment as reference.
Commonly used tests to assess intestinal permeability such as the sugar absorption test are based on the selective urinary excretion of orally administered probes, usually a combination of a relatively small permeant compound and a larger compound with restricted permeability. Relating recovery of the larger to that of the smaller probe minimizes the influence of factors like gastric emptying, intestinal motility, and renal function, which should affect both probes equally [21]. Parlesak et al. introduced a mixture of polyethylene glycols (PEG) with relative molecular masses Mr 400, 1500, 4000, and 10000, which may offer the possibility to assess size-dependent intestinal permeability [22, 23]. The molecular size of PEG 10000 represents the size of substances of interest such as allergens and bacterial products like lipopolysaccharides [23, 24]. Intestinal permeability in IBS has been studied by using sugar absorption tests and by testing the permeability for 51Cr-EDTA [4, 5, 8–11].
We decided to test intestinal permeability in IBS by using a polyethylene glycol mixture similar to that described by Parlesak et al. [22] and, moreover, by monitoring the kinetics of urinary excretion of the various polyethylene glycols anticipating that kinetic measurements might provide additional information on intestinal permeability. PEG excretion was studied before (and 2 days after) administration of NSAIDs in IBS patients and healthy subjects to analyze if permeability would be more affected by limited administration of NSAIDs in IBS patients than in healthy subjects. Enhanced intestinal permeability may also result from intestinal ischemia and enterocyte death. This was evaluated from the release of intestinal fatty acid-binding protein (I-FABP) into urine [25–27].
Materials and Methods
Subjects
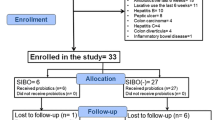
The PEG permeability test and analysis were evaluated in 15 healthy Caucasian persons. Healthy subjects had neither intestinal complaints nor a history of bowel resection, and were not receiving any treatment known to be associated with alterations in gastrointestinal function or with gastrointestinal side effects. The IBS study group consisted of 14 Caucasian IBS patients who were diagnosed according to the Rome II criteria for IBS [28]. The subjects were not allowed to take NSAIDs or acetylsalicylic acid 3 days prior to the tests [17, 18]. None of the healthy subjects and IBS patients used antibiotics in the 2 weeks prior to the test. There was no history of intestinal infection prior to and interfering with the study. None of the IBS patients was intolerant to lactose. The study was approved by the ethics committee of the University Medical Center Utrecht. Written informed consent was obtained from all subjects.
Study Protocol
Intestinal permeability was measured in IBS patients and healthy subjects using a PEG and a lactulose mannitol (L/M) test. The L/M test was meant as an alternative and well-established indicator of intestinal permeability. The PEG solution contained 5 g PEG 400, 1.5 g PEG 1500, 5 g PEG 4000, and 10 g PEG 10000 dissolved in 100 mL water [22]. Sorbate (0.1%) was added as preservative. PEGs with Mr 400, Mr 1500, and Mr 4000 were obtained from Bufa Chemical Company, Uitgeest, The Netherlands, and PEG with Mr 10000 from Sigma Chemical Company, St. Louis, MO. The L/M solution contained 2 g mannitol, 5 g lactulose, and 40 g sucrose in 100 mL water [29]. The PEG and L/M solutions were quality- and purity-controlled by the Department of Pharmacy of the UMC Utrecht. PEG and L/M tests were performed in random order, at least 1 week apart. In healthy subjects, the tests were performed twice to check the reproducibility of test procedure and assay (test 1 and test 2). At least 1 week after the PEG and L/M reproducibility tests, healthy subjects and IBS patients ingested the NSAID in the evenings at 10:00 pm for 2 days and intestinal permeability was measured using the PEG test starting at 8:00 am the next morning. The NSAID used was 750 mg (250 mg and 500 mg tablets) Naproxen (Centrafarm, Etten-Leur, The Netherlands). After voiding and discarding overnight urine, the fasting subjects drank a PEG or L/M solution. A further 6-h fast followed during which the subjects were allowed to drink water according to one’s needs. During the PEG test, before or after NSAID ingestion, the subjects collected urine eight times at 2-h intervals plus all the urine until the next morning. Aliquots of 30 mL of each urine portion were transferred to separate plastic tubes and the remaining parts were stored together in a container. Volumes of urine were recorded so that PEG excretion over a 24-h period could be calculated. During the L/M test, subjects collected urine over a single 6-h period. Urine samples were stored at −20°C until further analysis.
Analysis of Urine Samples
Urine samples were homogenized and 25 mL was centrifuged at 1,000 × g for 10 min. Two mL of clear supernatant was desalted by treatment with an ion-exchange resin (Bio-Rad RG 501-X8, Hercules, CA, USA). The resin was removed by centrifugation and 50 μL supernatant was analyzed by high-performance liquid chromatography (HPLC).
Parlesak et al. analyzed polyethylene glycols by two HPLC systems using differential refraction index detection [22]. These authors purified PEGs 1500, 4000, and 10000 from urine by extraction with chloroform and analyzed the extracts with one HPLC configuration. PEG 400 was analyzed in the post-extraction residue and analyzed by a different HPLC setup. We applied HPLC and implemented the novel technique of evaporative light-scattering detection [30, 31]. PEGs were analyzed with reversed-phase HPLC (Shimadzu SCL–10A VP, Shimadzu Benelux, ‘s-Hertogenbosch, The Netherlands) using a 25-cm, 5-μm Lichrospher 100-RP 18E column equipped with a 1.5-cm similar guard column (Li Chro Cart 2,504 mm, Merck KgaA, Darmstadt, Germany), and evaporative light-scattering detection (Alltech 500, Grace Alltech Applied Science, Breda, The Netherlands). The mobile phase consisted of a gradient of 40–80% methanol in water allowing analysis and quantification of all four polyethylene glycols in a single run.
Figure 1 shows a chromatogram of PEGs 400, 1500, 4000, and 10000. The compounds are mixtures of oligomers with molecular masses around the indicated means. PEG 400 was resolved into its various oligomers, the larger PEG compounds shown as a single peak each. Detection limits were 0.05 mg/mL for PEG 400 and 0.005 mg/mL for PEGs 1500, 4000, and 10000. Analytical recovery of all four PEGs from standard solutions of urine was 100 ± 4%, reproducibility 97 ± 1%. The detection limit of the analysis procedure of PEGs 1500, 4000, and 10000 could be improved by extracting PEGs from urine and concentrating the extract [22]. For this purpose, 8 mL of desalted urine supernatant was extracted with 2 mL of chloroform. One mL of the chloroform extract was dried under a mild stream of nitrogen, then the residue taken up in 200 μL of HPLC-mobile phase solvent and 50 μL was analyzed.
Urine lactulose, mannitol and creatinine concentrations were measured by routine clinical chemical analysis at the Central Diagnostic Laboratory of the UMC Utrecht with a Synchron CX4 random-access multi-analyzer (Beckman Instruments Inc., Brea, CA, USA). I-FABP was determined in urine using a human I-FABP sandwich ELISA (HyCult Biotechnology B·V., Uden, The Netherlands).
Calculations and Data Analysis
Intestinal permeability was evaluated from the area under the PEG-excretion time-curves and from the percentage PEG recovered from the ingested dose. An L/M ratio over 0.03 was considered as an indication of increased intestinal permeability [29, 32, 33].
Statistical Analysis
The significance of differences in recovery of PEGs between IBS patients and healthy subjects before and after NSAID ingestion was evaluated using Mann–Whitney U tests. Proportions of subjects with PEG 10000 recovery before and after NSAID ingestion and between groups were compared using the Chi-square test. Differences in areas under the curves of PEGs before and after NSAID ingestion were determined using a Wilcoxon signed rank test. Potential differences between the results of L/M test in healthy subjects and IBS patients were evaluated by the Chi-square test. Statistical significance was defined as a two-tailed probability <0.05. Statistical analysis was performed with SPSS version 12.0.1 for Windows.
Results
Subjects
The characteristics of the two groups of subjects are listed in Table 1. The mean age of IBS patients was not significantly different from that of healthy subjects. Healthy subjects passed equal volumes of urine in 24 h before and after NSAID consumption (means ± SEM, respectively: 2.06 ± 0.15 L and 2.11 ± 0.14 L). IBS patients passed 2.80 ± 0.32 L urine in 24 h before NSAID consumption, which is significantly more (P = 0.013) than after NSAID consumption (2.10 ± 0.30 L), and more (P = 0.050) than healthy subjects.
PEG Excretion Test in Healthy Subjects (Fig. 2)
The results of the PEG-excretion reproducibility tests 1 and 2 in healthy subjects are presented in Fig. 2. It shows the concentrations of PEGs 400, 1500, and 4000 in urine at the various time points over 24 h. PEG 10000 could be detected in one healthy subject only and therefore data from PEG 10000 are not included in this figure. Urinary concentrations of PEGs 400, 1500, and 4000 after NSAID consumption are also presented in Fig. 2.
Concentrations of PEGs 400 (a), 1500 (b), and 4000 (c) in urine of 15 healthy subjects, in mg/mL, at various times after consumption of PEGs. Test 1 (□) and 2 (■) were performed with a 1-week interval. One week later, the test was performed after 2-days consumption of NSAID (∆). Values represent means ± SEM
Excretion of PEGs 400 and 1500 was essentially complete within 12 h, and excretion of PEG 4000 after 24 h, independent of NSAID consumption. Peak concentrations of PEGs 400 and 1500 were reached within 2 h and the peak concentration of PEG 4000 after 4 h, reflecting a relatively reduced rate of intestinal permeation by the larger compound.
The areas under the concentration curves from tests 1 and 2 were identical (median (range), respectively: PEG 400: 13.3 (7.8–51.8) versus 13.8 (3.8–32.5); PEG 1500: 0.26 (0.08–1.52) versus 0.25 (0.04–0.60); PEG 4000: 0.013 (0.001–0.087) versus 0.012 (0–0.052) mg h mL−1). Figure 2 clearly illustrates that similar concentrations of PEGs 400, 1500, and 4000 were found in tests 1 and 2, indicating reliable reproducibility of test procedures and analysis. The means of data from tests 1 and 2 were used to represent data from healthy subjects before NSAID treatment.
PEG Excretion in Healthy Subjects After NSAID Ingestion
The 24-h recoveries of PEGs 400 and 1500 as percentages of the ingested doses were not different before or after NSAID consumption in healthy subjects (Table 2). Likewise, the 24-h recovery of PEG 4000 was not significantly different after NSAID intake, suggesting that intestinal permeability was not affected by 2 days of NSAID ingestion (Table 2). However, the area under the curve of PEG 4000 after NSAID (0.019, range 0.002–0.100 mg h mL−1, Fig. 2) was significantly (P = 0.050) enhanced compared to before NSAID ingestion (mean of test 1 and 2), which might be interpreted to indicate increased intestinal permeability after NSAID. The peak urinary excretion of PEG 4000 after NSAID ingestion was reached within 2 h after administration and the concentration of PEG 4000 at 2 h was significantly (P = 0.002) higher after than before NSAID intake, which is indicative of accelerated excretion of PEG 4000.
PEG Excretion in IBS Patients (Fig. 3)
Figure 3 shows the recovery of PEGs 400, 1500, and 4000 in mg in the urine from IBS patients before and after NSAID ingestion. PEG 10000 was detected in a limited number of subjects only and is therefore not included in this figure. Excretion of PEGs 400 and 1500 before and after NSAID ingestion, and of PEG 4000 before NSAID ingestion were essentially complete within 12 h. After NSAID intake, complete excretion of PEG 4000 took 24 h. Peak excretion of PEGs 400, 1500, and 4000 were reached within 2 h, and peak excretion of PEG 4000 after 4 h, independent of NSAID ingestion.
IBS patients passed significantly more urine in 24 h before than after NSAID consumption. Urinary flow and volume will contribute to PEG excretion. However, the rate-limiting step in permeability will be the passage of the intestinal mucosal barrier. Therefore, urinary recovery of PEGs will be mostly an indicator of passage of PEGs through the mucosal barrier. By expressing recovery as a percentage of the administered quantity (Table 2) or as mg per 24 h (Fig. 3), differences in urine volumes will have been accounted for.
PEG Excretion After NSAID Ingestion in IBS Patients
Table 2 shows that 24 h recoveries of PEGs 400, 1500, and 4000 in IBS patients after NSAID ingestion were not different from before NSAID intake suggesting that 2 days NSAID consumption did not enhance intestinal permeability in IBS patients. However, the areas under the recovery curves of PEGs 400, 1500, and 4000 in Fig. 3 are significantly larger after NSAID ingestion than before NSAID (median (range): PEG 400: 1,862 (1,266–2,314) versus 2,162 (921–3,988), P = 0.012; PEG 1500: 23.7 (13.1–67.3) versus 36.7 (8.11–203.5), P = 0.041; PEG 4000: 0 (0–0.564) versus 1.65 (0–23.7), P = 0.012, [mg h]), which again might be interpreted to indicate increased intestinal permeability after NSAID. Both Figs. 2 and 3 show that time-dependent registration of PEG excretion provides additional information on possible differences in intestinal permeability.
PEG Excretion in IBS Patients and Healthy Subjects
There were no significant differences in percentages recovered from the administered doses of PEGs 400, 1500, and 4000 between IBS patients and healthy subjects (Table 2), which indicates that intestinal permeability in IBS patients is not different from that in healthy subjects.
L/M Excretion in Healthy Subjects and IBS Patients
The median L/M-ratio from IBS patients was 0.013 (range: 0.005–0.040), which was similar to that from healthy subjects (0.011; range: 0.008–0.030). Both median L/M-ratios are below the cut-off value of 0.03 indicative for enhanced intestinal permeability; three IBS patients had L/M-ratios above 0.03.
I-FABP
I-FABP results showed no differences between healthy subjects and IBS-patients neither before (mean (range) respectively: 3.4 (0–34) versus 6.6 (0–48) pg/mL) nor after NSAID consumption (respectively: 9.1 (0–55) versus 3.9 (0–38) pg/mL), indicating absence of (micro) damage to the intestinal epithelium affecting intestinal permeability as a result of IBS or NSAID consumption.
Discussion
Reports on intestinal permeability in patients with IBS have been contradictory and can be subject to debate [4, 5, 8–10]. Marshall et al. found no significant difference in permeability between IBS patients and healthy subjects based on lactulose mannitol excretion using the conventional cut-off point of 0.03 [5]. However, when a cut-off value of 0.02 was used, an increase in intestinal permeability reached statistical significance [5]. According to these authors, lowering the threshold might open the possibility to distinguishing more subtle disorders like post-infectious IBS. Other studies have shown an increase in intestinal permeability when comparing IBS patients to healthy subjects [4, 8]. Using 51Cr-EDTA as a permeability marker, Dunlop et al. found increased intestinal permeability in post-infectious and diarrhea-predominant IBS patients, but only in the proximal small intestine and not in constipation-predominant IBS patients [8]. Spiller et al. reported increased intestinal permeability based on lactulose mannitol recovery in patients following Campylobacter enteritis [4]. These patients were studied acutely after contracting gastroenteritis and 8–48 months following the initial episode of enteritis. The Walkerton study showed that approximately 2 years after acute gastroenteritis intestinal permeability can be within normal limits [5]. On the other hand, using the L/M test, Lundin et al. reported decreased permeability in the proximal gastrointestinal tract of IBS patients without any relation to the predominant bowel habit of these patients [11]. The question remains whether results from studies on post-infectious IBS patients may be extrapolated to the IBS patient in general.
We hypothesized that the use of NSAIDs by IBS patients sustains a condition of low-grade inflammation mediated by increased intestinal permeability. We have not assessed mucosal inflammation from, e.g., the shedding of faecal calprotectin [34, 35]. Instead, we measured that IFABP shedding from the villous tips, which was not enhanced after 2 days of NSAIDs, indicating that an increase in intestinal permeability was caused by a compromised mucosal barrier function and not by (micro) damage to the mucosal epithelium.
Enhanced intestinal permeability in post-infectious IBS patients may reflect a lack of recovery of tight junction function that had become compromised during acute infection [36, 37]. Mast cells are key players in maintaining intestinal permeability integrity and may play a role in this lack of recovery [38–40]. The number of mast cells that infiltrate inflamed tissue is increased in large intestinal mucosa of IBS patients [3, 41–43]. Also, tryptase activity is enhanced in IBS mucosa [3, 41–43]. Tryptase activates PAR-2, which affects the tight junctions and increases intestinal permeability [44]. However, the effect of infection on permeability can not be generalized since acute infections with Giardia lamblia and rotavirus cause a decrease in intestinal permeability of PEG 400 [45]. It is clear that the pathophysiology of altered intestinal permeability in IBS patients in general remains to be clarified.
Intestinal permeability reflects the barrier function of gut mucosa. Disorders of the barrier function may be assessed from changes in permeability markers. In the present approach, intestinal permeability in IBS patients and sensitivity to factors affecting intestinal permeability were studied by (1) using a polyethylene glycol test mixture containing PEGs from Mr 400 to Mr 10000, (2) monitoring time-dependent urinary excretion of the various PEGs, and (3) testing the effect of 2 days of NSAID administration. Test and analytical procedures showed excellent reproducibility upon repeating the study in healthy subjects (Fig. 2).
The concomitant administration of a combination of markers is regarded as a useful technique to avoid interference from variances in gastric emptying and intestinal transit (premucosal factors) or urinary excretion (postmucosal factor) since, in those cases, excretion of the various markers should be equally affected. Therefore, the time-dependently increased intestinal permeability for PEG 4000 after the 2 days of ingestion of NSAID in healthy subjects and in particular in IBS patients should be ascribed to NSAID-induced changes in mucosal factors such as putative changes in tight junctions or an altered composition of the mucous surface layer [17.] NSAIDs can reduce the surface hydrophobicity of the gastrointestinal mucosal barrier facilitating exogenous water-dissolved agents to permeate the mucous barrier and damage the underlying epithelium [46, 47]. NSAIDs also intracellularly uncouple mitochondrial oxidative phosphorylation, which will contribute to disruption of the integrity of the tight junctions [48, 49].
Our results show the added value of time-dependent registration of PEG excretion. Total 24-h recoveries of PEGs 400, 1500, and 4000 did not show differences between healthy subjects and IBS patients, neither before nor after 2 days of NSAID ingestion (Table 2). Time-dependent monitoring of PEG excretion showed that NSAIDs enhanced intestinal permeability for PEG 4000 in healthy subjects, and for PEGs 400, 1500, and 4000 in IBS patients (Figs. 2 and 3). The time-dependent results also indicate that a 10–12 h period to collect urine would be sufficient to get a valid indication of the extent of PEG recovery, and therefore intestinal permeability.
In conclusion, the important result from this study is that intestinal permeability in IBS patients was found not to be different from that in healthy subjects. Yet, the capacity of the intestinal barrier to cope with luminal aggression is more limited in IBS. Time-dependent monitoring of PEG excretion showed that 2 days administration of NSAIDs enhanced intestinal permeability for PEG 4000 in healthy subjects, and for PEGs 400, 1500, and 4000 in IBS patients. Therefore, NSAIDs compromise intestinal permeability to a greater extent in IBS patients than in healthy subjects. Since intestinal permeability reflects the functional status of the intestinal barrier, the present findings support the idea that IBS is associated with as yet unknown changes in the physiology of the intestinal barrier, particularly expressed when triggered by action of noxious agents.
References
Mayer EA, Collins SM. Evolving pathophysiologic models of functional gastrointestinal disorders. Gastroenterology. 2002;122(7):2032–2048. doi:10.1053/gast.2002.33584.
Rodriguez LA, Ruigomez A. Increased risk of irritable bowel syndrome after bacterial gastroenteritis: cohort study. BMJ. 1999;318(7183):565–566.
Barbara G, Stanghellini V, De Giorgio R, et al. Activated mast cells in proximity to colonic nerves correlate with abdominal pain in irritable bowel syndrome. Gastroenterology. 2004;126(3):693–702. doi:10.1053/j.gastro.2003.11.055.
Spiller RC, Jenkins D, Thornley JP, et al. Increased rectal mucosal enteroendocrine cells, T lymphocytes, and increased gut permeability following acute Campylobacter enteritis and in post-dysenteric irritable bowel syndrome. Gut. 2000;47(6):804–811. doi:10.1136/gut.47.6.804.
Marshall JK, Thabane M, Garg AX, Clark W, Meddings J, Collins SM. Intestinal permeability in patients with irritable bowel syndrome after a waterborne outbreak of acute gastroenteritis in Walkerton, Ontario. Aliment Pharmacol Ther. 2004;20(11–12):1317–1322. doi:10.1111/j.1365-2036.2004.02284.x.
Parry S, Forgacs I. Intestinal infection and irritable bowel syndrome. Eur J Gastroenterol Hepatol. 2005;17(1):5–9. doi:10.1097/00042737-200501000-00002.
Minocha A, Johnson WD, Abell TL, Wigington WC. Prevalence, sociodemography, and quality of life of older versus younger patients with irritable bowel syndrome: a population-based study. Dig Dis Sci. 2006;51(3):446–453. doi:10.1007/s10620-006-3153-8.
Dunlop SP, Hebden J, Campbell E, et al. Abnormal intestinal permeability in subgroups of diarrhea-predominant irritable bowel syndromes. Am J Gastroenterol. 2006;101(6):1288–1294. doi:10.1111/j.1572-0241.2006.00672.x.
Tibble JA, Sigthorsson G, Foster R, Forgacs I, Bjarnason I. Use of surrogate markers of inflammation and Rome criteria to distinguish organic from nonorganic intestinal disease. Gastroenterology. 2002;123(2):450–460. doi:10.1053/gast.2002.34755.
Di L V, D’Inca R, Diaz-Granado N, et al. Lactulose/mannitol test has high efficacy for excluding organic causes of chronic diarrhea. Am J Gastroenterol. 2003;98(10):2245–2252.
Lundin P, Lofgren L, Agerforz P, Abrahamsson H, Simren M. Intestinal permeability in IBS patients and healthy subjects. Scand J Gastroenterol. 2006;41:42. doi:10.1080/00365520510023945.
Locke GR III, Zinsmeister AR, Talley NJ, Fett SL, Melton LJ. Risk factors for irritable bowel syndrome: role of analgesics and food sensitivities. Am J Gastroenterol. 2000;95(1):157–165. doi:10.1111/j.1572-0241.2000.01678.x.
Kalantar JS, Locke GR III, Talley NJ, Zinsmeister AR, Fett SL, Melton LJ III. Is irritable bowel syndrome more likely to be persistent in those with relatives who suffer from gastrointestinal symptoms? A population-based study at three time points. Aliment Pharmacol Ther. 2003;17(11):1389–1397. doi:10.1046/j.1365-2036.2003.01591.x.
Talley NJ, Spiller R. Irritable bowel syndrome: a little understood organic bowel disease? Lancet. 2002;360(9332):555–564. doi:10.1016/S0140-6736(02)09712-X.
Holtmann G, Gschossmann J, Buenger L, Gerken G, Talley NJ. Do changes in visceral sensory function determine the development of dyspepsia during treatment with aspirin? Gastroenterology. 2002;123(5):1451–1458. doi:10.1053/gast.2002.36556.
Brunsden AM, Grundy D. Sensitization of visceral afferents to bradykinin in rat jejunum in vitro. J Physiol. 1999;521(Pt 2):517–527. doi:10.1111/j.1469-7793.1999.00517.x.
Bjarnason I, Williams P, Smethurst P, Peters TJ, Levi AJ. Effect of non-steroidal anti-inflammatory drugs and prostaglandins on the permeability of the human small intestine. Gut. 1986;27(11):1292–1297. doi:10.1136/gut.27.11.1292.
Bjarnason I, Hayllar J, MacPherson AJ, Russell AS. Side effects of nonsteroidal anti-inflammatory drugs on the small and large intestine in humans. Gastroenterology. 1993;104(6):1832–1847.
Barbara G, De Giorgio R, Stanghellini V, Cremon C, Corinaldesi R. A role for inflammation in irritable bowel syndrome? Gut. 2002;51(Suppl 1):i41–i44. doi:10.1136/gut.51.suppl_1.i41.
Smecuol E, Bai JC, Sugai E, et al. Acute gastrointestinal permeability responses to different non-steroidal anti-inflammatory drugs. Gut. 2001;49(5):650–655. doi:10.1136/gut.49.5.650.
Bjarnason I, MacPherson A, Hollander D. Intestinal permeability: an overview. Gastroenterology. 1995;108(5):1566–1581. doi:10.1016/0016-5085(95)90708-4.
Parlesak A, Bode JC, Bode C. Parallel determination of gut permeability in man with M(r) 400, M(r) 1500, M(r) 4000 and M(r) 10000 polyethylene glycol. Eur J Clin Chem Clin Biochem. 1994;32(11):813–820.
Parlesak A, Schafer C, Schutz T, Bode JC, Bode C. Increased intestinal permeability to macromolecules and endotoxemia in patients with chronic alcohol abuse in different stages of alcohol-induced liver disease. J Hepatol. 2000;32(5):742–747. doi:10.1016/S0168-8278(00)80242-1.
Goldman RC, Leive L. Heterogeneity of antigenic-side-chain length in lipopolysaccharide from Escherichia coli 0111 and Salmonella typhimurium LT2. Eur J Biochem. 1980;107(1):145–153. doi:10.1111/j.1432-1033.1980.tb04635.x.
Kanda T, Fujii H, Tani T, et al. Intestinal fatty acid-binding protein is a useful diagnostic marker for mesenteric infarction in humans. Gastroenterology. 1996;110(2):339–343. doi:10.1053/gast.1996.v110.pm8566578.
Kanda T, Fujii H, Fujita M, Sakai Y, Ono T, Hatakeyama K. Intestinal fatty acid binding protein is available for diagnosis of intestinal ischaemia: immunochemical analysis of two patients with ischaemic intestinal diseases. Gut. 1995;36(5):788–791. doi:10.1136/gut.36.5.788.
Kanda T, Nakatomi Y, Ishikawa H, et al. Intestinal fatty acid-binding protein as a sensitive marker of intestinal ischemia. Dig Dis Sci. 1992;37(9):1362–1367. doi:10.1007/BF01296004.
Thompson WG, Longstreth GF, Drossman DA, Heaton KW, Irvine EJ, Muller-Lissner SA. Functional bowel disorders and functional abdominal pain. Gut. 1999;45(Suppl 2):II43–II47.
Uil JJ, van Elburg RM, van Overbeek FM, Mulder CJ, VanBerge-Henegouwen GP, Heymans HS. Clinical implications of the sugar absorption test: intestinal permeability test to assess mucosal barrier function. Scand J Gastroenterol Suppl. 1997;223:70–78.
Rissler K. Improved separation of polyethylene glycols widely differing in molecular weight range by reversed-phase high performance liquid chromatography and evaporative light scattering detection. Chromatographia. 1999;49(11–12):615–620. doi:10.1007/BF02466902.
Megoulas NC, Koupparis MA. Twenty years of evaporative light scattering detection. Crit Rev Anal Chem.. 2005;35:301–316. doi:10.1080/10408340500431306.
Duerksen DR, Wilhelm-Boyles C, Parry DM. Intestinal permeability in long-term follow-up of patients with celiac disease on a gluten-free diet. Dig Dis Sci. 2005;50(4):785–790. doi:10.1007/s10620-005-2574-0.
Pearson AD, Eastham EJ, Laker MF, Craft AW, Nelson R. Intestinal permeability in children with Crohn’s disease and coeliac disease. Br Med J (Clin Res Ed). 1982;285(6334):20–21.
Shah AA, Thjodleifsson B, Murray FE, et al. Selective inhibition of COX-2 in humans is associated with less gastrointestinal injury: a comparison of nimesulide and naproxen. Gut. 2001;48(3):339–346. doi:10.1136/gut.48.3.339.
Berni Canani R, Terrin G, Rapacciuolo L, et al. Faecal calprotectin as reliable non-invasive marker to assess the severity of mucosal inflammation in children with inflammatory bowel disease. Dig Liver Dis. 2008;40(7):533–547. doi:10.1016/j.dld.2008.01.017.
Berkes J, Viswanathan VK, Savkovic SD, Hecht G. Intestinal epithelial responses to enteric pathogens: effects on the tight junction barrier, ion transport, and inflammation. Gut. 2003;52(3):439–451. doi:10.1136/gut.52.3.439.
Serrander R, Magnusson KE, Kihlstrom E, Sundqvist T. Acute Yersinia infections in man increase intestinal permeability for low-molecular weight polyethylene glycols (PEG 400). Scand J Infect Dis. 1986;18(5):409–413. doi:10.3109/00365548609032356.
Santos J, Yang PC, Söderholm JD, Benjamin M, Perdue MH. Role of mast cells in chronic stress-induced colonic epithelial barrier dysfunction in the rat. Gut. 2001;48(5):630–636. doi:10.1136/gut.48.5.630.
Söderholm JD, Yang PC, Ceponis P, et al. Chronic stress induces mast cell-dependent bacterial adherence and initiates mucosal inflammation in rat intestine. Gastroenterology. 2002;123(4):1099–1108. doi:10.1053/gast.2002.36019.
McDermott JR, Bartram RE, Knight PA, Miller HR, Garrod DR, Grencis RK. Mast cells disrupt epithelial barrier function during enteric nematode infection. Proc Natl Acad Sci USA. 2003;100(13):7761–7766. doi:10.1073/pnas.1231488100.
O’Sullivan M, Clayton N, Breslin NP, et al. Increased mast cells in the irritable bowel syndrome. Neurogastroenterol Motil. 2000;12(5):449–457. doi:10.1046/j.1365-2982.2000.00221.x.
Weston AP, Biddle WL, Bhatia PS, Miner P B Jr. Terminal ileal mucosal mast cells in irritable bowel syndrome. Dig Dis Sci. 1993;38(9):1590–1595. doi:10.1007/BF01303164.
Dunlop SP, Jenkins D, Spiller RC. Distinctive clinical, psychological, and histological features of postinfective irritable bowel syndrome. Am J Gastroenterol. 2003;98(7):1578–1583. doi:10.1111/j.1572-0241.2003.07542.x.
Jacob C, Yang PC, Darmoul D, et al. Mast cell tryptase controls paracellular permeability of the intestine. Role of protease-activated receptor 2 and beta-arrestins. J Biol Chem. 2005;280(36):31936–31948. doi:10.1074/jbc.M506338200.
Serrander R, Magnusson KE, Sundqvist T. Acute infections with Giardia lamblia and rotavirus decrease intestinal permeability to low-molecular weight polyethylene glycols (PEG 400). Scand J Infect Dis. 1984;16(4):339–344.
Krugliak P, Hollander D, Le K, Ma T, Dadufalza VD, Katz KD. Regulation of polyethylene glycol 400 intestinal permeability by endogenous and exogenous prostanoids. Influence of non-steroidal anti-inflammatory drugs. Gut. 1990;31(4):417–421. doi:10.1136/gut.31.4.417.
Allen A, Hutton DA, Leonard AJ, Pearson JP, Sellers LA. The role of mucus in the protection of the gastroduodenal mucosa. Scand J Gastroenterol Suppl. 1986;125:71–78. doi:10.3109/00365528609093820.
Somasundaram S, Sigthorsson G, Simpson RJ, et al. Uncoupling of intestinal mitochondrial oxidative phosphorylation and inhibition of cyclooxygenase are required for the development of NSAID-enteropathy in the rat. Aliment Pharmacol Ther. 2000;14(5):639–650. doi:10.1046/j.1365-2036.2000.00723.x.
Bjarnason I, Takeuchi K, Bjarnason A, Adler SN, Teahon K. The G.U.T. of gut. Scand J Gastroenterol. 2004;39(9):807–815. doi:10.1080/00365520410003326.
Acknowledgments
We acknowledge the staff of the Department of Pharmacy of the UMC Utrecht for production and supply of PEG and L/M test solutions. We thank M. van Loon, BSc, R. Voorbij, PhD, and coworkers of the Central Diagnostic Laboratory of the UMC Utrecht for the measurements of lactulose, mannitol, and creatinine. This work was funded in part by a Gastrostart grant from the Netherlands Society of Gastroenterology. APM Kerckhoffs was financially supported by Numico Research BV. LMA Akkermans received financial support from AstraZeneca R&D, Mölndal, Sweden. Supporting institutions were not involved in design, performance, or publication of this study.
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Kerckhoffs, A.P.M., Akkermans, L.M.A., de Smet, M.B.M. et al. Intestinal Permeability in Irritable Bowel Syndrome Patients: Effects of NSAIDs. Dig Dis Sci 55, 716–723 (2010). https://doi.org/10.1007/s10620-009-0765-9
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s10620-009-0765-9