Abstract
Background
The current pilot study aimed to investigate the benefit of imagery rescripting (IR) as an adjunct to Group Cognitive Behavioural Therapy (GCBT) for SAD, given recent research suggesting that IR is beneficial in the treatment of social anxiety disorder (SAD).
Methods
Fifteen participants with SAD completed eight sessions of GCBT and two additional individual sessions of IR to address negative meanings embedded in memories of traumatic social experiences.
Results
As expected, participants reported significant reductions in fear of negative evaluation and identification of negative core beliefs as valid/accurate over the course of the two session IR intervention. Moreover, IR yielded significant improvements in negative affect and maladaptive appraisals associated with self-imagery and aversive memories, as well as depressive symptoms. However, unexpectedly, IR did not yield significant additive reductions in social anxiety symptoms over and above GCBT.
Discussion
Results indicate that IR appears to be a beneficial adjunct to GCBT, and lack of improvement in social anxiety symptoms across IR sessions may be due to methodological limitations. Outcomes suggest that IR may also benefit patients with comorbid depression, given high rates of comorbid unipolar depression for people with SAD, presenting an exciting area for further investigation.
Conclusions
Taken together, findings suggest that IR may be a valuable adjunct to GCBT for SAD, especially among patients with comorbid unipolar depression. However, further research including a follow up period is indicated.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Social anxiety disorder (SAD) is characterised by a marked and enduring fear of negative evaluation in situations related to public performance, close scrutiny, or social interaction (American Psychiatric Association [APA], 2013; Iza et al., 2014). Individuals with SAD have disproportionate fears that they will humiliate themselves or be rejected by others; and hence, they avoid social situations or endure them with great distress. SAD has an early onset and high prevalence, with 12.1% of the American population experiencing the disorder during their lifetime (Kessler et al., 2005; Stein et al., 2017). The disorder is associated with considerable disability and functional impairment across multiple domains (Hendriks et al., 2014; Ruscio et al., 2008). SAD has a high comorbidity rate, with up to 70% reporting additional mental health diagnoses (Crome et al., 2015; Ruscio et al., 2008). Mood disorders are the most common comorbidities, including Major Depressive Disorder (MDD; 36.5%) and Persistent Depressive Disorder (PDD; 16.8%) (Crome et al., 2015).
Recent research has found that aversive social experiences (e.g., bullying, interpersonal rejection) are a key and proximal cause of the development of SAD, and that appraisal of such socially traumatic experiences mediates the relationship between social anxiety symptoms and key variables that maintain the disorder (i.e., negative beliefs and imagery) (Norton & Abbott, 2016a). These data support cognitive models of SAD (Clark & Wells, 1995; Rapee & Heimberg, 1997), which suggest that past experiences give rise to a pattern of negative self-processing involving negative images and verbal beliefs about the self and the social world. These beliefs include excessively high standards for social performance (e.g., “I must always be entertaining to others”), conditional beliefs (e.g. “If I stammer, they’ll think I’m incompetent”), and unconditional beliefs (e.g., “I’m weird”) (Clark, 2001). Moreover, when beliefs are activated by social situations, they are often coupled with imagery in which individuals see themselves as depicting a grossly distorted and negative appearance (e.g., fire engine red, being pointed and laughed at; shrunk to Lilliputian size and frozen on a stage) (Hackmann et al., 1998). Focus on these biased images appears to increase anxiety, self-focused attention and safety behaviours, thus undermining social performance and increasing the likelihood of both perceived and actual negative feedback, and thereby preventing disconfirmation of social fears (Hirsch et al., ; Ng et al., 2014).
Given the role of negative imagery and beliefs rooted in historically aversive social experiences, recent research has investigated the efficacy of imagery rescripting (IR) for SAD. IR is a collection of transdiagnostic imagery techniques that aim to alter negative meanings and beliefs associated with autobiographical memories of distressing experiences (Holmes et al., 2007). Studies have found that 1–2 sessions of IR significantly reduces social anxiety symptoms, maladaptive beliefs and distress associated with negative imagery and aversive memories (Knutsson et al., 2019; Lee & Kwon, 2013; Nilsson et al., 2012; Norton & Abbott, 2016b; Reimer & Moscovitch, 2015; Romano, Hudd, et al., 2020; Romano, Moscovitch, et al., 2020; Romano, Moscovitch, et al., 2020; Wild et al., 2007, 2008). IR yields symptom reduction equivalent to in vivo exposure and greater than a control condition, as well as producing clinically meaningful change in a short time (Knutsson et al., 2019; Lee & Kwon, 2013; Nilsson et al., 2012; Norton & Abbott, 2016b; Reimer & Moscovitch, 2015; Romano, Moscovitch, et al., 2020). Some studies have included a session of cognitive restructuring prior to IR (e.g., Lee & Kwon, 2013; Wild et al., 2008), some researchers question whether this is necessary, and have found IR to be effective in updating socially traumatic memories as a standalone intervention (e.g., Nilsson et al., 2012; Norton & Abbott, 2016b). Indeed, Norton and Abbott (2016b) found that a single session of IR or cognitive restructuring yielded equivalent reductions in social anxiety symptomatology and state distress related to a speech task.
Effective treatment for SAD has been consistently shown through robust outcomes reported for both individual and group Cognitive Behavioural Therapy (CBT) (Clark et al., 2003, 2006; Rapee et al., 2009). Conventional CBT targets maintaining factors identified in cognitive models of SAD, including negative thoughts and beliefs, avoidance and safety behaviours, and self-focused attention (Clark & Wells, 1995; Rapee & Heimberg, 1997). However, they do not directly address cognitive and affective content linked to previous aversive experiences that appears to be a key maintaining factor in SAD.
Several studies have shown promising evidence for the benefits of IR to existing gold standard treatment for SAD, however no research has investigated the specific additive benefits of IR as an isolated intervention strategy. A number of studies have now integrated IR into group CBT (GCBT) for SAD, among other imagery-based intervention strategies (Ahn & Kwon, 2018; McEvoy & Saulsman, 2014; McEvoy et al., 2015). McEvoy and colleagues (McEvoy & Saulsman, 2014; McEvoy et al., 2015) incorporated a range of imagery-enhanced cognitive behavioural interventions into their GCBT, yielding large effect sizes and superior outcomes to a predominantly verbally-based GCBT program. Additional imagery-enhanced strategies included teaching participants to identify imagery, rather than cognitions, and focussed on imagery-challenging rather than traditional cognitive challenging. Participants were also taught to use coping imagery, and engaged in 1 session of IR. Furthermore, participants were required to listen back on their IR sessions daily, thus increasing exposure to the cognitive and affective content of the IR session. Moreover, Ahn and Kwon (2018a) demonstrated that compared to conventional GCBT, the addition of a number of interventions designed to change negative self-imagery (including IR, repeated video feedback, social mishap exposure training) produced significantly better and faster reductions in social anxiety, fears of negative evaluation, judgement bias, and dysfunctional self-beliefs. Recent research by Romano and colleagues (2020) compared a single session IR to imaginal exposure, and supportive counselling in order to isolate and examine the unique effects of IR upon aversive memories among individuals with SAD. Romano and colleagues (2020) found evidence to support the efficacy of IR in reducing negative memory appraisals, reducing negative self-directed core beliefs, and increasing both neutral and positive memory details. These findings support the potential benefits of IR in the treatment of SAD, as an isolated treatment component targeting negative autobiographical memories. However, there remains a dearth in the literature investigating whether IR, by extension, also reduced a broader range of social anxiety symptoms (e.g., fear of negative evaluation, avoidance). Furthermore, no studies to date have investigated the specific additive effect of IR in their enhanced treatment packages.
Hence, the current pilot study aimed to investigate the benefit of IR as an adjunct to CBT for SAD. Following eight sessions of GCBT, participants completed two additional individual sessions of IR to address negative meanings embedded in memories of traumatic social experiences. It was expected that the IR sessions would yield (1) additive reductions in social anxiety symptomatology over and above GCBT; reduced negative emotions associated with: (2) self-imagery and (3) traumatic memories; and (4) reduced identification of negative beliefs as valid/accurate.
Method
Participants
Participants were 15 (60% female) individuals who met criteria for DSM-5 (APA, 2013) social anxiety disorder (SAD). Participants were recruited via a referral of a health professional that had provided services to the participant and/or a direct referral of the participant. Referred individuals were contacted via telephone or email to provide information about the study and therapy groups and offered the option to participate. Participants were administered the Anxiety Disorders Interview Schedule (ADIS-5, Brown & Barlow, 2014) for DSM-5 (APA, 2013) by either a registered Clinical Psychologist or a postgraduate clinical psychology student.Footnote 1
Participants who met criteria for a principal diagnosis of SAD were included. Exclusion criteria included a primary substance-use disorder, an active psychotic illness, non-English speaking, or less than 16 years of age. Participants assessed with the ADIS-5 demonstrated significant rates of comorbidity, including Major Depressive Disorder (40%), Persistent Depressive Disorder (40%), Generalised Anxiety Disorder (33%), Specific Phobia (27%), Panic Disorder (20%), Obsessive Compulsive Disorder (7%), Body Dysmorphic Disorder (7%) and Agoraphobia (7%). It is noteworthy that 10 of the 13 participants (77%) assessed with the ADIS-5 met criteria for diagnosis of a DSM-5 unipolar Mood Disorder, and no participants met criteria for Post-Traumatic Stress Disorder (PTSD). However, consistent with previous findings (Norton & Abbott, 2016a), many participants reported a history of chronic relational trauma (e.g., emotional abuse or neglect by caregivers in childhood, severe bullying and exclusion by peers).
Symptom Measures
Anxiety Disorders Interview Schedule for DSM-5 (ADIS-5; Brown & Barlow, 2014). All participants were administered the ADIS-5 to confirm DSM-5 diagnosis of SAD, and 13 participants were assessed for comorbidities. The ADIS-5 is a gold standard semi-structured clinical interview based on DSM-5 criteria for assessment of Axis I disorders.
Social Interaction Anxiety Scale and Social Phobia Scale (SIAS and SPS; Mattick & Clarke, 1998)). The SIAS and SPS are companion measures designed to allow for thorough assessment of social fears (Mattick & Clarke, 1998). The SIAS assesses fears of social interaction (cognitive, affective and behavioural symptoms), while the SPS assesses fears of scrutiny by others, respectively (Mattick & Clarke, 1998). Each measure includes 20 items, and respondents indicate the degree to which they feel each statement is characteristic/true of them on a five-point scale ranging from 0 (not at all) to 4 (extremely). A systematic review of the psychometric properties of self-report measures of social anxiety indicated that the SIAS and SPS possesses strong psychometric properties, including responsiveness to clinically important changes as the result of an intervention (Modini et al., 2015). Participants completed the SIAS and SPS at baseline, after completing the CBT group, and after completing two session of imagery rescripting.
Brief Fear of Negative Evaluation Scale (B-FNE; Leary, 1983). The BFNE assesses fears of negative evaluation with 12-items describing fearful or worrying cognitions that are rated on a five-point scale ranging from 1 (not at all characteristic of me) to 5 (very characteristic of me) (Leary, 1983; Weeks et al., 2005). The BFNE demonstrates sound psychometric properties (Weeks et al., 2005). Participants completed the BFNE at baseline, after completing the CBT group, and after completing two session of imagery rescripting.
The Depression Anxiety Stress Scales – Short Form (DASS-21; Lovibond & Lovibond, 1995). The DASS-21 is a 21-item self-report measure that was used to assess severity of depression, anxiety, and stress-related symptoms over the last week. Respondents indicate the degree to which they feel each statement applies to them on a four-point scale ranging from 0 (not at all) to 4 (very much or most of the time). The full DASS-21 was administered to all participants, with interest being primarily in the depression subscale (DASS-D). Participants completed the DASS-21 at baseline after completing the CBT group, and after completing two session of imagery rescripting.
Imagery Interview
To assess participants’ descriptions of imagery experienced in social situations and their associated meanings, all participants completed an imagery interview in their first IR session. This was a semi-structured interview of approximately 30 minutes based on Hackmann et al. (2000) and Moscovitch, Gavric, Merrifield, Bielak, and Moscovitch (2011). The questions were standardised and asked in a fixed order. A detailed protocol of the imagery interview is available from the authors on request.
Participants were provided with brief psychoeducation on the nature of imagery, before guided assessment of negative self-imagery and associated distressing memories. To assess for negative self-imagery, participants were invited to close their eyes and imagine themselves in a highly socially threating situation (e.g., at a party, giving a speech). After dwelling on this imaginary scene, participants were asked whether a mental image or impression tends to come into their mind in such situations. All participants were able to identify a recurrent image and were asked to mentally recreate this image and prompted to describe it in detail (e.g., facial, expression, body language, physical sensations, associated emotions). To identify any distressing memories associated with the recurrent image, participants were asked to identify their first recollection of feeling the way they do in the image. Participants were then asked to describe any memories they identified as linked to the imagery.
Core Beliefs Module of the Waterloo Images and Memories Interview (WIMI; Reimer & Moscovitch, 2015 ).
The Core Beliefs Module of the WIMI was included as a standardised, semi-structured means of assessing core beliefs embedded or encapsulated in the memories identified in the imagery interview. Initially, participants are asked to identify any automatic thoughts that they experience along with their image. Prompts are provided as necessary, for example, When you experience this image, is there often a particular kind of thought that pops into your head along with it? Is there something you are thinking in the image? What are you thinking to yourself while…? Automatic thoughts reported by the participant are used to identify core beliefs encapsulated by the memory. The downward arrow technique is used to explore beneath the automatic thought, by asking such questions as: If that thought were true, what would it mean about/to you? This thread is followed to see if a core belief can be identified and then repeated for any additional thought/belief domains. If the participant does not identify spontaneous thoughts/beliefs, they are asked to directly reflect on the content of the memory to identify what it means to them or about them. As participants had already identified some core beliefs during the CBT group program, some participants were immediately able to identify core beliefs contained in their memories, and did not require these additional steps to access encapsulated core beliefs.
Imagery Ratings. Participants were asked to make a number of ratings regarding their negative self-image before the first IR session and after the second IR session. All ratings were made on a 5-point scale from 1 (not at all) to 5 (extremely), and included the degree to which emotions associated with the image were (1) positive, (2) negative and (3) intense, as well as the degree to which they felt (4) embarrassed/ashamed and (5) pleased/proud of the image.
Memory Ratings (Reimer & Moscovitch, 2015). Participants were asked to make a number of ratings regarding their distressing memory before the first IR session and after the second IR session. All ratings were made on a 5-point scale from 1 (not at all) to 5 (extremely), and included the degree to which emotions associated with the event were (1) positive, (2) negative and (3) intense, as well as the degree to which they felt (4) embarrassed/ashamed and (5) pleased/proud of the event.
Core Belief Ratings (Reimer & Moscovitch, 2015). For each core belief identified (up to three), participants were asked to rate the degree to which they believed the belief was (1) valid and (2) an accurate reflection of the way things “really are”. Ratings were made on a 5-point scale from 1 (not at all) to 5 (extremely). These two items were summed for each core belief to form an overall rating of degree of belief. As participants identified different numbers of core beliefs (between one and three), ratings were averaged for each participant to form a mean rating of degree of belief at each time point. Participants rated their core beliefs prior to the first rescripting session and after the second rescripting session.
Group Cognitive Behavioural Therapy Intervention (8 weekly sessions, 3 h per session).
Prior to the IR sessions, participants engaged in Group Cognitive Behaviour Therapy (GCBT) based on treatment protocols developed by Rapee and colleagues for GCBT (Rapee et al., 2009) and Clark and colleagues for individual CBT for SAD (e.g., Clark et al., 2003, 2006; Mörtberg, Clark, Sundin, & Åberg Wistedt, 2007; Stangier et al., 2003). The treatment targeted maintaining factors identified in cognitive models of SAD, including negative thoughts and beliefs, avoidance and safety behaviours, and self-focused attention (Clark & Wells, 1995; Rapee & Heimberg, 1997). Sessions were approximately 3 hours, conducted weekly over 8 weeks by a Clinical Psychologist experienced in cognitive-behavioural treatment of SAD and postgraduate clinical psychology interns. The groups comprised 7 or 8 members, and across the two groups included in the study, 53.5% agreed to participate in the additional IR sessions. Average attendance was 7.13 sessions (89%).
Session 1 involved psychoeducation about the nature of social anxiety, introduction to the cognitive model of SAD, setting up a rationale for the treatment components, and exploring ambivalence and obstacles to change. Session 2 focused on cognitive restructuring, while session 3 introduced behavioural experiments and included a group behavioural experiment. Session 4 aimed to help participants gain an accurate perception of how they appear to others via video feedback on a speech task. Session 5 focused on attention training to shift self-focused attention to the social situation. Session 6 introduced core beliefs and challenging of dysfunctional assumptions that maintain core beliefs, while session 7 focused on challenging core beliefs. Session 8 involved review, relapse prevention, and forward planning for ongoing goals.
Imagery Rescripting Intervention (2 sessions, 45–60 min each).
The IR intervention was administered across two sessions (Lee & Kwon, 2013) as previous research has demonstrated that while a single session is beneficial for symptom reduction, it is insufficient for full symptom alleviation (Norton & Abbott, 2016b). Rescripting was based on distressing memories identified in the imagery interview. Where multiple memories were identified, the most salient memory was chosen, based on consultation with the participant. Depending on the level of satisfaction with the rescript in the first session, the second session sometimes involved a repetition of the same memory, or a different memory with similar themes and encapsulated meaning. Each IR session followed the published protocol laid out by Wild and Clark (2011), and used in previous studies of IR for SAD (e.g., Norton & Abbott, 2016b; Wild et al., 2007). Sessions were conducted by the first author, a Clinical Psychologist with training and experience in imagery rescripting, or masters level clinical psychology interns under the supervision of the first author. A detailed protocol of the imagery rescripting procedure utilised in the present study is available from the authors on request.
The intervention included psychoeducation to provide a rationale for IR, followed by stages two and three of the three stages initially outlined by Arntz and Weertman (1999). Stage 1 of the procedure described by Arntz and Weertman (1999) (reliving the memory as it happened at the time) has been argued to be unnecessary or even counterproductive for the purpose of changing embedded meaning (e.g., Arntz, 2014), hence was excluded from this protocol. In the first phase of rescripting, participants were instructed to recount the memory from the perspective of the younger self as it happened until they reached the moment of peak distress, at which point they were asked to shift perspective to view the scene from the perspective of their current adult self. Participants were then invited to intervene to alter the course of events however they chose until the outcome was more positive or satisfying. In the second phase, participants were invited to relive the event from the perspective of their younger self, but incorporating the new content from phase one. Finally, the younger self was asked what else (s)he needed in order to feel better (e.g., nurturing, compassion, play), and any expressed desires were incorporated into the imagery. The procedure concluded with safe place imagery if required by the participant (Nilsson et al., 2012; Norton & Abbott, 2016b).
At times when the participant struggled to intervene in the first phase, commonly used variations to the IR procedure were used, as described by Arntz and Weertman (1999). These included (1) the participant using helpers to intervene (e.g., police, parent, teacher), (2) the therapist assisting the participant in the imagery, and (3) the therapist actively participating and directing the intervention.
Participants had completed cognitive restructuring interventions in the context of the CBT group, including challenging negative thoughts and core beliefs. Hence, no explicit cognitive restructuring was included in the IR sessions, as per several previous studies (e.g., Nilsson et al., 2012; Norton & Abbott, 2016a, 2016b; Reimer & Moscovitch, 2015). However, core beliefs identified in the CBT group were often also linked to distressing memories that were the focus of the IR sessions.
Procedure
Participants completed the ADIS-5 interview and baseline measures (SIAS, SPS, BFNE, DASS-21), followed by eight weeks of the GCBT intervention. Trait measures (SIAS, SPS, BFNE, DASS-21) were recompleted at the end of the group, prior to the IR sessions. In the final two sessions of the group, participants were offered the opportunity for two additional individual IR sessions with one of the group facilitators. Analyses suggest that there was no self-selection bias between those who elected to complete the IR sessions (n = 15) compared to those who did not (n = 10). A series of one-way ANOVAs demonstrated no significant differences in mean age or on key symptom measures before or after GCBT (ADIS severity, DASS-D, SIAS + SPS, BFNE) between those who selected to complete the IR sessions compared to those who did not, all p’s > 0.06. Moreover, no significant difference was evident in gender distribution, χ2(1) = 0.96, p = 0.33, between those who did and did not complete the IR sessions.
Those who chose to participate in these sessions completed them at the conclusion of the group, one week apart. The first IR session was approximately 1.5 hours, and included the Imagery Interview, Core Beliefs Module of the WIMI, completion of imagery, memory, and core belief ratings, as well as the first imagery rescript. The second session was approximately one hour, and included the second imagery rescript, as well as recompletion of imagery, memory, and core belief ratings. Finally, participants again completed trait measures (SIAS, SPS, BFNE, DASS-21). The University of Sydney Human Ethics Research Committee (HREC) approved all aspects of this research (reference number 2015/365).
Statistical Analyses
Statistical analyses were conducted using Statistical Package for the Social Sciences (SPSS) software 27.0 for Windows. The level of significance was set at α = .05 for all statistical analyses. The SIAS and SPS were summed to form a composite as they were developed as companion measures, assessing different aspects of social anxiety (Mattick & Clarke, 1998). Repeated measures ANOVAs were conducted for relevant symptom variables (SIAS, SPS, BFNE, DASS-D) across three time points: (1) Pre-GCBT, (2) Post-GCBT, and (3) Post-IR sessions. Follow up paired sample t-tests were conducted to assess the nature of changes over time. Bonferroni α rate corrections were used for the post-hoc comparison tests following ANOVAs, which were conducted for (1) before and after GCBT and (2) before and after IR (i.e., adjusted α = .05/2 = .025). Paired sample t-tests were also conducted on state variables (imagery ratings, memory ratings and core belief ratings) to assess changes pre and post IR sessions on these variables.
Results
Demographic Measures
The mean age of participants was 23.7 years (SD = 4.89, Range = 18–25 years). Participants were 60% female, all identified as never married and not having children. The majority of participants (69.2%) reported a secondary school qualification as their highest level of education attainment and their employment status as part-time (40%).
Symptom Measures
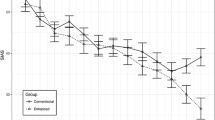
Social anxiety symptom composite (SIAS + SPS). There was a significant linear reduction in social anxiety symptoms across the three time points, F(1,14) = 12.86, p < 0.01. Follow up t-tests indicated that social interaction anxiety significantly reduced following GCBT, Mdiff = 22.16, t(14) = 4.33, p < 0.01, d = 1.06, but not the IR sessions, Mdiff = 0.78, t(14) = 0.26, p = 0.79, d = 0.07 (see Fig. 1). On examination of individual participant outcomes, 27% were no longer in the clinical range on the social anxiety symptom composite at post-IR (Peters, 2000), and 60% achieved a decrease their composite score of between 10- and 72-points from pre-GCBT to post-IR.
BFNE. There was a significant linear reduction in fears of negative evaluation across the three time points, F(1,13) = 6.35, p = 0.02. Follow up t-tests indicated that fears of negative evaluation did not significantly reduce following GCBT, Mdiff = 3.00, t(13) = 1.44, p = 0.17, d = 0.40, but did significantly reduce following the IR sessions, Mdiff = 3.21, t(13) = 0.2.56, p = 0.02, d = 0.67. On examination of individual participant outcomes, 47% achieved a decrease of between 7- and 26-points on the BFNE from pre-GCBT to post-IR.
DASS-D. There was a significant linear reduction in depression symptoms across the three time points, F(1,14) = 15.53, p < 0.01. Follow up t-tests indicated that depression symptoms significantly reduced during GCBT, Mdiff = 5.60, t(14) = 3.07, p < 0.01, d = 0.75, with further significant reductions following the IR sessions, Mdiff = 3.87, t(14) = 3.01, p < 0.01, d = 0.76 (see Fig. 1). On examination of individual participant outcomes, 53% reported depression symptoms in the Normal/Mild at post-IR (Lovibond & Lovibond, 1995), and 60% achieved a decrease their DASS-D score of between 8- and 26-points from pre-GCBT to post-IR Table 1.
State Measures
Imagery Ratings. From before the first IR session to after the second IR session, repeated measures t-tests demonstrated a significant reduction in negative emotions associated with the self-image, Mdiff = 0.73, t(14) = 2.32, p = 0.04, d = 0.72, and an increase in feeling pleased/proud of the image, Mdiff = 0.73, t(14) = -2.96, p = 0.01, d = 1.39. There were no significant changes in self-reported positive emotions, emotional intensity or embarrassment/shame associated with the image, all p’s > 0.07. Means and standard deviations are in Table 2.
Memory Ratings. From before the first IR session to after the second IR session, paired samples t-tests demonstrated a significant reduction in the emotional intensity of the negative memory, Mdiff = 0.67, t(14) = 2.32, p = 0.04, d = 0.56, as well as negative emotions, Mdiff = 1.2, t(14) = 3.85, p < 0.01, d = 1.17, and embarrassment/shame associated with the memory, Mdiff = 1.53, t(14) = 5.28, p < 0.01, d = 2.21 (negative emotions and shame are presented in Fig. 2). Participants also reported more positive emotions, Mdiff = 0.87, t(14) = -2.98, p = 0.01, d = 1.19, and feeling more being pleased/proud about the negative memory after the second IR session compared to before the first IR session, Mdiff = 1.27, t(14) = -0.383, p < 0.01, d = 3.13. Means and standard deviations are in Table 2.
Core Belief Ratings. From before the first IR session to after the second IR session, a repeated measures t-test demonstrated a significant reduction in the degree to which participants identified their core beliefs as valid/accurate, Mdiff = 1.93, t(14) = 4.88, p < 0.01, d = 2.04 (see Fig. 2). Means and standard deviations are in Table 2.
Description of Core Beliefs. On average participants identified 2.4 (SD = 0.74) core beliefs. All core beliefs were unconditional, and most (88%) were self-related (e.g., I’m useless, I’m worthless, I’m a failure, I will end up alone). The remaining 12% were other-related unconditional beliefs (e.g. The world is chaotic and unjust, I can’t trust others to take care of me).
Discussion
Study findings are considered in light of key methodological limitations. Specifically, that causal inferences cannot be drawn in the absence of a control condition as significant effects may be due to the passage of time rather than to the IR intervention. Nonetheless, outcomes of the current study provide preliminary support for the inclusion of IR as a beneficial adjunct to GCBT. As anticipated, participants reported significant reductions in negative emotions and appraisals associated with self-imagery and traumatic memories, as well as reduced identification of negative core beliefs as valid/accurate as a result of the two session IR intervention. Moreover, fears of negative evaluation significantly reduced during IR, but did not significantly reduce over the course of GCBT. However, contrary to expectations, IR did not yield significant additive reductions in social anxiety symptoms over and above GCBT.
Significant reductions in self-reported social anxiety symptoms (as measured by the SIAS and SPS) over the course of conventional GCBT are consistent with previous studies (e.g., Rapee et al., 2009). While effect sizes for these symptom improvements were large, SIAS and SPS scores remained in the clinical range (Peters, 2000). Unexpectedly, participants reported negligible further improvement in social anxiety symptoms on the SIAS and SPS following the IR sessions. This outcome does not appear to result from a lack of power to detect the effect (as reductions were < 1 point), nor does this seem to be a floor effect as the majority participants continued to report symptoms in the clinical range. Indeed, our data supports the need for a larger dose of therapy for symptoms to move out of the clinical range, and that two sessions of IR may be insufficient.
This finding is especially surprising as participants reported significant reductions in fears of negative evaluation, identification with core beliefs, and negative affect connected to their self-imagery and aversive memory over the course of the IR sessions. Indeed, social anxiety related cognitions (i.e., fears of negative evaluation) did not change significantly over the course of the group program, but significantly reduced during the IR sessions, with the effect size indicating a small to medium change. Further, participants reported significant reductions in the degree to which they identified their core beliefs as accurate/valid with a large effect size from pre to post IR. These cognitive variables are considered key maintaining factors in SAD (Clark & Wells, 1995), which typically predict symptom change (e.g., Rapee & Abbott, 2007).
Furthermore, negative self-imagery and associated aversive memories are also key processes that maintain social anxiety (see Ng & Abbott, 2014 and Ng, Abbott, & Hunt, 2014b for reviews), which significantly improved across the IR sessions. Following IR, participants reported that their self-imagery impacted them less negatively and they felt greater pride in relation to their revised self-image. Moreover, participant reports suggest that following IR, their aversive memories were less emotionally intense, they experienced less negative affect and more positive affect related to their memory, and that they felt less shame and more pride connected to the memory. Reductions in social anxiety symptoms would be expected in the context of these improvements in the cognitive appraisal and affective experience of self-imagery and associated memories, consistent with previous studies of IR for SAD (e.g., Nilsson et al., 2012; Reimer & Moscovitch, 2015; Wild et al., 2008).
Of particular note is the significant reduction in shame associated with the aversive memory. Shame is described as an intensely painful emotion in which the individual experiences themselves as defective and thus undeserving of acceptance or belonging (Brown, 2006; Tangney et al., 2007). Shame states are consistently correlated with social anxiety (e.g., Fergus et al., 2010; Gilbert, 2000; Hedman, Ström, Stünkel, & Mörtberg, 2013; Matos et al., 2013), and preliminary evidence suggest that shame-based schemata rooted in aversive childhood experiences may predict social anxiety symptomatology (Shahar et al., 2015). Shame is a common but notoriously difficult emotion to ameliorate in therapy, and is often resistant to verbal-cognitive intervention (Dearing et al., 2011). However, a number of studies have demonstrated that imagery rescripting is effective in reducing shame states (e.g., Grunert et al., 2007). Hence the benefits of IR for reducing shame in social anxiety is worthy of further investigation (see Norton & Abbott, 2017 for discussion of SAD as a shame-based disorder).
We propose that the discrepancy between outcomes on social anxiety processes (verbal cognitive, imaginal and affective) and symptom measures described above is due to a methodological limitation. Specifically, the final measure of social anxiety symptoms (SIAS and SPS) was assessed immediately following the second imagery rescripting session rather than at a follow up time. The SIAS and SPS focus on behaviours and experiences in social situations (e.g., SIAS: “I have difficulty talking to other people”, “I am tense mixing in a group”; SPS: “I can feel conspicuous standing in a line”, “When in an elevator, I’m tense if people look at me”) which participants were asked to rate “over the last week”. Hence, it is plausible that the observed changes in social anxiety processes had insufficient opportunity to impact situational behaviours and experiences at the point they were assessed. Thus, we would expect to find reductions in social anxiety symptoms with follow up to allow behavioural change to take place. This hypothesis is supported by other social anxiety treatment protocols that integrate IR and demonstrate improvements in social anxiety at follow up (e.g., Ahn & Kwon, 2018a; McEvoy et al., 2015). However, the specific effect of IR on social anxiety symptoms at long term follow up remains to be empirically assessed, highlighting the need for further research.
It is noteworthy that mood (DASS-D) improved over the course of the group and further improved during the IR sessions, with effect sizes in the moderate to large range. While depressed mood was not a direct target of the group, self-reported depression scores reduced from the severe to moderate range during this intervention, and almost into the mild range following IR (Lovibond & Lovibond, 1995). These outcomes suggest that improvement in social anxiety symptoms during the group may have flow on effects to improving mood, and/or that GCBT and IR may target mechanisms that are common social anxiety and low mood.
The trajectory of depression scores are of particular interest because depression is commonly comorbid with SAD (Kessler et al., 1999), as was the case for the majority of the present sample. SAD typically temporally precedes onset of depressive disorders, suggesting that SAD is a significant risk factor for developing depression (Grant et al., 2007; Kessler et al., 1999; Starr et al., 2005). Indeed, Ohayon and Schatzberg (2010) found that the odds of developing MDD were more than five times greater among individuals with SAD. Moreover, SAD patients who are also depressed tend to have poorer treatment outcomes, with SAD patients with comorbid depression reporting higher social anxiety symptoms following GCBT compared to those without a mood disorder (Fracalanza et al., 2014; Lemoult et al., 2014).
Starr and colleagues (2005) outline a number of shared factors that may underlie SAD and depression, including cognitive, behavioural and interpersonal factors. Common underlying self-related schemata (i.e., negative beliefs about self-worth and competence) and cognitive biases are found in both SAD and depression (Dozois & Frewen, 2006; Wilson & Rapee, 2005), along with a ruminative cognitive style (Drost et al., 2014). In addition, avoidance of social contexts is a hallmark of SAD, which reduces positively reinforcing interpersonal experiences and connections, as well as quality of life, thereby increasing the likelihood of developing depressive symptoms (Ottenbreit et al., 2014). Furthermore, peer rejection and victimisation has been associated with the development of both social anxiety and depressive symptoms (La Greca & Harrison, 2005), and intrusive imagery associated with autobiographical memories is common to both disorders (Hackmann et al., 2000; Kuyken & Howell, 2006).
Findings of the current study that IR significantly reduced depression symptoms are consistent with evidence that IR addresses the negative beliefs and experiences that drive depression (Wheatley & Hackmann, 2011). It is plausible that challenging toxic meanings (core beliefs) embedded in aversive social memories, and the associated positive shift in the sense of self (Çili & Stopa, 2015; Moscovitch, 2009; Romano, Hudd, et al., 2020), would also function to improve mood. Furthermore, pilot data suggests that IR may be beneficial in the treatment of depressed patients with intrusive memories (Brewin et al., 2009; Wheatley et al., 2009). Given the frequent comorbidity of SAD and depressive disorders, the addition of IR in GCBT for SAD may be beneficial for reducing comorbid depression symptoms, improving outcomes for those with both disorders, and preventing onset of depression among SAD patients. These possibilities are deserving of further investigation.
Despite these valuable findings, a number of limitations of the current study must be noted, which provide direction for future research. This was a pilot study with a relatively small (N = 15) sample size of young people, and a larger sample size is required to assess the clinical significance of these outcomes. However, the sample size was sufficient to detect a medium effect size (α = 0.05, power = 0.8, required n = 9; Faul et al., 2007) as evidenced by significant reductions in BFNE and DASS-D scores following IR, equating to medium to large effect sizes. Nonetheless, in order to detect smaller effects resulting from IR a larger sample size may have been required (α = 0.05, power = 0.8, required n = 42; Faul et al., 2007). This may be particularly the case for the symptom composite in the present study (SIAS + SPS). While it is possible that the symptom composite was not administered at the most appropriate time point, it also remains possible that IR following GCBT only produces a significant (albeit small effect) in reducing symptom severity. While prior research comparing IR to a control condition has demonstrated large effect sizes in symptom reduction (e.g., Norton & Abbott, 2016b), this may not be the case for additive effects of IR following GCBT. Therefore, it remains for future research to assess whether symptom severity shows the same pattern of reductions following IR as did BFNE and DASS-D scores in the present study when administered at a more appropriate time point and with a larger sample size. Moreover, the relatively young age range of participants (18–25 years) limits the generalisability of findings, hence requires replication with a more mature demographic.
In addition, the study did not include a control condition. Thus, further studies are needed utilising larger sample sizes and a randomised, controlled design. Indeed, one recent study investigating the unique mechanisms targeted by IR for SAD has incorporated control conditions, by introducing two control conditions, consisting of imaginal exposure (IE) and supportive counselling (SC) (Romano, Moscovitch, et al., 2020). Results found strong evidence to support the efficacy of IR to address negative memories present in SAD. Future research would benefit by adopting a control condition to assess whether significant effects are simply due to the passing of time, or to this specific intervention. Moreover, imagery, memory and core belief variables were only assessed at post-GCBT and post-IR, so could not be tracked from the pre-GCBT baseline. Crucially, final measures were given immediately following the final IR session, rather than at a follow up point when some time would have elapsed for behavioural changes to occur. We hypothesise that reductions in social anxiety symptoms would occur at follow up, and this will be an important question for future investigation. For example, Romano and colleagues (2020), investigated the unique mechanisms of IR upon aversive memories among individual with SAD when compared to imaginal exposure or supportive counselling, assessed memory outcomes (memory details, intrusiveness and vividness) as well as core beliefs at 1 week, 2 weeks, and 3 months post-intervention. Future research would benefit from assessing social anxiety symptoms through the use of reliable and valid measures (e.g., SPS, SIAS, BFNE) at similar follow up time points.
Finally, the current study suggests that IR holds promise in the treatment of depression, both as a primary disorder and when comorbid with SAD. To date, preliminary studies support the use of IR for depression (Brewin et al., 2009; Wheatley & Hackmann, 2011), and further investigation is warranted.
In sum, the current study provides preliminary information about the additive effects of a brief IR intervention on key symptom and process outcomes in individuals with SAD following their participation in a standard course of GCBT. Findings suggest that IR targets important aetiological and maintaining factors in SAD, including fear of negative evaluation and core beliefs, as well as negative affect and negative appraisals associated with self-imagery and aversive memories. Importantly, the ability of IR to reduce negative memory appraisals and associated core beliefs, has been supported by recent investigations, strengthening further the likely benefits of IR as an effective intervention component for SAD (Romano et al., 2020). Crucial methodological changes are necessary (i.e. a follow up period) to assess whether these shifts produce improvements in social anxiety symptoms. Finally, findings suggest that a brief IR intervention administered after standard GCBT may further reduce symptoms of depression in patients with SAD. Indeed, the utility of IR for patients with a primary depressive disorder remains an exciting area for future investigation.
Notes
Two participants were only administered the SAD section of the ADIS-5 rather than the complete interview.
References
Ahn, J. K., & Kwon, J. H. (2018). Modifying negative self-imagery increases the effectiveness of cognitive behavior therapy for social anxiety disorder: a benchmarking study. Cognitive Therapy and Research, 42(5), 598–611. https://doi.org/10.1007/s10608-018-9918-5.
American Psychiatric Association Arlington, VA, US, D.-5 T. F. (Ed.). (2013). Diagnostic and statistical manual of mental disorders: DSM-5. Diagnostic and Statistical Manual of Mental Disorders: DSM-5TM.
Arntz, A. (2014). Imagery Rescripting for Posttraumatic Stress Disorder. In Working with Emotion in Cognitive-Behavioral Therapy (pp. 203–215).
Arntz, A., & Weertman, A. (1999). Treatment of childhood memories: Theory and practice. Behaviour Research and Therapy, 37(8), 715–740. https://doi.org/10.1016/S0005-7967(98)00173-9.
Brewin, C. R., Wheatley, J., Patel, T., Fearon, P., Hackmann, A., Wells, A., Fisher, P., & Myers, S. (2009). Imagery rescripting as a brief stand-alone treatment for depressed patients with intrusive memories. Behaviour Research and Therapy, 47(7), 569–576. https://doi.org/10.1016/j.brat.2009.03.008.
Brown, B. (2006). Shame resilience theory: a grounded theory study on women and shame. Families in Society: The Journal of Contemporary Social Services, 87, 43–52. https://doi.org/10.1606/1044-3894.3483.
Çili, S., & Stopa, L. (2015). Intrusive mental imagery in psychological disorders: Is the self the key to understanding maintenance? Frontiers in Psychiatry, 6, 6–10. https://doi.org/10.3389/fpsyt.2015.00103.
Clark, D. M. (2001). Chapter 18 A Cognitive Perspective on Social Phobia. International Handbook of Social Anxiety: Concepts, Research and Interventions Relating to the Self and Shyness., https://doi.org/https://doi.org/10.11618/6323
Clark, D. M., Ehlers, A., Hackmann, A., McManus, F., Fennell, M., Grey, N., Waddington, L., & Wild, J. (2006). Cognitive therapy versus exposure and applied relaxation in social phobia: A randomized controlled trial. Journal of Consulting and Clinical Psychology, 74(3), 568–578. https://doi.org/10.1037/0022-006X.74.3.568.
Clark, D. M., Ehlers, A., McManus, F., Hackmann, A., Fennell, M., Campbell, H., Flower, T., Davenport, C., & Louis, B. (2003). Cognitive therapy versus fluoxetine in generalized social phobia: a randomized placebo-controlled trial. Journal of Consulting and Clinical Psychology, 71(6), 1058–1067. https://doi.org/10.1037/0022-006X.71.6.1058.
Clark, D. M., & Wells, A. (1995). A cognitive model of social phobia. In Social phobia: Diagnosis, assessment, and treatment. (pp. 69–93). Guilford Press.
Crome, E., Grove, R., Baillie, A. J., Sunderland, M., Teesson, M., & Slade, T. (2015). DSM-IV and DSM-5 social anxiety disorder in the Australian community. Australian and New Zealand Journal of Psychiatry, 49(3), 227–235. https://doi.org/10.1177/0004867414546699.
Dearing, R. L., & Tangney, J. P. (Eds.). (2011). Shame in the therapy hour. . Washington, DC: American Psychological Association.
Dozois, D. J. A., & Frewen, P. A. (2006). Specificity of cognitive structure in depression and social phobia: A comparison of interpersonal and achievement content. Journal of Affective Disorders, 90(2–3), 101–109. https://doi.org/10.1016/j.jad.2005.09.008.
Drost, J., van der Does, W., van Hemert, A. M., Penninx, B. W. J. H., & Spinhoven, P. (2014). Repetitive negative thinking as a transdiagnostic factor in depression and anxiety: A conceptual replication. Behaviour Research and Therapy, 63, 177–183. https://doi.org/10.1016/j.brat.2014.06.004.
Faul, F., Erdfelder, E., Lang, A. G., & Buchner, A. (2007). G*Power 3: A flexible statistical power analysis program for the social, behavioral, and biomedical sciences. Behavior Research Methods, 39(2), 175–191. https://doi.org/10.3758/BF03193146.
Fergus, T. A., Valentiner, D. P., McGrath, P. B., & Jencius, S. (2010). Shame- and guilt-proneness: Relationships with anxiety disorder symptoms in a clinical sample. Journal of Anxiety Disorders, 24(8), 811–815. https://doi.org/10.1016/j.janxdis.2010.06.002.
Fracalanza, K., McCabe, R. E., Taylor, V., & Antony, M. M. (2014). The effect of comorbid major depressive disorder or bipolar disorder on cognitive behavioral therapy for social anxiety disorder. Journal of Affective Disorders, 162, 61–66. https://doi.org/10.1016/j.jad.2014.03.015.
Gilbert, P. (2000). The relationship of shame, social anxiety and depression: the role of the evaluation of social rank. Clinical Psychology & Psychotherapy, 7(3), 174–189.
Grant, D. M., Beck, J. G., Farrow, S. M., & Davila, J. (2007). Do interpersonal features of social anxiety influence the development of depressive symptoms? Cognition and Emotion, 21(3), 646–663. https://doi.org/10.1080/02699930600713036.
Grunert, B. K., Weis, J. M., Smucker, M. R., & Christianson, H. F. (2007). Imagery rescripting and reprocessing therapy after failed prolonged exposure for post-traumatic stress disorder following industrial injury. Journal of Behavior Therapy and Experimental Psychiatry, 38(4), 317–328. https://doi.org/10.1016/j.jbtep.2007.10.005.
Hackmann, A., Clark, D. M., & McManus, F. (2000). Recurrent images and early memories in social phobia. Behaviour Research and Therapy, 38(6), 601–610. https://doi.org/10.1016/S0005-7967(99)00161-8.
Hackmann, A., Suraway, C., & Clark, D. M. (1998). Seeing yourself through others eyes : A study of spontaneous images in social phobia. Behavioural and Cognitive Psychotherapy, 26, 3–12.
Hedman, E., Ström, P., Stünkel, A., & Mörtberg, E. (2013). Shame and guilt in social anxiety disorder: effects of cognitive behavior therapy and association with social anxiety and depressive symptoms. PLoS ONE. https://doi.org/10.1371/journal.pone.0061713.
Hendriks, S. M., Spijker, J., Licht, C. M. M., Beekman, A. T. F., Hardeveld, F., De Graaf, R., Batelaan, N. M., & Penninx, B. W. J. H. (2014). Disability in anxiety disorders. Journal of Affective Disorders, 166, 227–233. https://doi.org/10.1016/j.jad.2014.05.006.
Hirsch, C. R., Clark, D. M., Mathews, A., & Williams, R. (2003). Self-images play a causal role in social phobia. Behaviour Research and Therapy, 41(8), 909–921. https://doi.org/10.1016/S0005-7967(02)00103-1.
Hirsch, C. R., Mathews, A., Clark, D. M., Williams, R., & Morrison, J. A. (2006). The causal role of negative imagery in social anxiety: A test in confident public speakers. Journal of Behavior Therapy and Experimental Psychiatry, 37(2), 159–170. https://doi.org/10.1016/j.jbtep.2005.03.003.
Hirsch, C. R., Meynen, T., & Clark, D. M. (2004). Negative self-imagery in social anxiety contaminates social interactions. Memory, 12(4), 496–506. https://doi.org/10.1080/09658210444000106.
Holmes, E. A., Arntz, A., & Smucker, M. R. (2007). Imagery rescripting in cognitive behaviour therapy: Images, treatment techniques and outcomes. Journal of Behavior Therapy and Experimental Psychiatry, 38(4), 297–305. https://doi.org/10.1016/j.jbtep.2007.10.007.
Iza, M., Wall, M. M., Heimberg, R. G., Rodebaugh, T. L., Schneier, F. R., Liu, S. M., & Blanco, C. (2014). Latent structure of social fears and social anxiety disorders. Psychological Medicine, 44(2), 361–370. https://doi.org/10.1017/S0033291713000408.
Kessler, R. C., Berglund, P., Demler, O., Jin, R., Merikangas, K. R., & Walters, E. E. (2005). Lifetime prevalence and age-of-onset distributions of DSM-IV disorders in the national comorbidity survey replication. Archives of General Psychiatry, 62(6), 593–602. https://doi.org/10.1001/archpsyc.62.6.593.
Kessler, R. C., Stang, P., Wittchen, H.-U., Stein, M., & Walters, E. E. (1999). Lifetime comorbidities between social phobia and mood disorders in the US National Comorbidity Survey. Psychological Medicine, 29(3), 555–567. https://doi.org/10.1017/S0033291799008375.
Knutsson, J., Nilsson, J. E., Eriksson, Å., & Järild, L. (2019). Imagery rescripting and exposure in social anxiety: A randomized trial comparing treatment techniques. Journal of Contemporary Psychotherapy, Abramowitz. https://doi.org/10.1007/s10879-019-09448-1.
Kuyken, W., & Howell, R. (2006). Facets of autobiographical memory in adolescents with major depressive disorder and never-depressed controls. Cognition and Emotion, 20(3–4), 466–487. https://doi.org/10.1080/02699930500342639.
La Greca, A., & Harrison, H. M. (2005). Adolescent peer relations, friendships, and romantic relationships: Do they predict social anxiety and depression? Journal of Clinical Child and Adolescent Psychology, 34(1), 49–61. https://doi.org/10.1207/s15374424jccp3401.
Landoll, R. R. (2005). the Teenage and Early Adult Years. 75–91.
Leary, M. R. (1983). A brief version of the Fear of Negative Evaluation Scale. Personality and Social Psychology Bulletin, 9, 371–375.
Lee, S. W., & Kwon, J. H. (2013). The efficacy of Imagery Rescripting (IR) for social phobia: A randomized controlled trial. Journal of Behavior Therapy and Experimental Psychiatry, 44(4), 351–360. https://doi.org/10.1016/j.jbtep.2013.03.001.
Lemoult, J., Rowa, K., Antony, M. M., Chudzik, S., & McCabe, R. E. (2014). Effect of comorbid depression on cognitive behavioural group therapy for social anxiety disorder. Behaviour Change, 31(1), 53–64. https://doi.org/10.1017/bec.2013.32.
Lovibond, P. F., & Lovibond, S. H. (1995). The structure of negative emotional states: Comparison of the Depression Anxiety Stress Scales (DASS) with the Beck Depression and Anxiety Inventories. Behaviour Research and Therapy, 33(3), 335–343. https://doi.org/10.1016/0005-7967(94)00075-U.
Matos, M., Pinto-Gouveia, J., & Gilbert, P. (2013). The effect of shame and shame memories on paranoid ideation and social anxiety. Clinical Psychology and Psychotherapy, 20(4), 334–349. https://doi.org/10.1002/cpp.1766.
Mattick, R., & Clarke, C. (1998). Development and validation of measure of social phobia scrutiny fear and social interaction anxiety. Behavior Research and Therapy, 36(455), 70. https://doi.org/10.1016/S0005-7967(97)10031-6.
McEvoy, P. M., Erceg-Hurn, D. M., Saulsman, L. M., & Thibodeau, M. A. (2015). Imagery enhancements increase the effectiveness of cognitive behavioural group therapy for social anxiety disorder: A benchmarking study. Behaviour Research and Therapy, 65, 42–51. https://doi.org/10.1016/j.brat.2014.12.011.
McEvoy, P. M., & Saulsman, L. M. (2014). Imagery-enhanced cognitive behavioural group therapy for social anxiety disorder: A pilot study. Behaviour Research and Therapy, 55(1), 1–6. https://doi.org/10.1016/j.brat.2014.01.006.
Modini, M., Abbott, M. J., & Hunt, C. (2015). A systematic review of the psychometric properties of trait social anxiety self-report measures. Journal of Psychopathology and Behavioral Assessment, 37(4), 645–662. https://doi.org/10.1007/s10862-015-9483-0.
Mörtberg, E., Clark, D. M., Sundin, Ö., & Åberg Wistedt, A. (2007). Intensive group cognitive treatment and individual cognitive therapy vs. treatment as usual in social phobia: A randomized controlled trial. Acta Psychiatrica Scandinavica, 115(2), 142–154. https://doi.org/10.1111/j.1600-0447.2006.00839.x.
Moscovitch, D. A. (2009). What is the core fear in social phobia? A new model to facilitate individualized case conceptualization and treatment. Cognitive and Behavioral Practice, 16(2), 123–134. https://doi.org/10.1016/j.cbpra.2008.04.002.
Moscovitch, D. A., Gavric, D. L., Merrifield, C., Bielak, T., & Moscovitch, M. (2011). Retrieval properties of negative vs. positive mental images and autobiographical memories in social anxiety: Outcomes with a new measure. Behaviour Research and Therapy, 49(8), 505–517. https://doi.org/10.1016/j.brat.2011.05.009.
Ng, A. S., & Abbott, M. J. (2014). The impact of self-imagery on affective, cognitive, and attentional processes in Social Phobia: A comprehensive literature review of the theoretical and empirical literature. Behaviour Change, 31(3), 159–174. https://doi.org/10.1017/bec.2014.12.
Ng, A. S., Abbott, M. J., & Hunt, C. (2014). The effect of self-imagery on symptoms and processes in social anxiety: A systematic review. Clinical Psychology Review, 34(8), 620–633. https://doi.org/10.1016/j.cpr.2014.09.003.
Nilsson, J. E., Lundh, L. G., & Viborg, G. (2012). Imagery rescripting of early memories in social anxiety disorder: An experimental study. Behaviour Research and Therapy, 50(6), 387–392. https://doi.org/10.1016/j.brat.2012.03.004.
Norton, A. R., & Abbott, M. J. (2016a). Bridging the gap between aetiological and maintaining factors in social anxiety disorder: The impact of socially traumatic experiences on beliefs, imagery and symptomatology. Clinical Psychology and Psychotherapy. https://doi.org/10.1002/cpp.2044.
Norton, A. R., & Abbott, M. J. (2016b). The efficacy of imagery rescripting compared to cognitive restructuring for social anxiety disorder. Journal of Anxiety Disorders. https://doi.org/10.1016/j.janxdis.2016.03.009.
Norton, A. R., & Abbott, M. J. (2017). The role of environmental factors in the aetiology of social anxiety disorder: A review of the theoretical and empirical literature. Behaviour Change. https://doi.org/10.1017/bec.2017.7.
Ohayon, M. M., & Schatzberg, A. F. (2010). Social phobia and depression: Prevalence and comorbidity. Journal of Psychosomatic Research, 68(3), 235–243. https://doi.org/10.1016/j.jpsychores.2009.07.018.
Ottenbreit, N. D., Dobson, K. S., & Quigley, L. (2014). An examination of avoidance in major depression in comparison to social anxiety disorder. Behaviour Research and Therapy, 56(1), 82–90. https://doi.org/10.1016/j.brat.2014.03.005.
Peters, L. (2000). Discriminant validity of the Social Phobia and Anxiety Inventory (SPAI), the Social Phobia Scale (SPS) and the Social Interaction Anxiety Scale (SIAS). Behaviour Research and Therapy, 38(9), 943–950. https://doi.org/10.1016/S0005-7967(99)00131-X.
Rapee, R. M., & Abbott, M. J. (2007). Modelling relationships between cognitive variables during and following public speaking in participants with social phobia. Behaviour Research and Therapy, 45(12), 2977–2989. https://doi.org/10.1016/j.brat.2007.08.008.
Rapee, R. M., Gaston, J. E., & Abbott, M. J. (2009). Testing the efficacy of theoretically derived improvements in the treatment of social phobia. Journal of Consulting and Clinical Psychology, 77(2), 317–327. https://doi.org/10.1037/a0014800.
Rapee, R. M., & Heimberg, R. G. (1997). A cognitive-behavioral model of anxiety in social phobia. Behaviour Research and Therapy, 35(8), 741–756. https://doi.org/10.1016/S0005-7967(97)00022-3.
Reimer, S. G., & Moscovitch, D. A. (2015). The impact of imagery rescripting on memory appraisals and core beliefs in social anxiety disorder. Behaviour Research and Therapy, 75, 48–59. https://doi.org/10.1016/j.brat.2015.10.007.
Romano, M., Hudd, T., Huppert, J. D., Reimer, S. G., & Moscovitch, D. A. (2020). Imagery rescripting of painful memories in social anxiety disorder: a qualitative analysis of needs fulfillment and memory updating. Cognitive Therapy and Research. https://doi.org/10.1007/s10608-020-10149-6.
Romano, M., Moscovitch, D. A., Huppert, J. D., Reimer, S. G., & Moscovitch, M. (2020). The effects of imagery rescripting on memory outcomes in social anxiety disorder. Journal of Anxiety Disorders, 69, 102169. https://doi.org/10.1016/j.janxdis.2019.102169.
Ruscio, A. M., Brown, T. A., Chiu, W. T., Sareen, J., Stein, M. B., & Kessler, R. C. (2008). Social fears and social phobia in the USA: Results from the National Comorbidity Survey Replication. Psychological Medicine, 38(1), 15–28. https://doi.org/10.1017/S0033291707001699.
Shahar, B., Doron, G., & Szepsenwol, O. (2015). Childhood maltreatment, shame-proneness and self-criticism in social anxiety disorder: A sequential mediational model. Clinical Psychology and Psychotherapy, 22(6), 570–579. https://doi.org/10.1002/cpp.1918.
Stangier, U., Heidenreich, T., Peitz, M., Lauterbach, W., & Clark, D. M. (2003). Cognitive therapy for social phobia: Individual versus group treatment. Behaviour Research and Therapy, 41(9), 991–1007. https://doi.org/10.1016/S0005-7967(02)00176-6.
Starr, L. R., Davila, J., La Greca, A., & Landoll, R. R. (2005). Social Anxiety and Depression: The Teenage and Early Adult Years. In C. A. Alfano & D. C. Beidel (Eds.), Social Anxiety in Adolescents and Young Adults: Translating Developmental Science Into Practice (pp. 75–91).
Stein, D. J., Lim, C. C. W., Roest, A. M., de Jonge, P., Aguilar-Gaxiola, S., Al-Hamzawi, A., Alonso, J., Benjet, C., Bromet, E. J., Bruffaerts, R., de Girolamo, G., Florescu, S., Gureje, O., Haro, J. M., Harris, M. G., He, Y., Hinkov, H., Horiguchi, I., Hu, C., & Williams, D. R. (2017). The cross-national epidemiology of social anxiety disorder: Data from the World Mental Health Survey Initiative. BMC Medicine, 15(1), 1–21. https://doi.org/10.1186/s12916-017-0889-2.
Tangney, J. P., Stuewig, J., & Mashek, D. J. (2007). Moral emotions and moral behavior. Annual Review of Psychology, 58, 345–372. https://doi.org/10.1146/annurev.psych.56.091103.070145.
Weeks, J. W., Heimberg, R. G., Hart, T. A., Fresco, D. M., Turk, C. L., Schneier, F. R., & Liebowitz, M. R. (2005). Empirical validation and psychometric evaluation of the brief fear of negative evaluation scale in patients with social anxiety disorder. Psychological Assessment, 17(2), 179–190. https://doi.org/10.1037/1040-3590.17.2.179.
Wheatley, J., & Hackmann, A. (2011). Using imagery rescripting to treat major depression: Theory and practice. Cognitive and Behavioral Practice, 18(4), 444–453. https://doi.org/10.1016/j.cbpra.2010.06.004.
Wheatley, J., Hackmann, A., & Brewin, C. R. (2009). Imagery rescripting for intrusive sensory memories in major depression following traumatic experiences. A Casebook of Cognitive Therapy for Traumatic Stress Reactions, 78–92. http://discovery.ucl.ac.uk/id/eprint/125465.
Wild, J., & Clark, D. M. (2011). Imagery rescripting of early traumatic memories in social phobia. Cognitive and Behavioral Practice, 18(4), 433–443. https://doi.org/10.1016/j.cbpra.2011.03.002.
Wild, J., Hackmann, A., & Clark, D. M. (2007). When the present visits the past: Updating traumatic memories in social phobia. Journal of Behavior Therapy and Experimental Psychiatry, 38(4), 386–401. https://doi.org/10.1016/j.jbtep.2007.07.003.
Wild, J., Hackmann, A., & Clark, D. M. (2008). Rescripting early memories linked to negative images in social phobia: A pilot study. Behavior Therapy, 39(1), 47–56. https://doi.org/10.1016/j.beth.2007.04.003.
Wilson, J. K., & Rapee, R. M. (2005). The interpretation of negative social events in social phobia with versus without comorbid mood disorder. Journal of Anxiety Disorders, 19(3), 245–274. https://doi.org/10.1016/j.janxdis.2004.03.003.
Acknowledgements
The authors would like to thank Amy Burton, Benjamin Larke, Brittany Killer, Cecilia Law Daniel Cheers, Grace Morris, Karishma Menon, and Taylor Moore for their assistance with data collection and administration of the GCBT and IR interventions.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of Interest
Author Alice R. Norton, Author Maree J. Abbott, Author Katie A. Dobinson, Author Karen L. Pepper and Author Adam J. Guastella declare that they have no conflict of interest.
Informed Consent
All procedures followed were in accordance with the ethical standards of the responsible committee on human experimentation (national and institutional). Informed consent was obtained from all individual subjects participating in the study. If any identifying information is contained in the paper the following statement is also necessary -- Additional informed consent was obtained from any subjects for whom identifying information appears in this paper.
Research Involving Human and Animal Participants
No animal studies were carried out by the authors for this article.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
About this article
Cite this article
Norton, A.R., Abbott, M.J., Dobinson, K.A. et al. Rescripting Social Trauma: A Pilot Study Investigating Imagery Rescripting as an Adjunct to Cognitive Behaviour Therapy for Social Anxiety Disorder. Cogn Ther Res 45, 1180–1192 (2021). https://doi.org/10.1007/s10608-021-10221-9
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s10608-021-10221-9