Abstract
Precision treatment for breast cancers has made several notable advances in recent decades, but challenges of tumor heterogeneity, drug resistance, and aggressive recurrence and metastases remain. To meet and overcome these challenges, we must refine our understanding of breast subtypes and treatment biomarkers according to the knowledge afforded across the spectrum of ‘omics assays. A critical aspect of harnessing this knowledge into actionable biomarkers for treatment decision relies on our ability to integrate knowledge across data types and leverage our insight in evidence-based clinical trials. We review recent advances in cutting-edge clinical trials for precision treatment of breast cancer, including chemotherapies, targeted therapies, immunotherapies, and combination therapies. We comment on promising future areas of development for this exciting point in precision breast cancer research.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
In recent decades, precision treatment for breast cancers has seen rapid progress. Indeed, breast cancer is the poster child with remarkable progress being made by subsetting ductal breast cancer into three different treatment platforms based on characterization of biomarkers: estrogen receptor/progesterone receptor (ER/PR) expression and human epidermal growth factor receptor 2 (HER2). The next step in improving outcomes for breast cancer patients is to refine subsets and treatments based on additional informational content such as that afforded by characterization of genomics and other omics platforms. One striking advance has been the identification of a group of low risk patients who do not need or benefit from chemotherapy. The next phase in this journey will encompass the much greater information content afforded by a comprehensive and integrative analysis of the tumor and the tumor ecosystem at the DNA, RNA, and protein levels.
Our ability to match therapies to patients based on specific tumor genetic alterations in breast cancer has been supported by large consortium efforts to profile breast cancers across the spectrum of ‘omics data. For breast cancer treatment, we have seen expansion of biomarkers designed to enable choice of specific chemotherapies, targeted therapies, immune therapies, and importantly combination therapy. However, most of these are in the preclinical phase and have not yet translated to the clinical arena. Indeed, despite our major gains, we currently face challenges, namely recurrence of cancers in aggressive and resistant forms which ultimately lead to patient relapse and death. There is, thus, a pressing need for treatment strategies that can provide a longer duration of benefit to the patient, prevent tumor recurrence, and overcome drug resistance. Further, there is great need of improved treatment options for recurrent and aggressive metastatic cancers, as these patients often exhaust all available therapy options.
Consortium efforts such as the Cancer Genome Atlas (TCGA) [1], the International Cancer Genome Consortium [2] and an East Asian breast cancer cohort [3] have enabled us to deeply profile breast cancers across data types and define molecular-driven subtypes for precision treatment. The canonical breast cancer molecular subtypes [1] (luminal A and B breast cancers, HER2 positive breast cancers, and triple-negative breast cancers (TNBC), have all seen improvements in outcomes and an expansion of targeted therapy options. Precision treatments based on subtype includes estrogen receptors for hormone driven cancers, HER2 inhibitors for HER2-positive cancers, and poly ADP Ribose Polymerase (PARP) inhibitors for triple negative breast (TNBC) with BRCA1/2 mutations and immune checkpoint blockade for patients with tumors with elevated programed-death ligand 1 (PD-L1). However, these efforts have thus far focused on profiling primary, un-treated breast cancer tumor samples with only a limited number of metastatic or drug-treated samples being deeply characterized. During tumor progression and therapy, breast cancers can gain additional aberrations with a coordinate increase in heterogeneity that can limit the efficacy of therapy; by the time a metastatic cancer is evident or becomes resistant to therapy, the complexity and heterogeneity present far outstrips our therapeutic capabilities.
While consortium efforts for metastatic breast cancers are currently underway, such as the AURORA [4] multi-national effort for longitudinal metastatic breast cancer screening, they are nascent and not yet publicly available to the greater research community. Cohort-level molecular profiling efforts for metastatic disease, such as the DNA analysis of 50 patients by Brown, et al. [5] and the combined genomic and immune analysis of 10 patients by De Mattos-Arruda, et al. [6] are demonstrating incredible complexity and heterogeneity in metastatic disease. Scaling up metastatic disease cohort studies will be critical for supporting future clinical trials for therapies focused on late stage aggressive disease.
In a parallel challenge, while our understanding of drug resistance mechanisms in breast cancer is improving, our ability to effectively treat resistant tumors is lagging. While there is wide consensus that precision treatment requires combination therapy, these therapies must be rigorously assessed for improved efficacy and acceptable toxicity as compared to monotherapies alone. Increasingly, we are seeing clinical trials for combination therapies across drug classes, such as targeted therapies and immunotherapies. However, our ability to select combination therapies that will be effective in individual patients based on biomarkers is very limited.
Next generation clinical trial design
Recent advancements of next generation sequencing and comprehensive genomic, transcriptomic and proteomic profiling enable detailed classification of breast tumors into different molecular subtypes. Targeted therapy against genomic vulnerabilities such as the HER2 [7, 8] or lineage dependencies such as the ER [9] in each subtype have remarkably improved patient survival and provides conceptual support for future trials guided by molecular markers. However, it is unrealistic to test a single drug in a single tumor subtype in one clinical trial given the lengthy timeline of clinical trial studies. The rise of the “master protocol” concept aims to establish a common protocol to assess several molecular markers and their targeted therapies by means of multiple sub-studies designed for each tumor subtype. The standardization of procedures in the development and assessment of different interventions enables more efficient and accelerated drug development. Furthermore, it provides a powerful platform for biomarker identification and validation as well as for elucidation of mechanisms of resistance and development of combination therapies. In addition, the sub-study design of master protocols allows researchers to evaluate multiple gene targets in the same pathway, which is otherwise impossible under the traditional design of a single intervention clinical trial.
Master protocols are often classified into “basket trials”, “umbrella trials”, and “adaptive trials” [10, 11] (Table 1). Basket trials are an innovative, histology-independent trial design where patients with different types of cancer that share common molecular aberrations are evaluated under a single protocol. For instance, an ongoing multicenter MEDIOLA basket trial (NCT02734004) has been conducted to evaluate the combination of durvalumab and olaparib in patients with BRCA1/2 mutated metastatic breast cancer, ovarian cancer, gastric cancer and relapsed small-cell lung cancer. In other words, BRCA1/2 mutation is the common predictive biomarker or risk factor that allows identification of patients who are predicted to respond to this combination targeted therapy, despite differing histological types of cancer. Another ongoing phase II HERALD trial (JapicCTI-194707) aims to evaluate efficacy and safety of trastuzumab deruxtecan in advanced HER2 amplified solid tumors identified by circulating tumor DNA (ctDNA) analysis, which is less invasive compared to the conventional tissue-based HER2 test.
Umbrella trials, on the other hand, evaluate multiple targeted therapies for patients with the same type of cancer where the patients are divided into many subgroups depending on molecular features in their tumors. For example, the MORPHEUS platform includes multiple phase Ib/II trials designed to assess activity of atezolizumab cancer immunotherapy combinations towards metastatic or unresectable locally advanced HR+ (NCT03280563) and TNBC breast cancer (NCT03424005). PlasmaMATCH (NCT03182634) is a multicenter umbrella trial assessing the feasibility and clinical utility of ctDNA analysis to direct therapy in patients with advanced breast cancer. The therapies are stratified into 5 treatment groups based on the expression of targetable mutations in ESR1, HER2, AKT and PTEN genes with therapies matched to the mutation found in the plasma. The fifth cohort includes patients with triple negative breast cancer (TNBC) with no targetable mutations, and patients in this cohort will receive olaparib plus ATR inhibitor AZD6738.
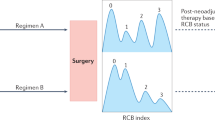
The purpose of adaptive trials is to introduce flexibility in the selection of therapy and biomarkers that may become desirable during the course of trial. Further, it allows rapid changes in light of data arising within the trial. This type of study designs allow modifications in the study during its conduct in accordance with pre-specified rules. Trials with an adaptive design can make better use of resources and are designed to decrease the number of patients enrolled on ineffective therapies, and thus are more efficient, informative and ethical than traditional trials with a fixed design. The Investigation of Serial Studies to Predict Your Therapeutic Response with Imaging and Biomarker Analysis-1 (I-SPY 1) [12] and -2 (I-SPY 2) trials [13] involved early stage breast cancer patients, in the neoadjuvant setting. The goal of these studies is to improve precision medicine by learning which drug agents are more effective in subtypes of breast cancer classified by molecular signatures, and to identify indicators of response (biomarkers) that are predictors of treatment success. During the course of trials, regimens that show a high probability of being more effective than standard therapy will graduate to further trials with their molecular signatures, while regimens show low predictive probability of improved efficacy will be dropped. New drugs can also enter throughout the course of the trial.
Recent evidence supports the concept of clonal evolution of breast tumors, with metastases acquiring new molecular aberrations as compared to the primary tumors that can be further exacerbated by the selective pressures induced by therapy, and eventually alter treatment sensitivity. To understand the tumor life cycle and its clinical impact, longitudinal trials such as the Aiming to Understand the Molecular Aberrations in Metastatic Breast Cancer (AURORA) study (NCT02102165) is designed to characterize molecular landscape of metastatic breast tumors and compare this to matched primary breast tumor data. This longitudinal analysis has the potential to provide detailed information on tumor evolution under therapy. When coupled with clinical outcomes, the molecular information will help identify biomarkers for prediction of treatment success that can be applied in subsequent trials. Moreover, subsequent translational research conducted using the AURORA biological samples collected at multiple timepoints will identify emergent mechanisms of resistance that can be targeted in subsequent trials. Therefore, the AURORA trial is designed to provide a molecular screening filter to direct metastatic breast cancer patients to clinical trials and thus accelerate the development of promising targeted agents. The Serial Measurements of Molecular and Architectural Responses to Therapy (SMMART) trial (NCT03878524) uses longitudinal biopsies early in the treatment cycle to understand how tumors rapidly adaptive to therapy and then counter the adaptive evolution by selecting appropriate combination therapies. Using deep sequential multi-omics analysis on patient tumors along treatment, SMMART will aid in identifying emergent resistance mechanisms to treatments, and thus support development and implementation of new treatment strategies to tumors that stop responding to therapy. The adaptive multi-drug therapy for evolving cancer (AMTEC NCT03801369) is a subset of SMMART wherein patients are treated for a short time period with monotherapy (olaparib) and deep real-time analytics are used to assess response of tumors to the drug before patients are treated with the combo therapy of olaparib and durvalumab. The goal of AMTEC is to identify and interdict the tumor and ecosystem rewiring that occurs in response to therapy.
The majority of the previously mentioned biomarkers are single-platform based, either in terms of the therapeutic agent or in terms of the analytic platform. Even within a platform (such as genomic analysis), selection criteria is frequently based on aberrations in a single gene. Precision medicine is increasingly requiring that we move towards a systems-based understanding of cancer for therapy choice; our efforts are now beginning to look across genomics, transcriptomics, proteomics, functional screening, and imaging to provide a more holistic picture of tumor aberrations and druggability. Importantly, these studies are beginning to elucidate pathways, networks and states that extend beyond single gene characteristics and more likely reflect the pathophysiology of the tumor and the tumor ecosystem providing approaches to refine therapy choice. This perspective enables us to investigate combination therapies that target both intrinsic and extrinsic aberrations; such as the combination of targeted therapies and immunotherapies.
Beyond single biomarker assays
Traditionally, precision medicine has relied on the presence of a biomarker, or molecular indicator, in a single disease to stratify patients for choice of targeted therapy. However, as mentioned above, there is increasing motivation to move beyond this paradigm. DNA damage repair is emerging as a pan-tumor process that can be used to select patients for particular therapies. Indeed, two pan-tumor genomic events that regulate DNA damage repair have emerged as opportunities to direct therapy. Patients with microsatellite instability (MSI) have a high rate of genomic mutations that are associated with an increased sensitivity to immune checkpoint blockade inhibitors such as antibodies to PDL1 or programmed death 1 (PD1). However, MSI is rare in breast cancer. The second pathway involves defects in homologous recombination most commonly mediated by germline or acquired mutations in the breast cancer associated 1(BRCA1) 1 and breast cancer associated 2 (BRCA2) genes. BRCA1/2 mutations occur in approximately 15% of breast cancers whereas homologous recombination deficiency (HRD) may occur in a similar number of breast cancer without BRCA1/2 mutations. PARP inhibitors, by increasing the number of double strand breaks (DSB) present in cancer cells, were found to be synthetic lethal with aberrations in BRCA1/2 and HRD. Initially approved for BRCA1/2 mutant ovarian cancers, the use of PARP inhibitors has been expanded to breast cancers as well as beyond BRCA1/2 mutant status to include tumors that exhibit HRD signatures at the genomic and transcriptomics level [14, 15]. The HRDetect [14] algorithm assesses both mutational signatures and loss of heterozygosity to determine an HRD “score” for tumors, which indicates a good match (i.e. predicted sensitivity) to PARP inhibitors. Work by Peng, et al. [15] has identified a “PARPness” transcriptomic signature that can also be assessed for the ability to match patients to PARP inhibitors. In this vein, work by McGrail et al. [16] has found transcriptomic signatures of PARPness for PARP inhibitor treatment in breast cancers. Cellular proliferation and in particular dysregulated cell cycle progression can also result in the accumulation of DNA damage known as replication stress. Replication stress may provide a novel signature for drugs targeting DNA damage checkpoints such as inhibitors of WEE1 G2 Checkpoint Kinase (WEE1), Ataxia Telangiesctasia Mutated Serine/Threonine Kinase (ATM), Ataxia Telangiesctasia And Rad3-Related Protein (ATR) and Checkpoint Kinase (CHK) 1/2. Signatures of replication stress are emerging but not yet in use to select patients for particular therapies. Mechanistically, whether defects in DNA damage repair increase mutational load or increase immune activation through DNA damage induced interferon production and subsequent activation of innate immunity remains to be fully elucidated. However, there is strong preclinical and emerging clinical evidence for combination of agents targeting DNA damage repair and immune checkpoint blockade.
The tumor microenvironment (TME) is a key mediator of immunosuppression and immune evasion [17]. For example, the hostile metabolic environment limits nutrient support to T cells as well as exposes T cells to suppressive metabolites that reduce T cell effector function [18]. Chronic activation of T cell receptor signaling can lead to T cell exhaustion, and thus reduces sensitivity to immune checkpoint blockage [19]. Also, the TME composed of heterogeneous cell types contributes to T cell suppression through both direct contact and secretion of soluble factors [20,21,22,23]. Recently, the nervous system has been reported to suppress the anti-tumoral immune response [24, 25]. It is worthwhile to note that tumor cells can directly recruit stromal cells, immune cells and vascular cells to reshape the microenvironment and remodel tissue structure that permit tumor cells to escape from the host immune system as well as promote tumor progression [26]. Ongoing and future efforts on understanding the contribution of TME to immune system regulation will inform trials involved immunotherapy on cancer types in dire need of new therapy.
As we move towards systems-level understanding of tumor biology and response to therapy, we require deep profiling and analytics across data types to guide effective tumor treatment. The Pan-Cancer TCGA effort for breast and gynecological cancers took a systems perspective and provides an assessment across mutation, copy number, expression, and proteomics data; pathway and network analysis across multiple data types identified 5 clinically relevant subgroups [27]. However, while widely touted, the use of multiple assay types is currently not widely adopted [28]; indeed challenges in leveraging multi-omics assays include the need for a team of researchers well-versed across data types, strategies for handling lack of concordance across data types, and performing integrative analysis that enables deep interpretation. Analysis of genomic mutations has the advantage that they are “digital” i.e. present or absent and thus relatively easy to assay and evaluate. There is a continuing challenge in determining which mutations are passengers or drivers and thus targetable, however, the identification of a mutation in tumor DNA has become efficient both within institutions and through outside companies. However, many new and emerging biomarkers are continuous variables, where the analytics require strategic planning with regards to controls, population comparisons, and establishing thresholds and cut-offs.
SMMART clinical trials platform
The Serial Measurements of Molecular and Architectural Responses to Therapy (SMMART) clinical trials platform in the Knight Cancer Institute aims to deeply profile tumor biopsies for metastatic breast cancer patients [29]. The SMMART team is comprised of physicians, cancer biologists, pathologists, genomics experts, and data scientists who provide expertise across multiple assay types and platform. Patients on these clinical trials undergo biopsies that receive extensive Clinical Laboratory Improvement Act (CLIA)-certified assays as well as research assays. CLIA assays are used in clinical tumor boards to enable formal recommendations for treatment options to the treating physician and patient, while research assays are used in research analytics for researching combination drug therapies for future patients [29]. Data on SMMART tumors includes whole exome sequencing (WES), transcriptomics (RNAseq), and proteomics that includes reverse phase protein arrays (RPPA), which assesses approximately 500 targets on bulk tumor lysates, NanoString DSP (digital spatial profiling) which provides regions of interest for approximately 100 proteins in the CLIA environment, cyclic immunofluorescence (cycIF) which provides tumor intrinsic and microenvironment status on 50 proteins with single cell spatial resolution and multiplex IHC (mIHC), which provides spatially-resolved single cell analysis of immune contexture. By taking this multi-assay perspective, the goal is to assess concordance across data types and thereby increase our confidence in tumor aberrations to achieve a more complete picture of tumor pathway signaling to inform treatment decision-making. Overall, the SMMART platform seeks to gain a deep understanding of aggressive and metastatic breast cancers and thereby enable choice of effective precision therapies for each patient.
Limitation of current precision medicine trials
Although master protocol trials accelerate targeted therapy development by assessing multiple drugs and biomarkers simultaneously, the concept of precision medicine is far from being cost-effective, primarily because currently only a small fraction of patients benefit from this treatment strategy [30]. According to a study from MD Anderson Cancer Center, only 6.4% of patients assessed for genomic aberrations ultimately received therapy targeted to their genomic aberrations [31]. The NCI-MATCH trial (NCT02465060) that seeks to determine the effectiveness of treating cancer based on specific genetic changes also showed that only 5.1% (33/645) patients with successful genome profiling were assigned to a matched therapy [32]. Recognizing the need of new therapeutic targets, functional genomics studies which aim to link target and drug [33, 34], have played a critical role, and will continue to support the identification of new biomarkers to guide therapy.
Breast cancer, along with many other cancers, displays a high level of inter- and intra-tumor heterogeneity [35, 36], which remains a major obstacle to successful implementation of precision medicine when the target genes are only expressed in tumor subclones or in the primary tumor but not in distal metastases. Minimizing tumor relapse due to tumor heterogeneity will require advanced sampling methods such as circulating tumor DNA (ctDNA) which has the potential to identify targetable alterations in metastatic tissue that are not sampled by tumor biopsies [37]. In addition, longitudinal tumor sampling including ctDNA during treatment could provide a robust approach to monitoring clonal evolution under therapeutic stress and offer opportunities for new treatments designed to counter clonal expansion.
Conclusion/future directions
Precision medicine has improved the outcome of patients with HER2+ and HR+ breast cancer subtypes, which both harbor targetable vulnerabilities. The first tamoxifen trial in breast cancer, which demonstrated promising results, recruited all types of breast cancer patients disregarding HR status [38, 39]. The importance of HR to tamoxifen sensitivity was recognized afterwards and its true benefit to HR+ breast cancer patients was subsequently revealed. Recent research efforts on cancer immunotherapy and the tumor microenvironment has the potential to be particularly valuable for TNBC where there are no subtype-specific biomarkers for guiding treatment other than mutations in BRCA1/2. Although current immunotherapy trial designs are mostly immune marker-independent, retrospective patient outcome analysis from these trials, advancement in single cell technology such as molecular profiling and tissue imaging, and new immune marker development will inform future trials and eventually enable us to identify patients who will benefit the most from combination cancer immunotherapy. However, even for immunotherapy, it is expected that we will require combinations with traditional chemotherapy, radiation therapy and/or targeted therapy. We await with excitement the evolution of rational biomarker-driven combination therapy that can benefit a greater population of breast cancer patients.
Abbreviations
- AKT1:
-
AKT serine/threonine kinase 1
- ATM:
-
Ataxia telangiesctasia mutated serine/threonine kinase
- ATR:
-
Ataxia telangiesctasia and rad3-related protein
- BRCA1:
-
BRCA1 DNA repair associated
- BRCA2:
-
BRCA2 DNA repair associated
- CHK1:
-
Checkpoint kinase 1
- CHK2:
-
Checkpoint kinase 2
- CLIA:
-
Clinical laboratory improvement act
- ctDNA:
-
Circulating tumor DNA
- ER:
-
Estrogen receptor 1
- HR+:
-
Hormone receptor positive
- HER2:
-
Human epidermal growth factor receptor 2
- MSI:
-
Microsatellite instability
- PARP1:
-
Poly(ADP-Ribose) polymerase
- PTEN:
-
Phosphatase and tensin homolog
- TNBC:
-
Triple negative breast cancer
- WEE1:
-
WEE1 G2 checkpoint kinase
References
Cancer Genome Atlas Network (2012) Comprehensive molecular portraits of human breast tumours. Nature 490(7418):61–70
Nik-Zainal S, Davies H, Staaf J, Ramakrishna M, Glodzik D, Zou X et al (2016) Landscape of somatic mutations in 560 breast cancer whole-genome sequences. Nature 534(7605):47–54
Jiang Y-Z, Ma D, Suo C, Shi J, Xue M, Hu X et al (2019 Mar) Genomic and transcriptomic landscape of triple-negative breast cancers: subtypes and treatment strategies. Cancer Cell 35(3):428-440.e5
Zardavas D, Maetens M, Irrthum A, Goulioti T, Engelen K, Fumagalli D et al (2014 Nov) The AURORA initiative for metastatic breast cancer. Br J Cancer 111(10):1881–7
Brown D, Smeets D, Székely B, Larsimont D, Szász AM, Adnet P-Y et al (2017 Apr 28) Phylogenetic analysis of metastatic progression in breast cancer using somatic mutations and copy number aberrations. Nat Commun 8(1):14944
De Mattos-Arruda L, Sammut S-J, Ross EM, Bashford-Rogers R, Greenstein E, Markus H et al (2019) The genomic and immune landscapes of lethal metastatic breast cancer. Cell Rep 27(9):2690–2708
Moasser MM (2007 Oct 4) The oncogene HER2: its signaling and transforming functions and its role in human cancer pathogenesis. Oncogene 26(45):6469–87
Wilson FR, Coombes ME, Wylie Q, Yurchenko M, Brezden-Masley C, Hutton B et al (2017) Herceptin® (trastuzumab) in HER2-positive early breast cancer: protocol for a systematic review and cumulative network meta-analysis. Syst Rev 6(1):196
Early Breast Cancer Trialists’ Collaborative Group (1988) Effects of adjuvant tamoxifen and of cytotoxic therapy on mortality in early breast cancer. An overview of 61 randomized trials among 28,896 women. N Engl J Med 319(26):1681–1692
Redman MW, Allegra CJ (2015 Oct) The master protocol concept. Semin Oncol 42(5):724–30
Hirakawa A, Asano J, Sato H, Teramukai S (2018 Dec) Master protocol trials in oncology: review and new trial designs. Contemp Clin Trials Commun 12:1–8
Esserman LJ, Berry DA, DeMichele A, Carey L, Davis SE, Buxton M et al (2012) Pathologic complete response predicts recurrence-free survival more effectively by cancer subset: results from the I-SPY 1 TRIAL–CALGB 150007/150012, ACRIN 6657. J Clin Oncol Off J Am Soc Clin Oncol 30(26):3242–9
Barker AD, Sigman CC, Kelloff GJ, Hylton NM, Berry DA, Esserman LJ (2009) I-SPY 2: an adaptive breast cancer trial design in the setting of neoadjuvant chemotherapy. Clin Pharmacol Ther 86(1):97–100
Davies H, Glodzik D, Morganella S, Yates LR, Staaf J, Zou X et al (2017) HRDetect is a predictor of BRCA1 and BRCA2 deficiency based on mutational signatures. Nat Med 23(4):517–25
Peng G, Chun-Jen Lin C, Mo W, Dai H, Park Y-Y, Kim SM et al (2014) Genome-wide transcriptome profiling of homologous recombination DNA repair. Nat Commun 5(1):3361
McGrail DJ, Lin CC-J, Garnett J, Liu Q, Mo W, Dai H et al (2017) Improved prediction of PARP inhibitor response and identification of synergizing agents through use of a novel gene expression signature generation algorithm. Npj Syst Biol Appl 3(1):8
Pitt JM, Vétizou M, Daillère R, Roberti MP, Yamazaki T, Routy B et al (2016) Resistance mechanisms to immune-checkpoint blockade in cancer: tumor-intrinsic and -extrinsic factors. Immunity 44(6):1255–69
Chang C-H, Pearce EL (2016) Emerging concepts of T cell metabolism as a target of immunotherapy. Nat Immunol 17(4):364–8
Pauken KE, Sammons MA, Odorizzi PM, Manne S, Godec J, Khan O et al (2016) Epigenetic stability of exhausted T cells limits durability of reinvigoration by PD-1 blockade. Science 354(6316):1160–5
Haddad R, Saldanha-Araujo F (2014) Mechanisms of T-cell immunosuppression by mesenchymal stromal cells: what do we know so far? BioMed Res Int 2014:216806
Stromnes IM, Greenberg PD, Hingorani SR (2014 Oct 15) Molecular pathways: myeloid complicity in cancer. Clin Cancer Res Off J Am Assoc Cancer Res 20(20):5157–70
Chou CK, Schietinger A, Liggitt HD, Tan X, Funk S, Freeman GJ et al (2012) Cell-intrinsic abrogation of TGF-β signaling delays but does not prevent dysfunction of self/tumor-specific CD8 T cells in a murine model of autochthonous prostate cancer. J Immunol Baltim Md 1950 89(8):3936–3946
Soliman H, Rawal B, Fulp J, Lee J-H, Lopez A, Bui MM et al (2013) Analysis of indoleamine 2–3 dioxygenase (IDO1) expression in breast cancer tissue by immunohistochemistry. Cancer Immunol Immunother CII 62(5):829–37
Kuol N, Stojanovska L, Apostolopoulos V, Nurgali K (2018 Feb) Crosstalk between cancer and the neuro-immune system. J Neuroimmunol 15(315):15–23
Gajewski TF, Schreiber H, Fu Y-X (2013) Innate and adaptive immune cells in the tumor microenvironment. Nat Immunol 14(10):1014–22
Whiteside TL (2008 Oct 6) The tumor microenvironment and its role in promoting tumor growth. Oncogene. 27(45):5904–12
Berger AC, Korkut A, Kanchi RS, Hegde AM, Lenoir W, Liu W et al (2018) A comprehensive pan-cancer molecular study of gynecologic and breast cancers. Cancer Cell 33(4):690-705.e9
Olivier M, Asmis R, Hawkins GA, Howard TD, Cox LA (2019 Sep 26) The need for multi-omics biomarker signatures in precision medicine. Int J Mol Sci 20(19):4781
Mitri ZI, Parmar S, Johnson B, Kolodzie A, Keck JM, Morris M et al (2018) Implementing a comprehensive translational oncology platform: from molecular testing to actionability. J Transl Med 16(1):358
Prasad V (2016) Perspective: the precision-oncology illusion. Nature 537(7619):S63
Meric-Bernstam F, Brusco L, Shaw K, Horombe C, Kopetz S, Davies MA et al (2015) Feasibility of large-scale genomic testing to facilitate enrollment onto genomically matched clinical trials. J Clin Oncol Off J Am Soc Clin Oncol 33(25):2753–62
Flaherty KT, Gray R, Chen A, Li S, Patton D, Hamilton SR et al (2020) The molecular analysis for therapy choice (NCI-MATCH) trial: lessons for genomic trial design. J Natl Cancer Inst 112(10):1021–9
Ng PK-S, Li J, Jeong KJ, Shao S, Chen H, Tsang YH et al (2018) Systematic functional annotation of somatic mutations in cancer. Cancer Cell 33(3):450–462
Tsang YH, Dogruluk T, Tedeschi PM, Wardwell-Ozgo J, Lu H, Espitia M et al (2016) Functional annotation of rare gene aberration drivers of pancreatic cancer. Nat Commun 25(7):10500
Ellsworth RE, Blackburn HL, Shriver CD, Soon-Shiong P, Ellsworth DL (2017) Molecular heterogeneity in breast cancer: State of the science and implications for patient care. Semin Cell Dev Biol 64:65–72
Turashvili G, Brogi E (2017) Tumor heterogeneity in breast cancer. Front Med 4:227
Pectasides E, Stachler MD, Derks S, Liu Y, Maron S, Islam M et al (2018) Genomic heterogeneity as a barrier to precision medicine in gastroesophageal adenocarcinoma. Cancer Discov 8(1):37–48
Ward HW (1973 Jan 6) Anti-oestrogen therapy for breast cancer: a trial of tamoxifen at two dose levels. Br Med J 1(5844):13–4
Lerner HJ, Band PR, Israel L, Leung BS (1976) Phase II study of tamoxifen: report of 74 patients with stage IV breast cancer. Cancer Treat Rep 60(10):1431–5
Author information
Authors and Affiliations
Corresponding author
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Presented at the 8th International Cancer Metastasis Congress in San Francisco, CA, USA from October 25–27, 2019 (http://www.cancermetastasis.org). To be published in an upcoming Special Issue of Clinical and Experimental Metastasis: Novel Frontiers in Cancer Metastasis.
Rights and permissions
About this article
Cite this article
Blucher, A.S., Mills, G.B. & Tsang, Y.H. Precision oncology for breast cancer through clinical trials. Clin Exp Metastasis 39, 71–78 (2022). https://doi.org/10.1007/s10585-021-10092-0
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s10585-021-10092-0