Abstract
Cytoplasmic vacuolization upon exposure to a variety of chemicals and bioactive substances has been extensively reported. Nearly 30 years have passed since the description by Nobel Laureate Christian de Duve of the mechanism underlying the lysosomal accumulation of lipophilic weak bases referred to these substances as lysosomotropic agents. It has now been revealed, however, that vacuolization occurs upon exposure to compounds other than lipophilic weak bases. Vacuolization of organelles/vesicles other than acidic compartments has also now been reported. In this mini-review, we provide an overview of the origin, mechanism, and possible outcomes of cellular vacuolization during exposure to substances with lysosomotropic as well as other properties.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Cellular vacuolization is a frequently observed phenomenon upon exposure to pharmaceutical agents and other chemicals and has been extensively reported in the literature over many decades (Belkin et al. 1962; Henics and Wheatley 1999; Yang et al. 1965). In 1974, Christian de Duve, who first identified the cellular digestive acidic compartment known as the lysosome, described the mechanism responsible for the lysosomal accumulation of lipophilic amines such as chloroquine and neutral red (de Duve et al. 1974). The sequestration of lipophilic amine within lysosomes, also known as lysosomal trapping, is dependent on the physicochemical properties of these substances. Many amine-containing drugs are weak bases and possess a near neutral pKa. In neutral extracellular environments, these molecules are uncharged and can therefore easily enter cells via simple diffusion. They could be transported not only to the cytoplasm but also to the luminal spaces of intracellular compartments. When these molecules diffuse into the highly acidic lysosomes, they become charged through protonation after which they can no longer traverse the lipid bilayers of membranes and are therefore “trapped” by these acidic compartments (Fig. 1). This is a process that is dependent on physicochemical interactions between the drug in question and the cell. Several assumptions are made in relation to this mechanism, i.e., that (1) the membrane is permeable to lipophilic amine in its uncharged form through passive diffusion or other mechanisms, (2) the membrane is not permeable to lipophilic amine in its charged (protonated) form, and (3) the pH gradient between the lysosome and cytosol is large enough that protonation of lipophilic amines occurs inside the lysosome only.
Mechanism underlying the acidotropic accumulation of lipophilic weak bases. Lipophilic weak base is in its neutral (not-protonated) form (B) under neutral environment. It can enter cells through simple diffusion. When it enters intracellular acidic compartments (such as late endosomes and lysosomes), lipophilic weak base become to be protonated (BH +) and cannot go out of the compartment. Compartments that accumulate lipophilic weak base in their structures became to be enlarged (vacuolated) due to the influx of water
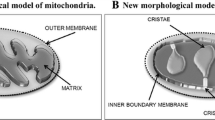
Although overall appearances of the vacuoles look similar under light microscopy, cytoplasmic vacuolization can occur by a wide variety of stimulus, and the vacuoles can be derived from distinct membrane sources (Fig. 2). This is a natural consequence of the facts that there are many acidic compartments other than lysosomes (pH ~5.5) in the cells such as endosomes (pH 6.0–6.5) and the Golgi apparatus (pH 6.0–6.7) (Paroutis et al. 2004). Moreover, cytoplasmic vacuolization is dependent not only on the physicochemical but also on the biological characteristics of the substances in question, as recent reports have shown that cytoplasmic vacuoles can be derived from endoplasmic reticulum (ER) and mitochondria, in which only a slightly acidic milieu is thought to exist (pH ~7.1 for endoplasmic reticulum; 6.7~7.0 for mitochondria) (Paroutis et al. 2004; Soboll et al. 1980). Furthermore, it has been shown that lysosomotropicity is not solely dependent on the physicochemical characteristics of the drugs. Duvvuri and Krise have directly measured the concentrations of two lysosomotropic agents, quinacrine and LysoTracker Red, in the lysosome and found these to be approximately 3- and 15-fold higher than the theoretically estimated levels, respectively. Therefore, physicochemical property of the drugs does not fully accounts even for their lysosomotropicity. In spite of the complex physicochemical as well as biochemical backgrounds, a uniform cellular phenotype is frequently observed during exposure to many types of drugs/stresses, i.e., a massive accumulation of phase-lucent vacuoles in the cytoplasm (Fig. 3). Since there have been many reports describing the occurrence of cytoplasmic vacuolization, we hereafter refer to only representative examples of this process that are caused by fundamentally different mechanisms.
Vacuolation of cellular compartments. Cellular compartments from which cytoplasmic vacuolization is frequently observed during exposure to drugs. Compartments on endosome to lysosome pathway are vacuolated upon exposure to several substances such as phosphoinositide 3-kinase inhibitor wortmannin (Reaves et al. 1996) and H. pylori cytotoxin VacA (Hotchin et al. 2000). Compartments on autophagy to lysosome pathway are vacuolated upon exposure to various substances including chloroquine (Fedorko et al. 1968). Endoplasmic reticulum is vacuolated by a panel of substances such as taxol (Chen et al. 2008), calphostin C (Guo et al. 2003), and 15-deoxy-Δ12,14-prostaglandin J2 (Kar et al. 2009)
Cytoplasmic vacuolization derived from various cellular organelles. a, b Vacuolation from ER. Light micrograph (a) and transmission electron micrograph (b) of HCT116 colon cancer cells upon exposure to 15-deoxy-Δ12,14-prostaglandin J2. Reprinted by permission from Macmillan Publishers Ltd: [Oncogene] (Kar et al. 2009), copyright (2009). c, d Vacuolation from endocytosis to lysosome pathway. Light micrograph (c) and transmission electron micrograph (d) of glioma cells in which the expression of Vps34 was suppressed by expression of shRNA. Reproduced with permission from Journal of Cell Science (Johnson et al. 2006). e, f Cytoplasmic vacuolization from autophagy to lysosome pathway. Light micrograph (e) and transmission electron micrograph (f) of mouse macrophage treated with chloroquine (Fedorko et al. 1968). Originally published in The Journal of Cell Biology 38:377–390 (Fedorko et al. 1968)
Transport into cells
There are at least three pathways by which extracellular substances enter cells: passive diffusion, carrier-mediated transport, and endocytosis (Fig. 4). It has been shown that organic cation transporter (OCT), a member of the SLC family, plays major role in the delivery of organic amines into cells (Koepsell et al. 2007). Carrier-mediated processes would be expected to play important roles in the transport of organic amines into the cells when these agents are added at concentrations around and below the K m value of the carrier systems. However, this might not be case in many of the examples of cytoplasmic vacuolization induced by organic amines. Cytoplasmic vacuolization by these compounds generally occurs at several hundred micromolar or even several millimolar doses (Ohkuma and Poole 1981). These concentrations would typically be several orders of magnitude higher than the K m of the carriers, suggesting a relatively lower contribution of carrier-mediated transport of organic amines to cytoplasmic vacuolization. In addition, cytoplasmic vacuolization by organic amines is generally abolished when the pH of the medium is lowered (Ohkuma and Poole 1981). Hence, most organic amines should be transported into cells in an uncharged form and not in a charged form, during cytoplasmic vacuolization. For example, Morissette et al. (2008, 2004) have extensively reported on cellular vacuolization processes upon exposure to a panel of basic organic compounds including procainamide. These authors have shown that cytoplasmic vacuolization is activated upon exposure to millimolar concentrations of procainamide in rabbit smooth muscle cells. Moreover, this induction of vacuolization by procainamide was not suppressed by any of the inhibitors of membrane cation transporters tested, including that of OCT (Morissette et al. 2008). It was further shown in this study that procainamide-induced vacuolization requires vacuolar proton ATPase, since an inhibitor of this enzyme bafilomycin A1 effectively inhibited this process. Procainamide is transported into cells through a “pseudo transport” mechanism, which involves translocation of the drug in its uncharged form, followed by trapping within the cellular acidic compartment on which vacuolar proton ATPase resides (Morissette et al. 2008). Passive diffusion and/or endocytosis would be regarded as the major route by which lipophilic amines enter cells during cytoplasmic vacuolization.
Cell entry processes of drugs. There are at least three pathway by which drugs enter cells: (1) passive diffusion, (2) carrier-mediated transport, and (3) endocytosis. Carrier-mediated process play major roles in medical actions of the drugs while passive diffusion and endocytosis should be main processes to enter the cells during cytoplasmic vacuolization
Endosomes
Growing evidences indicate that endocytosis should play important role in drug transport during cytoplasmic vacuolization. For example, it has been reported that in some cells, late endosome is vacuolated by inhibition of phosphoinositide 3-kinase pharmacologically (Reaves et al. 1996) as well as genetically (Johnson et al. 2006). Endosomes could also be vacuolated due to the perturbations of endosomal trafficking and/or functions. For example, Helicobacter pylori vacuolating cytotoxin VacA induces endolysosomal vacuolation through disturbing endosomal trafficking (Hotchin et al. 2000; Molinari et al. 1997). Vacuolin-1, a small chemical inhibitor of Ca2+-dependent exocytosis, induces vacuolization from endosome and lysosome (Cerny et al. 2004). Michlik et al. (2003) have shown that vacuolization upon exposure to procaine, a drug that is structurally related to procainamide, is dependent on endocytosis. Interestingly, Morissette et al. (2004) exclude the involvement of endocytosis during procainamide-induced vacuolization. These discrepancies might be derived either from the slight difference in the structures of procaine (ester) and procainamide (amide) or from the cells used (skin fibroblasts in the procaine study and smooth muscle cells for the procainamide experiments). Endocytosis occurs through both clathrin-dependent and clathrin-independent processes. Macropinocytosis is a clathrin-independent bulk fluid uptake process and is mediated by the actin-dependent formation of ruffle membrane/lamellipodia (to surround the extracellular fluid with membrane) and an Na+/H+ exchanger (for membrane closure and to decrease the intra-vesicular pH) (Swanson and Watts 1995). Overmeyer et al. (2008) were the first to describe “methuosis,” a form of cell death caused by hyperstimulation of macropinocytosis upon overexpression of an activated form of the ras oncogene in glioblastoma cells. These authors also reported a series of small molecules that cause cytoplasmic vacuolization in glioblastoma cells even at micromolar concentrations. MIPP, a chalcone (also known as calconoid)-related molecule, has been found to induce massive cytoplasmic vacuolization with characteristics of methuosis (Overmeyer et al. 2011). During methuosis, macropinosomes are transported to the late endosome but not to the lysosome. The late endosome expands to form cytoplasmic vacuoles. Cytoplasmic vacuolization caused by hyperstimulation of macropinocytosis has also been described by a previous study from our laboratory (Nara et al. 2010) as well as a report from another group (Li et al. 2010).
Autophagic vacuole
Cytoplasmic vacuolization via the accumulation of “autophagic vacuoles” is a frequently observed phenomenon when cells are under stress (Kroemer and Levine 2008). Autophagosomes and autolysosomes are cellular compartments formed under nutrient deficient and other pathological conditions (Kroemer and Levine 2008). Autophagosomes contain cytoplasmic proteins and/or organelles in their structures and deliver these contents to lysosomes. Autolysosomes, generated by fusion between autophagosomes and lysosomes, digest contents that are delivered from autophagosomes. In contrast to the relatively small size of autophagosomes (~1 μm in diameter), autolysosomes sometimes expand to fill the cytoplasm (~10 μm in diameter) and therefore often referred to as autophagic vacuoles, which could be observed under light microscopy (Fedorko et al. 1968). These dilated autolysosomes are not true vacuoles, but they are observed as phase-lucent vacuoles due to the dilation of the compartments and the subsequent dilution of their contents. Although autophagy is induced during stressed conditions, it also occurs in the absence of stress and performs essential cellular activities. Hence, there is a possibility that the lysosome dysfunction by lysosomotropic agents results in an accumulation of autolysosomes, which can no longer digest their intravesicular contents. Autophagic vacuoles can be accumulated without any induction of autophagy when lysosomal activity is decreased. Indeed, the lysosomotropic agent chloroquine is used as a stabilizer of autophagosomes and has been shown to cause the accumulation of autophagic vacuoles (Fedorko et al. 1968). Whether autophagic vacuolization is the result of a massive induction of autophagy and/or of severe defects in lysosome function is an issue that will require careful consideration and analysis. This is an issue that has received much attention, and the methods to discriminate between the two possible mechanisms have been established (Mizushima et al. 2010).
Lysosome
Lysosomes are the major targets of lipophilic bases, and a previous study from Ohkuma and Poole (1981) has reported that many drugs, including chloroquine, neutral red, propranolol, atropine, and lidocaine, show the tendency to induce lysosome accumulation. These same authors further showed in additional studies that these lysosomotropic agents promote a substantial increase in the intra-lysosomal pH and thereby a dysfunctional lysosome (Ohkuma and Poole 1978; Poole and Ohkuma 1981). Lysosomal dysfunction caused by lysosomotropic drugs is of importance in relation to the cytotoxicity of these agents and is discussed in a later section.
Endoplasmic reticulum
The ER is involved in protein quality control throughout their life cycle from synthesis to degradation. In addition to autophagy, the ubiquitin–proteasome system is another major degradative process in the cells that is mainly carried out in the ER. ER stress, which often triggers apoptosis, sometimes causes cytoplasmic vacuolization. The vacuolation of the ER proceeds through a mechanism that is essentially distinct from that of the lysosome or endosome. Enlargement/dilation of the ER, which results in the occupation of the cytoplasm by massive vacuoles, is often observed following treatments with proteasome inhibitors such as lactacystin and MG132 (Ding et al. 2007; Ustundag et al. 2007; Wagenknecht et al. 2000). Mimnaugh et al. (2004, 2006) and Ustundag et al. (2007) have observed massive cytoplasmic vacuolization in the SV40-transformed monkey kidney cell line COS-7 upon exposure of these cells to the anticancer drugs geldanamycin and velcade (bortezomib). Geldanamycin is a well-known inhibitor of the chaperone protein HSP90 (Taldone et al. 2008) while velcade is an inhibitor of the proteasome (Chauhan et al. 2005). When cells are exposed to these compounds, cytoplasmic vacuolation occurs even at the concentration of 50 nM geldanamycin plus 10 nM velcade (Mimnaugh et al. 2006). It was further shown in this report that these cytoplasmic vacuoles are derived from the ER as they incorporated red fluorescent protein harboring the KDEL ER localization sequence (Mimnaugh et al. 2006). Recently, Kar et al. (2009) have observed that a thiol-reactive cyclopentenone prostaglandin, 15-deoxy-Δ12,14-prostaglandin J2, causes ER-derived cytoplasmic vacuolization in some cancer cells. All of the cytoplasmic vacuolization, ER stress, and cell death events caused by this molecule were markedly inhibited by a reactive oxygen species scavenger (Kar et al. 2009). Taxol, an anticancer drug, also has been shown to cause ER-derived vacuolization when added at relatively high concentrations (e.g., 70 μM) compared with the dose used to induce mitotic arrest (less than 100 nM) (Chen et al. 2008). Interestingly, calphostin C, a well-known inhibitor for protein kinase C, induces ER-derived vacuolation and subsequent death of the cells that are resistant to pacilitaxel (taxol) (Guo et al. 2003; Kaul and Maltese 2009), indicating its possible usefulness for cancer therapy. Cytoplasmic vacuolization derived from enlarged/dilated ER upon exposure to these drugs could be rationally interpreted as a consequence of excessive ER stress. Although these vacuolization processes are completely different from that induced by lysosomotropic agents, they could not be distinguished by light microscopic observations. Electron microscopic observations, immunocytochemical analyses, and/or fluorescence microscopic observations with appropriate organelle markers are required to elucidate the origin of these vacuoles.
Cytotoxic implications of vacuolization
One of the most significant unsolved questions in relation to cytoplasmic vacuolization is its role in cytotoxicity, particularly cell death. There is limited information on this issue at present. The origin, underlying mechanism, and consequences of cytoplasmic vacuolization vary depending on the nature of the drugs to which the cells have been exposed as well as the cell types in which the vacuoles expand. Cytoplasmic vacuolization may be a cell autonomous process that is designed to protect the cell against toxins. Vacuoles are often cleared after the removal of drugs from the culture medium, suggesting that vacuolization is a reversible process and might be involved in the isolation and buffering of toxins (Henics and Wheatley 1999). However, prolonged exposure to toxic agents and the duration of the resultant cytoplasmic vacuolization might cause irreversible cellular injuries that ultimately lead to cell death (Henics and Wheatley 1999). In support of this possibility, Ohkuma and Poole (1978) have reported that prolonged vacuolation of the lysosome by organic bases results in the release of these substances into cytosol in their cationic forms, suggesting that a permeability transition and/or rupture of the lysosomal membrane had occurred. During the last decade, the release of lysosomal enzymes to the cytoplasm due to an increase in the lysosomal membrane permeability has been reported as one of the triggers of apoptotic cell death (Kroemer and Jaattela 2005). In addition, methuosis, a form of cell death involving the accumulation of late endosomes in the cytoplasm, can be induced by ectopic expression of an activated form of ras, with no exposure to chemicals (Overmeyer and Maltese 2011). During methuosis, cytoplasmic vacuolation persists for several days before the cells eventually die (Overmeyer and Maltese 2011). This might indicate that cytoplasmic vacuolation itself has toxic effects in cells. Other than methuosis, cell deaths associated with cytoplasmic vacuolization are reported including oncosis (Trump et al. 1997), paraptosis (Sperandio et al. 2000), and necroptosis (Han et al. 2007). During the execution of these processes, cytoplasmic vacuolization from the compartments, such as ER and Golgi, is observed along with the swelling of mitochondria. However, there is a possibility that cytoplasmic vacuolization is a process unrelated to cytotoxicity of the stimulants. This might be the case upon infection of gastric epithelial cells with H. pylori. Although the H. pylori vacuolating cytotoxin VacA induces both cytoplasmic vacuolization and mitochondrial apoptosis, recent reports indicate that the vacuolization elicited by VacA is a process that is independent of its cytotoxicity (Willhite et al. 2003; Yamasaki et al. 2006).
Conclusions
A growing body of evidence now indicates that cytoplasmic vacuolization is a phenomenon commonly observed during exposure to various clinically used drugs as well as other substances. Vacuolation of the lysosome, endosome, autolysosome, and ER may suggest that almost all cellular compartments can be dilated and vacuolated. Other than the dilation, cytoplasmic vacuolization could be derived from the homotypic fusion of these compartments (Overmeyer et al. 2011). Although the origin and molecular mechanisms underlying cytoplasmic vacuolization have been extensively studied to date, the pathophysiological significance of cellular vacuolation has not been well characterized. The outcomes from cellular vacuolation are of some importance for a more comprehensive understanding of the cytotoxicity of various pharmaceuticals that are both in current clinical use and still under development.
References
Belkin M, Hardy WG, Orr HC, Lachman AB. Induction in vitro by autonomic drugs of cytoplasmic vacuoles in ascites tumor cells. J Natl Cancer Inst. 1962;28:187–201.
Cerny J, Feng Y, Yu A, Miyake K, Borgonovo B, Klumperman J, et al. The small chemical vacuolin-1 inhibits Ca(2+)-dependent lysosomal exocytosis but not cell resealing. EMBO Rep. 2004;5:883–8.
Chauhan D, Hideshima T, Mitsiades C, Richardson P, Anderson KC. Proteasome inhibitor therapy in multiple myeloma. Mol Cancer Ther. 2005;4:686–92.
Chen TS, Wang XP, Sun L, Wang LX, Xing D, Mok M. Taxol induces caspase-independent cytoplasmic vacuolization and cell death through endoplasmic reticulum (ER) swelling in ASTC-a-1 cells. Cancer Lett. 2008;270:164–72.
de Duve C, de Barsy T, Poole B, Trouet A, Tulkens P, Van Hoof F. Commentary. Lysosomotropic agents. Biochem Pharmacol. 1974;23:2495–531.
Ding WX, Ni HM, Yin XM. Absence of Bax switched MG132-induced apoptosis to non-apoptotic cell death that could be suppressed by transcriptional or translational inhibition. Apoptosis. 2007;12:2233–44.
Fedorko ME, Hirsch JG, Cohn ZA. Autophagic vacuoles produced in vitro. I. Studies on cultured macrophages exposed to chloroquine. J Cell Biol. 1968;38:377–91.
Guo B, Hembruff SL, Villeneuve DJ, Kirwan AF, Parissenti AM. Potent killing of paclitaxel- and doxorubicin-resistant breast cancer cells by calphostin C accompanied by cytoplasmic vacuolization. Breast Cancer Res Treat. 2003;82:125–41.
Han W, Li L, Qiu S, Lu Q, Pan Q, Gu Y, et al. Shikonin circumvents cancer drug resistance by induction of a necroptotic death. Mol Cancer Ther. 2007;6:1641–9.
Henics T, Wheatley DN. Cytoplasmic vacuolation, adaptation and cell death: a view on new perspectives and features. Biol Cell. 1999;91:485–98.
Hotchin NA, Cover TL, Akhtar N. Cell vacuolation induced by the VacA cytotoxin of Helicobacter pylori is regulated by the Rac1 GTPase. J Biol Chem. 2000;275:14009–12.
Johnson EE, Overmeyer JH, Gunning WT, Maltese WA. Gene silencing reveals a specific function of hVps34 phosphatidylinositol 3-kinase in late versus early endosomes. J Cell Sci. 2006;119:1219–32.
Kar R, Singha PK, Venkatachalam MA, Saikumar P. A novel role for MAP1 LC3 in nonautophagic cytoplasmic vacuolation death of cancer cells. Oncogene. 2009;28:2556–68.
Kaul A, Maltese WA. Killing of cancer cells by the photoactivatable protein kinase C inhibitor, calphostin C, involves induction of endoplasmic reticulum stress. Neoplasia. 2009;11:823–34.
Koepsell H, Lips K, Volk C. Polyspecific organic cation transporters: structure, function, physiological roles, and biopharmaceutical implications. Pharm Res. 2007;24:1227–51.
Kroemer G, Jaattela M. Lysosomes and autophagy in cell death control. Nat Rev Cancer. 2005;5:886–97.
Kroemer G, Levine B. Autophagic cell death: the story of a misnomer. Nat Rev Mol Cell Biol. 2008;9:1004–10.
Li C, Macdonald JI, Hryciw T, Meakin SO. Nerve growth factor activation of the TrkA receptor induces cell death, by macropinocytosis, in medulloblastoma Daoy cells. J Neurochem. 2010;112:882–99.
Michalik M, Pierzchalska M, Pabianczyk-Kulka A, Korohoda W. Procaine-induced enhancement of fluid-phase endocytosis and inhibition of exocytosis in human skin fibroblasts. Eur J Pharmacol. 2003;475:1–10.
Mimnaugh EG, Xu W, Vos M, Yuan X, Isaacs JS, Bisht KS, et al. Simultaneous inhibition of hsp 90 and the proteasome promotes protein ubiquitination, causes endoplasmic reticulum-derived cytosolic vacuolization, and enhances antitumor activity. Mol Cancer Ther. 2004;3:551–66.
Mimnaugh EG, Xu W, Vos M, Yuan X, Neckers L. Endoplasmic reticulum vacuolization and valosin-containing protein relocalization result from simultaneous hsp90 inhibition by geldanamycin and proteasome inhibition by velcade. Mol Cancer Res. 2006;4:667–81.
Mizushima N, Yoshimori T, Levine B. Methods in mammalian autophagy research. Cell. 2010;140:313–26.
Molinari M, Galli C, Norais N, Telford JL, Rappuoli R, Luzio JP, et al. Vacuoles induced by Helicobacter pylori toxin contain both late endosomal and lysosomal markers. J Biol Chem. 1997;272:25339–44.
Morissette G, Moreau E, Gaudreault RC, Marceau F. Massive cell vacuolization induced by organic amines such as procainamide. J Pharmacol Exp Ther. 2004;310:395–406.
Morissette G, Lodge R, Marceau F. Intense pseudotransport of a cationic drug mediated by vacuolar ATPase: procainamide-induced autophagic cell vacuolization. Toxicol Appl Pharmacol. 2008;228:364–77.
Nara A, Aki T, Funakoshi T, Uemura K. Methamphetamine induces macropinocytosis in differentiated SH-SY5Y human neuroblastoma cells. Brain Res. 2010;1352:1–10.
Ohkuma S, Poole B. Fluorescence probe measurement of the intralysosomal pH in living cells and the perturbation of pH by various agents. Proc Natl Acad Sci U S A. 1978;75:3327–31.
Ohkuma S, Poole B. Cytoplasmic vacuolation of mouse peritoneal macrophages and the uptake into lysosomes of weakly basic substances. J Cell Biol. 1981;90:656–64.
Overmeyer JH, Maltese WA. Death pathways triggered by activated Ras in cancer cells. Front Biosci. 2011;16:1693–713.
Overmeyer JH, Kaul A, Johnson EE, Maltese WA. Active ras triggers death in glioblastoma cells through hyperstimulation of macropinocytosis. Mol Cancer Res. 2008;6:965–77.
Overmeyer JH, Young AM, Bhanot H, Maltese WA. A chalcone-related small molecule that induces methuosis, a novel form of non-apoptotic cell death, in glioblastoma cells. Mol Cancer. 2011;10:69.
Paroutis P, Touret N, Grinstein S. The pH of the secretory pathway: measurement, determinants, and regulation. Physiology (Bethesda). 2004;19:207–15.
Poole B, Ohkuma S. Effect of weak bases on the intralysosomal pH in mouse peritoneal macrophages. J Cell Biol. 1981;90:665–9.
Reaves BJ, Bright NA, Mullock BM, Luzio JP. The effect of wortmannin on the localisation of lysosomal type I integral membrane glycoproteins suggests a role for phosphoinositide 3-kinase activity in regulating membrane traffic late in the endocytic pathway. J Cell Sci. 1996;109(Pt 4):749–62.
Soboll S, Elbers R, Scholz R, Heldt HW. Subcellular distribution of di- and tricarboxylates and pH gradients in perfused rat liver. Hoppe Seylers Z Physiol Chem. 1980;361:69–76.
Sperandio S, de Belle I, Bredesen DE. An alternative, nonapoptotic form of programmed cell death. Proc Natl Acad Sci U S A. 2000;97:14376–81.
Swanson JA, Watts C. Macropinocytosis. Trends Cell Biol. 1995;5:424–8.
Taldone T, Gozman A, Maharaj R, Chiosis G. Targeting Hsp90: small-molecule inhibitors and their clinical development. Curr Opin Pharmacol. 2008;8:370–4.
Trump BF, Berezesky IK, Chang SH, Phelps PC. The pathways of cell death: oncosis, apoptosis, and necrosis. Toxicol Pathol. 1997;25:82–8.
Ustundag Y, Bronk SF, Gores GJ. Proteasome inhibition-induces endoplasmic reticulum dysfunction and cell death of human cholangiocarcinoma cells. World J Gastroenterol. 2007;13:851–7.
Wagenknecht B, Hermisson M, Groscurth P, Liston P, Krammer PH, Weller M. Proteasome inhibitor-induced apoptosis of glioma cells involves the processing of multiple caspases and cytochrome c release. J Neurochem. 2000;75:2288–97.
Willhite DC, Cover TL, Blanke SR. Cellular vacuolation and mitochondrial cytochrome c release are independent outcomes of Helicobacter pylori vacuolating cytotoxin activity that are each dependent on membrane channel formation. J Biol Chem. 2003;278:48204–9.
Yamasaki E, Wada A, Kumatori A, Nakagawa I, Funao J, Nakayama M, et al. Helicobacter pylori vacuolating cytotoxin induces activation of the proapoptotic proteins Bax and Bak, leading to cytochrome c release and cell death, independent of vacuolation. J Biol Chem. 2006;281:11250–9.
Yang WC, Strasser FF, Pomerat CM. Mechanism of drug-induced vacuolization in tissue culture. Exp Cell Res. 1965;38:495–506.
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Aki, T., Nara, A. & Uemura, K. Cytoplasmic vacuolization during exposure to drugs and other substances. Cell Biol Toxicol 28, 125–131 (2012). https://doi.org/10.1007/s10565-012-9212-3
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s10565-012-9212-3