Abstract
Data on 1,271 clients in three residential care services funded by the Department of Veterans Affairs was used to examine: (1) how religious-oriented programs differ in their social environment from secular programs, (2) how religious-oriented programs affect the religiosity of clients, and (3) how client religiosity is associated with outcomes. Programs were categorized as: secular, secular now but religious in the past, and currently religiously oriented. Results showed (1) participants in programs that were currently religious reported the greatest program clarity, but secular services reported the most supportive environments; (2) participants in programs that were currently religious did not report increases in religious faith or religious participation over time; nevertheless (3) greater religious participation was associated with greater improvement in housing, mental health, substance abuse, and quality of life. These findings suggest religious-oriented programs have little influence on clients’ religious faith, but more religiously oriented clients have somewhat superior outcomes.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Faith-based organizations have a long history of providing social services in America. In fact, one of the earliest progressive movements in psychiatric care in the United States was “moral treatment”, in which therapies were based on Christian values and Protestant ethics (Taubes 1998). Mental health treatment has changed dramatically in the last century, with advances in science and medicine. But religious congregations continue to play a central role in local social services nationwide (Wineburg 1993). Moreover, various large organizations, such as the Salvation Army and Habitat for Humanity, have promoted ministry through religiously motivated social programs and homeless services (Hayes 2002; Winston 2000).
There has been little research on the religious orientation of homeless programs and the effect of religious orientation on clients’ religious beliefs and clinical outcomes. The 1996 National Survey of Homeless Assistant Providers and Clients found that of the 40,000 homeless assistance programs operating on an average day, a third were run by faith-based non-profit organizations (Aron and Sharkey 2002). Faith-based providers were found to serve a more diverse group of clients (e.g., single men, females with children) than secular services, and were less likely to have a special focus (e.g., victims of domestic violence or clients with AIDS). They have also been found to differ from secular providers on several other dimensions, including more reliance on volunteers, lack of government funding, religious leaders as board members, and hiring of religiously oriented staff (Ebaugh et al. 2003). Proponents of expanding faith-based social services have argued that religiously-based groups provide more effective social services because of their supportive and caring religious attitudes and because faith itself leads to a better life, while opponents have challenged these assertions noting the lack of empirical evidence.
A religious presence or influence on services may not only exist in faith-based organizations; but also in non-religious organizations, such as Alcoholics Anonymous, that include a spiritual component in their peer support groups (Kurtz 1991; Tonigan et al. 2002). Other organizations, like United Way, Volunteers of America, and the Young Men’s Christian Association (YMCA), were founded on religious principles, but have since become a more secular or “general service” (Zald and Denton 1963). Most homeless programs do not hold any religious ideology and the first amendment constraints governmentally funded services from promoting religious practice or faith. Nonetheless, many organizations have formal or informal referral systems to and from religious service providers (Gottlieb and Olfson 1987; Oppenheimer et al. 2004).
Research on religion and health have consistently shown that religious involvement reduces the likelihood of developing illness and improves recovery from a variety of physical diseases, including cardiovascular diseases, emphysema, cirrhosis, hypertension, and mortality (George et al. 2000; Strawbridge et al. 1997). Even stronger evidence has been found between religious involvement and mental health and substance abuse outcomes. In both cross-sectional and longitudinal studies, institutional religious participation is correlated with reduced likelihood of developing a variety of mental illness, including anxiety disorders, depression, and alcohol and drug use disorders (George et al. 2000; Koenig et al. 2001). Religious involvement has also been associated with greater improvement in psychiatric and substance use disorder, and in quality of life.
Proposed pathways by which religion is related to health include better health behaviors, social support, and a sense of coherence and meaning in life (George et al. 2000; Strawbridge et al. 1997). The “coherence hypothesis” has received the most support, suggesting a sense of coherence buffers the effects of stress on health. These findings have led many researchers to encourage better cooperation between religious providers and mental health systems and for mental health professionals to incorporate religiosity into their clinical practice (Koenig et al. 2001; Larimore et al. 2002; Oppenheimer et al. 2004). President Bush’s Faith-based and Community Initiative was a prominent example (Formicola et al. 2003). The extent to which homeless clients with mental illness are affected by their own religious orientations or those of their programs has not been well-researched.
The current study differentiated between programs that were once religious but are now secular from programs that have always been secular and programs that currently have a religious orientation. First, we examined at the program level, how religious-oriented residential care programs differ in their social environment from secular programs and how religiously oriented programs affect the religious faith of clients. Then, at the individual level, we examined the association between clients’ religious faith and their clinical outcomes net of potentially confounding factors. Our hypotheses were that: (1) religious-oriented programs would have more structure, clarity, and staff control than secular programs; (2) religious-oriented programs would be associated with increased religious faith of clients over time; and (3) increase in religious faith would be associated with improvements in clinical outcomes.
Methods
Program Type
Three major forms of VA-funded residential care service for homeless veterans were included in this study: the Health Care for Homeless Veterans (HCHV) program, the Grant and Per Diem (GPD) program, and the Domiciliary Care for Homeless Veteran Program (DCHV). The HCHV and GPD programs provide assistance to veterans through contracts with community service providers while the DCHV program provides services directly through VA staff in domiciliaries located on VA grounds. Data was collected for a prospective, naturalistic study to compare these three VA-funded residential care programs (McGuire et al. 2011). The current study included a total of 1,271 participants at 16 HCHV, 18 GPD, and 6 DCHV programs, spread across five VA administrative regions encompassing Cleveland/Cincinnati, Ohio; Los Angeles, California; Philadelphia, Pennsylvania; Tampa/Miami, Florida; Baltimore/Martinsburg/Washington, District of Columbia. All three types of residential care services were available to veterans at each of the five sites.
Procedures
Data collection was conducted from May 2002 through September 2005. At each site, independent study evaluators recruited, consented, and conducted baseline interviews with veterans in the residential care programs. Follow-up interviews were conducted with veterans 1, 3, 6, and 12 months after leaving the program. Homeless veterans were eligible for participation if they were currently admitted to one of the three residential care programs. Each participant gave informed consent and was paid $10 for the baseline interview and $25 for each of the follow-up interviews. At each site, program directors were also interviewed on the size, location, policy, services, treatment philosophy, and faith-based program characteristics of their program. All procedures were approved by the institutional review boards at each of the sites.
Measures
Program-Level Measures
An annual program survey documented the sponsoring organization of each program and whether it was secular, formerly faith-based, or currently faith-based based on program directors’ report. Secular was defined as “a private or public agency with no religious base or history”; formerly faith-based was defined as a “private agency that at one time had a religious orientation but today has evolved into an agency that is largely secularly based”; and currently faith-based was defined as a “private agency that continues to have a clear religious base and orientation.”
Individual-Level Measures
Sociodemographics, a brief housing history, and psychiatric diagnoses of participants were obtained during baseline interviews after they had been admitted to the residential program. Diagnostic assessments were conducted by VA staff, most of whom were master’s level social workers, paraprofessional social work staff, or nursing staff and reviewed by licensed clinical social workers. At baseline, participants were also asked to complete a measure of the program environment in their residential care service (Moos and Otto 1972).
At both baseline and follow-up interviews, a series of measures were administered to participants to assess their religiosity, employment status, housing status, physical and mental health, and quality of life.
Religiosity
Participants were asked to rate how often they attended “church, synagogue, mosque, temple or other religious services or meetings” on a 6-point scale from 0 (More than once a week) to 5 (Never). Responses were reverse-coded so that higher scores indicated greater religious participation.
Religious faith was assessed with a question adapted from a religious coping index (Koenig et al. 1992) that asked participants to rate how important was “religious faith or belief, for example, Christianity, Islam, Judaism, or Buddhism” in their lives on a 5-point scale from 0 (Not important) to 4 (Extremely important).
Work
Participants were asked about their current employment pattern and classified as either employed (i.e., full time, part time, vocational training) or not employed (i.e., retired/disability, unemployed). Participants were also asked the number of days they worked for pay in the past 30 days.
Housing
Participants were asked how many days in the last 30 days they had slept in nine different types of places. These places were classified as days housed (i.e., own apartment, room, or house; somebody else’s apartment, room, or house), days in institution (i.e., hospital or nursing home, domiciliary, halfway house programs, hotels, boarding homes, hotels, prisons, jails) and days homeless (i.e., shelters, outdoors, abandoned buildings, automobiles, boats).
Health Measures
Medical conditions were assessed with 12 questions that asked participants yes/no whether they had any of 12 common serious medical problems (e.g., hypertension, cardiovascular problems, liver disease, orthopedic problems). Responses were summed for a total score indicating the number of serious medical problems participants had (Melfi et al. 1995).
Alcohol and drug use in the past month was assessed with the Addiction Severity Index (ASI; McLellan et al. 1980), which consists of 6 items on an alcohol subscale, 13 items on a drug subscale, and 8 items on a psychiatric subscale. Responses are calculated for a standard index score ranging from 0 to 1 for each subscale with higher scores reflecting more serious substance use or psychiatric problems.
General physical and mental health were assessed with the Medical Outcomes Short-Form 12 (SF-12; Ware et al. 1996). The SF-12 consists of 12 items that generate a standardized mental component summary (MCS) score and a physical component summary (PCS) score. Scores range from 0 to 100, with an average score of 50 (SD = 10) in the general population and higher scores indicating better health. The SF12 has been validated as an outcome measure in homeless populations (Larson 2002).
Quality of Life
Subjective quality of life was assessed with the Lehman Quality of Life Interview (Lehman 1988) in the following domains: general quality of life, perceptions of quality of employment, and quality of social life. Participants were asked to rate these following domains on a 7-point scale from 1 (Terrible) to 7 (Delighted).
Program Environment
At baseline, participants were asked to rate their perceptions of the treatment environment of their residential care program using the Community-Oriented Programs Environment Scale (COPES; Moos and Otto 1972). This well-validated 100-item instrument consists of ten subscales: Involvement, Support, Spontaneity, Autonomy, Practical Orientation, Personal Problem Orientation, Anger and Aggression, Order and Organization, Program Clarity, and Staff Control.
The Involvement subscale reflects how active participants are in day-to-day functioning of the program. The Support subscale reflects how much participants help and support each other and how supportive staff members are toward participants. The Spontaneity subscale assesses how much the program encourages open expression of feelings by participants and staff. The Autonomy subscale measures how self-sufficient and independent participants are in decision making and how much they are encouraged to take leadership in the program. The Practical Orientation subscale assesses the degree to which participants learn practical skills and are prepared for program release. The Personal Problem Orientation subscale measures the extent to which participants are encouraged to understand their feelings and personal problems. The Anger and Aggression subscale measures how much program participants argue with each other and with staff, become openly angry, and display aggressive behavior. The Order and Organization subscale rates how important order and organization are in the program. The Program Clarity subscale rates the extent to which participants know what to expect in the day-to-day routine of the program and the explicitness of program rules and procedures. The Staff Control subscale reflects the extent to which staff members try to keep participants under a level of control.
Data Analysis
Participants were grouped into three categories based on the program to which they had been admitted: secular residential care programs, programs with a religious history but presently secular in orientation, and services that currently had a religious orientation. Baseline individual differences among participants in each type of program were examined with analysis of variance (ANOVA) and Chi-square tests. Then, linear mixed regression analyses were conducted to examine the religious participation and religious faith of participants in different programs over time. Baseline differences were controlled for and an autoregressive covariance structure was specified in a mixed longitudinal model. Least square means were calculated and Fisher’s Least Significant Difference test was used to make post-hoc comparisons among pairs of programs.
To examine the association between change in religiosity and clinical outcomes at the individual level, Pearson correlations were conducted between program religious orientation, individual change scores in religious faith and in religious participation, and clinical outcomes. Change scores were calculated by subtracting 12 months follow-up scores from baseline scores. To examine this further, hierarchical multiple regression analyses were conducted to control for the effect of site and sociodemographics on clinical outcomes. Site and sociodemographics were entered into the first block and religious variables were entered into the second block to observe their incremental validity.
Results
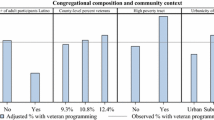
Table 1 shows the baseline characteristics of all participants. As the DCHV was a uniformly secular VA residential care program with no religious affiliation, participants in programs with either a religious history or a current religious orientation were all from GPD or HCHV groups. Participants in programs with a current religious orientation were more likely to be White than participants in other programs while participants in secular residential care programs were more likely to be Black, have a mood disorder or a drug disorder, than other participants.
At baseline, participants in secular programs actually reported more active religious participation than participants in programs with a religious history, but there were no program differences in personal religious faith (Table 1). A higher proportion of participants in secular programs reported that they were employed at the time of program entry and they also reported more days of work than other participants. On health measures, participants in programs with a religious history reported better mental health on the ASI-Psych and the SF-12 MCS. There were no baseline group differences in housing or quality of life ratings.
In comparing the social environment of the three types of programs, significant differences were found on 9 of the 10 subscales of the COPES. Participants in secular residential care services reported the highest scores on several subscales, including Involvement, Practical Orientation, Personal Problem Orientation, and Anger and Aggression. Participants in programs with a current religious orientation were similar to secular services on Support and Spontaneity, and reported more Program Clarity than participants in other programs. Participants in programs with a religious history reported the greatest Staff Control, but had the lowest scores on many other subscales, including Involvement, Support, Spontaneity, Order and Organization, and Program Clarity.
Overall, there was an increase in religious participation among participants over time (Table 2); however, this was limited to participants who were in programs with a religious history that were now secular. There was a significant group*time interaction, F(3,1374) = 4.69, P < .01, such that participants in currently religious or secular programs did not show an increase in religious participation.
There was no greater increase in religious faith among participants in any of the programs. However, surprisingly, there was a group effect among participants in programs that had a current religious orientation, with greater religious faith reported among participants in secular programs.
The religious orientation of the program was not correlated with clinical outcomes with the single exception that religious-oriented programs were associated with a greater decrease in SF-12 PCS scores (Table 3).
Participants who reported they were more engaged in religious activities reported a smaller increase in days housed and more days in institutions than others. They also reported greater improvements on SF-12 MCS scores, general quality of life, quality of their social life, quality of their employment life, and lower ASI-Alcohol and ASI-Drug scores. Similarly, positive changes in participants’ religious faith was associated with fewer days homeless, higher general quality of life, higher ratings of social life, and higher quality of employment. The correlation between change in religious faith and change in religious participation was weak to moderate in magnitude (r = 0.23, P < .001).
When site and sociodemographics were controlled for in hierarchical multiple regression analyses (Table 4), individual-level religious variables were still significantly associated with superior clinical outcomes (Table 4). Increase in religious participation was associated with fewer days housed, but also increases in SF-12 MCS scores, general quality of life, quality of social life, and lower ASI-Alcohol and ASI-Drug scores. Increase in religious faith was associated with positive changes in social quality of life. Together, religious variables explained significant (2–5%) variance in days housed, SF-12 MCS scores, general quality of life, social quality of life, ASI-Alcohol scores, and ASI-Drug scores. Variables reflecting individual religiosity were not associated with any adverse outcomes.
Discussion
This study compared three types of VA-funded residential care services for homeless veterans: programs that have always been secular, programs that have a religious history but are currently secular, and programs that have a current religious orientation. At the program level, our first hypothesis was only partially supported: participants in programs that were currently religiously oriented reported the greatest amount of program clarity, but it was participants in secular programs who reported the most order and organization in their services and participants in programs with a religious history who reported the greatest amount of staff control. These differences are of small magnitude, but may reflect differences in funding sources, organizational culture, leadership preferences, and staffing characteristics found between secular and faith-based social services (Ebaugh et al. 2003).
In general, participants in programs with a religious history reported having the least supportive environments, as indicated by measures of client involvement, staff support, program organization, and the degree to which client feelings were encouraged. In contrast, participants in programs that were secular reported the most involvement and reported their programs encouraged the most active learning and emotional expression. Programs with a current religious orientation did not stand out, in that participants in those programs mostly reported relatively moderate scores on measures of program environment.
Contrary to our second hypothesis, participants in programs that had a current religious orientation did not report increased religious faith or religious participation over time. In fact, most participants reported they attended religious services between “a few times a year” to “a few times a month” and that religion was somewhere between “somewhat important” to “very important” to them throughout the study, regardless of time or the religious orientation of the program. On the one hand, religiosity may be a personal, stable characteristic that is not easily influenced by external factors. On the other, programs may not place much emphasis on changing religious attitudes, in part, because it would conflict with First Amendment requirements for separation of church and state.
Our third hypothesis was empirically supported, in that at the client level, greater religious faith and, particularly, religious participation, were associated with greater improvement in clinical outcomes. Participants who reported an increase in their religious participation experienced slightly fewer days housed, but better mental health symptoms, less substance abuse, and higher quality of life. Although religious participation explained only a small amount of variance in clinical outcomes, it is consistent with previous studies that have shown religious participation is a strong predictor of mental illness and recovery (George et al. 2000; Koenig et al. 2001).
These findings are consistent with the extant literature on religion and mental health, which suggest religious involvement can improve the health practices and social lives of clients (George et al. 2000; Strawbridge et al. 1997). The implications of this study are that support should be provided to clients who are religious, regardless of housing type, to enhance treatment outcomes. Increasingly, researchers have begun to recognize the importance of religion and spirituality, more generally, in the recovery process. They have recommended clinicians support their clients’ spiritual beliefs, encourage participation in religious institutions as a possible social resource, and help coordinate and refer religious services when appropriate (Johnson et al. 2011; Koenig et al. 2001; Larimore et al. 2002). Some possible ways religious support can be provided, include offering spirituality groups, inviting clergy or chaplains to be part of services, making referrals for worship services, and encouraging the use of religious resources as effective coping methods.
This study had several limitations. Although our data were longitudinal in nature, we cannot infer causal relationships between religious faith and participation and superior outcomes because clinical improvement could have led to greater appreciation, faith, and worship. Furthermore, since DCHV was solely a secular program, differences found between secular and religious programs may have been due to the type of residential care service rather than the religious history and orientation of the program. However, we did include site as a covariate in the analyses, which would have controlled for the effect of the HCHV and GPD programs. Participant attrition was moderate, and there was a limited sample of participants that provided data throughout the one-year period. However, statistical power was adequate as many findings reached statistical significance. In this study, we only assessed religiosity and did not measure spirituality. Some participants may define themselves as being more spiritual than religious (Pardini et al. 2000). Nonetheless, this study showed that faith-based organizations had little impact on the religious participation or religious faith of homeless veterans, but that veterans who were more active in their religion had better mental health outcomes.
Conclusions
The religious faith of homeless veterans appears to be a stable characteristic and religious-oriented programs had little influence on religious faith. Compared to secular programs, participants in religious-oriented programs report greater program clarity but not necessarily more supportive environments. Regardless, religious participation is associated with better housing and clinical outcomes suggesting that spirituality and religious practice may be of importance in the recovery of homeless clients.
References
Aron, L. Y., & Sharkey, P. T. (2002). The 1996 national survey of homeless assistance providers and clients: A comparison of faith-based and secular non-profit programs. Washington, D.C.: The Urban Institute.
Ebaugh, H. R., Pipes, P. F., Chafetz, J. S., & Daniels, M. (2003). Where’s the religion? Distinguishing faith-based from secular social services agencies. Journal for the Scientific Study of Religion, 42(3), 411–426.
Formicola, J. R., Segers, M. C., & Weber, P. (2003). Faith-based initiatives and the Bush administration: The good, the bad, and the ugly. Lanham, MD: Rowman & Littlefield Publishers, Inc.
George, L. K., Larson, D. B., Koenig, H. G., & McCullough, M. E. (2000). Spirituality and health: What we know, what we need to know. Journal of Social and Clinical Psychology, 19(1), 102–116.
Gottlieb, J. F., & Olfson, M. (1987). Current referral practices of mental health care providers. Hospital & Community Psychiatry, 38(11), 1171–1181.
Hayes, R. A. (2002). Habitat for humanity: Building social capital through faith based service. Journal of Urban Affairs, 24(3), 247–269.
Johnson, K. S., Tulsky, J. A., Hays, J. C., Arnold, R. M., Olsen, M. K., Lindquist, J. H., et al. (2011). Which domains of spirituality are associated with anxiety and depression in patients with advanced illness? Journal of General Internal Medicine, 26(7), 751–758.
Koenig, H. G., Cohen, H. J., Blazer, D. G., Pieper, C., Meador, K. G., Shelp, F., et al. (1992). Religious coping and depression among elderly, hospitalized medically ill men. American Journal of Psychiatry, 149(12), 1693–1700.
Koenig, H. G., McCullough, M. E., & Larson, D. B. (2001). Handbook of religion and health: A century of research reviewed. New York: Oxford University Press.
Kurtz, E. (1991). Not-god: A history of alcoholics anonymous. Center City, MN: Hazelden Publishing.
Larimore, W. L., Parker, M., & Crowther, M. (2002). Should clinicians incorporate positive spirituality into their practices? What does the evidence say? Annals of Behavioral Medicine, 24(1), 69–73.
Larson, C. O. (2002). Use of the SF-12 instrument for measuring the health of homeless persons. Health Services Research, 37, 733–750.
Lehman, A. F. (1988). A quality of life interview for the chronically mentally ill. Evaluation and Program Planning, 11, 51–62.
McGuire, J. F., Rosenheck, R. A., & Kasprow, W. J. (2011). Patient and program predictors of 12-month outcomes for homeless veterans following discharge from time-limited residential treatment. Administration and Policy in Mental Health and Mental Health Services Research, 38(3), 142–154.
McLellan, A. T., Luborsky, L., Woody, G. E., & O’Brien, C. P. (1980). An improved diagnostic evaluation instrument for substance abuse patients: The Addiction Severity Index. Journal of Nervous and Mental Disease, 168, 26–33.
Melfi, C., Holleman, E., Arthur, D., & Katz, B. (1995). Selecting a patient characteristics index for the prediction of medical outcomes using administrative claims data. Journal of Clinical Epidemiology, 48(7), 917–926.
Moos, R., & Otto, J. (1972). The Community-Oriented Programs Environment Scale: A methodology for the facilitation and evaluation of social change. Community Mental Health Journal, 8(1), 28–37.
Oppenheimer, J. E., Flannelly, K. J., & Weaver, A. J. (2004). A comparative analysis of the psychological literature on collaboration between clergy and mental health professionals—perspectives from secular and religious journals: 1970–1999. Pastoral Psychology, 53(2), 153–162.
Pardini, D. A., Plante, T. G., Sherman, A., & Stump, J. E. (2000). Religious faith and spirituality in substance abuse recovery: Determining the mental health benefits. Journal of Substance Abuse Treatment, 19(2), 347–354.
Strawbridge, W. J., Cohen, R. D., Shema, S. J., & Kaplan, G. A. (1997). Frequent attendance at religious services and mortality over 28 years. American Journal of Public Health, 87(6), 957–961.
Taubes, T. (1998). ‘Healthy avenues of the mind’: Psychological theory building and the influence of religion during the era of moral treatment. American Journal of Psychiatry, 155(8), 1001–1008.
Tonigan, J. S., Miller, W. R., & Schermer, C. (2002). Atheists, agnostics and alcoholics anonymous. Journal of Studies on Alcohol, 63(5), 534–541.
Ware, J. E., Kosinski, M., & Keller, S. D. (1996). A 12-item Short-Form Health Survey: Construction of scales and preliminary tests of reliability and validity. Medical Care, 34(3), 220–233.
Wineburg, R. J. (1993). Social policy, community service development, and religious organizations. Nonprofit Management & Leadership, 3(3), 283–297.
Winston, D. (2000). Red-hot and righteous: The urban religion of the Salvation Army. Boston: Harvard University Press.
Zald, M. N., & Denton, P. (1963). From evangelism to general service: The transformation of the YMCA. Administrative Science Quarterly, 8(2), 214–234.
Acknowledgments
This work was supported by the Department of Veterans Affairs, Veterans Health Administration, Office of Research and Development. The views presented here are those of the authors, alone, and do not represent the position of any federal agency or of the United States Government.
Conflict of Interest
None of the authors had any conflict.
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Tsai, J., Rosenheck, R.A., Kasprow, W.J. et al. Do Faith-Based Residential Care Services Affect the Religious Faith and Clinical Outcomes of Homeless Veterans?. Community Ment Health J 48, 682–691 (2012). https://doi.org/10.1007/s10597-011-9456-z
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s10597-011-9456-z