Abstract
Cell encapsulation, a strategy whereby a pool of live cells is entrapped within a semipermeable membrane, represents an evolving branch of biotechnology and regenerative medicine. For example, over the last 20 years, male and female gametes and embryos have been encapsulated with or without somatic cells for different purposes, such as in vitro gametogenesis, embryo culture, cell preservation and semen controlled release. Beside that, cell encapsulation technology in alginate, which is a natural biodegradable polymer that mimics the extracellular matrix and supports both cell functions and metabolism, has been developed with the aim of obtaining three-dimensional (3D) cultures. In this context, adipose-derived stromal vascular fraction (SVF) has attracted more and more attention because of its enormous potential in tissue regeneration. In fact, the SVF represents a rich source of mesenchymal cells (ADSCs), potentially able to differentiate into adipocytes, chondrocytes, osteoblasts, myocytes, cardiomyocytes, hepatocytes, and neuronal, epithelial and endothelial cells. These cells are ideal candidates for use in regenerative medicine, tissue engineering, including gene therapy and cell replacement cancer therapies. As long as technological resources are available for large-scale cell encapsulation intended for advanced therapies (gene therapy, somatic cell therapy and tissue engineering), the state-of-the-art in this field is reviewed in terms of scientific literature.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Adipose tissue has traditionally been considered as a virtually inert tissue, mainly devoted to energy storage. As a consequence, research on the role of adipose tissue in physiology and pathology has been relatively neglected until the discovery of leptin (Zhang et al. 1994) and adiponectin (Scherer et al. 1995); more recently, adipose tissue has been also identified as a source of mesenchymal stem cells (MSCs) able to differentiate into adipocytes, chondrocytes, osteoblasts, myocytes, cardiomyocytes, hepatocytes, and neuronal, epithelial and endothelial cells (Helder et al. 2007; Romanov et al. 2005; Dicker et al. 2005). Adipose tissue is composed of two main populations, mature adipocytes and stromal vascular fraction (SVF): the latest is a heterogeneous population of cell including preadipocytes, endothelial cells, smooth muscle cells, pericytes, macrophage, fibroblasts (Mizuno and Hyakusoku 2003; Fraser et al. 2006; Gomillion and Burg 2006) and adipose MSCs (Romanov et al. 2005; Dicker et al. 2005; Fraser et al. 2006; Rydèn et al. 2003; Rodriguez et al. 2004, 2005; Nakagami et al. 2006; Strem et al. 2005; Musina et al. 2006; Guilak et al. 2006; Mitchell et al. 2006) that share many characteristics of bone marrow MSCs.
Because such tissue is considered as an important, easily, available source of mesenchymal stem cells (ADSCs) for use in regenerative medicine, three-dimensional systems have been developed during last decades in order to promote their culture, expansion and co-culture with target cell-lines.
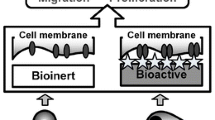
In fact traditional methods of cell growth and manipulation on two-dimensional (2D) surfaces have been revealed insufficient for the new challenges in cell biology, biochemistry, and even in pharmaceutical assays. That is the reason why advances in materials chemistry, fabrication, processing technologies and developmental biology have led to design of the above-mentioned 3D cell culture matrices which better represent the geometry, chemistry, and signalling environment of natural extra cellular matrix (ECM) than 2D cultures. In fact such matrices or scaffolds are porous substrates that can support cell growth, organization, and differentiation on or within their structure. The unique compositional and structural combination supplies appropriate biophysical and biochemical functions, such as facilitating the transport of soluble signaling molecules, nutrients, and metabolic wastes and providing mechanical integrity by absorbing compressive and tensile stresses (Liu and Chen 2007). Moreover the ECM structure can guide morphological changes and cellular organization (Bissell et al. 2003), and specific signalling molecules on the ECM itself can direct cell differentiation into a particular lineage (Lukashev and Werb 1998). Beside that cells can also respond to their local environment, they can remodel local ECM by degrading or synthesizing new ECM elements (Even-Ram and Yamada 2005). Because of the particular application of 3D implantable matrix, only a few biodegradable polymers are suitable (Martina and Hutmacher 2007): materials should be biodegradable and metabolized in the body without causing serious systemic or immunogenic problems (Griffith and Naughton 2002; Muschler et al. 2004).
In parallel to the development of advanced materials and process engineering, 3D matrix formation and fabrication techniques have evolved considerably to manufacture more elaborated 3D structures with a broad range of biomaterials. The earliest is the encapsulation of cells within a hydrogel matrix: in this culture system, a hydrated nano-scale fibrous structure similar to natural ECM surrounds cells completely. In order to produce this 3D system hydrogel precursor solution is mixed with a cell suspension and then quickly gelled using random or self-assembling polymerization via changes of physical or chemical conditions (Uludag et al. 2000). The unique advantage of this technique is that cell culture is performed within a 3D environment that completely surrounds cells, enabling the delivery of intense signals to cells from all directions.
The pioneering paper published in 1964 by Chang describe that artificial microcapsules of comparable dimensions and properties could be made simply and in large numbers, and that enzymes and other proteins loaded into such particles were able to retain useful biological activity in vitro and in vivo. After more than four decades, numerous microencapsulation procedures are still developed according to Chang’s original idea that is a procedure which consists in the generation of a controlled-size droplet followed by the process of stabilizing the interface and creating a membrane around a core. The breakthrough in applying Chang’s principles of bioencapsulation came then: in this case alginate, that is a natural, anionic and biocompatible polymer, was employed for the first time (Lim and Sun 1980). Shortly after such encapsulation technique was adopted for pancreatic islets and for bovine spermatozoa (Goosen et al. 1985; Nebel et al. 1985, 1993, 1996). Starting from these works, the applications of cell encapsulation in biotechnologies have been expanded to other fields with different aim: this review will be focussed on germ cell lineage and adipose derived SVF for cartilage regeneration.
Alginate-based cell encapsulation
Alginates are a family of unbranched anionic polysaccharides derived from brown algae (Phaeophyta) which occur extracellularly and intracellularly at approximately 20% to 40% of the dry weight. The 1,4-linked α-l-guluronate (G) and β-d-mannuronate (M) are arranged in homopolymeric (GGG blocks and MMM blocks) or heteropolymeric block structures (MGM blocks). Cell walls of brown algae also contain 5% to 20% of fucoidan, a branched polysaccharide sulphate ester with l-fucose four-sulfate blocks as the major component. Guluronate blocks selectively bind divalent cations that induce chain-chain association and constitute the junction zones of the so-called “egg box model” (Draget et al. 2001; Braccini and Pérez 2001). Commercial alginates are often extracted from algae washed ashore, and their properties depend on the harvesting and extraction processes.
Alginate has been employed for encapsulating cells to be transplanted, since it is biocompatible both with host and with enclosed cells; moreover, its quality can be constantly ensured. Rough surfaces of capsules must also be avoided because they can elicit immunological reactions when implanted: these devices in fact are supposed to protect the entrapped cell/tissue fragments against the components of the host immune system, while simultaneously permitting the unhindered passage of nutrients, oxygen and secreted therapeutics factors. Furthermore, mechanical strength and elasticity of these pharmaceutical forms should be high enough to guarantee consistent therapy over prolonged periods, and their manufacturing process must not only be reproducible but also meet the demands for medical approval (Lee et al. 2008).
Alginate capsules in mammal reproduction
Spermatozoa encapsulation for controlled release and preservation
Artificial insemination (AI) techniques are processes that involve the collection of semen, its preservation and transfer to the fertilization site. These practices are widely diffused in both in animal and human fields, but several difficulties are still to be overcome. For example, in order to favour sperm preservation, a suitable extender assuring energy supply for spermatozoa and counteracting metabolic process related acidosis, should be employed. In fact, because seminal plasma contains membrane-stabilizing agents and capacitation-preventing molecules (Maxwell and Johnson 1999; Johnson et al. 2000), its removal or dilution leads to membrane destabilization, capacitation and precocious acrosomal reaction. Moreover, the antioxidant system connected with plasma-cell factor interactions can be unpaired (Maxwell and Johnson 1999). Further difficulties in AI practices depend on female reproductive physiology and that is the reason why different strategies have been proposed to improve such procedure. For example, controlled release delivery systems by sperm encapsulation were developed in the veterinary field (Nebel et al. 1985, 1993, 1996): in this case high sperm concentrations could be maintained in bovine uterus during the ovulation, thus guaranteeing an increase in fertility and prolificacy. The encapsulation procedure implicated three steps, that is, the production of a calcium alginate cell-containing matrix, the formation of a semipermeable membrane by interfacial polymerization with a multivalent polyamine, and the semisolid matrix liquefaction by chelation of calcium with sodium citrate. The use of a biocompatible polymer as alginate leads to the maintenance of optimal cell viability levels both in vivo and in vitro and, besides that, the resulting capsule membrane is permeable to small molecules as, glucose and oxygen, but impermeable to large molecules, such as immunoglobulins (Lim and Sun 1980). Moreover, such capsules could protect male gametes from uterine macrophage phagocytosis and promote the bioadhesion to endometrium, thus preventing semen reflux (Nebel et al. 1985, 1993, 1996; Munkittrick et al. 1992). In 1999, Conte et al. proposed a one-step reverse technique for encapsulating swine spermatozoa in barium alginate (Conte et al. 1999): in this case barium chloride was added to the semen and the resulting suspension dropped into a sodium alginate solution. In this way barium ions contained into the ejaculate diffuse out of the droplets and, once reach the interface, react with the alginate chains, leading to the formation of a barium alginate gel membrane around the semen droplet.
Such a method presented two fundamental advantages: firstly, the obtained capsules consisted of a core of undiluted spermatozoa, surrounded by a polymeric membrane which separate the cells from the extender (Munoz-Garay et al. 2001; Torre et al. 2000) and, secondly, barium ions were employed as gelling agent in lieu of calcium, thus avoiding the promotion of precocious capacitation processes (Munoz-Garay et al. 2001). This technique was successfully applied even in other species, as for example Equidae and humans (Vigo et al. 2005, b). It was also demonstrated by Herrler et al. (2006) that human semen-containing alginate microcapsules can be cryopreserved, yielding a decreased motility compared to standard protocols, but with a higher vitality of the immotile spermatozoa. This technique could then be useful when small amounts of spermatozoa collected by microsurgical epididymal sperm aspiration, testicular sperm extraction, or from cryptozoospermic men should be preserved in several small samples feasible for a possible intracytoplasmatic sperm injection.
Germ cell lineage encapsulation for in vitro maturation
During recent decades, several attempts have been made to design oocyte in vitro maturation and/or in vitro fertilization culture systems. These culture methods are generally based on protein and growth factor-enriched media with the purpose of replacing the biological milieu for the isolated ova, but nowadays alternative oocyte maturation systems have been conceived. This is the case of the 3D approach for cumulus/oocyte complexes co-culture in alginate matrix, a culture system which considers both that oocytes are surrounded by a cellular environment (e.g. granulosa cell cumulus) with a well-defined extracellular matrix, and that in vivo cells present a three-dimensional (3D) organization (Pangas et al. 2003). Another culture system is based on barium alginate capsules able to mimic basal membrane. According to this approach an oocyte and a pool of granulosa cells are enclosed in a fluid core and, once in the core, the granulosa cells organize themselves into a pseudofollicular structure, morphologically resembling a mature Graafian follicle, and thus creating a milieu capable of inducing oocyte maturation without exogenous hormones (Vigo et al. 2006; Vigo et al. 2005a, b; Torre et al. 2007). Beside that scanning electron microscopy and the analysis of progesterone/oestradiol synthesis performed on bovine/porcine models showed that the barium alginate co-culture maintains a better environmental condition for granulosa cells with delayed luteinization phenomena when compared with a monolayer culture (Vigo et al. 2005a, b). The membrane-core model has also been applied to human oocytes, obtaining better results in terms of maturation yield when compared to routine methods like microdrop oocyte culture (90.3% vs. 52%, respectively after 48 h of culture) (Torre et al. 2006). In conclusion, fluid core alginate capsules should be considered as an alternative method for facilitating conceptus development as long as this technology is able to permit a better self-organization of the cellular systems.
Adipose stromal vascular fraction encapsulation for cartilage regeneration
During last years cell encapsulation has emerged as a promising regenerative therapeutic strategy to treat a wide range of diseases. In this context alginate capsules represent an interesting innovation in culture and co-culture systems. The major advantage of such technology is that cells are not entrapped in the gel but suspended in the most suitable medium, as well as in a natural or artificial ECM. Moreover, the inner surface of capsule membrane can promote cell anchorage through pseudo-basal membrane simulation (Vigo et al. 2005a, b, 2006; Torre et al. 2006, 2007; Benzoni et al. 2005).
The optimisation process of such encapsulation technology depends on several critical issues, such as the careful selection of the cell line, the controlled manufacture of capsules and the suitable adaptation of the construct design to the selected cell line. Because adipose tissue represents an important, easily ADSCs, during the last decades researchers have focused their attention on the isolation of adipose SVF as an ideal candidate for use in regenerative medicine and in tissue engineering.
Adult ADSCs represent a promising therapeutic source for treating degenerative and post-traumatic pathologies like bone-marrow neurological lesions or intervertebral disc (IVD) diseases, for curing subjects affected by atrium-ventricular block and, finally, for regenerating damaged epithelium or cartilage hit by traumas or burns. For example adipose tissue has been used in plastic surgery for a long term in order to correct body defects related to age, traumas or pathological conditions that alter patient appearance (i.e. wrinkle-filling or scar removing) (Ellenborgen 2000; Patrick 2000, 2001; De Ugarte et al. 2003; Casteilla et al. 2004; Coleman 2004; Barrilleux et al. 2006). During the last decades many authors have confirmed the advantages of lipoaspirate transplant: in fact they have noticed consistent improvement of both skin structure and tissue turgidity near treated zones (Von Heimburg et al. 2001; Andrè 2002; Matsumoto et al. 2006). Moreover, it was clearly demonstrated that such lipoinnests are able to promote neovascularization inside epithelial tissue (Rigotti et al. 2007; Klinger et al. 2008) and it was also hypothesized that such tissue regeneration could be related to the presence of mesenchymal stem cells within transplanted adipose tissue (Mizuno and Hyakusoku 2003; Brzoska et al. 2005; Tholpady et al. 2006; Torre 2007).
ADSCs regenerative therapy has also been implied for the treatment of IVD diseases (O’Halloran and Pandit 2007; Gaetani et al. 2008; Helder et al. 2007; Li et al. 2005; Richardson et al. 2006): in fact, chondrocytes could be retrieved, expanded in a 3D in vitro system consisting of alginate capsules, and finally re-implanted through a mini-invasive technique. Moreover it is now possible to regenerate or replace damaged IVDs through the implants of biodegradable scaffolds seeded with autologous ADSCs previously induced to differentiate to the chondrogenic phenotype (Helder et al. 2007).
In this context three-dimensional adipose tissue-derived cell culture in alginate capsules seems to be a promising technique to allow for optimal cell expansion, following GMP guidelines (Villani et al. 2008). Moreover, in rabbits, the adipose tissue-derived cells co-cultured with Nucleus Polposus (NP) cells showed a significant increase in the expression of type II collagen and aggrecan genes, suggesting that ADSCs might respond to mediators contained in the IVD (Li et al. 2005). The barium alginate encapsulation technique applied by Gaetani et al. (2008) showed that ADSCs improve the quality of in vitro reconstructed NP tissue for the regeneration of the human degenerated IVD. The results suggest that 3D co-culture of NP cells and non-adipocyte cell fraction improves the quality of the in vitro reconstructed tissue in terms of the extracellular matrix production and cell organization. Therefore this represents a realistic and innovative approach in regenerative cell therapy for the IVD disease.
Conclusion and future directions
Three dimensional scaffolds represent important steps in the development of biomedical engineering, which has already generated much success but is also associated with substantial new challenges. The next trend in 3D cell culture should involve escaping from a largely empirical approach to a more systematic methodology. This requires developing advance 3D-matrix fabrication techniques coupled with biomaterial engineering. Although current production techniques are valuable within a limited range of resolutions, future fabrication methods must interlace multiple-scale structures with exceptional controllability. Chemistry and engineered functionalities of biomaterials also need to be controlled further for an enhanced systematic approach; this can also be accomplished using the hybridization of manufacturing techniques and materials. For example cell-entrapping alginate capsules represent an excellent cell culture system that allows both expansion and differentiation of interested cell lines. In fact it is supposed to maintain cell viability, to promote cell polarization and abundant extra-cellular matrix release, and, finally, to guarantee homogeneous cell distribution.
A variety of cell types can be enclosed in alginate, maintaining their morphology: fibroblasts and chondrocytes adhere to the polymer, proliferate and express genes of extracellular matrix components; hepatocytes secrete albumin, and cardiomyocytes, bone marrow cells and Schwann cells present normal cell functions. Adult stem cells are more accessible, and there are no ethical dilemmas for their use. At present the routine use of adult stem cells is limited to the treatment of haematological disorders, but they are also being used in clinical trials for therapy of several diseases. Because of SVF importance in regenerative medicine and its enormous potential and plasticity, these cells can be cultured in alginate capsules for expansion purposes and co-cultured for differentiation objectives.
Future research must focus on the development of a technically advanced capsule technology to satisfy the demands of the GMP-guide lines for large scale transplantation. This ambitious goal requires the interdisciplinary and integrated effort of scientists with different areas of expertise such as physico-chemistry, biology and medicine.
References
Andrè P (2002) Facial lipoatrophy secondary to a new synthetic filler device (Profill) treated by lipofilling. J Cosmet Dermatol 1:59–61. doi:10.1046/j.1473-2165.2002.00044.x
Barrilleux B, Phinney DG, Prockop DJ, O’Connor K (2006) Review: ex-vivo engineering of living tissues with adult stem cells. Tissue Eng 12:3007–3019. doi:10.1089/ten.2006.12.3007
Benzoni E, Torre ML, Faustini M, Stacchezzini S, Cremonesi F, Conte U, Villani S, Russo V, Ricevuti G, Vigo D (2005) Transient transfection of porcine granulosa cells after 3D culture in barium alginate capsules. Int J Immunopathol Pharmacol 18:677–682
Bissell MJ, Rizki A, Mian IS (2003) Tissue architecture: the ultimate regulator of breast epithelial function. Curr Opin Cell Biol 15:753–762. doi:10.1016/j.ceb.2003.10.016
Braccini I, Pérez S (2001) Molecular basis of C(2+)-induced gelation in alginates and pectins: the egg-box model revisited. Biomacromolecules 2:1089–1096. doi:10.1021/bm010008g
Brzoska M, Geiger H, Gauer S, Baer P (2005) Epithelial differentiation of human adipose tissue-derived adult stem cells. Biochem Biophys Res Commun 330:142–150. doi:10.1016/j.bbrc.2005.02.141
Casteilla L, Charrière G, Laharrague P, Cousin B, Planat-Benard V, Pèricaud L, Chavoin JP (2004) Adipose tissue, plastic and reconstructive surgery: come back to sources. Ann Chir Plast Esthet 49:409–418. doi:10.1016/j.anplas.2004.08.001
Chang TMS (1964) Semipermeable microcapslules. Science 146:524–525. doi:10.1126/science.146.3643.524
Coleman SR (2004) Rèinjection de graisse autologue ou lipofilling ou Lipostructure®. Ann Chir Plast Esthet 49:456–458. doi:10.1016/j.anplas.2004.09.005
Conte U, Torre ML, Maggi L, Giunchedi P, Vigo D, Maffeo G, Russo V (1999) EP0922451
De Ugarte DA, Ashjian PH, Elbarbary A, Hedrick MH (2003) Future of fat as raw material for tissue regeneration. Ann Plast Surg 50:215–219. doi:10.1097/01.SAP.0000029661.38066.15
Dicker A, LeBlanc K, Åstrom G, van Harmelen V, Götherström C, Blomqvist L, Arner P, Rydén M (2005) Functional studies of mesenchymal stem cells derived from adult human adipose tissue. Exp Cell Res 308:283–290. doi:10.1016/j.yexcr.2005.04.029
Draget KI, Gaserod O, Aune I (2001) Effects of molecular weight and elastic segment flexibility on syneresis in Ca alginate gels. Food Hydrocoll 15:485–490. doi:10.1016/S0268-005X(01)00046-7
Ellenborgen R (2000) Fat transfer: current use in practise. Cinical Plast Surg 27:545–546
Even-Ram S, Yamada KM (2005) Cell migration in 3D matrix. Curr Opin Cell Biol 17:524–532. doi:10.1016/j.ceb.2005.08.015
Fraser JK, Wulur I, Alfonso Z, Hedrick MH (2006) Fat tissue an underappreciated source of stem cells for biotechnology. Trends Biotechnol 24:150–154. doi:10.1016/j.tibtech.2006.01.010
Gaetani P, Torre ML, Klinger M, Faustini M, Crovato F, Bucco M, Marazzi M, Chlapanidas T, Levi D, Tancioni F, Vigo D, Rodriguez y Baena R (2008) Adipose-derived stem cell therapy for intervertebral disc regeneration: an in vitro reconstructed tissue in alginate capsules. Tissue Eng Part A 141:415–423
Gomillion CT, Burg K (2006) Stem cells and adipose tissue engineering. Biomaterials 27:6052–6605. doi:10.1016/j.biomaterials.2006.07.033
Goosen MF, O’Shea GM, Gharapetian HM, Chou S, Sun AM (1985) Optimization of microencapsulation parameters: Semipermeable microcapsules as a bioartificial pancreas. Biotechnol Bioeng 27(2):146–150. doi:10.1002/bit.260270207
Griffith LG, Naughton G (2002) Tissue engineering—current challenges and expanding opportunities. Science 295:1009–1014. doi:10.1126/science.1069210
Guilak F, Lott KE, Awad HA, Cao Q, Hicok KC, Fermor B, Gimble JM (2006) Clonal analysis of the differentiation potential of human adipose-derived adult stem cells. J Cell Physiol 206:229–237. doi:10.1002/jcp.20463
Helder MN, Knippenberg M, Klein-Nulend J, Wuisman PI (2007) Stem cells from adipose tissue allow challenging new concepts for regenerative medicine. Tissue Eng 13:1799–1808. doi:10.1089/ten.2006.0165
Herrler A, Eisner S, Bach V, Weissenborn U, Beier HM (2006) Cryopreservation of spermatozoa in alginic acid capsules. Fertil Steril 85:208–213. doi:10.1016/j.fertnstert.2005.06.049
Johnson LA, Weitze KF, Fiser P, Mawxell WMC (2000) Storage of boar semen. Anim Reprod Sci 62:143–172. doi:10.1016/S0378-4320(00)00157-3
Klinger M, Marazzi M, Vigo D, Torre ML (2008) Fat injection in severe burn outcomes: a new perspective of scar remodelling and reduction. Aesthetic Plast Surg 32:465–469. doi:10.1007/s00266-008-9122-1
Lee J, Cuddihy MJ, Kotov NA (2008) Three-dimensional cell culture matrices: state of the art. Tissue Eng Part B 1:61–86. doi:10.1089/teb.2007.0150
Li X, Lee JP, Balian G, Anderson DG (2005) Modulation of chondrocytic properties of fat-derived mesenchymal cells in co-cultures with nucleus pulposus. Connect Tissue Res 46:75–82. doi:10.1080/03008200590954104
Lim F, Sun AM (1980) Microencapsulated islets as bioartificial endocrine pancreas. Science 210:908–910. doi:10.1126/science.6776628
Liu WF, Chen CS (2007) Cellular and multicellular form and function. Adv Drug Deliv Rev 59:1319–1328. doi:10.1016/j.addr.2007.08.011
Lukashev ME, Werb Z (1998) ECM signalling: orchestrating cell behaviour and misbehaviour. Trends Cell Biol 8:437–441. doi:10.1016/S0962-8924(98)01362-2
Martina M, Hutmacher DW (2007) Biodegradable polymers applied in tissue engineering research: a review. Polym Int 56:145–151. doi:10.1002/pi.2108
Matsumoto D, Sato K, Gonda K, Takaki Y, Shigeura T, Sato T, Aiba-Kojima E, Iizura F, Keita I, Suga H, Yoshimura K (2006) Cell-assisted lipotransfer: supportive use of human adipose-derived cells for soft tissue augmentation with lipoinjection. Tissue Eng 12:3375–3381. doi:10.1089/ten.2006.12.3375
Maxwell WMC, Johnson LA (1999) Physiology of spermatozoa at high dilution rates: the influence of seminal plasma. Theriogenology 52:1353–1362. doi:10.1016/S0093-691X(99)00222-8
Mitchell JB, McIntosh K, Zvonic S, Garrett S, Floyd ZE, Kloster A, Di Halvorsen Y, Storms RW, Goh B, Kilroy G, Wu X, Gimble JM (2006) Immunophenotype of human adipose-derived cells: temporal changes in stromal-associated and stem cell-associated markers. Stem Cells 24:376–385. doi:10.1634/stemcells.2005-0234
Mizuno H, Hyakusoku H (2003) Mesengenic potential and future clinical perspective of human processed lipoaspirate cells. J Nippon Med Sch 70:300–306. doi:10.1272/jnms.70.300
Munkittrick TW, Nebel RL, Saacke RG (1992) Accessory sperm numbers for cattle inseminated with protamine sulphate microcapsules. J Dairy Sci 75:725–731
Munoz-Garay C, De la Vega-Beltràn JL, Delgado R (2001) Inwardly rectify K+ channels in spermatogenic cells: functional expression and implication in sperm capacitation. Dev Biol 234:261–274. doi:10.1006/dbio.2001.0196
Muschler GF, Nakamoto C, Griffith LG (2004) Engineering principles of clinical cell-based tissue engineering. J Bone Joint Surg Am 86:1541–1558
Musina RA, Bekchanova ES, Belyavskii V (2006) Differentiation potential of mesenchymal stem cells of different origin. Technol Biol Med 2:147–151
Nakagami H, Morishita R, Maeda K, Kikuchi Y, Ogihara T, Kaneda Y (2006) Adipose tissue-derived stromal cells as a novel option for regenerative cell therapy. J Atheroscler Thromb 13:77–81
Nebel RL, Bame JH, Saacke RG, Lim F (1985) Microencapsulation of bovine spermatozoa. J Anim Sci 60(6):1631–1639
Nebel RL, Vishwanath R, McMillan WH, Pitt CJ (1996) Microencapsulation of bovine spermatozoa viability and fertility. Anim Reprod Sci 44:79–89. doi:10.1016/0378-4320(96)01540-0
Nebel RL, Vishwanath R, McMillan WH, Saacke RG (1993) Microencapsulation of bovine spermatozoa for use in artificial insemination: a review. Reprod Fertil Dev 5:701–712. doi:10.1071/RD9930701
O’Halloran D, Pandit AS (2007) Tissue-engineering approach to regenerating the intervertebral disc. Tissue Eng 13:1927–1954. doi:10.1089/ten.2005.0608
Pangas SA, Saudye H, Shea LD, Woodruff TK (2003) Novel approach for the three-dimensional culture of granulose cell-oocyte complexes. Tissue Eng 9:1013–1021. doi:10.1089/107632703322495655
Patrick CW (2000) Adipose tissue engineering: the future of breast and soft tissue reconstruction following tumor resection. Semin Surg Oncol 19:302–311. doi:10.1002/1098-2388(200010/11)19:3<302::AID-SSU12>3.0.CO;2-S
Patrick CW (2001) Tissue engineering strategies for adipose tissue repair. Anat Rec 263:361–366. doi:10.1002/ar.1113
Richardson SM, Walker RV, Parker S, Rhodes NP, Hunt JA, Freemont AJ, Hoyland JA (2006) Intervertebral disc cell-mediated mesenchymal stem cell differentiation. Stem Cells 24:707–716. doi:10.1634/stemcells.2005-0205
Rigotti G, Marchi A, Galiè M, Baroni G, Benati D, Krampera M, Pasini A, Sbarbati A (2007) Clinical treatment of radiotherapy tissue damage by lipoaspirate transplant: a healing process mediated by adipose-derived adult stem cells. Plast Reconstr Surg 119:1409–1422. doi:10.1097/01.prs.0000256047.47909.71
Rodriguez AM, Elabd C, Delteil F, Astier J, Vernochet C, Saint-Marc P, Guesnet J, Guezennec A, Amri EZ, Dani C, Ailhaud G (2004) Adipocyte differentiation of multipotent cells estabilished from human adipose tissue. Biochem Biophys Res Commun 315:255–263. doi:10.1016/j.bbrc.2004.01.053
Rodriguez AM, Elabd C, Amri E, Ailhaud G, Dani C (2005) The human adipose tissue is a source of multipotent stem cells. Biochimie 87:125–128. doi:10.1016/j.biochi.2004.11.007
Romanov A, Darevskaya A, Merzlikina N (2005) Mesenchymal stem cells from human bone marrow and adipose tissue: isolation, characterization, and differentiation potentialities. Cell Technol Biol Med 3:158–163
Rydèn M, Dicker A, Götherström C, Aström G, Tammik C, Arner P, Le Blanc K (2003) Functional characterization of human mesenchymal stem cell-derived adipocytes. Biochem Biophys Res Commun 14:391–397. doi:10.1016/j.bbrc.2003.10.010
Scherer PE, Williams S, Fogliano M, Baldini G, Lodish HF (1995) A novel serum protein similar to C1q, produced exclusively in adipocytes. J Biol Chem 270:26746–26749. doi:10.1074/jbc.270.45.26746
Strem BM, Hicok KC, Zhu M, Wulur I, Alfonso Z, Schreiber RE, Fraser JK, Hedrick MH (2005) Multipotential differentiation of adipose tissue-derived stem cells. Keio J Med 3:132–141. doi:10.2302/kjm.54.132
Tholpady SS, Llull R, Ogle RC, Rubin JP, Futrell JW, Katz AJ (2006) Adipose tissue: stem cell and beyond. Clin Plast Surg 33:55–62. doi:10.1016/j.cps.2005.08.004
Torre ML (2007) Microincapsulazione di cellule staminali da tessuto adiposo per la terapia rigenerativa di tessuti epiteliali. Acta Vulcanol 5:48–50
Torre ML, Maggi L, Vigo D, Galli A, Bornaghi V, Conte U (2000) Controlled release of swine semen encapsulated in calcium alginate beads. Biomaterials 21:1493–1498. doi:10.1016/S0142-9612(00)00035-1
Torre ML, Munari E, Albani E, Levi-Setti PE, Villani S, Faustini M, Conte U, Vigo D (2006) In vitro maturation of human oocytes in a follicle-mimicking three-dimensional coculture. Fertil Steril 86:572–576. doi:10.1016/j.fertnstert.2006.02.090
Torre ML, Faustini M, Klinger M, Vigo D (2007) Cell encapsulation in reproduction. Recent Patents Drug Deliv Formul 1:85
Uludag H, De-Vos P, Tresco PA (2000) Technology of mammalian cell encapsulation. Adv Drug Deliv Rev 42:29–64. doi:10.1016/S0169-409X(00)00053-3
Vigo D, Torre ML, Faustini M, Munari E, Russo V, Conte U (2005a) I. Capsules containing seminal material for artificial insemination. European Application WO2006106400
Vigo D, Villani S, Faustini M, Accorsi PA, Galeati G, Munari E, Russo V, Asti A, Conte U, Torre ML (2005b) A follicle-like model by granulosa cell encapsulation in a barium alginate/protamine membrane. Tissue Eng 11:709–714. doi:10.1089/ten.2005.11.709
Vigo D, Russo V, Faustini M, Stacchezzini S, Conte U, Torre ML, Accorsi PA, Galeati G, Spinaci M (2006) Preparation of three-dimensional mammalian ovarian follicular cells and ovarian follicle culture systems in a biocompatible matrix. European Patent EP1706103
Villani S, Marazzi M, Bucco M, Faustini M, Klinger M, Gaetani P, Crovato F, Vigo D, Caviggioli F, Torre ML (2008) Statistical approach in alginate membrane formulation for cell encapsulation in a GMP-based cell factory. Acta Biomater 4:943–949. doi:10.1016/j.actbio.2008.01.007
Von Heimburg D, Zachariah S, Heschel I, Kuhuling H, Schoof H, Hafemann B, Paulla N (2001) Human preadypocites seeded on freeze-dried collagen scaffold investigated in vitro and in vivo. Biomaterials 22:429–438. doi:10.1016/S0142-9612(00)00186-1
Zhang Y, Proenca R, Maffei M, Barone M, Leopold L, Friedman JM (1994) Positional cloning of the mouse obese gene and its human homologue. Nature 372:425–432. doi:10.1038/372425a0
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Ghidoni, I., Chlapanidas, T., Bucco, M. et al. Alginate cell encapsulation: new advances in reproduction and cartilage regenerative medicine. Cytotechnology 58, 49–56 (2008). https://doi.org/10.1007/s10616-008-9161-0
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s10616-008-9161-0