Abstract
Given the relationship between internalizing disorders and deficits in emotion regulation in youth, the emotion science literature has suggested several avenues for increasing the efficacy of interventions for youth presenting with anxiety and depression. These possibilities include the identification and addition of emotion-regulation skills to existing treatment packages and broadening the scope of those emotions addressed in cognitive-behavioral treatments. Current emotion-focused interventions designed to meet one or both of these goals are discussed, and the developmental influences relevant to the selection of emotion-focused treatment goals are explored using the framework of a modal model of emotion regulation. These various lines of evidence are woven together to support the utility of a novel emotion-focused, cognitive-behavioral intervention, the Unified Protocol for the Treatment of Emotional Disorders in Youth, a transdiagnostic treatment protocol that aims to treat the range of emotional disorders (i.e., anxiety and depression) simultaneously. Avenues for future directions in treatment outcome and assessment of emotion regulation are also discussed.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Deficits in emotion regulation (ER) have been consistently linked with childhood psychopathology in general (Bradley 2000; Cicchetti et al. 1995; Keenan 2000; Vasey and Dadds 2001), and emotional disorders in particular (Campbell-Sills and Barlow 2007; Garber et al. 1995; Hannesdottir and Ollendick 2007; Ladouceur et al. 2005; Southam-Gerow and Kendall 2000; Suveg and Zeman 2004; Zeman et al. 2002), which are defined here as the anxiety and unipolar mood disorders. These studies have highlighted the fact that anxious and depressed children alike have difficulty managing sadness, anger, and anxiety, suggesting an overarching deficiency in effective emotional coping.
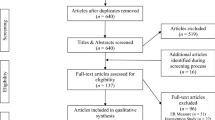
Despite the evidence linking poor ER processes more broadly to childhood psychopathology, emotion theory has only recently been applied to treatment protocols in youth (e.g., Denham and Burton 1996; Izard and Bear 2001; Suveg et al. 2006). One possible reason for the lack of an emotion focus in current treatments is the availability of cognitive-behavioral therapy (CBT), which is considered to be among the most efficacious treatments for internalizing disorders in children and adolescents (King et al. 2005; Stark et al. 2005). Results from cognitive-behavioral treatment outcome studies show that 60–70% of anxious children participating in a CBT protocol experienced a significant reduction in anxiety symptoms (Kendall et al. 2005; Ollendick et al. 2006). Similar results occur with CBT for depression. A recent meta-analysis of CBT outcome studies reported that 63% of depressed children showed clinically significant improvement in their depression by the end of treatment (Lewinsohn and Clarke 1999). In addition, the application of cognitive-behavioral interventions has been associated with a reduction in both the disorder being treated, as well as comorbid internalizing disorders (Borkovec et al. 1995; Brown et al. 1995). This is true both within adult (Tsao et al. 2002, 2005) and child and adolescent populations (Kendall et al. 2001).
It is clear that cognitive-behavioral treatments that target a specific disorder, such as depression, can be effective in reducing symptomatology associated with that disorder as well as comorbid diagnoses. Given the non-specificity of response to CBT, it can be argued that treatment components formatted appropriately to generalize to a broader range of emotions might be appropriate in treating individuals with multiple diagnoses. Also, given the literature indicating that anxious and depressed youth exhibit emotional impairment beyond their specified disorder(s), treatments that incorporate broader emotion-focused content may help individuals regulate emotions that, while not causing functional impairment per se, are subjectively distressing. Although the literature in this area is still sparse, there is evidence to show that most current versions of CBT do not address this issue. A recent study by Suveg et al. (in press) examined changes in emotion-related functioning in clinically anxious youth following a traditional course of CBT. Investigators found that treated youth exhibited significant improvements in anxiety symptoms, perceived ability to cope with anxiety-provoking situations (i.e., anxiety self-efficacy), and regulation of worry (i.e., less inhibition and dysregulation, greater culturally appropriate coping). However, these results did not generalize to anger or sadness, suggesting that participants still had regulation deficits in these areas.
Emotion theory as it relates to treatment of clinical disorders provides an exciting opportunity to enhance the applicability of existing cognitive-behavioral treatments, with some researchers positing that the addition of ER skills could be a key ingredient for expanding the efficacy of treatments for internalizing disorders in youth (Hannesdottir and Ollendick 2007; Samoilov and Goldfried 2000; Southam-Gerow and Kendall 2002). In this article, we provide a rationale for utilizing a broader emotion and ER context within cognitive-behavioral treatment and describe the Unified Protocol for the Treatment of Emotional Disorders in Youth (UP-Y; Ehrenreich et al. 2008), as an example of a transdiagnostic, emotion-focused approach to psychological intervention for the emotional disorders. We begin by briefly describing recent treatment outcome studies for protocols that have infused emotion-focused content into CBT protocols. Next, we present literature that highlights the need for a transdiagnostic approach to treatment and describe how ER is conceptualized in the UP-Y. Using a modal model of ER as a framework, we outline how maladaptive use of ER strategies correlates with anxiety and depression. We then delineate how the intervention components in the UP-Y protocol map directly onto the theoretical ER model in question. We conclude by providing preliminary treatment outcome data on the UP-Y with regard to improvements in diagnostic severity and overall emotion dysregulation, discussing future directions for our work based on these results.
Current Emotion-Focused Treatments
Recent efforts to integrate ER skills into efficacious cognitive-behavioral interventions have shown considerable promise in the alleviation of emotional disorders (Kovacs et al. 2006; Suveg et al. 2006). Suveg et al. (2006) developed an Emotion-Focused Cognitive-Behavioral Therapy (ECBT), which has initially been examined for efficacy for children ages 7–13 with anxiety disorders. This treatment protocol utilized all of the components of Kendall’s (2000) CBT “Coping Cat” program, such as psychoeducation, cognitive restructuring, relaxation, and exposure hierarchies. In addition, ECBT had additional content to address regulation of emotion, emotion expression, and emotion understanding, deficits in which have been linked to child anxiety (Southam-Gerow and Kendall 2002; Suveg and Zeman 2004). For example, emotion awareness was expanded from the originally specified single session to be included as content for discussion in all sessions. Participants were also taught skills related to the regulation of any emotions with which they had difficulty. For instance, they might be provided with a vignette about an emotionally salient situation and asked to brainstorm and problem solve based on the situation the vignette’s protagonist was facing (Suveg et al. 2006).
Using a multiple baseline design, six children with a principal diagnosis of either generalized anxiety disorder (GAD), social phobia, or separation anxiety disorder, completed the 16-session treatment at either 0, 2, or 3 weeks following their initial evaluation. Using parent and child self-report as well as clinician interviews, the children were assessed at posttreatment for anxious symptomatology and improved ability to regulate worry (i.e., better emotion understanding, competency in ER, and effective emotion expression). Results indicated that the majority of participants improved in all assessed areas and showed improved overall functioning.
Kovacs et al. (2006) recently pilot-tested a similarly emotion-focused treatment entitled Contextual Emotion-Regulation Therapy (CERT), which teaches the regulation of dysphoria in depressed youth by identifying the context of symptoms with regard to ER responses to stress and coping. Children ages 7–12 years with a diagnosis of chronic depressive disorder received 30 sessions in a multiphase design over a 10-month period. Children were provided with individualized interpersonal, cognitive, behavioral, and problem-solving strategies to help regulate mood. In addition, didactic aids were used to teach children to recognize situations that had historically elicited dysphoric states, and participants were asked to practice adaptive ER responses in order to prevent an increase in negative affect (NA). Parent- and child-reports of internalizing symptoms and diagnostic clinician interviews were administered pre- and post-treatment as well as at 6- and 12-month follow-up. Results revealed an overall improvement in self-reported and parent-reported internalizing symptoms as well as loss of diagnostic status, with 92% of completers having full remission of dysthymia 1 year after treatment completion.
Implications for an Emotion-Focused, Transdiagnostic Approach
Despite the promising results from the two studies described above, the protocols under investigation focus on specific disorders or clusters of disorder rather than on emotional disorders overall. Specifically, CERT (Kovacs et al. 2006) aims to reduce dysphoria in depressed youth, and ECBT (Suveg et al. 2006) has only been tested for efficacy among children with anxiety disorders. While there will always be justification for improving upon specific treatments for both anxiety and depression separately, we believe that the field is also in need of cognitive-behavioral protocols that aim to reduce anxiety and depression simultaneously given the high rates of comorbidity between these disorders in youth (Biederman et al. 1995; Kovacs and Devlin 1998), and given evidence suggesting that deficits in emotional processing are one reason for such high rates of comorbidity in internalizing disorders (Mennin et al. 2007).
Anxiety and Depression: Commonalities and Comorbidity
Multiple lines of research have confirmed that emotional disorders are highly related and frequently co-occur (for reviews, see Brady and Kendall 1992; Kendall and Brady 1995). A meta-analysis by Angold et al. (1999) revealed that anxiety disorders and depressive disorders in youth are more strongly associated with each other than to other forms of psychopathology. In addition, studies using latent class analysis have shown that it is rare for youth with internalizing disorders to have solely anxiety or depressive symptoms (van Lang et al. 2006). In an overview of studies spanning various child populations (pediatric clinics, community, inpatient units), Brady and Kendall (1992) reported that the percentage of each sample that met criteria for both anxiety and depression ranged from 15.9% to 61.9%, with clinical samples showing higher rates possibly due to the fact that children with both disorders are more symptomatic and therefore more likely to present to treatment facilities.
Many explanations have been put forward to explain the observed comorbidity. For instance, behavioral genetics research has shown that genetic influences on anxiety and depression are almost entirely shared (Eley 2001; Eley and Stevenson 1999; Thapar and McGuffin 1997). In fact, GAD is more similar to depression genotypically than it is to other anxiety disorders (Kendler et al. 2003).
It has also been argued that common temperamental risk factors account for the relationship between the emotional disorders (Barlow et al. 1996; Brady and Kendall 1992; King et al. 1991; Watson and Clark 1984). Some of the more tested models examining temperamental vulnerabilities for anxiety and depression include the constructs of NA, positive affect (PA), and physiological hyperarousal (PH), which were first described in Clark and Watson’s (1991) tripartite model of the affective disorders. PA and NA have been characterized as the tendency to feel pleasant or unpleasant emotional experiences, respectively (Clark and Watson 1991). PH is defined as a tendency to experience physical feelings associated with activation of the sympathetic nervous system (Clark and Watson 1991).
Recent research has suggested that NA is a risk factor for the development of both anxious and depressive disorders (e.g., Chorpita et al. 2000a; Clark et al. 1994; Lonigan and Phillips 2001; Watson et al. 1994). Although low PA was originally conceptualized as distinguishing depression from anxiety, it has been consistently linked to the depressive disorders as well as social phobia (Brown, Chorpita and Barlow 1998; Chorpita et al. 2000a; Watson et al. 2005). Similar surprises have come from studies examining PH. This construct was thought to be unique to fear-based anxiety disorders, such as panic disorder; however, studies in child samples have shown PH to be significantly associated with panic and separation anxiety (Chorpita et al. 2000a) as well as depression (Chorpita and Daleiden 2002; Jacques and Mash 2004). Although a full review of these constructs and their accompanying models is beyond the scope of this paper (for a review, see Anderson and Hope 2007), the evidence suggests that there are common underlying pathways that may lead to the development and maintenance of anxiety and depressive disorders.
Facilitating Dissemination of Empirically Supported Treatments
While emotion theory has garnered attention in treatment outcome studies, there has been a simultaneous interest in the importance of effective dissemination and implementation of evidence-based treatments to community settings. The National Institute of Mental Health has increasingly focused on the difficulties of bridging science and practice, organizing workshops on advancing implementation practices and increasing community access to evidence-based interventions (Chambers 2008; Hollon et al. 2002). The resulting recommendations of these task forces has consistently been to create “user-friendly” treatments that can be of equal benefit in both controlled conditions, such as those found in university-based clinics, as well as community settings that likely have reduced resources. There are myriad protocols available for specific disorders, but it is difficult to comprehend an overtaxed clinician becoming proficient in all of them given the inevitable time constraints and clinical burden that often accompanies serving youth in the community. These constraints, coupled with the fact that comorbidity is more common than not in clinical samples (Francis et al. 1992) and community populations (Kashani and Orvaschel 1990; Woodward and Fergusson 2001) may leave clinicians frustrated and baffled as they attempt to fuse the various methodologies recommended for treating the different disorders. By targeting the common diatheses and processes underlying comorbid conditions, a unified, emotion-focused approach might result in a greater degree of treatment efficacy for comorbid conditions in less time. This theory is bolstered by the literature indicating that disorder-specific treatments can generalize their effects to other comorbid disorders in both academic and community settings, even without treatment material that explicitly highlights common vulnerabilities (Barlow et al. 2004; Jenson-Doss and Weisz 2006).
ER and the UP-Y
As has now been discussed, there are many reasons to believe that the development of a transdiagnostic and emotion-focused cognitive-behavioral treatment approach would be a useful addition to the treatment literature. Perhaps more importantly, such a development is justifiable given our current understanding of the emotional disorders and their response to CBT. This section of the text provides a description of the UP-Y and a brief overview of the emotion and ER literature supporting the creation of a unified treatment approach for the emotional disorders.
The UP-Y (Ehrenreich et al. 2008) was developed to address all anxiety and unipolar mood disorders and is unique in the particular emphasis placed on the way individuals with emotional disorders experience and respond to a range of emotions. First introduced as a treatment for emotional disorders in adults (Barlow et al. 2004), the treatment was revised consistent with developments in the field of emotion science and was adapted for an adolescent population. A more in-depth description of the treatment and its components is provided later in this article. However, given the numerous definitions of emotion and ER in the field, it is useful first to clarify how these terms are conceptualized in the UP-Y. Our definitions of emotion and ER closely follow those defined by Gross and Thompson (2007). We consider emotions to be multifaceted phenomena that entail changes in one’s experience, reactive behaviors, and physiology. Emotions surge in reaction to internal and external stimuli that are seen as relevant to one’s survival and well-being. According to the modal model of emotion (Gross and Thompson 2007) upon which the development of the UP-Y is based, automatic appraisals occur when one is confronted with a salient event and allow one to interpret the situation’s valence. Depending on that interpretation, an emotional response is generated that leads to changes in behavioral, experiential, and physiological reactions.
When used here, ER refers to the cognitive and behavioral processes that act to change the frequency, intensity, duration, and expression of the experienced emotion. These regulatory strategies follow a dynamic process that changes over time, and this dynamic process involves repeated attempts using one or many strategies to regulate emotions as they unfold. Gross and Thompson’s (2007) modal model highlights five families of ER processes that occur along the temporal course of emotion generation. These processes include: situation selection, situation modification, attentional deployment, cognitive change, and response modulation (Gross 1998). As stated by Campbell-Sills and Barlow (2007), an ineffective ER strategy is either “(a) unsuccessful in reducing the unwanted affect or (b) associated with long-term costs that outweigh the benefit of short-term reduction of affect” (p. 543).
In the sections that follow, we argue that children and adolescents with internalizing disorders may be ineffective in their use of the five ER strategies defined by the modal model of emotion, and we provide a review of the literature which lends evidence to our viewpoint. Given that the effectiveness of ER strategies is largely dependent on the context of the specific stressor or event and can foster risk for as well as resiliency against psychological problems (Compas et al. 2006; Thompson and Calkins 1996; Weisz et al. 1994), we attempt to highlight both beneficial and maladaptive use of the ER strategies in question. The research outlined in the following section lends credence to the treatment principles of the UP-Y, which stipulate that adaptive cognitive appraisal, prevention of emotional avoidance, and reduction of maladaptive behavioral action tendencies are all necessary components of an effective treatment for emotional disorders in youth.
ER Components: Links to Anxiety and Depression
Situation Selection
The most conscious ER strategy in Gross’s model is situation selection, which involves the purposeful approach toward situations believed to result in pleasant emotions, and avoidance of situations believed to result in undesirable emotions. This strategy is used by all children and adolescents in the course of their daily lives. For instance, a child might not invite a classmate over to play because she believes the classmate won’t treat her fairly, or a teenager might avoid taking an optional chemistry class for fear that it will be too difficult. However, there can be barriers to situation selection that make this strategy less sufficient, including misunderstanding of one’s expected emotional responses and failure to appropriately weigh short-term benefits of ER versus long-term costs. With regard to the former, anxious and depressed individuals tend to overestimate the intensity and duration of negative emotions when confronted with certain events (Hammen and Rudolph 2003; Micco and Ehrenreich 2008). With regard to the latter, avoidance is an effective strategy for reducing negative emotions in the short-term as it does ensure that an individual will not be confronted with a situation that can cause intense fear, worry, or sadness. However, anxious individuals overly rely on avoidant coping and depressed individuals over-utilize social withdrawal as a coping mechanism (Mash and Wolfe 2002). Children with internalizing disorders do not seem to realize that this strategy prevents the natural reduction of fear and sadness that occurs with increased experiencing of stressful situations (habituation).
Avoidance of potential threat is one of the central features of anxiety disorders (Rapee 2002). A prominent example is agoraphobia, which involves the systematic avoidance of situations for fear of ensuing distressing physical symptoms. Social phobia in children is observed through distress in and/or avoidance of social events and specific phobias are defined by avoidance of situations that will produce the feared stimulus. It appears that this tendency toward avoidance can appear very early in a child’s development. Infants who are labeled as behaviorally inhibited (i.e., withdraw from or avoid new or unfamiliar people or situations) have been found to be at increased risk for developing an anxiety disorder in childhood (Biederman et al. 1990). Similar to what has been found in anxious samples, behavioral inhibition has been linked to depression in youth. Children labeled as inhibited at age three were found to be at increased risk for depression and suicide (Caspi et al. 1996). It can be argued that an inhibited temperamental style leads to a deficit in appropriate situation selection, thus increasing risk for anxiety and depression later in development.
The avoidance strategy that is typical of children and adolescence with major depression is social withdrawal (Bell-Dolan et al. 1993; Goodyer and Cooper 1993). In an observational study of an inpatient sample, depressed youths were found to engage in less social interaction and to produce less affect-related expression than nondepressed psychiatric inpatients (Kazdin et al. 1985). This withdrawal is a natural off-shoot of anhedonia, or a lack of interest in pleasurable activities, that is considered to be one of the key features of depression (Hammen and Rudolph 2003). Campbell-Sills and Barlow (2007) speculate that social withdrawal is a regulatory strategy specific to sadness as depressed individuals might predict that their NA will worsen in social settings. However, this maladaptive ER strategy also prevents access to successful and/or pleasurable experiences, further increasing feelings of sadness and decreasing social support. In fact, adolescent self-report of extreme social withdrawal was found to be predictive of suicide attempts (Invarsson et al. 2002).
Situation Modification
Absolute avoidance of distressing or unpleasant situations is not always feasible. When this is the case, an individual has the option of modifying the situation so as to decrease its emotional impact. Given that children often do not have the choice of whether or not to avoid unwanted situations, this can be a useful strategy. For instance, a child who is nervous about going to a birthday party can work to ensure that a friend comes with him or her.
Situation modification is often employed as an ER strategy in anxious and depressed youth. One of the more notable examples of this method in anxious individuals (Campbell-Sills and Barlow 2007) is the use of “safety signals,” which include objects or persons that reduce the overall emotional salience of a situation as they signal that a feared or aversive stimulus will not occur. There is no predetermined set of safety signals as they can be inanimate objects (e.g., a certain room in the home), behaviors (e.g., sitting at a desk close to an exit), or other people (e.g., a parent). For example, a child with panic disorder might feel comfortable going to school if and only if his medicine is in his backpack, or a depressed teenager might feel less distressed while walking the hallways if she is listening to her iPod.
Attending to safety signals is a strategy that is useful in the short-term given that it does reduce emotional distress. There is some evidence for its long-term effectiveness as well. A recent study by Milosevic and Radomsky (2008) points to the fact that judicious use of safety behaviors can lead to increased treatment retention and better treatment outcome. However, an over-reliance on safety signals helps maintain catastrophic beliefs when a person confronts a stimulus believed to be dangerous and the feared outcome does not occur (Salkovskis et al. 1996). In the long-term, individuals who exclusively count on safety signals may fail to learn corrective information and believe that situations are only harmless if their safety object/person is in place, failing to recognize their ability to cope effectively in a situation that is objectively free of danger (Salkovskis 1991). This theory is bolstered by recent research showing that the use of safety signals leads to poorer treatment response (Kim 2005; Powers et al. 2004; Sloan and Telch 2002). For instance, Sloan and Telch (2002) examined the effects of safety-seeking behaviors and guided threat focus during exposure-based treatment for individuals with claustrophobia. They found that participants who were encouraged to use safety behaviors (e.g., standing near an exit) during exposure exhibited significantly more fear at post-treatment and follow-up compared to those who were asked to focus on and reevaluate their core fear during exposure. The investigators also found that use of safety behaviors resulted in a detrimental effect on between-trial habituation. Taken together, the research just described indicates that, while judicious use of safety signals may be beneficial, the consistent and inflexible use of these techniques leads to long-term maintenance of anxiety.
With regard to situation modification in depressed youth, one interpersonal behavior that is common in this population is excessive reassurance seeking (Joiner et al. 1992; Katz et al. 1998), defined as “the relatively stable tendency to excessively and persistently seek assurances from others that one is lovable and worthy, regardless of whether such assurance has already been provided” (Joiner et al. 1999). It can be argued that this is a form of situation modification, as the intended effect is to reduce NA by transmitting distress from one person to another (Joiner et al. 1999). According to this interpersonal model of depression (see Coyne 1976, for an in-depth description), dysphoric individuals seek reassurance from others but doubt the reassuring message that is received. However, the need for comfort is powerful and leads to more reassurance-seeking, creating a pattern, which can lead to frustration in individuals whom the person consistently questions. Any apparent signs of frustration are internalized by the dysphoric individual, and a cycle is created in which any subclinical symptoms of depression are exacerbated due to perceived rejection. This model has been supported in the literature. Potthoff et al. (1995) examined a college sample of 267 students and found that a reassurance-seeking style, along with minor interpersonal stressors (e.g., a disagreement with a friend), contributed to increases in depressive symptoms over a 5-week period.
Attentional Deployment
Once individuals find themselves in a situation that is likely to induce a negative emotional response, they can regulate affect by directing their attention in a manner that either increases or decreases emotions. For example, an adolescent might find himself in a movie that was more frightening than he was prepared for. He could easily reduce feelings of fear by distracting himself during more terrifying scenes (e.g., covering his eyes). Once again, using attentional deployment as a strategy for changing unwanted emotions can be adaptive, but it can also hinder effective ER when used systematically across situations.
Many methods utilized for directing attention away from an unwanted stimulus are unconscious rather than effortful; therefore, it is important to mention the tendency for anxious and depressed individuals to have an implicit bias toward negative cues. Children with high levels of anxiety have been shown to give higher processing priority to threatening information in both salient and non-salient situations, meaning they interpret ambiguous or objectively non-threatening situations as more harmful than non-anxious children (Bögels and Zigterman 2000; Hadwin et al. 1997; Micco and Ehrenreich 2008; Muris, Rapee, Meesters, Schouten and Geers 2003; Suarez and Bell-Dolan 2001; Vasey and MacLeod 2001). Anxious children have also demonstrated hypersensitivity and responsiveness to bodily cues that anticipate negative emotions (Thompson 2001).
This pattern has been replicated in depressed samples as well. In fact, attentional bias is at the root of many cognitive theories of depression, which posit that depressed individuals selectively attend to negative stimuli while simultaneously ignoring positive stimuli. Depression then develops when stressful life events or negative mood states cue pre-existing maladaptive schemas, leading to biased informational processing and depressed mood (see Gotlib and Krasnoperova 1998; Whitehouse et al. 2000, for reviews of cognitive models). This model has been validated by studies of depressed youth, which have found that children with depression, or those at high risk for depression, have a tendency to recall negative information more readily than positive information when discussing past memories (Bishop et al. 2004) and are more easily distracted by negative pictures than by neutral pictures (Ladouceur et al. 2005). Reid et al. (2006) examined information processing in 133 children (ages 8–14), looking to discover whether children with anxiety, depression, and aggression displayed pervasive cognitive biases of attention, judgment, and memory. They found a general bias across the disorders for attention to negative information, negative interpretation of ambiguous situations, and preferential recall of negative words.
Although unconscious strategies such as information processing are certainly influential in attentional deployment, there are many strategies that are more effortful in nature. These include thought suppression, distraction, and maladaptive concentration. Thought suppression, or the effort to control verbal thoughts and mental images in order to reduce negative emotions, is a tactic that individuals use to make thoughts disappear by intentionally shifting attention away from stressful or depressing stimuli. Attempts to suppress unwanted thoughts are associated with a paradoxical increase in these unwanted thoughts and associated negative emotions (Trinder and Salkovskis 1994). Therefore, it is not surprising that use of thought suppression as an ER strategy has been consistently linked with anxiety and mood disorders.
Distraction, or reducing attention to emotionally charged stimuli by focusing on less salient or less distressing stimuli, is often used by individuals in order to avoid feelings of physical and mental discomfort. When used flexibly and in concert with other coping strategies such as cognitive restructuring and acceptance, distraction has been linked to lower levels of anxiety and depression symptoms (Compas et al. 2006; Kocovski et al. 2005; Nolen-Hoeksema et al. 1993; Oliver and Page 2003; Sica et al. 2007). However, it has also been argued that distraction maintains symptoms of anxiety and mood disorders, primarily as it does not lead to effective problem solving, nor does it allow for the effective challenging of anxious or depressed thinking (Campbell-Sills and Barlow 2007).
Finally, maladaptive concentration, which encompasses worry and rumination (Gross and Thompson 2007), involves focusing one’s attention on the emotional aspects of a situation without attempts toward resolution. Research has shown that both worry and rumination are viewed by anxious and depressed individuals as methods for reducing emotional distress, perhaps by making them feel more prepared for an upcoming situation or helping them avoid even more stressful thoughts (Borkovec and Roemer 1995; Wells and Carter 2001). A recent study by Gosselin et al. (2007) examined avoidant cognitive strategies in a sample of 777 adolescents. Results indicated that adolescents with a high level of worry used more avoidant strategies, including thought suppression, thought substitution, and distraction, than did adolescents with moderate levels of worry. Burwell and Shirk (2007) used a longitudinal design to investigate the relationship between rumination and depressive symptoms in a community sample of adolescents (n = 168), finding that brooding, a subtype of rumination that involves passively focusing on symptoms, predicted the development of depressive symptoms over time. Rumination also predicts the duration and severity of depressive symptoms (Nolen-Hoeksema et al. 1993).
Cognitive Change
Cognitive change occurs when individuals shift how they think about a situation in order to increase or decrease its emotional significance. This strategy can occur in two different ways, either by changing how the situation is thought of or by reconfiguring one’s capacity to manage the emotional demands of the situation. Cognitive change can be applied to both internal and external events. Consider the child who tries to think “happy thoughts” when in a dark room at bedtime instead of dwelling on thoughts about monsters in the closet, or a student athlete who interprets a racing heart before a game as a much-needed adrenaline rush as opposed to a dangerous physical condition.
The most studied form of cognitive change takes the form of reappraisal, or the alteration of meanings assigned to emotionally charged stimuli in order to regulate affect. Studies of depressed and anxious populations have shown a weakness in the ability to reappraise salient events either in order to reduce distress or increase pleasant emotions. Negatively biased cognition is a core feature of depression, and depressed individuals often distort their appraisals of events and situations in order to fit their pre-existing negative view of themselves (Young et al. 2001). For instance, one study found that children with high levels of depressive symptoms are likely to appraise rejection situations as more emotionally distressing and to have more catastrophic thoughts about the event than children without depressive symptomatology (Reijntjes et al. 2006). Moreover, youth who score higher on measures of depression expect lower mood improvement from cognitive reappraisal strategies (Garber et al. 1995; Quiggle et al. 1992). Some of the more common cognitive distortions of depression include arbitrary inference (reaching a conclusion not justified by evidence), all-or-none thinking (ignoring the “gray” areas of an emotionally charged event), and selective abstraction (only attending to negative aspects of a situation without attending to positive aspects; Beck et al. 1979).
Anxious individuals also have a tendency toward negative attributions. Although anxious children have been shown to report the same frequency of negative cognitions and depressed children, the schemata and form of their automatic thoughts leads to differences symptoms (Stark et al. 1993). As noted by Kendall and Ingram (1987), depressed youth make negative declarative statements, whereas the negative cognitions of anxious youth tend to take the form of a question. For instance, individuals with social phobia often ask themselves if they are unacceptable to others and question their ability to behave in a normal manner in social situations (Turk et al. 2001). Those who suffer from panic disorder often question the meaning of bodily sensations and view them as dangerous, which can increase distress during a panic episode.
Based on the findings that cognitive distortions are linked to internalizing psychopathology, it is not surprising that effective reappraisal, which takes the form of developing evidence-based reinterpretations of thoughts, feelings, or behaviors, is the cornerstone of CBT for mood and anxiety disorders. Cognitive restructuring has been deemed an ER strategy because it involves a change in cognitive appraisal that can lead to change in emotion (Hannesdottir and Ollendick 2007). The specificity of restructuring may vary across anxiety and depression (e.g., perceptions of threat may be the focus for anxious youth while thoughts contributing to feelings of hopelessness may be targeted in depression), but replacing dysfunctional thoughts with more functional thinking is a common goal (Clarke et al. 2003; Kendall et al. 2003; Weisz et al. 2003). In general, changes in one’s ability to reconstruct negative cognitions are associated with enhanced psychological adjustment and emotional well-being (Compas et al. 2001; Prins and Ollendick 2003). Moreover, reappraising one’s cognitions before entering an emotionally evocative situation appears to result in an even greater change in the emotion experienced (Gross 2003).
Response Modulation
The regulatory approaches previously discussed are utilized in order to avoid experiencing emotion; however, response modulation occurs after other strategies have failed and the unwanted emotion has been generated. This form of regulation allows the individual to alter the manifestation or experience of an emotion via physiological or behavioral means. Adolescents are keenly aware of the interpersonal and social consequences of emotion displays, and this heightened awareness effects their decisions to express or contain certain emotions with particular individuals (Fuchs and Thelen 1988; Zeman and Shipman 1997, 1998).
For example, older children are more selective with their use of emotion expression than younger children, and are more likely to modify their emotional responding with peers than with their parents (Zeman and Garber 1996). Many forms of response modulation are utilized in non-clinical samples. Imagine an adolescent suppressing anxious behaviors during his or her first job interview. As seen in the misuse of all previously discussed ER strategies, though, an over-reliance on certain forms of response modulation can promote and maintain internalizing symptoms.
The most studied behavioral manifestation of response modulation is expression of emotion, which can include the inhibition, appropriate expression, or exaggeration of emotional response. Emotion expression serves to signal an emotional state to the self and to others in the environment. Like any ER strategy, its success is highly reliant on context. For instance, a maltreated child might inhibit emotion expression so as not to induce a negative response from a caretaker. However, research indicates that individuals with internalizing symptomatology tend to express emotions inflexibly and in ways that are inappropriate to dynamically changing contexts (Rottenberg and Vaughan 2008). For instance, a depressed adolescent might use inhibition as a sole form of emotion expression, therefore failing to send signals to a caretaker that he needs to be soothed. Children who are diagnosed with a psychological disorder have been found to have difficulty with emotion expression, whether through inhibiting the expression of emotion (e.g., holding back tears), or exhibiting non-normative or culturally inappropriate expression (e.g., taking anger out on others when having a bad day; Southam-Gerow and Kendall 2002; Suveg and Zeman 2004). These maladaptive patterns of emotion expression, particularly inhibition of worry, anger, and sadness, have been shown to predict both anxious and depressive symptoms (Zeman et al. 2002). In a recent study of college students, Chaplin (2006) used self-report and observational methods to assess links between emotion expression and depressive symptoms. Participants completed questionnaires about overall emotion experience during the past month and were then asked to complete a frustration task with a peer. Associations were found between depression and emotion expression when a participant’s reported overall emotion experience was incongruent with reported emotion experience during the frustration task (e.g., reports of high anger experience during the past month but displays of low anger during the task). This study also highlights the importance of emotion expression of all emotions, not just sadness, with regard to depression.
In addition to emotion expression, cognitive-behavioral theorists who espouse the link between emotions and action tendencies would argue that a surge of unwanted emotion often motivates depressed or anxious individuals to escape situations that they find threatening or undesirable (Hammen and Rudolph 2003; Albano et al. 2003). Barlow and colleagues call such action tendencies emotion-driven behaviors (EDBs), defined as any number of specific behaviors that are driven by the height of the emotional experience itself (Barlow et al. 2004). From an ER perpective, EDBs are a form of response modulation as the behavior is aimed at reducing the impact of the ongoing emotional response. These behaviors are considered to be adaptive under circumstances in which escape is preferential, for instance during objectively dangerous situations, but can lead to the maintenance of emotional disorders when emotional events are subjectively dangerous but not objectively so. For example, an adolescent with social phobia is likely to have a similar fear response when faced with speaking to unfamiliar persons as a non-anxious youth might have facing a peer in a fight, and both are likely to attempt escape. Certainly the fear feels real for the anxious individual, but the emotion felt and the subsequent behavioral response is incongruent with the context. Such escape responses are reinforcing for the individual, however, and contribute to the maintenance of emotional disorders by preventing emotional habituation (Campbell-Sills and Barlow 2007).
Parenting Factors and ER Development in Adolescence
When considering ER in children and adolescents, it is imperative that the emotion socialization process in families is taken into account given that caretakers are a primary influence in how youth learn to interpret, manage, and express emotion (Saarni 1999; Thompson and Meyer 2007). Research has shown that parents socialize ER in their children both directly (e.g., direct instruction) and indirectly (e.g., discussion of emotion-related issues, modeling appropriate emotional responses; Saarni 1999). Parental responses to their adolescent’s emotions and attempts at ER are related to the adolescent’s emotional competency. Yap et al. (2008) found that adolescents whose mothers responded to their PA in an invalidating manner were more likely to endorse depressive symptoms, report using maladaptive ER strategies, and display emotionally dysregulated behaviors. Further, parents who respond with facilitative behavior contingent on their adolescent’s anxious or depressed behavior decrease the likelihood that the adolescent will employ successful ER strategies to attenuate their own anxious and/or depressed behaviors (Gar and Hudson 2008; Sheeber et al. 2000). Literature supporting how various parenting factors contribute to the modal model of ER is outlined briefly below.
Situation Selection
Not only do anxious and depressed children avoid situations that are likely to result in negative emotions, but parents often aid their children in this process. For instance, it is also not uncommon to see parents abetting their child’s compulsive rituals, perhaps going to extremes to keep “contaminated” items out of the child’s way. Studies examining the relationship between parental behavior and childhood anxiety suggest that parents of anxious children may affect increases in avoidant behaviors through modeling, prompting, and reinforcing anxious behavior in their children (Muris et al. 1996). These parents influence their child’s attention to and interpretation of threat cues. Research on contextual family variables that are linked with depression has produced substantial data showing differences in the family atmosphere and home environment of depressed youth and offspring of depressed parents. With regard to social withdrawal, families with depressed members have been found to be less likely to engage in pleasant activities (McKeown et al. 1997), which models detrimental use of situation selection. These studies demonstrate that parents who model avoidant coping and attend more substantially to threatening cues are more likely to have children who lack the ability to regulate fear and anxiety effectively.
Situation Modification
Parents can be instrumental in situation modification via their attempts to alter a child’s emotional response during potentially distressing situations. For instance, a mother might see her son struggling with math homework and help him solve the items giving him trouble. This strategy may be useful for certain situations and is often developmentally appropriate. However, parental control and lack of autonomy granting has been consistently linked with anxiety disorders in youth (for a meta-analytic review, see McLeod et al. 2007b). Observations of depressed mothers and their children reveal myriad interactional difficulties, among them a pattern of withdrawal, disengagement, and lack of contingent responding (Field et al. 1990; Gordon et al. 1989; Hops et al. 1987; Radke-Yarrow 1998). Given the clear evidence that depression runs in families in part due to modeling of depressive behaviors (for reviews, see Cummings and Davies 1999; Gelfand and Teti 1990; Goodman and Gotlib 1999; Hammen 1991), it can be argued that children of depressed parents learn insufficient strategies for modifying distressing situations.
Attentional Deployment
Parents can attempt to influence their child’s attentional deployment when he or she is confronted with a potentially frightening or distressing event. They might distract the child’s attention away from aversive stimuli or attempt to alter a negatively valenced interpretation of an object or event, thereby increasing their child’s attention toward or away from aversive stimuli. Parental coaching by way of parent–child conversation is an important contributor to emotional understanding and regulation (Thompson 2006). Studies indicate that when mothers talk about emotions more frequently and with more flexible interpretations of emotion-inducing events, children develop greater sophistication in their own emotional knowledge (Gottman et al. 1997; Thompson and Meyer 2007). This allows them greater flexibility when attending to and interpreting the meaning of aversive events. With regard to internalizing psychopathology, anxious children may in part glean their information processing style from parents who also have a tendency toward negative interpretation bias (e.g., Bögels et al. 2003; Creswell et al. 2005).
Cognitive Change
Children’s cognitive appraisals as they are related to emotion are influenced by the socially prescribed causes and consequences of emotions (Stegge and Terwogt 2007). Parents are on the front line of passing down socialized representations of emotion and are therefore pivotal instruments for teaching their child how to appraise emotionally salient events. Parents influence this process via (1) the information they provide when their child is confronted with emotionally provoking circumstances, (2) the explanation of causes of different emotions in others, and (3) providing rules about feelings or emotional scripts to live by (Denham 1998; Eisenberg et al. 1998; Thompson 1994). Given these parameters, it is not surprising that both overt and covert negative messages from parents directed toward a child about him- or herself, the future, and the environment have been shown to distinguish youth with internalizing disorders from youth without anxious or depressive symptoms (Stark et al. 1993).
Response Modulation
Studies of parent–child interactions reveal that attempts to influence a child’s emotion expression, and in particular attempts to limit or suppress the expression of NA, can contribute to internalizing psychopathology. There is a significant body of research indicating that parental support of the child’s emotional expression leads to the acquisition of more adaptive ER strategies. On the contrary, children who perceive parental responses to their emotional states as shaming, dismissive, or demeaning are less likely to cope effectively when confronted with distressing situations (for reviews, see Eisenberg et al. 1998; Thompson and Meyer 2007). Eisenberg et al. (1996) examined parental response to negative emotion and found that maternal reports of problem-solving approaches were associated with constructive coping strategies (e.g., positive thinking, seeking support) in children. However, mothers’ reports of denigrating reactions to their child’s emotions were associated with the child’s use of avoidant coping, which as previously discussed is a strategy commonly employed by anxious youth. There is also data, which indicate that families with depressed members are perceived to be less open to emotional expressiveness (McKeown et al. 1997; Oliver et al. 1987).
Parent Involvement in Treatment
The findings described above suggest that parental factors are important targets for treatment for adolescent internalizing disorders, with particular focus on removing reinforcement for anxious and depressed behaviors, teaching of appropriate modeling, and reduction of family conflict and parental rejection. Other advantages of including parents in treatment are the generalization of skills to other family members and maintenance of gains at the termination of therapy (Ginsburg et al. 1995). However, the literature is inconclusive with regard to the benefits of parental involvement (for a review, see Barmish and Kendall 2005). Recent meta-analyses of parenting and childhood psychopathology revealed that parenting factors account for less than 4% of the variance in childhood anxiety (McLeod et al. 2007a) and less than 8% of variance in child depression (McLeod et al. 2007b), which suggests that parenting factors should not be a primary focus of treatment. Also, given the developmental task of individuation and autonomy in adolescence, it might be that a parental adjunct to treatment is preferable for younger but not older children. This theory is supported by a study in which the inclusion of parents was found to be favorable for children ages 7–10 but not children ages 11–14 (Barrett et al. 1996). Therefore, the decision whether or not to include parents in treatment should be considered with regard to many factors and should be based on clinical judgment stemming from thorough case conceptualization.
The UP-Y Protocol: Description and Treatment Components
Throughout this article, we have discussed the modal model of ER (Gross and Thompson 2007) and have provided examples suggesting that internalizing symptomatology can be viewed as problematic use of five specific ER processes. Now we will describe the treatment components of the UP-Y, using the modal model of ER as a useful heuristic in highlighting the rationale for inclusion of each skill in the protocol. A list of the treatment modules included in the UP-Y, along with their relationship to this model of ER, is presented in Table 1.
The UP-Y is a flexibly administered, emotion-focused, cognitive-behavioral treatment package designed to enhance adolescents’ ER skills and decrease emotional disorder symptomatology. In this protocol, treatment techniques are explicitly applied to a broad range of emotional experiences including, but not limited to, sadness, anxiety, fear, and anger. This structure was chosen because we expect it will increase the applicability of a cognitive-behavioral treatment protocol to a broad range of emotional disorders.
In order to increase treatment flexibility, the protocol is broken up into eight sections, including five required sections and three optional sections. A required treatment section includes material which must be provided, although the number of sessions utilized to accomplish these goals may vary. At this time, the ordering of the required treatment sections is fixed, although the number of sessions used by the clinician to complete each section’s goals may vary depending on the needs of the individual adolescent. An optional treatment section is flexible, such that a clinician may decide how much, if any, of these optional materials to use, and material can be utilized at any point in treatment. Given this flexibility in administration, the overall length of the protocol can vary between 8 and 21 sessions.
The five required treatment sections include (a) psychoeducation regarding common emotional states, including the purpose and utility of these emotional experiences, (b) increasing awareness of one’s own emotional experiences, (c) identification and evaluation of one’s automatic interpretations, (d) a systematic reduction of behaviors designed to avoid or reduce uncomfortable emotional experiences, and (e) discussions of how to maintain the gains made during treatment while encouraging the attainment of future gains. The optional treatment sections include (a) motivational enhancement techniques, (b) the management of emergent crisis situations and/or the development of suicidal or homicidal ideation, and (c) parent training material designed to help parents learn to respond to their adolescents’ emotionally driven behaviors in adaptive ways.
A series of knowledge checks have been embedded within each of the required treatment sections. As the adolescent proceeds through the therapeutic material, the clinician is instructed to assess understanding of the treatment concepts using these knowledge checks. Those adolescents able to show they have adequately mastered the material in question are able to move on to the next portion of the protocol. Those unable to complete the knowledge checks spend additional time on the material in question.
A summary of each treatment section is provided below. As many of the components include CBT skills described in great detail elsewhere (Hannesdottir and Ollendick 2007; Kendall 2000; Weisz et al. 1997), we will focus on how each module attempts to apply the treatment techniques being discussed to a wide range of emotions rather than focusing on a single symptom set or disorder.
Required Treatment Section One: Getting to Know Your Emotions and Behaviors (Attentional Deployment)
The psychoeducation section is designed to provide the adolescent and parent with a framework for understanding emotion in general and uncomfortable emotional experiences in particular. This includes discussions of the emotional knowledge frequently lacking in adolescents with internalizing disorders. For instance, psychoeducation regarding the adaptive function of various emotional experiences is presented. As an example, the description that might be provided for anger is described below:
Anger is a natural response to the belief that you have been hurt or mistreated. This includes ideas, objects, dreams, values, and people. Anger motivates us to take action to defend ourselves and/or the things we care about and is often directed at the person or thing we find threatening.
Therefore, an adolescent learns that anger, while an uncomfortable to experience, may provide the energy and focus to stand up to a threat. The normal, natural, and potentially helpful nature of each emotion is emphasized. The role of one’s responses to emotion is also discussed, such that certain responses may maintain uncomfortable emotional experiences. At least two emotions relevant to the adolescent’s presenting complaint are discussed. However, clinicians are encouraged to cover at least three emotions typically difficult for adolescents presenting with an anxious and/or depressive disorder (e.g., anger; Suveg and Zeman 2004).
As previously defined, emotions are multifaceted phenomena that entail changes in one’s internal experience (e.g., thoughts), reactive behaviors (e.g., avoidance, EDBs), and physiology. Therefore, adolescents are taught to monitor their emotions via these three pathways. Adolescents are informed that one’s thoughts, physical sensations, and actions are all related to each other and, in turn, to the emotions experienced. Therefore, a change in any one of these components will impact all the others.
A functional analytic monitoring scheme is also introduced such that adolescents are asked to track the triggers and consequences associated with their emotional experiences. Adolescents are encouraged to examine the impact of their attempts to manage their uncomfortable emotional experiences, determining whether these strategies are leading to the desired outcome. Once the adolescent understands the application of this material (i.e., has met the predefined mastery criteria, or knowledge check, referenced above), the next treatment section begins.
Required Treatment Section Two: Awareness of Emotions (Attentional Deployment, Response Modulation)
The next focus of the protocol is on increasing awareness of one’s current emotional experiences. The eventual goal of these awareness exercises is to learn to be non-judgmentally aware of one’s current emotional experiences without making efforts to suppress the emotional response or inhibit emotion expression. Early versions of the protocol included complex, multi-sensory awareness exercises. However, our experiences piloting the protocol suggested that many adolescents evidenced difficulty mastering this material. Therefore, it was decided to break the awareness exercises into its component parts. In the current version of the protocol, adolescents are encouraged to increase awareness of and attention toward one part of an emotional experience at a time. Once an adolescent has shown an ability to remain aware of all three parts of the emotional experience individually, awareness exercises are broadened to include awareness of multiple components and the relationships among those components. Examples of such awareness exercises may include progressive muscle relaxation (as described in Kendall and Hedtke 2006), but may also include any number of other exercises (e.g., attending only to one’s thoughts, taking a walk, doing push-ups, etc.).
In the latter part of this treatment section, and throughout the rest of treatment, adolescents are asked to practice these awareness exercises in the context of generalized emotion exposures, which are emotionally evocative, although disorder non-specific, stimuli. Disorder-specific treatments focus on the stimuli associated with the disordered emotion in question; the emotion exposures in this protocol are designed to encourage adolescents to experience a range of emotional experiences, including both pleasant and uncomfortable (or previously avoided) emotions. Adolescents may choose to listen to a song, watch a movie clip, or write and re-read a narrative that elicits a given emotion. At this point in the protocol, the goal is for adolescents to experience a range of emotions (and not just those specific to their emotional disorders), merely observing their subjective reactions (especially their thoughts, physical sensations, and behaviors). This focus on present-moment awareness helps adolescents begin to identify their current (and frequently maladaptive) attempts at ER and helps set the stage for the use of future ER strategies presented in the protocol. As this stage of treatment is designed to ensure awareness of emotional experiences as they occur, without judging or avoiding them, it represents an attempt to correct maladaptive attentional deployment strategies while laying the groundwork for the use of future ER strategies.
Required Treatment Section Three: Being Flexible in Your Thinking (Cognitive Change)
Building on the increased awareness of emotional experiences, adolescents are then asked to focus on the evaluation of their thoughts (or interpretations). This part of the protocol utilizes a traditional Beckian cognitive therapy (described extensively elsewhere, e.g., Beck 1995). As the emotion science literature has suggested that cognitive reappraisal is most effective when completed before entering an emotionally evocative situation (discussed above; Gross 2003), adolescents learn to engage in antecedent-focused cognitive reappraisal prior to contact with the emotionally evocative stimuli in question. Once again, adolescents are given the opportunity to practice the use of this skill in the context of the generalized emotion exposures described above. However, by this point in treatment, these emotion exposures become increasingly specific to the presenting complaint and may, at times, be targeting the specific emotion (if not the exact stimuli) bringing the adolescent in for treatment. For example, an adolescent seeking treatment for depression may be asked to watch a movie clip that has elicited feelings of sadness in the past. Prior to watching the film, the adolescent may generate the thoughts he expects will occur as a result of this viewing. Along with his clinician, the adolescent might then utilize his newly acquired cognitive reappraisal techniques to determine whether his thoughts or interpretations are realistic or useful. If the adolescent deemed the thoughts or interpretations unrealistic, he would work to generate more useful or balanced interpretations that could be recalled while emotionally engaged with the film clip.
The above emphasis on increasing cognitive flexibility becomes key in the later part of this treatment section, during which a series of problem-solving steps are taught. As with several of the other components in this protocol, problem-solving is frequently included in cognitive-behavioral treatment approaches because some emotional disorders are accompanied by poor problem-solving efforts, or at least the perception that one’s problem-solving abilities are poor (Blankstein et al. 1992; Gosselin et al. 1997). In the context of this protocol, problem-solving is introduced as a series of concrete steps that are utilized to reappraise decision-making in an emotionally evocative situation. Similar to cognitive reappraisal, adolescents are encouraged to use problem solving steps prior to entering an emotionally evocative situation.
As is now evident, this treatment section aligns with Gross’s principle of cognitive change as a means of regulating emotion, although problem-solving is a strategy that can be utilized in future situation selection. Regardless, throughout this phase of treatment, adolescents learn to examine and alter their automatic appraisals allowing for more adaptive thoughts and problem solutions.
Required Treatment Section Four: Emotion Exposure (Situation Selection, Situation Modification and Response Modulation)
During this phase of the protocol, adolescents move from the generalized emotion exposures conducted in required treatment sections two and three, to situational emotional exposure. Situational emotion exposure is similar to both traditional exposure paradigms for anxiety disorders and behavioral activation for depression (e.g., Kendall and Hedtke 2006; Weisz et al. 1999). As part of these exposure activities, adolescents gradually enter situations associated with the emotional experiences they have been trying to avoid. This treatment component is specifically designed to encourage the adolescent to enter situations associated with previously avoided or uncomfortable emotional experiences while remaining in full contact with the emotion in question. Attempts to avoid or reduce contact with the emotion, whether through behavioral avoidance and/or ineffective emotion expression, are noted and counteracted.
For instance, an adolescent presenting with depression who also experiences periods of intense anger may be asked to have a conversation with her parent about standards for keeping her room clean (a situation in which she may feel angry). Before entering this emotionally evocative situation, the adolescent would be encouraged to reappraise her automatic interpretation (e.g., “My mom does not care what I want.”). The adolescent would also be encouraged to remain aware of her emotional experience throughout the exposure, but to act in a manner that is likely in opposition to reactions that might have been previously used to regulate the uncomfortable emotional experience (e.g., speaking calmly with her parent when she may wish to yell and walk away). By choosing to face such stimuli without engaging in any attempts to avoid the emotional experience, while at the same time learning ways to modulate the emotional response appropriately, the adolescent learns she is able to handle these emotional experiences successfully.
Required Treatment Section Five: Keeping It Going—Maintaining Your Gains
The final required section involves a fairly standard review of the newly learned cognitive behavioral ER skills. For instance, adolescents are encouraged to summarize each of the treatment techniques they learned and to describe the use of these skills in their daily lives. Working with their therapist, adolescents identify a personally meaningful way of capturing and preserving the knowledge gained in therapy (e.g., by making a memory book). Adolescents are encouraged to identify whether any emotion exposures still remain to be completed and to plan for the completion of these exposures in the coming weeks. Finally, adolescents are asked to predict future difficulties they might experience and criteria for differentiating normal fluctuation in emotional experiences from a full return of disordered emotional responding. Use of these ER skills in the face of future uncomfortable emotional experiences as a way of preventing the development or recurrence of future emotional disorders is emphasized and adolescents are encouraged to continue to use these skills in the face of future uncomfortable emotional experiences.
Optional Treatment Section One: Building and Keeping Motivation
Early on in the evaluation of this treatment, it became clear that not all the adolescents enrolled in an open pilot trial (Ehrenreich et al. 2009) were pursuing treatment out of their own desire to change. Rather, some adolescents had been encouraged to seek services because some other person or agency believed it necessary (e.g., parents, school counselor). Techniques based on the seminal work by Miller and Rollnick (2002) have been included in the protocol as motivational enhancement techniques have proven useful with youth in other forms of treatment (e.g., Gowers and Smyth 2004). Although this material is described as an optional treatment section, it is conceptualized as a set of techniques therapists may opt to use at any point throughout treatment. We have chosen to define it as an optional treatment section to encourage therapists to track the use of this material across sessions, aiding in the further evaluation of the role of motivational enhancement techniques in the protocol.
Optional Treatment Section Two: Keeping Safe/Dealing with Tough Times
This portion of the protocol is designed to provide clinicians with ideas for, and the flexibility sometimes necessary to, manage events that might otherwise interfere with the adolescent’s ability to benefit from this intervention. Treatment impairing situations might include a significant decrease in the adolescent’s functioning (e.g., significant worsening of the adolescent’s depressive symptoms) or an increase in suicidal ideation. Should such an event arise, this portion of the protocol includes suggestions for creating a safety plan as well as guidelines for ER strategies the adolescent may be able to use to remain safe. Perhaps most importantly, one or more sessions from this treatment section can be inserted into any portion of the protocol, allowing the clinician to flexibly respond to crises, which cannot be adequately handled by material being covered at that point in the protocol.
Optional Treatment Section Three: Parenting the Emotional Adolescent
As noted above, the literature on parental socialization of emotion suggests that parents may play a role in shaping how children and adolescents deploy or regulate their emotions. However, parental involvement in the treatment of an adolescent’s ER difficulties may vary, given heterogeneity in parental psychopathology and family circumstances among individual adolescent clients. Therefore, similar to traditional CBT formats, the UP-Y provides several options for increasing or decreasing the amount of parental involvement in an adolescent’s treatment. At the start of required treatment section one, the therapist and adolescent confer on the role of the parent in each treatment session and determine when and how the parent should participate in these adolescent-focused sessions. Adolescents are not given the option of no parental involvement, but may set appropriate boundaries about the circumstances for transmitting information to parents about adolescent session content and homework assignments. Most typically, the parent is invited to join the adolescent for 5–10 min at the end of a given session to review session material and discuss plans and/or barriers for homework.
In addition to this general parent involvement, therapists are provided with the option to include up to three additional sessions with the parent(s) alone as part of optional treatment section three. One or all of the optional parenting sessions may be used at any time during the course of treatment. Content for these optional parenting sessions is divided into three topic areas: (1) independence, where the parent is encouraged to aid the adolescent in making appropriate personal choices and developmental transitions; (2) consistency, in which appropriate parental discipline and positive reinforcement strategies are reviewed; and (3) empathy, during which parents are given a better understanding of the difficulties their adolescent is coping with at the present time and the strategies they are learning in treatment to help them with these concerns. In the UP-Y, the acronym “I–C–E” is utilized to help parents recall these three topics, along with the notion that by using their I–C–E skills, parents can help their adolescent to “keep cool” and use appropriate regulation strategies when dealing with difficult situations.
In discussing independence with parents, the therapist reviews the function of parental behaviors like overprotection or poor psychological autonomy granting in the course of child and adolescent emotional disorders and encourages parents to consider how to shape appropriate independent choices in their adolescent. Within this topic area, there is also an option to further explore parental distress about increases in an adolescent’s independence and autonomy that may result from the lessening of emotional disorder intensity. Discussion regarding the negative reinforcement function of resolving parental distress through excessive control or limit-setting strategies with their adolescent may be provided.
Consistency session(s) were originally developed in the UP-Y with the goal of helping parents that may be having a moderate degree of conflict with their adolescent or demonstrating poor or inappropriate discipline strategies in their behavior management. These topics include the use of positive reinforcement, including labeled praises, appropriate consequences for adolescent misbehavior, rule-setting, and other parental behavioral management strategies. This topic area may be provided in a more extensive manner for parents with particular deficits in their behavior management style. However, it is not designed for use with the families of adolescents that may be presenting with more extensive or primary behavioral problems.
The empathy session(s) of this optional treatment section may be generally used with most families of adolescents with emotional disorders. In this section, the therapist reviews the adolescent’s emotional difficulties more thoroughly with the parent(s) and provides further rationale to support the use of the UP-Y treatment strategies that may help. In this regard, the empathy session(s) provided in this optional treatment section is largely extensions of the brief time spent with parents during individual treatment sessions. Wherever possible, the therapist is encouraged to have parents directly experience or practice the UP-Y techniques and practice them, along with their adolescent, to act as models of appropriate regulation strategy usage.
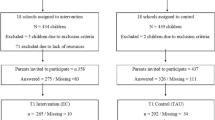
Current Research on the UP-Y and Directions for Future Research
An open trial investigation examining the preliminary feasibility and effects of the UP-Y was recently completed (Ehrenreich et al. 2009). The open trial employed a slightly earlier version of the UP-Y that emphasized the same primary treatment components and broad emotion focus, but which was limited to 16 sessions in duration. Twelve adolescents (ages 12–17, 57% male) with any principal anxiety or depressive disorder, as determined by the Adolescent Disorders Interview Schedule for DSM-IV, Child- and Parent-report Version (ADIS-IV-C/P; Albano and Silverman 1996) completed this open trial. According to the pre-treatment ADIS-IV-C/P, approximately 42% of participants met criteria only for anxiety disorders, 58% met criteria for both depressive and anxiety disorders, with no participants meeting criteria for depressive disorders only. In addition to the ADIS-IV-C/P, adolescents and their parents completed questionnaires about the adolescent’s anxiety and mood symptoms (Revised Child Anxiety and Depression Scale [RCADS]; Chorpita et al. 2000b) and ER strategies for anger, sadness, and worry (Children’s Emotion Management Scales [CEMS]; Zeman et al. 2001), at pre- and post-treatment, and again at 3- and 6-month follow-up. Results of the open trial investigation (further details on which may be found in Ehrenreich et al. 2009) demonstrated that clinical severity ratings (CSR) of all anxiety and depressive disorders reported for individual adolescents on the ADIS-IV-C/P at pre-treatment (referred to collectively as pre-treatment emotional disorder CSRs) significantly reduced at post-treatment. These treatment gains were also maintained at 3- and 6-month follow-up assessment. Results using the RCADS indicated that adolescents’ report of anxiety and depressive symptoms also declined from pre- to post-treatment assessments, and continued to decline at the 3-month follow-up, with maintenance of gains at 6-month follow-up.
When examining parental report of ER in this open trial, results indicate that the UP-Y may impact parents’ perceptions of an adolescent’s regulation above and beyond the regulation of the emotion that is specifically troubling the adolescent (Laird et al. 2009). This is in contrast to recent findings on CBT protocols for anxiety disorders in children and adolescents, which indicate that CBT is associated with improved parent-reported ER in the context of worry, but not other emotions (Suveg et al. in press). In examining results for the CEMS, adolescents in the UP-Y open trial demonstrated reductions in overall emotion dysregulation at post-treatment, t(8) = 3.86, p < .01, and positive gains in overall emotion coping at a 3-month follow-up, t(9) = –2.73, p < .05. Paired t-tests comparing emotional dysregulation and emotion coping at 3- and 6-month follow-ups were not significant, t(9) = .287, p < .78, and t(9) = .126, p = .90, respectively. Similar to previous findings, adolescents exhibited improvements in worry-related emotional dysregulation, t(8) = 3.26, p = .01. A trend evidencing improved coping with worry through the 6-month follow-up was also observed, F(3,21) = 2.77, p = .07. In contrast to results for CBT targeting youth anxiety alone, adolescents in the current study exhibited improvements in dysregulation of sadness at post-treatment, t(9) = 4.74, p = .001, and again at 3-month follow-up, t(10) = 3.95, p < .01. Paired t-tests comparing sadness dysregulation at 3- and 6-month follow-ups were not significant, t(9) = −.635, p = .541, suggesting a maintenance of the treatment gains. Following treatment, adolescents also demonstrated better coping with anger, F(1,8) = 6.13, p < .05. Taken together, these preliminary results suggest that the UP-Y, which frames CBT strategies in a broader emotion context appropriate for various emotional disorders, may aid adolescents by decreasing emotion dysregulation and improving coping across multiple emotions.
In addition to demonstrating the feasibility of the UP-Y as a treatment for emotional disorders, the results of this initial open trial investigation of the UP-Y also indicated several promising trends with regard to the possibility that ER is more broadly impacted by the UP-Y. However, many of these trends only approached significance, likely due to the small sample size employed. The open trial sample was also limited in the recruitment of individuals who were primarily or principally depressed. We are currently conducting a randomized controlled trial (RCT) of the UP-Y with a larger sample size and recruitment efforts targeting a more equivalent number of participants with anxiety and depressive disorders. We have also significantly broadened our assessment of ER in this new trial. Although the UP-Y specifically posits an ER framework inspired by Gross and Thompson (2007), the open trial did not tailor measurement of ER to assess the degree to which corresponding ER skills were taught effectively or acquired in each section of treatment.
For the current trial, each section of the UP-Y (including optional sections, as appropriate) is followed by a short assessment that examines ER skills targeted in the preceding section. For instance, the first required section of the protocol, Getting to Know Your Emotions and Behaviors, is devoted to educating adolescents about emotions. Before and after this section is completed, adolescents now complete the Emotional Expression Scale for Children (EESC; Penza-Clyve and Zeman 2002). The EESC is a 16-item scale that assesses an individual’s emotion awareness. Such assessment allows us to examine gains in general emotion awareness following this section on emotion education. Similarly, required section three, Being Flexible in Your Thinking, focuses on teaching adolescents cognitive reappraisal skills to increase flexibility around their automatic appraisals. Adolescents now complete the Children’s Automatic Thoughts Scale (CATS; Schniering and Rapee 2002) and other measures of reappraisal before and after this section to discern the degree to which this section effectively promotes such skills.
Summary and Conclusion
In this review, we presented findings that specify both a rationale and a need for a transdiagnostic approach to treatment, based on high comorbidity rates between anxiety and depression as well as common vulnerabilities between these disorders. We also outlined the modal model of ER, its application to youth with emotional disorders, and its viability as a theoretical model for therapeutic intervention with adolescents exhibiting a range of anxiety and depressive disorders. We described the UP-Y protocol and provided initial research findings that lend evidence to its utility in decreasing internalizing symptomatology and reducing overall emotion dysregulation across a broader spectrum of emotions. Research regarding ER and associated intervention models is obviously quite new and the future of such work is not yet clear. While the modal model of ER seems to map well onto the psychopathology of common emotional disorders in youth, related intervention research is really in its infancy and is fraught with needs to better examine the acceptability, efficacy, and effectiveness of related treatment approaches, including the UP-Y, as well as the potential mechanisms of change in an emotion-focused intervention. For instance, a greater understanding of the role emotional development plays in the course of treatment for youth emotional disorders is certainly required. Further research about the relative benefit of adding emotion-focused components to evidence-based treatments like CBT for the full array of emotional disorders is also needed. Specifically, the incremental utility of using an emotion-focused intervention approach, such as the UP-Y, in lieu of CBT for anxiety or depressive disorders is unclear. Many of the components in the UP-Y mirror CBT and other evidence-based treatment components that have been formatted in an emotion-focused manner as to be applicable to a larger audience of emotionally dysregulated adolescents. This overlap with evidence-based treatment components is purposeful, as research has demonstrated the efficacy of CBT for child and adolescent internalizing disorders, and we believe such overlap is unlikely to diminish the current protocol’s attractiveness to a wider audience of clinicians, particularly those treating highly comorbid or more challenging adolescent clients. However, further research will be necessary to clarify whether clinicians find this approach to have relative benefit for their practice versus evidence-based treatments aimed at specific disorders or a narrow class of disorders.
As discussed previously, the open trial provided us a first step toward better understanding the acceptability and feasibility of the UP-Y. Both the diagnostic-level and ER findings are exciting and hopeful. Although we are early into the RCT that may help us to better understand the efficacy of this approach with adolescents experiencing emotional disorders, we are also thinking ahead to the future of intervention research on the UP-Y. If the UP-Y demonstrates efficacy in its current trial, future directions for the UP-Y will include testing the potential utility of this intervention approach with adolescents exhibiting anxiety, depression, or a combination of emotional disorders presenting in a variety of settings (e.g., schools, pediatric settings, residential facilities) and with varying life circumstances. Ultimately, further research that elucidates changes in ER across physiological, cognitive, and experiential methods of assessment in the course of the UP-Y will be needed to clarify the role ER plays in both youth emotional disorders and their amelioration over time.
References
Albano, A. M., Chorpita, B. F., & Barlow, D. H. (2003). Anxiety disorders. In E. J. Mash & R. A. Barkley (Eds.), Child psychopathology (2nd ed., pp. 279–329). New York: The Guilford Press.
Albano, A. M., & Silverman, W. K. (1996). Clinician manual for the Anxiety Disorders Interview Schedule for DSM-IV-Child Version. San Antonio, TX: The Psychological Corporation.
Anderson, E. R., & Hope, D. A. (2007). A review of the tripartite model for understanding the link between anxiety and depression in youth. Clinical Psychology Review, 28(2), 275–287. doi:10.1016/j.cpr.2007.05.004.
Angold, A., Costello, E. J., & Erkanli, A. (1999). Comorbidity. Journal of Child Psychology and Psychiatry, and Allied Disciplines, 40, 57–87. doi:10.1111/1469-7610.00424.
Barlow, D. H., Allen, L. B., & Choate, M. (2004). Toward a unified treatment for emotional disorders. Behavior Therapy, 35, 205–230. doi:10.1016/S0005-7894(04)80036-4.
Barlow, D. H., Chorpita, B. F., & Turovsky, J. (1996). Fear, panic, anxiety, and disorders of emotion. In D. A. Hope (Ed.), Perspectives on anxiety, panic, and fear (pp. 251–328). Lincoln: University of Nebraska Press.
Barmish, A. J., & Kendall, P. C. (2005). Should parents be co-clients in cognitive-behavioral therapy for anxious youth? Journal of Clinical Child and Adolescent Psychology, 34(3), 569–581. doi:10.1207/s15374424jccp3403_12.
Barrett, P. M., Dadds, M. R., & Rapee, R. M. (1996). Family treatment of childhood anxiety: A controlled trial. Journal of Consulting and Clinical Psychology, 64, 333–342. doi:10.1037/0022-006X.64.2.333.
Beck, J. S. (1995). Cognitive therapy: Basics and beyond. New York: The Guilford Press.
Beck, A. T., Rush, A. J., Shaw, B. P., & Emery, G. (1979). Cognitive therapy of depression. New York: The Guilford Press.
Bell-Dolan, D. J., Reaven, N. M., & Peterson, L. (1993). Depression and social functioning: A multidimensional study of the linkages. Journal of Clinical Child Psychology, 22, 306–315. doi:10.1207/s15374424jccp2203_1.
Biederman, J., Faraone, S., Mick, E., & Lelon, E. (1995). Psychiatric comorbidity among referred juveniles with major depression: Fact or artifact? Journal of the American Academy of Child and Adolescent Psychiatry, 34, 579–590.
Biederman, J., Rosenbaum, J. F., Hirshfeld, D. R., Faraone, V., Bolduc, E., Gersten, M., et al. (1990). Psychiatric correlates of behavioral inhibition in young children of parents with and without psychiatric disorders. Archives of General Psychiatry, 47, 21–26.
Bishop, S. J., Dalgleish, T., & Yule, W. (2004). Memory for emotional stories in high and low depressed children. Memory, 12, 214–230. doi:10.1080/09658210244000667. Hove, England.
Blankstein, K. R., Flett, G. L., & Johnston, M. E. (1992). Depression, problem-solving ability, and problem-solving appraisals. Journal of Clinical Psychology, 48, 749–759. doi:10.1002/1097-4679(199211)48:6<749::AID-JCLP2270480609>3.0.CO;2-V.
Bögels, S. M., van Dongen, L., & Muris, P. (2003). Family influences on dysfunctional thinking in anxious children. Infant and Child Development, 12, 243–252. doi:10.1002/icd.288.
Bögels, S. M., & Zigterman, D. (2000). Dysfunctional cognitions in children with social phobia, separation anxiety disorder, and generalised anxiety disorder. Journal of Abnormal Child Psychology, 28, 205–211. doi:10.1023/A:1005179032470.
Borkovec, T. D., Abel, J. L., & Newman, H. (1995). Effects of psychotherapy on comorbid conditions in generalized anxiety disorder. Journal of Consulting and Clinical Psychology, 63, 479–483. doi:10.1037/0022-006X.63.3.479.
Borkovec, T. D., & Roemer, L. (1995). Perceived functions of worry among generalized anxiety disorder subjects: Distraction from more emotionally distressing topics? Journal of Behavior Therapy and Experimental Psychiatry, 26, 25–30. doi:10.1016/0005-7916(94)00064-S.
Bradley, S. J. (2000). Affect regulation and the development of psychopathology. New York: The Guilford Press.
Brady, E. U., & Kendall, P. C. (1992). Comorbidity of anxiety and depression in children and adolescents. Psychological Bulletin, 111, 244–255. doi:10.1037/0033-2909.111.2.244.
Brown, T. A., Antony, M. M., & Barlow, D. H. (1995). Diagnostic comorbidity in panic disorder: Effect on treatment outcome and course of comorbid diagnoses following treatment. Journal of Consulting and Clinical Psychology, 63, 408–418. doi:10.1037/0022-006X.63.3.408.
Brown, T. A., Chorpita, B. F., & Barlow, D. H. (1998). Structural relationships among dimensions of the DSM-IV anxiety and mood disorders and dimensions of negative affect, positive affect, and autonomic arousal. Journal of Abnormal Psychology, 107, 179–192. doi:10.1037/0021-843X.107.2.179.
Burwell, R. A., & Shirk, S. R. (2007). Subtypes of rumination in adolescence: Association between brooding, reflection, depressive symptoms, and coping. Journal of Clinical Child and Adolescent Psychology, 36, 56–65. doi:10.1207/s15374424jccp3601_6.
Campbell-Sills, L., & Barlow, D. H. (2007). Incorporating emotion regulation conceptualizations and treatments of anxiety and mood disorders. In J. J. Gross (Ed.), Handbook of ER. New York: The Guilford Press.
Caspi, A., Moffitt, T. E., Newman, D. L., & Silva, P. A. (1996). Behavioral observations at 3 years predict adult psychiatric disorders. Archives of General Psychiatry, 53, 1033–1039.
Chambers, D. (2008). Introduction: Advancing implementation research in mental health. Administration and Policy in Mental Health and Mental Health Services Research; Special issue: Improving mental health services, 35, 1–2.
Chaplin, T. M. (2006). Anger, happiness, and sadness: Associations with depressive symptoms in late adolescence. Journal of Youth and Adolescence, 35(6), 1573–6601. doi:10.1007/s10964-006-9033-x.
Chorpita, B. F., & Daleiden, E. L. (2002). Tripartite dimensions of emotion in a child clinical sample: Measurement strategies and implications for clinical utility. Journal of Consulting and Clinical Psychology, 70, 1150–1160. doi:10.1037/0022-006X.70.5.1150.
Chorpita, B. F., Plummer, C. M., & Moffitt, C. E. (2000a). Relations of tripartite dimensions of emotion to childhood anxiety and mood disorders. Journal of Abnormal Child Psychology, 28, 299–310. doi:10.1023/A:1005152505888.
Chorpita, B. F., Yim, L., Moffitt, C. E., Umemoto, L. A., & Francis, S. E. (2000b). Assessment of symptoms of DSM-IV anxiety and depression in children: A revised child anxiety and depression scale. Behaviour Research and Therapy, 38, 835–855. doi:10.1016/S0005-7967(99)00130-8.
Cicchetti, D., Ackerman, B. P., & Izard, C. E. (1995). Emotions and emotion regulation in developmental psychopathology. Development and Psychopathology, 7, 1–10. Special issue.
Clark, D. A., Steer, R. A., & Beck, A. T. (1994). Common and specific dimensions of self-reported anxiety and depression: Implications for the cognitive and tripartite models. Journal of Abnormal Psychology, 103, 645–654. doi:10.1037/0021-843X.103.4.645.
Clark, L. A., & Watson, D. (1991). Tripartite model of anxiety and depression: Evidence and taxonomic implications. Journal of Abnormal Psychology, 100, 316–336. doi:10.1037/0021-843X.100.3.316.
Clarke, G. N., DeBar, L. L., & Lewinsohn, P. M. (2003). Cognitive behavioral group treatment for adolescent depression. In A. E. Kazdin & J. R. Weisz (Eds.), Evidence-based psychotherapies for children and adolescents (pp. 120–134). New York: The Guilford Press.
Compas, B. E., Boyer, M. C., Stanger, C., Colletti, R. B., Thomsen, A. H., Dufton, L. M., et al. (2006). Latent variable analysis of coping, anxiety/depression, and somatic symptoms in adolescents with chronic pain. Journal of Consulting and Clinical Psychology, 74(6), 1132–1142. doi:10.1037/0022-006X.74.6.1132.
Compas, B. E., Connor-Smith, J. K., Saltzman, H., Thomsen, A. H., & Wadsworth, M. E. (2001). Coping with stress during childhood and adolescence: Progress, problems, and potential in theory and research. Psychological Bulletin, 127, 87–127. doi:10.1037/0033-2909.127.1.87.
Coyne, J. C. (1976). Depression and the response of others. Journal of Abnormal Psychology, 85, 186–193. doi:10.1037/0021-843X.85.2.186.
Creswell, C., Schniering, C. A., & Rapee, R. M. (2005). Threat interpretation in anxious children and their mothers: Comparison with non-clinical children and the effects of treatment. Behaviour Research and Therapy, 43, 1375–1381. doi:10.1016/j.brat.2004.10.009.
Cummings, E. M., & Davies, P. T. (1999). Depressed parents and family functioning: Interpersonal effects and children’s functioning and development. In T. E. Joiner & J. C. Coyne (Eds.), The interactional nature of depression: Advances in interpersonal approaches (pp. 299–327). Washington, DC: American Psychological Association.
Denham, S. A. (1998). Emotional development in young children. New York: The Guilford Press.
Denham, S. A., & Burton, R. (1996). A socio-emotional intervention program for at risk four year-olds. Journal of School Psychology, 34, 225–245. doi:10.1016/0022-4405(96)00013-1.
Ehrenreich, J. T., Buzzella, B. A., Trosper, S. E., Bennett, S. M., Wright, L. R., & Barlow, D. H. (2008). The Unified Protocol for treatment of emotional disorders in adolescents. Unpublished manuscript, Boston University.
Ehrenreich, J. T., Buzzella, B. A., Wright, L. R., & Barlow, D. H. (2009). An open-trial evaluation of a unified treatment for adolescents with emotional disorders. Manuscript in preparation.
Eisenberg, N., Cumberland, A., & Spinrad, T. L. (1998). Parental socialization of emotion. Psychological Inquiry, 9, 241–273. doi:10.1207/s15327965pli0904_1.
Eisenberg, N., Fabes, R. A., & Murphy, B. C. (1996). Parents’ reactions to children’s negative emotions: Relations to children’s social competence and comforting behavior. Child Development, 67, 2227–2247. doi:10.2307/1131620.
Eley, T. C. (2001). Contributions of behavioral genetics research: Quantifying genetic, shared environmental and nonshared environmental influences. In M. W. Vasey & M. R. Dadds (Eds.), Developmental psychopathology of anxiety (pp. 45–59). London: Oxford University Press.
Eley, T. C., & Stevenson, J. (1999). Using genetic analyses to clarify the distinction between depressive and anxious symptoms in children and adolescents. Journal of Abnormal Child Psychology, 27, 105–114. doi:10.1023/A:1021947113860.
Field, T., Healy, B., Goldstein, S., & Gutherz, M. (1990). Behavior-state matching and synchrony in mother–infant interactions of nondepressed versus depressed dyads. Developmental Psychology, 26, 7–14. doi:10.1037/0012-1649.26.1.7.
Francis, G., Last, C. G., & Strauss, C. C. (1992). Avoidant disorder and social phobia in children and adolescents. Journal of the American Academy of Child and Adolescent Psychiatry, 31, 1086–1089.
Fuchs, D., & Thelen, M. H. (1988). Children’s expected interpersonal consequences of communicating their affective state and reported likelihood of expression. Child Development, 59, 1314–1322. doi:10.2307/1130494.
Gar, N. S., & Hudson, J. L. (2008). An examination of the interactions between mothers and child with anxiety disorders. Behaviour Research and Therapy, 46, 1266–1274. doi:10.1016/j.brat.2008.08.006.
Garber, J., Braafladt, N., & Weiss, B. (1995). Affect regulation in depressed and nondepressed children and young adolescents. Development and Psychopathology, 7, 93–115.
Gelfand, D. M., & Teti, D. M. (1990). The effects of maternal depression on children. Clinical Psychology Review, 10, 320–354. doi:10.1016/0272-7358(90)90065-I.
Ginsburg, G. S., Silverman, W. K., & Kurtines, W. M. (1995). Family involvement in treating children with phobic and anxiety disorders. International Review of Psychiatry (Abingdon, England), 14, 143–154. doi:10.1080/09540260220132662.
Goodman, S. H., & Gotlib, I. H. (1999). Risk for psychopathology in the children of depressed mothers: A developmental model for understanding mechanisms of transmission. Psychological Review, 106, 458–490. doi:10.1037/0033-295X.106.3.458.
Goodyer, I. M., & Cooper, P. (1993). A community study of depression in adolescent girls: II. The clinical features of identified disorder. The British Journal of Psychiatry, 163, 374–380. doi:10.1192/bjp.163.3.374.
Gordon, D., Burge, D., Hammen, C., Adrian, C., Jaenicke, C., & Hiroto, D. (1989). Observations of interactions of depressed women with their children. The American Journal of Psychiatry, 146, 50–55.
Gosselin, P., Langlois, F., Freeston, M. H., Ladouceur, R., Laberge, M., & Lemay, D. (2007). Cognitive variables related to worry among adolescents: Avoidance strategies and faulty beliefs about worry. Behaviour Research and Therapy, 45, 225–233. doi:10.1016/j.brat.2006.03.001.
Gosselin, M. J., Trois-Riviéres, P. Q., & Marcotte, D. (1997). The role of self-perceived problem-solving skills in relation with depression during adolescence. Science et Comportement, 25, 299–314.
Gotlib, I. H., & Krasnoperova, E. (1998). Biased information processing as a vulnerability factor for depression. Behavior Therapy, 29, 603–617. doi:10.1016/S0005-7894(98)80020-8.
Gottman, J. M., Katz, L. F., & Hooven, C. (1997). Meta-emotion: How families communicate emotionally. Mahwah, NJ: Erlbaum.
Gowers, S. G., & Smyth, B. (2004). The impact of a motivational assessment interview on initial response to treatment in adolescent anorexia nervosa. European Eating Disorders Review, 12, 87–93. doi:10.1002/erv.555.
Gross, J. J. (1998). Antecedent- and response-focused ER: Divergent consequences for experience, expression, and physiology. Journal of Personality and Social Psychology, 74, 224–237. doi:10.1037/0022-3514.74.1.224.
Gross, J. J. (2003). ER: Affective, cognitive, and social consequences. Psychophysiology, 39, 281–291. doi:10.1017/S0048577201393198.
Gross, J. J., & Thompson, R. A. (2007). ER: Conceptual foundations. In J. J. Gross (Ed.), Handbook of emotion regulation. New York: The Guilford Press.
Hadwin, J., Frost, S., French, C. C., & Richards, A. (1997). Cognitive processing and anxiety in mainstream children: Trait anxiety and interpretation bias. Journal of Abnormal Psychology, 106, 486–490.
Hammen, C. (1991). Depression runs in families: The social context of risk and resilience in children of depressed mothers. New York: Springer.
Hammen, C., & Rudolph, K. D. (2003). Childhood depression. In E. J. Mash & R. A. Barkley (Eds.), Child psychopathology (2nd ed., pp. 233–278). New York: The Guilford Press.
Hannesdottir, K. H., & Ollendick, T. H. (2007). The role of emotion regulation in the treatment of child anxiety disorders. Clinical Child and Family Psychology Review, 10(3), 1096–4037. doi:10.1007/s10567-007-0024-6.
Hollon, S. D., Thase, M. E., & Markowitz, J. C. (2002). Treatment and prevention of depression. Psychological Science in the Public Interest, 3, 39–77. doi:10.1111/1529-1006.00008.
Hops, H., Biglan, A., Sherman, L., Aurther, J., Friedman, L., & Osteen, V. (1987). Home observations of family interactions of depressed women. Journal of Consulting and Clinical Psychology, 55, 341–346. doi:10.1037/0022-006X.55.3.341.
Invarsson, T., Gillberg, C., & Arvidsson, T. (2002). The Youth Self-Report (YSR) and the Depression Self-Rating Scale (DSRS) as measures of depression and suicidality among adolescents. European Child & Adolescent Psychiatry, 11, 31–37. doi:10.1007/s007870200005.
Izard, C. E., & Bear, G. (2001). Head Start/ECAP emotions curriculum. Newark, DE: University of Delaware Instructional Resources Center.
Jacques, H. A. K., & Mash, E. J. (2004). A test of the tripartite model of anxiety and depression in elementary and high school boys and girls. Journal of Abnormal Child Psychology, 32, 13–25. doi:10.1023/B:JACP.0000007577.38802.18.
Jenson-Doss, A., & Weisz, J. R. (2006). Syndrome co-occurrence and treatment outcomes in youth mental health clinics. Journal of Consulting and Clinical Psychology, 74, 416–425. doi:10.1037/0022-006X.74.3.416.
Joiner, T. E., Jr., Alfano, M. S., & Metalsky, G. I. (1992). When depression breeds contempt: Reassurance-seeking, self-esteem, and rejection of depressed college students by their roommates. Journal of Abnormal Psychology, 101, 165–173. doi:10.1037/0021-843X.101.1.165.
Joiner, T. E., Metalsky, G. I., Katz, J., & Beach, S. R. H. (1999). Depression and excessive reassurance-seeking. Psychological Inquiry, 10, 269–278. doi:10.1207/S15327965PLI1004_1.
Kashani, J. H., & Orvaschel, H. (1990). A community study of anxiety in children and adolescents. The American Journal of Psychiatry, 147, 313–318.
Katz, J., Beach, S. R. H., & Joiner, T. E., Jr. (1998). When does partner devaluation predict depression? Prospective moderating effects of reassurance-seeking and self-esteem. Personal Relationships, 5, 409–421. doi:10.1111/j.1475-6811.1998.tb00179.x.
Kazdin, A. E., Esveldt-Dawson, K., Sherick, R. B., & Colbus, D. (1985). Assessment of overt behavior and childhood depression among psychiatrically disturbed children. Journal of Consulting and Clinical Psychology, 53, 201–210. doi:10.1037/0022-006X.53.2.201.
Keenan, K. (2000). Emotion dysregulation as a risk factor for child psychopathology. Clinical Psychology: Science and Practice, 7, 418–434. doi:10.1093/clipsy/7.4.418.
Kendall, P. C. (2000). Cognitive-behavioral therapy for anxious children: Treatment manual. Ardmore, PA: Workbook Publishing Inc.
Kendall, P. C., Aschenbrand, S., & Hudson, J. (2003). Child-focused treatment of anxiety. In A. E. Kazdin & J. R. Weisz (Eds.), Empirically-based psychotherapies for children and adolescents (pp. 81–100). New York: The Guilford Press.
Kendall, P. C., & Brady, E. U. (1995). Comorbidity in the anxiety disorders of childhood: Implications for validity and clinical significance. In K. D. Craig & K. S. Dobson (Eds.), Anxiety and depression in adults and children (pp. 3–36). Thousand Oaks, CA: Sage Publications.
Kendall, P. C., Brady, E. U., & Verduin, T. L. (2001). Comorbidity in childhood anxiety disorders and treatment outcome. Journal of the American Academy of Child and Adolescent Psychiatry, 40, 787–794. doi:10.1097/00004583-200107000-00013.
Kendall, P. C., & Hedtke, K. A. (2006). Cognitive-behavioral therapy for anxious children: Therapist manual (3rd ed.). Ardmore, PA: Workbook Publishing Inc.
Kendall, P. C., Hudson, J., Choudhury, M., Webb, A., & Pimentel, S. (2005). Cognitive-behavioral treatment for childhood anxiety disorders. In E. D. Hibbs & P. S. Jensen (Eds.), Psychosocial treatments for child and adolescent disorders: Empirically based strategies for private practice. Washington, DC: American Psychological Association.
Kendall, P. C., & Ingram, R. E. (1987). The future for cognitive assessment of anxiety: Let’s get specific. In L. Michelson & L. M. Ascher (Eds.), Anxiety and stress disorders: Cognitive-behavioral assessment and treatment (pp. 89–104). The Guilford Press: New York.
Kendler, K. S., Prescott, C. A., Myers, J., & Neale, M. C. (2003). The structure of genetic and environmental risk factors for common psychiatric and substance use disorders in men and women. Archives of General Psychiatry, 60, 929–937. doi:10.1001/archpsyc.60.9.929.
Kim, E. J. (2005). The effect of decreased safety behaviors on anxiety and negative thoughts in social phobics. Journal of Anxiety Disorders, 19, 69–86. doi:10.1016/j.janxdis.2003.11.002.
King, N. J., Heyne, D., & Ollendick, T. H. (2005). Cognitive-behavioral treatments for anxiety and phobic disorders in children and adolescents: A review. Behavioral Disorders, 30, 241–257.
King, N. J., Ollendick, T. H., & Gullone, E. (1991). Negative affectivity in children and adolescents: Relations between anxiety and depression. Clinical Psychology Review, 11, 441–459. doi:10.1016/0272-7358(91)90117-D.
Kocovski, N. L., Endler, N. S., Rector, N. A., & Flett, G. L. (2005). Ruminative coping and post-event processing in social anxiety. Behaviour Research and Therapy, 43(8), 971–984. doi:10.1016/j.brat.2004.06.015.
Kovacs, M., & Devlin, B. (1998). Internalizing disorders in childhood. Journal of Child Psychology and Psychiatry, and Allied Disciplines, 39, 47–63. doi:10.1017/S0021963097001765.
Kovacs, M., Sherrill, J., George, C. J., Pollock, M., Tumuluru, R. V., & Ho, V. (2006). Contextual emotion-regulation therapy for childhood depression: Description and pilot testing of a new intervention. Journal of the American Academy of Child and Adolescent Psychiatry, 45, 892–903. doi:10.1097/01.chi.0000222878.74162.5a.
Ladouceur, C. D., Dahl, R. E., & Williamson, D. E. (2005). Altered emotional processing in pediatric anxiety, depression, and comorbid anxiety-depression. Journal of Abnormal Child Psychology, 33, 165–177. doi:10.1007/s10802-005-1825-z.
Laird, E. A., Buzzella, B. A., & Ehrenreich, J. T. (2009, March). Changes in adolescents’ emotion regulation following use of the Unified Protocol for the Treatment of Emotional Disorders in Youth. Poster to be Presented at the Annual Conference of the Anxiety Disorders Association of America, Santa Ana Pueblo, New Mexico.
Lewinsohn, P. M., & Clarke, G. N. (1999). Psychosocial treatments for adolescent depression. Clinical Psychology Review, 19, 329–342. doi:10.1016/S0272-7358(98)00055-5.
Lonigan, C. J., & Phillips, B. M. (2001). Temperamental basis of anxiety disorders in children. In M. W. Vasey & M. R. Dadds (Eds.), The developmental psychopathology of anxiety (pp. 60–91). New York: Oxford University Press.
Mash, E. J., & Wolfe, D. A. (2002). Abnormal child psychology (2nd ed.). Belmont, CA: Wadsworth.
McKeown, R. E., Garrison, C. Z., Jackson, K. L., Cuffe, S. P., Addy, C. L., & Waller, J. L. (1997). Family structure and cohesion, and depressive symptoms in adolescents. Journal of Research on Adolescence, 7, 267–281. doi:10.1207/s15327795jra0703_2.
McLeod, B. D., Weisz, J. R., & Wood, J. J. (2007a). Examining the association between parenting and childhood depression: A meta-analysis. Clinical Psychology Review, 27, 986–1003. doi:10.1016/j.cpr.2007.03.001.
McLeod, B. D., Wood, J. J., & Weisz, J. R. (2007b). Examining the association between parenting and childhood anxiety: A meta-analysis. Clinical Psychology Review, 27, 155–172. doi:10.1016/j.cpr.2006.09.002.
Mennin, D. S., Holaway, R., Fresco, D. M., Moore, M. T., & Heimberg, R. G. (2007). Delineating components of emotion and its dysregulation in anxiety and mood psychopathology. Behavior Therapy, 38, 284–302. doi:10.1016/j.beth.2006.09.001.
Micco, J. A., & Ehrenreich, J. T. (2008). Children’s interpretation and avoidant response biases in response to non-salient and salient situations: Relationships with mothers’ threat perception and coping expectations. Journal of Anxiety Disorders, 22, 371–385. doi:10.1016/j.janxdis.2007.03.009.
Miller, W. R., & Rollnick, S. (2002). Motivational interviewing: Preparing people for change (2nd ed.). New York: The Guilford Press.
Milosevic, I., & Radomsky, A. S. (2008). Safety behavior does not necessarily interfere with exposure therapy. Behaviour Research and Therapy, 46, 1111–1118. doi:10.1016/j.brat.2008.05.011.
Muris, P., Rapee, R., Meesters, C., Schouten, E., & Geers, M. (2003). Threat perception abnormalities in children: The role of anxiety disorders symptoms, chronic anxiety, and state anxiety. Journal of Anxiety Disorders, 17, 271–287. doi:10.1016/S0887-6185(02)00199-8.
Muris, P., Steerneman, P., Merckelback, H., & Meesters, C. (1996). The role of parental fearfulness and modeling in children’s fear. Behaviour Research and Therapy, 34, 265–268. doi:10.1016/0005-7967(95)00067-4.
Nolen-Hoeksema, S., Morrow, J., & Fredrickson, B. L. (1993). Response styles and the duration of episodes of depressed moods. Journal of Abnormal Psychology, 102, 20–28. doi:10.1037/0021-843X.102.1.20.
Oliver, J. M., Handal, P. J., Finn, T., & Herdy, S. (1987). Depressed and nondepressed students and their siblings in frequent contact with their families: Depression and perceptions of the family. Cognitive Therapy and Research, 11, 501–515. doi:10.1007/BF01175359.
Oliver, N. S., & Page, A. C. (2003). Fear reduction during in vivo exposure to blood injection stimuli: Distraction vs attentional focusing. The British Journal of Clinical Psychology, 42, 13–25. doi:10.1348/014466503762841986.
Ollendick, T. H., King, N. J., & Chorpita, B. F. (2006). Empirically supported treatments for children and adolescents. In P. C. Kendall (Ed.), Child and adolescent therapy: Cognitive-behavioral procedures (pp. 492–520). New York: The Guilford Press.
Penza-Clyve, S., & Zeman, J. (2002). Initial validation of the Emotion Expression Scale for Children (EESC). Journal of Clinical Child and Adolescent Psychology, 31(4), 540–547.
Potthoff, J. G., Holahan, C. J., & Joiner, T. E., Jr. (1995). Reassurance-seeking, stress generation, and depressive symptoms: An integrative model. Journal of Personality and Social Psychology, 68, 664–670. doi:10.1037/0022-3514.68.4.664.
Powers, M. B., Smits, J. A. J., & Telch, M. J. (2004). Disentangling the effects of safety-behavior utilization and safety-behavior availability during exposure-based treatment: A placebo-controlled trial. Journal of Consulting and Clinical Psychology, 72, 448–454. doi:10.1037/0022-006X.72.3.448.
Prins, P., & Ollendick, T. H. (2003). Cognitive change and enhanced coping: Missing mediational links in cognitive behavior therapy with anxiety-disordered children. Clinical Child and Family Psychology, 6, 87–105. doi:10.1023/A:1023730526716.
Quiggle, N. L., Garber, J., Panak, W. F., & Dodge, K. A. (1992). Social information processing in aggressive and depressed children. Child Development, 63, 1305–1320. doi:10.2307/1131557.
Radke-Yarrow, M. (1998). Children of depressed mothers: From early childhood to maturity. Cambridge: Cambridge University Press.
Rapee, R. M. (2002). The development and modification of temperamental risk for anxiety disorders: Prevention of a lifetime of anxiety? Biological Psychiatry, 52, 947–957. doi:10.1016/S0006-3223(02)01572-X.
Reid, S. C., Salmon, K., & Lovibond, P. F. (2006). Cognitive biases in childhood anxiety, depression, and aggression: Are they pervasive or specific? Cognitive Therapy and Research, 30, 531–549. doi:10.1007/s10608-006-9077-y.
Reijntjes, A. H. A., Stegge, H., & Terwogt, M. M. (2006). Children’s coping with peer rejection: The role of depressive symptoms, social competence, and gender. Infant and Child Development, 15, 989–1107. doi:10.1002/icd.435.
Rottenberg, J., & Vaughan, C. (2008). Emotion expression in depression: Emerging evidence for emotion context-sensitivity. In A. Vingerhoets & I. Nyklicek (Eds.), Emotion regulation: Conceptual and clinical Issues (pp. 125–139). New York: Springer Science and Business Media.
Saarni, C. (1999). The development of emotional competence. New York: The Guilford Press.
Salkovskis, P. M. (1991). The importance of behaviour in the maintenance of anxiety and panic: A cognitive account. Behavioural Psychotherapy, 19, 6–19.
Salkovskis, P. M., Clark, D. M., & Gelder, M. G. (1996). Cognition-behaviour links in the persistence of panic. Behaviour Research and Therapy, 34, 453–458. doi:10.1016/0005-7967(95)00083-6.
Samoilov, A., & Goldfried, M. R. (2000). Role of emotion in cognitive-behavior therapy. Clinical Psychology: Science and Practice, 7, 373–385. doi:10.1093/clipsy/7.4.373.
Schniering, C. A., & Rapee, R. M. (2002). Development and validation of a measure of children’s automatic thoughts: The Children’s Automatic Thoughts Scale. Behaviour Research and Therapy, 40, 1091–1109. doi:10.1016/S0005-7967(02)00022-0.
Sheeber, L., Allen, N., Davis, B., & Sorensen, E. (2000). Regulation of negative affect during mother–child problem-solving interactions: Adolescent depressive status and family processes. Journal of Abnormal Child Psychology, 28, 467–479. doi:10.1023/A:1005135706799.
Sica, C., Steketee, G., Ghisi, M., Chiri, L. R., & Franceschini, S. (2007). Metacognitive beliefs and strategies predict worry, obsessive-compulsive symptoms and coping styles: A preliminary prospective study on an Italian non-clinical sample. Clinical Psychology & Psychotherapy, 14(4), 258–268. doi:10.1002/cpp.520.
Sloan, T., & Telch, M. J. (2002). The effects of safety behavior and guided threat reappraisal on fear reduction during exposure: An experimental investigation. Behaviour Research and Therapy, 40, 235–251. doi:10.1016/S0005-7967(01)00007-9.
Southam-Gerow, M. A., & Kendall, P. C. (2000). A preliminary study of the emotion understanding of youth referred for treatment of anxiety disorders. Journal of Clinical Child Psychology, 29, 319–327. doi:10.1207/S15374424JCCP2903_3.
Southam-Gerow, M. A., & Kendall, P. C. (2002). Emotion regulation and understanding: Implications for child psychopathology and therapy. Clinical Psychology Review, 22, 189–222. doi:10.1016/S0272-7358(01)00087-3.
Stark, K. D., Hoke, J., Ballatore, M., Valdez, C., Scammaca, N., & Griffin, J. (2005). Treatment of child and adolescent depressive disorders. In E. D. Hibbs & P. S. Jensen (Eds.), Psychosocial treatments for child and adolescent disorders: Empirically based strategies for clinical practice (2nd ed., pp. 239–265). Washington, DC: American Psychological Association.
Stark, K. D., Humphrey, L. L., Laurent, J., Livingston, R., & Christopher, J. (1993). Cognitive, behavioral, and family factors in the differentiation of depressive and anxiety disorders during childhood. Journal of Consulting and Clinical Psychology, 61, 878–886. doi:10.1037/0022-006X.61.5.878.
Stegge, H., & Terwogt, M. M. (2007). Awareness and regulation of emotion in typical and atypical development. In J. J. Gross (Ed.), Handbook of emotion regulation (pp. 269–286). New York: The Guilford Press.
Suarez, L., & Bell-Dolan, D. (2001). The relationship of child worry to cognitive biases: Threat interpretation and likelihood of event occurrence. Behavior Therapy, 32, 425–442. doi:10.1016/S0005-7894(01)80029-0.
Suveg, C., Kendall, P. C., Comer, J. S., & Robin, J. (2006). Emotion-focused cognitive-behavioral therapy for anxious youth: A multiple baseline evaluation. Journal of Contemporary Psychotherapy, 36, 77–85. doi:10.1007/s10879-006-9010-4.
Suveg, C., Sood, E., Comer, J., & Kendall, P. C. (in press). Changes in emotion regulation following cognitive-behavioral therapy for anxious youth. Journal of Clinical Child and Adolescent Psychology.
Suveg, C., & Zeman, J. (2004). Emotion regulation in anxiety-disordered children. Journal of Clinical Child and Adolescent Psychology, 33, 750–759. doi:10.1207/s15374424jccp3304_10.
Thapar, A., & McGuffin, P. (1997). Anxiety and depressive symptoms in childhood: A genetic study of comorbidity. Journal of Child Psychology and Psychiatry, and Allied Disciplines, 38, 651–656. doi:10.1111/j.1469-7610.1997.tb01692.x.
Thompson, R. A. (1994). ER: A theme in search of a definition. The development of emotion regulation: Biological and behavioral considerations. Monographs of the Society for Research in Child Development, 59, 25–52. doi:10.2307/1166137.
Thompson, R. A. (2001). Childhood anxiety disorders from the perspective of emotion regulation and attachment. In M. W. Vasey & M. R. Dadds (Eds.), The developmental psychopathology of anxiety (pp. 160–182). Oxford: Oxford University Press.
Thompson, R. A. (2006). The development of the person: Social understanding, relationships, self, conscience. In W. Damon, R. M. Lerner, & N. Eisenberg (Eds.), Handbook of child psychology (Vol. 3). Social, emotional, and personality development (6th ed., pp. 24–98). New York: Wiley.
Thompson, R. A., & Calkins, S. D. (1996). The double-edged sword: Emotion regulation for children at risk. Development and Psychopathology, 8(1), 163–182.
Thompson, R. A., & Meyer, S. (2007). Socialization of emotion regulation in the family. In J. J. Gross (Ed.), Handbook of emotion regulation (pp. 249–268). New York: The Guilford Press.
Trinder, H., & Salkovskis, P. M. (1994). Personally relevant intrusions outside the laboratory: Long-term suppression increases intrusion. Behaviour Research and Therapy, 32, 833–842. doi:10.1016/0005-7967(94)90163-5.
Tsao, J. C., Mystkowski, J. L., Zucker, B. G., & Craske, M. G. (2002). Effects of cognitive behavioral therapy for panic disorder on comorbid conditions: Replication and extension. Behavior Therapy, 33, 493–509. doi:10.1016/S0005-7894(02)80013-2.
Tsao, J. C., Mystkowski, J. L., Zucker, B. G., & Craske, M. G. (2005). Impact of cognitive-behavioral therapy for panic disorder on comorbidity: A controlled investigation. Behaviour Research and Therapy, 43, 959–970. doi:10.1016/j.brat.2004.11.013.
Turk, C. L., Heimberg, R. G., & Hope, D. A. (2001). Social anxiety disorder. In D. H. Barlow (Ed.), Clinical handbook of psychological disorders: A step-by-step treatment manual (3rd ed., pp. 114–153). New York: The Guilford Press.
van Lang, N. D. J., Ferdinand, R. F., Ormel, J., & Verhulst, F. C. (2006). Latent class analysis of anxiety and depressive symptoms of the Youth Self-Report in a general population sample of young adolescents. Behaviour Research and Therapy, 44(6), 849–860. doi:10.1016/j.brat.2005.06.004.
Vasey, M. W., & Dadds, M. R. (2001). An introduction to the developmental psychopathology of anxiety. In M. W. Vasey & M. R. Dadds (Eds.), The developmental psychopathology of anxiety (pp. 3–26). New York: Oxford University Press.
Vasey, M. W., & MacLeod, C. (2001). Information-processing factors in childhood anxiety: A review and developmental perspective. In M. W. Vasey & M. R. Dadds (Eds.), The developmental psychopathology of anxiety (pp. 253–277). New York: Oxford University Press.
Watson, D., & Clark, L. A. (1984). Negative affectivity: The disposition to experience aversive emotional states. Psychological Bulletin, 96, 465–490. doi:10.1037/0033-2909.96.3.465.
Watson, D., Clark, L. A., & Harkness, A. R. (1994). Structures of personality and their relevance to psychopathology. Journal of Abnormal Psychology, 103, 18–31. doi:10.1037/0021-843X.103.1.18.
Watson, D., Gamez, W., & Simms, L. J. (2005). Basic dimensions of temperament and their relation to anxiety and depression: A symptom-based perspective. Journal of Research in Personality, 39, 46–66. doi:10.1016/j.jrp.2004.09.006.
Weisz, J. R., McCabe, M., & Dennig, M. D. (1994). Primary and secondary control among children undergoing medical procedures: Adjustment as a function of coping style. Journal of Consulting and Clinical Psychology, 62, 324–332. doi:10.1037/0022-006X.62.2.324.
Weisz, J. R., Moore, P. S., Southam-Gerow, M. A., Weersing, V. R., Valeri, S. M., & McCarty, C. A. (1999). Therapist’s manual: Primary and secondary control enhancement training program. Los Angeles: University of California.
Weisz, J. R., Southam-Gerow, M., Gordis, E. B., & Connor-Smith, J. (2003). Primary and secondary control enhancement training for youth depression: Applying the deployment-focused model of treatment development and testing. In A. E. Kazdin & J. R. Weisz (Eds.), Evidence-based psychotherapies for children and adolescents (pp. 165–183). New York: The Guilford Press.
Weisz, J. R., Thurber, C., Sweeney, L., Proffitt, V. D., & LeGagnoux, G. L. (1997). Brief treatment of mild-to-moderate child depression using primary and secondary control enhancement training. Journal of Consulting and Clinical Psychology, 65, 703–707. doi:10.1037/0022-006X.65.4.703.
Wells, A., & Carter, K. (2001). Further tests of a cognitive model of generalized anxiety disorder: Metacognitions and worry in GAD, panic disorder, social phobia, depression, and non-patients. Behavior Therapy, 32, 85–102. doi:10.1016/S0005-7894(01)80045-9.
Whitehouse, W. G., Turanski, W. L., & Murray, L. A. (2000). Cognitive processing anomalies in depressive mood disorders. In F. Columbus (Ed.), Advances in psychology research (Vol. 1, pp. 111–125). Huntington, NY: Nova Science Publishers.
Woodward, L. J., & Fergusson, D. M. (2001). Life course outcomes of young people with anxiety disorders in adolescence. Journal of the American Academy of Child and Adolescent Psychiatry, 40, 1086–1093. doi:10.1097/00004583-200109000-00018.
Yap, M. B. H., Allen, N. B., & Ladouceur, C. D. (2008). Maternal socialization of positive affect: The impact of invalidation on adolescent emotion regulation and depressive symptomatology. Child Development, 79, 1415–1431. doi:10.1111/j.1467-8624.2008.01196.x.
Young, J. E., Weinberger, A. D., & Beck, A. T. (2001). Cognitive therapy for depression. In D. H. Barlow (Ed.), Clinical handbook of psychological disorders (3rd ed., pp. 264–308). New York: The Guilford Press.
Zeman, J., & Garber, J. (1996). Display rules for anger, sadness, and pain: It depends on who’s watching. Child Development, 67, 957–973. doi:10.2307/1131873.
Zeman, J., & Shipman, K. (1997). Social-contextual influences on expectancies for managing anger and sadness: The transition from middle childhood to adolescence. Developmental Psychology, 33, 917–924. doi:10.1037/0012-1649.33.6.917.
Zeman, J., & Shipman, K. (1998). Influence of social context on children’s affect regulation: A functional perspective. Journal of Nonverbal Behavior, 22, 141–1166. doi:10.1023/A:1022900704563.
Zeman, J., Shipman, K., & Penza-Clyve, S. (2001). Development and initial validation of the children’s sadness management scale. Journal of Nonverbal Behavior, 25, 540–547. doi:10.1023/A:1010623226626.
Zeman, J., Shipman, K., & Suveg, C. (2002). Anger and Sadness Regulation: Predictions to Internalizing and Externalizing Symptoms in Children. Journal of Clinical Child and Adolescent Psychology, 31, 393–398.
Acknowledgement
The authors wish to thank Emily Laird for editorial assistance and for help in preparing this manuscript.
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Trosper, S.E., Buzzella, B.A., Bennett, S.M. et al. Emotion Regulation in Youth with Emotional Disorders: Implications for a Unified Treatment Approach. Clin Child Fam Psychol Rev 12, 234–254 (2009). https://doi.org/10.1007/s10567-009-0043-6
Published:
Issue Date:
DOI: https://doi.org/10.1007/s10567-009-0043-6