Abstract
The obsessive–compulsive manifestations course was assessed with the Leyton obsessional inventory-child version survey (LOI-CV) in a 3-year prospective study, using a non-clinical sample. From an initial sample of 1,514 school-age children who underwent symptoms screening for obsessive–compulsive, anxiety and depression, 562 subjects (risk group/without risk group) were re-assessed in the 2nd phase and 242 subjects were monitored after 3 years. LOI-CV scores significantly decreased over time independently of age and gender. The prevalence, persistence and incidence for two levels of severity of obsessive–compulsive manifestations ranged between 4.8–30.4 %, 9.3–28.4 % and 1.1–14.4 %, respectively. 34.6–64.5 % of obsessive–compulsive symptomatology was predicted by anxiety, depressive and obsessive–compulsive symptoms. For the obsessiveness (less severe form of obsessive–compulsive manifestations), the depressive symptoms were not predictors. Gender and socioeconomic status were not related with obsessive–compulsive manifestations. These data support a substantial continuity of the obsessive–compulsive manifestations and the existence of different levels of severity within the obsessive–compulsive spectrum.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
It is commonly known that obsessive–compulsive disorder (OCD) in children and adolescents has been little studied in the past and may have been under-diagnosed and under-treated. OCD occurs either as the full-blown disorder, in the form of subclinical OCD or as obsessive–compulsive (OC) symptoms. In fact, several studies have used case definitions for different severity levels of the OC manifestations [1, 2]. Some epidemiological studies have demonstrated that children and adolescents often present with some form of OCD from the OCD spectrum and that it has an early age of onset [3, 4]. The prevalence of OCD from childhood to the end of adolescence ranges from 0.1 to 4 % [5–7]. Specifically, an OCD prevalence of 1.8 % was found in a Spanish non-clinical sample of school children [1]. For subclinical OCD and OC symptomatology, the rates are larger and range from 2.7 to 19 % [1, 3, 8].
Most authors regard OCD as a chronic disorder that interferes in the daily lives of the subjects and that presents high persistence rates throughout a person’s life, especially if left untreated [9–11]. Eisen et al. [12] conducted a prospective clinical study in which they suggested that full remission was rare, whereas Palermo et al. [13] showed that a large frequency of children with OCD experience remission by early adulthood. Therefore, can OCD be considered a chronic condition? Are the OC symptoms in childhood evolutionary manifestations? How persistent is the disorder?
Other studies have investigated the relationship between OC symptoms and psychopathological or socio-demographic factors and data are somewhat inconsistent. As for gender, generally females reported significantly more symptoms and interference than males [3, 14]; although at early ages several authors have reported a slight male predominance [4, 15]. In this regard, Ruscio et al. [16] stated that nearly one quarter of boys experienced the onset of the disorder before the age of 10, whereas girls usually experienced the onset of OCD after the age of 10. Moreover, Geller [15] conducted an extensive study which compared specific OC manifestations across different age groups and found several differences between children, adolescents and adults in the frequency of particular obsessions and compulsions; children and adolescents had much higher rates of aggressive/harm obsessions than adults. Likewise, religious obsessions were over-represented in adolescents, and sexual obsessions were less frequent in children compared with adolescents and adults. In terms of compulsions, both Geller [15] and Nikolajsen et al. [11] found that only hoarding was more prevalent in children and adolescents than in adults. The results are at odds concerning the relationship between other socio-demographic variables and OC manifestations. The review by Fontenelle and Hasler [17] found that some authors observed OC symptoms in subjects had been raised in significantly higher social classes [18], whereas others such as Heyman et al. [19] reported a trend for higher rates of OCD in lower socioeconomic groups. The situation is similar for educational level. While some authors have suggested that subjects with OCD show significant impairment in their academic life [20] others have found that OCD is more common among individuals with higher educational levels [21]. In adults, Grabe et al. [22] found higher prevalence rates of OCD among subjects who were unemployed, and that subjects with OCD are less likely to be married. There is still controversy regarding the role of race-ethnicity as a predisposition factor for developing OCD; some studies have found that the black ethnic identity can have a protective role [23], whereas others have been unable to find differences in prevalence of OCD between different ethnical groups [24].
Subjects with OC manifestations are at risk of presenting higher rates of comorbidity with other psychiatric conditions [25, 26]. Thus, some authors have found that OCD and depressive disorders co-occur frequently in both adults and children [1, 27], thus suggesting that depression was a product of the OC symptoms [28]. Moreover, children with autism spectrum disorders have shown increased rates of OC manifestations [29] and conversely, paediatric OCD patients have shown increased frequencies of autism spectrum symptoms [30]. Furthermore, several authors have found higher frequencies of comorbid tic disorders, disruptive behaviour disorders and attention deficit hyperactivity disorder (ADHD) in children with OCD [27, 31]. It is important to study the possible correlates between OCD and other psychiatric conditions because the two conditions may need separate treatment, for example when OCD is presented with ADHD [15]. On the other hand, some authors have suggested that OCD with comorbid ADHD could be a specific subgroup of OCD patients whose condition follows a more homogeneous course [32].
Another issue is that sometimes shame associated with the disorder may inhibit people from disclosing the symptoms, thus delaying detection, diagnosis and treatment. Affected people are often reluctant to reveal symptoms, particularly if the symptoms are perceived as embarrassing. For this reason screening tools are needed. As other authors, we also consider that the Leyton obsessional inventory-child version (LOI-CV) [33] has important advantages in that it is brief, simple and self-reporting and, having evaluated the properties of the LOI-CV in our sample, we conclude that it is a reliable and valid instrument for detecting OCD in children from a non-clinical population [34, 35].
After reviewing the existing literature, we observed that only a few prospective studies had used community samples of early adolescents to clarify the course that OCD takes when it begins at early ages. Consequently, we decided to prospectively examine the clinical course of OC manifestations in a longitudinal epidemiological study with the main aims of: (1) exploring the relationships between the LOI-CV scores and socio-demographic variables in the 3 periods of the follow-up; (2) studying the evolution of the LOI-CV total and the factors scores throughout the follow-up, controlling for age and gender; (3) determining the course taken by the OC manifestations by estimating its prevalence, persistence, recurrence, and incidence at two levels of severity (obsessiveness and OC symptomatology); (4) exploring the predictive psychopathological factors of the two severity levels of OC manifestations at the end of the study. Taking all the above into account, we first hypothesized that, as LOI-CV scores suggest, OC manifestations vary according to gender, age and other socio-demographic characteristics. We also hypothesized that the rates of persistence and recurrence of OC are considerable, which means that it is present throughout development, and that manifestations are related to previous anxiety, depression, and OC symptoms.
Method
Participants
2,023 4th, 5th and 6th grade students from thirteen primary schools (7 state schools and 6 state-subsidized private schools) in Reus (a medium-sized Spanish town of 100,000 habitants) were invited to participate in an epidemiological study of anxiety and depression disorders. The study was conducted in three-phases. 1,514 students participated in the 1st phase (720 boys and 794 girls) between 8 and 12 years of age (mean = 10.23; SD = 1.23). A total of 39.5 % of the children belonged to families of a low socioeconomic status (SES), 42.5 % to families of medium SES and 18 % to families of high SES. 87.5 % of the sample was born in Spain, and 85.9 % belonged to a nuclear family. Once we had screened the 1st phase, 562 students (254 boys and 308 girls) of mean age 11.25 (SD = 1.04) were selected to participate in the 2nd phase as subjects at risk of OCD (41.8 %) or as members of a control group without risk (58.2 %). There were no significant differences between risk and control group subjects for gender (χ2 = .132, p = .716), birthplace (χ2 = .075, p = .784), family type (χ2 = .227, p = .634), SES (χ2 = 1.306, p = .520) and age (t = .947, p = .344). Two years later all 562 subjects were invited to participate in the 3rd phase follow-up and 242 subjects (95 boys and 147 girls) (mean age was 13.52, SD = .94) participated. There were no emotional and socio-demographic differences between subjects who participated in the 3rd phase and subjects who dropped out in this last step of the study. However there were differences related to the SES factor: low SES participants were associated with higher dropout rates than were medium or high SES participants (χ 22.561 = 13.557; p = .001).
Instruments
Leyton obsessional inventory-child version survey (LOI-CV) [33] is a self-reported 20-item questionnaire asking about the presence or absence (described in the item Yes/No) of a number of obsessive preoccupations and behaviours, including, for each positive response, a rating of interference with personal functioning (range 0–3, no interference-interferes a lot). LOI-CV has been proven to be a valid screening instrument for assessing OCD or OC symptoms in children and adolescents [34]. Despite the fact that over the years several questionnaires have been published for assessing OC symptoms in children, some of which derive from adult assessment instruments [36–38], we nevertheless chose the LOI-CV because, when we began the present study, the LOI-CV was the most widely used instrument in Spanish clinical samples and in any case no other questionnaires for screening OC symptoms had been adapted for use in Spain. We found that the best factorial structure was a model using three factors; these three factors explained 46.30 % of the variance. The factors were the following: order/checking/pollution, obsessive concern, and superstition/mental compulsion (30.15, 8.53 and 7.62 % of the variance, respectively). Total reliability was good (α = .78) [34]. In this study, we considered two types of LOI-CV scores: the interference score, which is the sum of the interferences regardless of the “yes” responses; and the total score, which is the sum of the “yes” score plus the interference scores. We also established two levels of severity for OC manifestations: (1) we defined an interference score of 25 or above as indicative of OC symptomatology, a cut-off point that was proposed by the author of the questionnaire [33] and that has been used by other authors [3, 14]; (2) on the basis of data obtained by Canals et al. [34] we used the total score of 21 as the cut-off point to define a less severe category for the OC manifestations, and we called this obsessiveness.
Youth’s inventory-4 (YI-4) [39] is a self-report rating scale of 120 items that evaluates DSM-IV symptoms of emotional and behaviour disorders in youths between 12–18 years old. To obtain our results we took into account nine symptom categories from this instrument, corresponding to nine types of disorders: ADHD, conduct disorders, tic disorders, eating disorders, depression, bipolar disorder, schizophrenia, schizoid personality, and substance use. The YI-4 demonstrated satisfactory internal consistency (α = .95).
Screen for childhood anxiety and related emotional disorders (SCARED) [40] is a self-report questionnaire that assesses anxiety disorder symptoms in children and adolescents from 8 to 18 years old. The scale is composed of 41 items and children were asked the frequency of each symptom on a 3-point-scale: 0 (almost never), 1 (sometimes), 2 (often). The internal consistency of the Spanish version was good (α = .86) [41]. A score of 32 was considered to be the cut-off point for risk of anxiety. Given that in Spain the cut-off has not been validated, this score corresponded to percentile 75 of our sample, the same percentile used by Birmaher et al. [42] in a sample of outpatients from the USA.
Children’s depression inventory (CDI) [43] is a 27-item self-report symptom-oriented scale suitable for youths aged 7–17. The CDI is sensitive to changes in depressive symptoms over time and is a useful index of the severity of the depressive syndrome. The Spanish version demonstrated good internal consistency in community and clinical samples (α = .81–.85) [44]. A score of 17 was considered as the cut-off point for risk of depression [45].
Socio-demographic characteristics of the sample were collected at baseline with a questionnaire designed for this study by the authors. The children answered questions about age, gender, place and date of birth, family type and occupation of parents. This information was corroborated by the parents. The SES was established by the Hollingshead index [46]. This index allows the social status of each individual to be determined by categorizing his or her occupation into one of nine categories (from unskilled work to highly skilled work) and his or her level of education into one of seven categories (from non-completed primary education to completed higher education). The status score is estimated by multiplying the occupation scale value by a weight of five and the education scale value by a weight of three and then combining the two scores. We thus determined family SES on a scale from 0 to 66. This gave us three categories (low, medium and high) we considered scores lower than 22 to be low SES, scores between 23 and 44 to be medium, and over 44 to be high.
Academic performance was assessed by a questionnaire designed for this study by the authors. It was answered by teachers at the 2nd phase and by parents at the 3rd phase.
Procedure
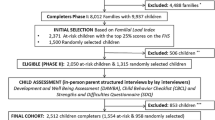
This is a prospective longitudinal study with three phases. Following approval from the Department of Education of the Catalan Government, we selected a representative sample of subjects. Cluster sampling was conducted by randomly selecting a set of 13 schools (7 state schools and 6 state-subsidized private schools) from a total of 26 schools from all five representative areas of Reus (Spain). We then contacted the 13 school boards, all of whom agreed to participate. After that, we sent all parents a letter to inform them about the study and to ask for their written informed consent. The 1st phase took place during the 2006/2007 academic year with a representative sample of school-age subjects (subjects in 4th, 5th and 6th primary grades). The 2nd phase (2007/2008 academic year) took place during the following academic year and the 3rd during the 2009/2010 academic year. Participants in the 1st phase were administered screening tests for anxiety symptoms (SCARED), depressive symptoms (CDI) and obsessive–compulsive disorder symptoms (LOI-CV) and were assessed on the basis of their socio-demographic data. This data was collected using a questionnaire designed for this study in which children were asked about their parents’ jobs, family structure and other socio-demographic variables. Over the following academic year, in the 2nd phase of the study, a subsample was selected formed by subjects at risk of mood and anxiety disorders according to their cut-off scores in the screening tests (SCARED, CDI and/or LOI-CV). Additionally, we selected controls with the same age and gender characteristics, but without risk scores on any test. In the 2nd phase the SCARED, CDI and LOI-CV were re-administered to the children and teachers answered questions about academic performance. Finally in the 3rd phase we invited all subjects of the 2nd phase to participate and conducted a retest with the SCARED and the LOI-CV. We also administered the YI-4 in order to evaluate psychopathology. Parents also informed about the academic performance of their children. The participants completed the questionnaires in small groups of three or four and the investigators were present to instruct the children on how to answer the surveys. Figure 1 summarizes the study design and the sample recruitment.
Data Analysis
A series of statistical analyses were performed using SPSS software version 19.0.
The Chi square statistical test was used to study possible socio-demographic differences between the risk-group and the control-group subjects, and also between the subjects who participated in the 3rd phase and those who dropped out in the last phase of the study.
t Test analyses were used to find possible differences between two independent groups, and ANOVA was used to find possible differences between three independent groups. In particular, t test analyses were used to assess the relationship between various socio-demographic variables—gender: boys/girls; birthplace: foreign/native; family type: single parent/nuclear; and academic performance: low/high—and LOI-CV total and factor scores. ANOVA was used to test the possible relation between SES (high, medium or low), and LOI-CV total and factor scores. T test analyses and ANOVA were performed for each phase of the study.
Repeated-measures MANOVA (controlling for age and gender) was used to examine the evolution of the LOI-CV total and factor scores, over the three phases among the subjects who participated.
In order to observe the predictors of the OC manifestations (obsessiveness and OC symptomatology) in the 3rd phase, logistic regression models using the stepwise method, were performed. Both regression models were performed in three steps. The candidate variables entered into the model in the first step were: psychopathological variables of the 1st phase (LOI-CV factors scores, SCARED factors scores, and CDI total score) and socio-demographic variables such as gender and age. In the second step we added to the candidate variables of the first step: psychopathological variables of the 2nd phase (LOI-CV factors scores, SCARED factors scores, and CDI total score). In the third step we added the SCARED factors scores of the 3rd phase and the scores of the nine YI-4’s categories. We adjusted the model for SES because there were significant differences between the subjects who participated in the last phase of the study and the subjects who declined to participate. Before performing the regression models, collinearity between the variables was assessed and analyses show that the LOI-CV total score was collinear with LOI-CV factors scores, and the SCARED total score was also collinear with the SCARED factors scores, so we selected the LOI-CV and the SCARED factors scores instead of the total scores.
Bonferroni correction was applied to control the increase in type I error caused by multiple comparisons, which meant that we used a significance level of .01.
Results
Descriptive Data of the LOI-CV Scores for the Socio-Demographic Variables per Phase of the Study
t Test analyses only showed some trends. Females obtained higher scores for order/checking/pollution factor (mean score = 7.33, SD = 5.4) than males (mean score = 6.76, SD = 5.2) (t = −2.08, p = .037), whereas males obtained higher scores for superstition/mental compulsion factor (mean score = 2.65; SD = 3.4) than females (mean score = 2.31, SD = 3.0) (t = 1.99, p = .046). Results also showed that subjects with single-parent families obtained higher scores (mean score = 2.94, SD = 3.8) than subjects with nuclear families (mean scores = 2.39, SD = 3.1) for superstition/mental compulsion factor (t = 2.03, p = .044). In the 3rd phase subjects with lower academic performance tended to obtain higher total scores on the LOI-CV (mean score = 17.78, SD = 12.3) than subjects with higher academic performance (mean score = 13.45, SD = 9.38) (t = −1.97, p = .05).
The ANOVA showed significant differences in the 1st phase of the study. Thus, LOI-CV scores were found to be inversely related to SES for order/checking/pollution (F = 7.54, p = .001) and superstition/mental compulsion factors (F = 8.37, p = .0001), and total score (F = 7.62, p = .001).
Clinical and Epidemiological Evolution of the OC Manifestations
Repeated-measures MANOVA showed that scores for the LOI-CV (factors and total) significantly decreased over time independently of age and gender (Table 1).
For the two levels of severity of the OC manifestations (obsessiveness and the OC symptomatology) we obtained an obsessiveness prevalence of 30.4 % (95 % CI 28.4–33.1, N = 459) with no differences between boys and girls. The prevalence of the OC symptomatology was 4.8 % (95 % CI 3.7–5.9, N = 71) [1] and also no significant differences were found in terms of gender.
Table 2 shows the persistence, recurrence and incidence of the two levels of OC manifestations at different points during the follow-up. When subjects obtained scores above the cut-off point in the 1st phase of the study and also in the 2nd phase, we regarded this as the persistence rate over 1 year; and when subjects obtained scores above the cut-off point in the 1st phase, in the 2nd phase and also in the 3rd phase, we regarded this as the persistence rate over 3 years. When a subject obtained a score above the cut-off point in the 1st phase and in the 3rd phase of the study, but not in the 2nd phase, we regarded this as the recurrence rate. When subjects obtained a score below the cut-off point in the 1st phase and above the cut-off point in the 2nd phase we regarded this as annual incidence rate; and when subjects only scored above the cut-off point in the 3rd phase of the study and not in the 1st and in the 2nd phase we regarded this as the incidence rate over 3 years.
Predictive Factors of the Two Types of OC Manifestations
To predict the obsessiveness in the 3rd phase (see Table 3), in step 1 we entered the psychopathological variables collected in the 1st phase (LOI-CV factors scores, SCARED factors scores and CDI total scores) and gender and age of subjects. We observed that separation anxiety factor of the SCARED was a good predictor and that the model explained 8.6 % of the obsessiveness. In the second step we added the psychopathological variables collected in the 2nd phase and the scores on order/checking/pollution factor and the scores on the superstition/mental compulsion factor were the best predictors. This model explained 33.1 % of the obsessiveness. Finally when we added the psychopathological variables collected in the last phase of the study to the candidate variables of the previous steps, the best predictors were the scores for the order/checking/pollution factor of the 2nd phase LOI-CV, the social phobia scores obtained in the SCARED of the 2nd and 3rd phase, and also the separation anxiety factor of the 3rd phase SCARED. These variables and the score of the schizoid personality disorder obtained from the YI-4 explained 53.3 % of the obsessiveness.
The results showed that in the first step the best predictors for OC symptomatology in the 3rd phase were separation anxiety factor and order/checking/pollution factor, and the model explained 34.6 % of the OC symptomatology. In the second step when we added the variables collected in the 2nd phase we observed that the best predictors were superstition/mental compulsion and the score of the CDI, both from the 2nd phase. The model explained a 64.5 % of the OC symptomatology. Finally in the last step we found that the best predictors were again the superstition/mental compulsion factor and the CDI total score of the 2nd phase. The model explained a 61.9 % of the OC symptomatology.
Discussion
This study used the LOI-CV to examine prospectively the OC manifestations in a school age community sample.
Statistical trends have been found for the relationship between the scores on the LOI-CV and some socio-demographic variables in each phase of the study, and these could be due to the sample sizes. Consequently, children who came from environments where the SES was lower had higher scores on the LOI-CV. These differences were significant in the 1st phase due probably to the large sample size. The present results support those of Heyman et al. [19], but do not coincide with data from Degonda et al. [18], who concluded that individuals with OC symptoms were raised in significantly higher social classes than controls. On the other hand, in contrast with Van Oort et al. [47] we did not find that SES was a risk indicator. As for the other socio-demographic variables, the data did not support our hypothesis, which indicates that OC manifestations could be relatively independent of socio-cultural features.
It has been reported that there are some inconsistent results regarding the age variable; while some studies note that older subjects present more OC symptoms [19, 48] other studies such as the one by Zohar and Bruno [49] have found the opposite result. Similarly our results reflect a general decrease of the LOI-CV scores over the three phases. We found that this decrease over time was not related to the sex of the participants and was also independent of the subjects’ age at the beginning of the study. These results suggest some interpretations; for example the decrease in the scores may be because OC manifestations decrease with age. Likewise, there may be methodological reasons that would mean that younger subjects would be more likely to exaggerate the severity of their symptoms in the questionnaire, or that the answers in the retest may be attenuated, although this possible statistical effect is taken into account by the repeated measures MANOVA.
We did not find any significant differences between genders in the LOI-CV total scores in any phase of the study nor in obsessiveness and OC symptomatology prevalence. Our data does not support those of other studies of non-clinical samples that reported more symptoms and interference in females than in males [3, 14]. Also the present results did not support those from clinical samples that indicate a certain propensity towards OCD in adult women and in male children and adolescents [50, 51]. However, some gender differences in clinical manifestations were observed; that is, superstition/mental compulsion symptoms were found more often in males whereas females obtained higher scores for the order/checking/pollution factor. Similarly, Maggini et al. [14] found a certain preponderance of males in items related to superstition symptomatology. The superstition/mental compulsion factor was also a predictor of the obsessiveness and OC symptomatology over the long term. Consequently, we suggest that it is important to take into account symptoms related to superstition because although it may be a manifestation that can go unnoticed or be considered milder, we have shown that it is closely related to the subclinical diagnosis of OCD [52].
The association between early anxiety and the OC manifestations might support the comorbid relationships among these symptoms; specifically the most significant anxiety manifestations were separation anxiety and social phobia. In this regard, Angst et al. [53] found that in adults the prevalence of OCD was significantly increased if the subject also had social phobia and the recent study of Assunçao et al. [54] also found higher rates of comorbidity between OCD and social phobia. Furthermore, in this early developmental stage, one of the most frequent disorders is the separation anxiety; indeed, Mroczkowski et al. [55] stated that this disorder has been shown to have a clear influence on the course of OCD, which may even mean that it is difficult to distinguish the symptomatology qualities of one from the other. In our data, separation anxiety appeared as a predictor for the two severity levels of OCD, which indicates that anxiety symptomatology may be a pre-existing feature in OCD development. In this regard, in the recent study by Jakubovski et al. [56] the OCD presented a worse prognosis when there was a family history of anxiety disorders. The data presented have also shown a relation between depression and OC symptomatology, as is the case in other studies [1, 28]. This predictive relation was observed for the severest category of OC (OC symptomatology and not for obsessiveness) which suggests that depression symptoms are due to the distress caused by the day-to-day impairment of the obsessions and compulsions in children’s lives, as shown in previous studies [57]. Likewise, the results have shown a significant and positive relation between the schizoid personality disorder symptoms and obsessiveness, probably because in many cases it would be difficult to make a distinction between obsessions and delusions, as was observed Joo [58].
Results of persistence and incidence were hardly comparable to those of other studies because the design and the methodology are very different. Despite this, we did not find low rates of incidence as is the case in other studies [59, 60]. Our data have shown significant rates of incidence that we believe show the emergence of new cases in the age period studied. Moreover, although data show a significant pattern of symptom quantitative reduction over time, the rates of persistence both for obsessiveness and for OC symptomatology (around 30 %), indicate that OCD presents continuity over time within a clinical spectrum and therefore could be chronic in the long term for some cases, as we hypothesized. Also, for recurrence our findings showed high rates demonstrating that within the chronicity, the OCD can be fluctuating or episodic [10, 61]. Furthermore, the results relate to persistence rates in the two levels of severity and the predictors support the importance of taking into account the two LOI-CV cut-off points. In addition, our data were consistent with those from the meta-analysis by Stewart et al. [62] in that rates of persistence for full OCD ranged from 13 to 87 % and for subclinical OCD ranged from 17 to 46 %. Heyman et al. [63] also found that many adults recognized that the symptoms began in childhood and adolescence and Jakubovski et al. [56] found a worse prognosis associated with an earlier age of OCD onset.
This work has certain limitations that should not be overlooked. One limitation is the use of self-informant questionnaires, which runs the risk of responders misunderstanding some questions, or of having poor or limited insight into their condition. It is common in OCD cases for subjects and especially young subjects not to recognize their obsessions or compulsions as excessive or unreasonable [64]. Another limitation is that the study did not control for whether the subjects had been treated in any of the three phases, and this may interfere in the interpretation of the results obtained by the repeated-measures MANOVA. Thirdly, the major limitation is that despite the efforts of the researchers, the study suffered from reduced parental consent in the last phase. However, no differences were found between the emotional and the socio-demographic characteristics of subjects who participated and those who did not, and SES differences were controlled in the regression models. Despite these limitations, we have obtained data from a large sample followed-up at three key points in the early adolescence period and the findings indicate continuous OC manifestations and the possible occurrence of new cases during this period. The chronic evolution of the OC manifestations shows that they present recurrences and fluctuations in their level of severity, which supports the OCD spectrum. In this regard, the two levels of severity of OC manifestations were predicted by factors such as previous anxiety, previous OC manifestations or depressive symptomatology. Specifically, the less severe form of OC (obsessiveness) was related more to anxiety symptoms and OC symptoms, whereas the more severe form of OC (OC symptomatology) was related more to previous OC manifestations and depressive symptoms. We think that more prospective and large follow-up studies need to be carried out to support to the data presented.
Summary
In this study we aimed to explore prospectively the clinical course of OC manifestations using the LOI-CV. The questionnaire was administered to a non-clinical sample of school-age children at three points in their development. From an initial sample of 1,514 subjects (aged between 8 and 12) who underwent symptoms screening for OCD (LOI-CV), anxiety (SCARED) and depression (CDI), 562 subjects (risk group and without risk group) were re-assessed in the 2nd phase (1st phase, 2006/2007 academic year; 2nd phase, 2007/2008 academic year). 242 subjects were monitored at 3 years (3rd phase, 2009/2010 academic year). Relationships between the LOI-CV scores and socio-demographic factors were explored as well as the evolution of the LOI-CV scores over the three phases. LOI-CV scores significantly decreased over time independently of age and gender. On the other hand, we did not observe conclusive results for the association between socio-demographic variables and OC manifestations. The prevalence, persistence and incidence for two levels of severity of OC manifestations (obsessiveness and OC symptomatology) ranged between 4.8 and 30.4 %, 9.3 and 28.4 % and between 1.1 and 14.4 %, respectively. Also, 15.8 % of OC symptomatology and 21.6 % of obsessiveness presented remission and subsequent recurrence. Logistic regression models showed that between 34.6 and 64.5 % of OC symptomatology was predicted by previous OC symptoms and previous anxiety and depressive symptoms. For the obsessiveness, the depressive symptoms were not significant predictors. Our data support a substantial continuity of the OC manifestations during the period studied and the existence of different levels of severity within the OCD spectrum. We suggest that early recognition of anxiety, depression and OC symptoms may help to prevent chronicity and worse prognosis of OCD.
References
Canals J, Hernández-Martínez C, Cosi S, Voltas N (2012) The epidemiology of obsessive-compulsive disorder in Spanish school children. J Anxiety Disord 26:746–752
Roussos A, Francis K, Koumoula A, Richardson C, Kabakos C, Kiriakidou T et al (2003) The Leyton obsessional inventory-child version in Greek adolescents: standardization in a national school-based survey and two-year follow-up. Eur Child Adolesc Psychiatry 12:58–66
Brynska A, Wolanczyk T (2005) Epidemiology and phenomenology of obsessive-compulsive disorder in non-referred young adolescents. A polish perspective. Eur Child Adolesc Psychiatry 14:319–327
Mancebo MC, Garcia AM, Pinto AM, Freeman JB, Przeworski A, Stout R et al (2008) Juvenile-onset OCD: clinical features in children, adolescents and adults. Acta Psychiatr Scand 118:149–159
Carter AS, Wagmiller RJ, Gray SA, McCarthy KJ, Horwitz SM, Briggs-Gowan MJ (2010) Prevalence of DSM-IV disorder in a representative, healthy birth cohort at school entry: sociodemographic risks and social adaptation. J Am Acad Child Adolesc Psychiatry 49:686–698
Douglass HM, Moffit TE, Dar R, McGee R, Silva P (1995) Obsessive-compulsive disorder in a birth cohort of 18-years-olds: prevalence and predictors. J Am Acad Child Adolesc Psychiatry 34:1424–1431
Lewinsohn PM, Hops H, Roberts RE, Seeley JR, Andrews JA (1993) Adolescent psychopathology: I. Prevalence and incidence of depression and other DSM-III-R disorders in high school students. J Abnorm Psychol 102:133–144
Valleni-Basile LA, Garrison CZ, Waller JL, Addy CL, McKeown RE, Jackson KL et al (1994) Frequency of obsessive-compulsive disorder in a community sample of young adolescents. J Am Acad Child Adolesc Psychiatry 33:782–791
Abramowitz JS, Taylor S, McKay D (2009) Obsessive-compulsive disorder. Lancet 374:491–499
Micali N, Heyman I, Perez M, Hilton K, Nakatani E, Turner C et al (2010) Long-term outcomes of obsessive-compulsive disorder: follow-up of 142 children and adolescents. Br J Psychiatry 197:128–134
Nikolajsen KH, Nissen JB, Thomsen PH (2010) Obsessive-compulsive disorder in children and adolescents. Symptom dimensions in naturalistic setting. Nord J Psychiatry 65:244–250
Eisen JL, Pinto A, Mancebo MC, Dyck I, Orlando ME, Rasmussen SA (2010) A 2-year follow-up study of the course of obsessive-compulsive disorder. J Clin Psychiatry 71:1033–1039
Palermo S, Bloch M, Craiglow B, Landeros-Weisenberger A, Dombrowski P, Panza K et al (2011) Predictors of early adulthood quality of life in children with obsessive-compulsive disorder. Soc Psychiatry Psychiatr Epidemiol 46:291–297
Maggini C, Ampollini P, Gariboldi S, Cella PL, Peqlizza L, Marchesi C (2001) The parma high school epidemiological survey: obsessive-compulsive symptoms. Acta Psychiatr Scand 103:441–446
Geller DA (2006) Obsessive-compulsive and spectrum disorders in children and adolescents. Psychiatr Clin N Am 29:353–370
Ruscio AM, Stein DJ, Chiu WT, Kessler RC (2010) The epidemiology of obsessive-compulsive disorder in the National Comorbidity Survey Replication. Mol Psychiatry 15:53–63
Fontenelle LF, Hasler G (2008) The analytical epidemiology of obsessive-compulsive disorder: risk factors and correlates. Progr Neuropsychopharmacol Biol Psychiatry 32:1–15
Degonda M, Wyss M, Angst J (1993) The Zurich study XVIII. Obsessive-compulsive disorders and syndromes in the general population. Eur Arch Psychiatry Clin Neurosci 243:16–22
Heyman I, Fombonne F, Simmons H, Ford T, Meltzer H, Goodman R (2001) Prevalence of obsessive-compulsive disorder in the British nationwide survey of child mental Health. Br J Psychiatry 179:324–329
Piacentini J, Bergman RL, Keller M, McCracken J (2003) Functional impairment in children and adolescents with obsessive-compulsive disorder. J Child Adolesc Psychopharmacol 13:61–69
Mohammadi MR, Ghanizadeh A, Rahgozar M, Noorbala AA, Davidian H, Afzali HM et al (2004) Prevalence of obsessive-compulsive disorder in Iran. BMC Psychiatry 4:2
Grabe HJ, Meyer C, Hapke U, Rumpf HJ, Freyberger H, Dilling H et al (2000) Prevalence, quality of life and psychosocial function in obsessive-compulsive disorder and subclinical obsessive-compulsive disorder in northern Germany. Eur Arch Psychiatry Clin Neurosci 250:262–268
Karno M, Golding JM, Sorenson SB, Burnam MA (1988) The epidemiology of obsessive-compulsive disorder in five US communities. Arch Gen Psychiatry 45:1094–1099
Breslau J, Aguilar-Gaxiola S, Kendler KS, Su M, Williams D, Kessler RC (2006) Specifying race-ethnic differences in risk for psychiatric disorder in a USA national sample. Psychol Med 36:57–68
Marcks BA, Weisberg RB, Dyck I, Keller MB (2011) Longitudinal course of obsessive-compulsive disorder in patients with anxiety disorders: a 15-year prospective follow-up study. Compr Psychiatry 52:670–677
Walitza S, Melfsen S, Jans T, Zellmann H (2011) Obsessive-compulsive disorder in children and adolescents. Dtsch Arztebl Int 108:173–179
Helbing ML, Ficca M (2009) Obsessive-compulsive disorder in school-age children. J Sch Nurs 25:15–26
Storch EA, Lewin AB, Larson MJ, Geffken GR, Murphy TK, Geller DA (2012) Depression in youth with obsessive-compulsive disorder: clinical phenomenology and correlates. Psychiatry Res 196:693–699
Leyfer OT, Folstein SE, Bacalman S, Davis NO, Dinh E, Morgan J et al (2006) Comorbid psychiatric disorders in children with autism: Interview development and rates of disorders. J Autism Dev Disord 36:849–861
Ivarsson T, Melin K (2008) Autism spectrum traits in children and adolescents with obsessive-compulsive disorder (OCD). J Anxiety Disord 22:969–978
Masi MG, Millepiedi S, Perugi G, Pfanner C, Berloffa S, Pari C et al (2010) A naturalistic exploratory study of the impact of demographic, phenotypic and comorbid features in pediatric obsessive-compulsive disorder. Psychopathology 43:69–78
Masi G, Millepiedi S, Mucci M, Bertini N, Pfanner C, Arcangeli F (2006) Comorbidity of obsessive-compulsive disorder and attention-deficit/hyperactivity disorder in referred children and adolescents. Compr Psychiatry 47:42–47
Berg CZ, Whitaker A, Davies M, Flament MF, Rapoport JL (1988) The survey form of the Leyton obsessional inventory child version: norms from an epidemiological study. J Am Acad Child Adolesc Psychiatry 27:759–763
Canals J, Hernández-Martínez C, Cosi S, Lázaro L, Toro J (2012) The Leyton obsessional inventory-child version: validity and reliability in Spanish non-clinical population. Int J Clin Health Psychol 12:81–96
Grabill K, Merlo L, Duke D, Hardford KL, Keeley ML, Geffken GR et al (2008) Assessment of obsessive-compulsive disorder: a review. J Anxiety Disord 22:1–17
Storch EA, Khanna M, Merlo LJ, Loew B, Franklin M, Reid JM et al (2009) Children’s Florida obsessive compulsive inventory: psychometric properties and feasibility of a self-report measure of obsessive-compulsive symptoms in youth. Child Psychiatry Hum Dev 40:467–483
Storch EA, Muroff J, Lewin AB, Geller D, Ross A, McCarthy K et al (2011) Development and preliminary psychometric evaluation of the children’s saving inventory. Child Psychiatry Hum Dev 42:166–182
Foa EB, Coles M, Huppert JD, Pasupuleti RV, Franklin ME, March J (2010) Development and validation of child version of the obsessive compulsive inventory. Behav Ther 41:121–132
Gadow K, Sprafkin J (1999) Youth’s inventory-4 manual. Checkmate Plus, Ltd, Stony Brook, NY
Birmaher B, Khetarpal S, Brent D, Cully M, Balach L, Kaufman J et al (1997) The screen for child anxiety related emotional disorders (SCARED): scale construction and psychometric characteristics. J Am Acad Child Adolesc Psychiatry 36:545–553
Vigil-Colet A, Canals J, Cosi S, Lorenzo-Seva U, Ferrando PJ, Hernández-Martínez C et al (2009) The factorial structure of the 41-item versión of the screen for child anxiety related emotional disorders (SCARED) in a Spanish population of 8 to 12 years-old. Int J Clin Health Psychol 9:313–327
Birmaher B, Brent DA, Chiappetta L, Bridge J, Monga S, Baugher M (1999) Psychometric properties of the screen for child anxiety related emotional disorders (SCARED): a replication study. J Am Acad Child Adolesc Psychiatry 38:1230–1236
Kovacs M (1992) Manual for the children’s depression inventory. Multi-Health Systems, North Tonawanda
Figueras A, Amador-Campos JA, Gómez-Benito J, del Barrio V (2010) Psychometric properties of the children’s depression inventory in community and clinical sample. Span J Psychol 13:990–999
Canals J, Martí-Henneberg C, Fernández-Ballart J, Domènech E (1995) A longitudinal study of depression in urban Spanish puberal population. Eur Child Adolesc Psychiatry 4:102–111
Hollingshead AB (2011) Four factor index of social status. YJS 8:21–52
Van Oort FVA, Greaves-Lord K, Ormel J, Verhulst FC, Huizink AC (2011) Risk indicators of anxiety throughout adolescence: the trails study. Depress Anxiety 28:485–494
Valleni-Basile LA, Garrison CZ, Waller JL, Addy CL, McKeown RE, Jackson KL et al (1996) Incidence of obsessive-compulsive disorder in a community sample of young adolescents. J Am Acad Child Adolesc Psychiatry 35:898–906
Zohar AH, Bruno R (1997) Normative and pathological obsessive-compulsive behaviour and ideation in childhood: a question of timing. J Child Psychol Psychiatry 38:993–999
Fontenelle LF, Mendlowicz MV, Marques C, Versiani M (2004) Transcultural effects of obsessive-compulsive disorder: a description of a Brazilian sample and a systematic review of international clinical studies. J Psychiatr Res 38:403–411
Thomsen PH (1991) Obsessive-compulsive symptoms in children and adolescents. A phenomenological analysis of 61 Danish cases. Psychopathology 24:12–18
Voltas N, Hernández-Martínez C, Arija V, Canals J (2013) Socio-demographic and psychopathological risk factors in obsessive-compulsive disorder: epidemiologic study of school population. Int J Clin Health Psychol 13:118–126
Angst J, Gamma A, Endrass J, Goodwin R, Ajdacic V, Eich D et al (2004) Obsessive-compulsive severity spectrum in the community: prevalence, comorbidity, and course. Eur Arch Psychiatry Clin Neurosci 254:156–164
Assunçao MC, da Conceiçao Lucas, Costa D, Mathis MA, Gedanke Shavitt R, Arzeno Ferrao Y, Rosário MC et al (2012) Social phobia in obsessive-compulsive disorder: prevalence and correlates. J Affect Disord 143:138–147
Mroczkowski M, Goes F, Riddle M, Grados M, Bienvenu O, Greenberg B et al (2011) Separation anxiety disorder in OCD. Depress Anxiety 28:256–262
Jakubovski E, Diniz JB, Valerio C, Fossaluza V, Belotto-Silva C, Gorenstein C et al (2012) Clinical predictors of long-term outcome in obsessive-compulsive disorder. Depress Anxiety. doi:10.1002/da.22013
Abramowitz JS, Storch E, Keeley M, Cordell E (2007) Obsessive-compulsive disorder with comorbid major depression: what is the role of cognitive factors? Behav Res Ther 45:2257–2267
Joo JC (2011) Comorbidity between schizophrenia and obsessive compulsive disorder: two distinct entities or a spectrum between the two disorders? Salud Ment 34:179–286
De Graaf R, Bijl RV, Ravelli A, Smit F, Vollebergh WA (2002) Predictors of first incidence of DSM-III-R psychiatric disorders in the general population: findings from the Netherlands Mental Health Survey and Incidence Study. Acta Psychiatr Scand 106:303–313
Veldhuis J, Dieleman JP, Wohlfarth T, Storosum JG, van den Brink W, Sturkenboom MC et al (2012) Incidence and prevalence of “diagnosed OCD” in a primary care, treatment seeking, population. Int J Psychiatry Clin Pract 16:85–92
Grisham JR, Fullana MA, Mataix-Cols D, Moffitt TE, Caspi A, Poulton R (2011) Risk factors prospectively associated with adult obsessive-compulsive symptom dimensions and obsessive-compulsive disorder. Psychol Med 41:2495–2506
Stewart SE, Geller DA, Jenike M, Pauls D, Shaw D, Mullin B et al (2004) Long-term outcome of pediatric obsessive-compulsive disorder: a meta-analysis and qualitative review of the literature. Acta Psychiatr Scand 110:4–13
Heyman I, Mataix-Cols D, Fineberg NA (2006) Clinical review. Obsessive-compulsive disorder. BMJ 333:424–429
Kalra SK, Swedo SE (2009) Children with obsessive-compulsive disorder: are they just “little adults”? J Clin Invest 119:737–746
Acknowledgments
This research was supported by a grant from the Fondo de Investigaciones Sanitarias (PI07/0839), Instituto de Salud Carlos III of the Spanish Ministry of Health and Consumption and by a doctoral grant from the Department of Universities, Research and the Information Society of the Generalitat de Catalunya (Catalan Government) and the European Social Fund.
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Voltas, N., Hernández-Martínez, C., Arija, V. et al. A Prospective Study of Paediatric Obsessive–Compulsive Symptomatology in a Spanish Community Sample. Child Psychiatry Hum Dev 45, 377–387 (2014). https://doi.org/10.1007/s10578-013-0408-4
Published:
Issue Date:
DOI: https://doi.org/10.1007/s10578-013-0408-4